Abstract
Background
The purpose of this study was to evaluate the relationship between preoperative inflammatory markers (neutrophil-lymphocyte ratio and platelet-lymphocyte ratio) and cervical stromal involvement in patients with endometrioid adenocarcinoma.
Methods
We studied 318 patients with endometrioid adenocarcinoma who underwent comprehensive surgical staging. We used univariate and multivariate analyses of cervical stromal involvement and receiver-operating curves to calculate optimal cutoff values for neutrophil-lymphocyte and platelet-lymphocyte ratios to predict cervical stromal involvement.
Results
The presence of cervical stromal involvement was associated with neutrophil-lymphocyte ratio and platelet-lymphocyte ratio (P = 0.009 and P = 0.031, respectively). Multivariate analysis showed that higher neutrophil-lymphocyte and platelet-lymphocyte ratios independently predicted cervical stromal involvement (odds ratio 3.10, 95% confidence interval 1.10–8.76, P = 0.032, and odds ratio 5.27, 95% confidence interval 1.94–14.35, P = 0.001, respectively). At a threshold of 2.01, the neutrophil-lymphocyte ratio was 71.0% sensitive and 63.8% specific for stromal involvement; at a 172.24 threshold, the platelet-lymphocyte ratio was 48.4% sensitive and 88.9% specific.
Conclusion
Preoperative neutrophil-lymphocyte and platelet-lymphocyte ratios can help identify the risk of cervical stromal involvement in patients with endometrial cancer. Evaluating these ratios may help select patients who should be particularly watched and tested for cervical stromal involvement.
Introduction
Endometrioid adenocarcinoma is the most common gynecological cancer in the western world.Citation1 Most endometrial cancer presents with disease limited to the uterus, but 7%–15% of cases present with some cervical stromal involvement. Patients with cervical stromal involvement have significantly worse prognoses than those whose endometrial cancer is confined to the uterine body. Furthermore, cervical stromal involvement is considered to increase the risk of lymph node metastasis. For patients with cervical involvement, radical hysterectomy including parametrectomy and lymphadenectomy may be advocated. The Surveillance Epidemiology and End Results analysis of 932 patients with International Federation of Gynecology and Obstetrics (FIGO) stage II endometrial cancer indicated a better prognosis using radical hysterectomy than simple hysterectomy.Citation2 For patients undergoing lymphadenectomy, more surgical blood loss, longer surgical time, and high complication rates were reported.Citation3 Thus, preoperatively identifying patients at high risk for cervical stromal involvement, and who may need radical surgery and lymphadenectomy is important in terms of both treatment and prognosis. Unfortunately, preoperative evaluation methods, including fractional curettage, transvaginal sonography, and hysteroscopic assessment, are not sensitive enough to detect cervical stromal involvement.Citation4,Citation5 Although magnetic resonance imaging is highly sensitive and specific for cervical stromal involvement, it is costly and time-consuming.Citation6 Therefore, development of a noninvasive and readily available preoperative test is needed to identify patients with cervical stromal involvement in endometrial cancer.
Inflammation evidently plays an important role in development of cancer and its progression.Citation7 Systemic inflammatory markers have been reported to be prognostic and predictive markers in various kinds of cancers.Citation8 C-reactive protein is one index of systemic inflammation. However, C-reactive protein is not routinely measured as part of preoperative examination. The neutrophil to lymphocyte ratio (NLR) is another marker of systemic inflammatory response,Citation9 and some studies have shown elevated NLR to be a significant prognostic factor in patients with various malignancies.Citation8 The platelet to lymphocyte ratio (PLR) is reportedly a significant prognostic indicator in resected pancreatic cancer.Citation10 However, little is known about the predictive values of NLR and PLR in endometrial cancer, and only a few studies have evaluated their predictive value for lymph node metastasis in the disease.Citation11
To the best of our knowledge, there have been no reports about the predictive value of inflammatory markers for cervical stromal involvement in endometrioid adenocarcinoma. Therefore, in this study, we evaluated the relationship between preoperative inflammatory markers and cervical stromal involvement in endometrioid adenocarcinoma.
Materials and methods
Retrospective data were collected for patients treated by surgical staging procedures between January 2003 and June 2012 at Peking Union Medical College Hospital. Eligibility criteria for this study included histologically confirmed endometrioid adenocarcinoma, and comprehensive surgical staging, including pelvic or para-aortic lymph node dissection. Patients with second malignancies, hematological disease, inflammatory disease, recombinant granulocyte colony-stimulating factor use, or missing preoperative complete blood cell count or complete blood cell count drawn more than two weeks prior to surgery were excluded. Patients who had undergone prior chemotherapy or pelvic radiation were excluded. Surgical staging consisted of peritoneal cytology, total abdominal hysterectomy, bilateral salpingooophorectomy, and systemic pelvic lymphadenectomy with or without para-aortic lymphadenectomy. Radical hysterectomy was performed when cervical stromal involvement was suspected. Pelvic lymphadenectomy includes the common iliac and obturator nodes above the obturator nerve.
Patients were staged according to the 2009 FIGO guidelines. Endometrial cancer was graded according to FIGO classification. Complete blood cell count, age, stage, histologic grade, lower uterine segment involvement, presence of lymphovascular invasion, depth of myometrial invasion, cervical stromal involvement, positive peritoneal cytology, and pelvic or para-aortic lymph node status were reviewed from patients’ medical records. The study was approved by the institutional review board of Peking Union Medical College Hospital.
The NLR was defined as the absolute neutrophil count divided by the absolute lymphocyte count; similarly, PLR was defined as the absolute platelet count divided by the absolute lymphocyte count.
Statistical analyses
Categorical variables were analyzed using Pearson’s Chisquare test and Fisher’s Exact test. Continuous variables were expressed as the mean ± standard deviation and compared using the Student’s t-test. Univariate and multivariate analyses were used to assess relationships between the various factors and cervical stromal involvement. Odds ratios (OR) with 95% confidence interval (CI) were calculated by univariate or multivariate analysis using the logistic regression test. Sensitivity and specificity for different NLR and PLR cutoffs were calculated with receiver-operating curves. Receiver-operating curve analysis was plotted to investigate optimal cutoff values that maximized sensitivity and specificity. All statistical analyses were performed using the Statistical Package for Social Sciences version 16.0 software (SPSS Inc, Chicago, IL, USA). P < 0.05 was considered to be statistically significant.
Results
Three hundred and eighteen patients (mean age 55.14 years) with endometrioid adenocarcinoma who met the criteria were included in the study. The distribution of surgical FIGO stages was 254 in stage I, 19 in stage II, 41 in stage III, and four in stage IV. Of the 318 patients, 31 (9.75%) presented with cervical stromal involvement.
shows the clinicopathological features of the patients with and without cervical stromal involvement. Cervical stromal involvement was more common in the presence of advanced FIGO stage, higher grades of tumor, lower uterine segment involvement, deep myometrial invasion, positive lymph node status, and positive adnexal involvement (P < 0.001, P = 0.035, P < 0.001, P = 0.002, P < 0.001, and P = 0.024, respectively). Logistic regression analysis found that only lower uterine segment involvement and positive lymph node status were independent risk factors for cervical stromal involvement (OR 9.18, 95% CI 3.17–26.58, P < 0.001, and OR 4.82, 95% CI 1.21–19.21, P = 0.026, respectively).
Table 1 Patient characteristics and pathological findings in patients with or without cervical stromal involvement
Mean counts of white blood cell subtypes, platelets, NLR, and PLR are shown in . Mean values for white blood cells, neutrophils, platelets, NLR, and PLR were increased in the positive group (P = 0.012, P < 0.001, P = 0.001, P = 0.009, and P = 0.031, respectively). There was no significant difference in the mean value for lymphocytes between the two groups.
Table 2 Mean white blood cell subtype counts, neutrophil-to-lymphocyte ratio, and platelet-to-lymphocyte ratio in study subjects
The cutoff values for preoperative NLR and PLR predicting the presence of cervical stromal involvement along with receiver-operating curves are shown in . An optimal cutoff value that maximized the sum of sensitivity and specificity in the receiver-operating curve was used. The best cutoff value for NLR was 2.01, which was 71.0% sensitive and 63.8% specific for the presence of cervical stromal involvement. The best cutoff value for PLR was 172.24, which was 48.4% sensitive and 88.9% specific. NLR and PLR were independent predictors of cervical stromal involvement in patients with endometrial cancer when using 2.01 (NLR) and 172.24 (PLR) as threshold values (OR 3.10, 95% CI 1.10–8.76, P = 0.032, and OR 5.27, 95% CI 1.94–14.35, P = 0.001, respectively, ).
Figure 1 Receiver-operating curve for the relationship between NLR and PLR and cervical involvement.
Abbreviations: NLR, neutrophil-lymphocyte ratio; PLR, platelet-lymphocyte ratio.
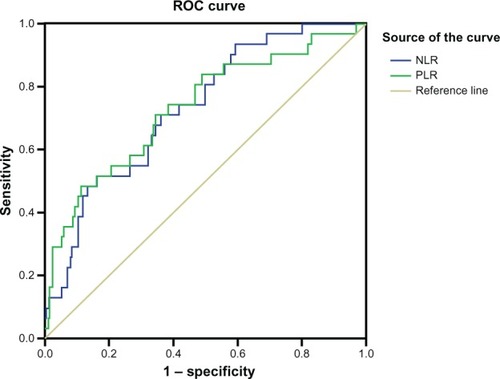
Table 3 Effect of univariate and multivariate variables on the presence of cervical stromal involvement in patients with endometrial cancer
Discussion
To our knowledge, this is the first study to describe an association between preoperative NLR and PLR and cervical stromal involvement in endometrioid carcinoma. Our results show that preoperative NLR and PLR are independent predictors of cervical stromal involvement in the disease.
Endometrial cancer with cervical stromal involvement has a worse prognosis than cancer confined to the corpus uteri.Citation12 Cervical stromal involvement should also be considered a risk factor for lymph node metastasis; in our cases, lymph node metastasis rates were 22.6% and 4.9%, respectively, in cases with and without cervical stromal involvement. For patients with cervical stromal involvement, radical hysterectomy and systemic lymphadenectomy were required to identify extension of disease and the type of adjuvant therapy. These patients may also benefit from primary radical hysterectomy, with removal of the uterus, cervix, parametrium, and upper vagina.Citation13 A publication by the US National Institute of Cancer reported that patients with stage II disease had better survival after radical surgery than after simple hysterectomy.Citation2 Therefore, preoperative evaluation of cervical stromal involvement may be needed to determine the best surgical approach.
Different preoperative diagnostic tools were used to evaluate the cervical stromal involvement in endometrial cancer. Transvaginal sonographies followed by endometrial sampling or diagnostic hysteroscopy with biopsy are often used. However, there has been no consensus as to the best predictor of cervical stromal involvement.Citation14 Endocervical curettage as a part of a procedure that includes dilation and curettage under general anesthesia is costly and may lead to complications in elderly patients.Citation6 Magnetic resonance imaging with contrast enhancement is highly sensitive and specific in detecting cervical stromal involvement, but is also costly, time-consuming, and often unavailable, and requires contrast agents that can cause allergic reactions.Citation15
The association between cancer and inflammation was discovered over a century ago. Cancer-related inflammation causes suppression of antitumor immunity by recruiting regulatory T cells and activating chemokines, which results in tumor growth and metastasis.Citation10 The presence of both neutrophilia and thrombocytosis tends to represent a nonspecific response to cancer-related inflammation.Citation10 The mechanism between preoperative leukocytosis and neutrophilia and cancer remains unclear. However, cancer has been shown to produce myeloid growth factors, such as granulocyte colony-stimulating factor, interleukin (IL)-1, IL-6, and tumor necrosis factor-alpha, which may influence tumor-related leukocytosis and neutrophilia.Citation8 Neutrophilia promotes development and progression of cancer by providing a suitable environment and secreting most circulating vascular endothelial growth factors.Citation16 In a study by Worley et al in patients with leukocytosis in endometrial carcinoma, presentations accompanied by pathologic factors associated with poorer prognoses and with leukocytosis were independently associated with increased risk of death.Citation17 Tavares-Murta et al showed that in patients with cervical cancer, those with advanced cancers had significantly higher frequency of leukocytes alterations than did those with preinvasive cancers, and that neutrophilia was the best indicator of cancer invasiveness.Citation18
The underlying mechanism for the relationship between platelet expression and the biologic behavior of cancer cells is unclear. Thrombocytosis may be mediated by megakaryocytes and their precursors as a result of stimulation by proinflammatory mediators such as IL-1, IL-2, and IL-6.Citation19 An elevated platelet count may simply be an additional indicator of the severity of inflammation.Citation10
A major risk factor for endometrial cancer is a low-grade inflammatory state. Chronic inflammation, through its association with insulin resistance and estrogen production, might mediate the obesity-related increase in risk of endometrial cancer.Citation20 Dossus et al report that elevated prediagnostic levels of the inflammatory markers C-reactive protein, IL6, and IL1Ra were associated with an increased risk of endometrial cancer.Citation20 In a multicenter study, elevated serum C-reactive protein was associated with a less favorable prognosis in patients with surgically treated endometrial cancer.Citation21 However, C-reactive protein is not routinely measured in clinic. Elevated NLR and PLR are likely to represent nonspecific responses to cancer-related inflammation. Many studies have shown elevated NLR and PLR to be prognostic factors in various kinds of cancers.Citation8,Citation10 Although NLR and PLR have been associated with lymph node metastasis in endometrial cancer,Citation11 we have seen no previous report on the relationship between inflammatory markers and cervical stromal involvement.
Our most interesting finding here is that elevated preoperative NLR and PLR were correlated with an increased risk of cervical stromal involvement, which was noted after multivariate analysis. Cervical stromal involvement was significantly associated with both elevated NLR and PLR (OR 3.10, 95% CI 1.10–8.76, P = 0.032, and OR 5.27, 95% CI 1.94–14.35, P = 0.001, respectively).
Although preoperative assessment of cervical stromal involvement using magnetic resonance imaging is highly sensitive and specific, this method is also expensive; however, preoperative leukocyte, neutrophil, and platelet counts are routinely performed for such patients. Thus, NLR and PLR may be an accessible preliminary tool to select patients for further evaluation of cervical stromal involvement, eg, via magnetic resonance imaging.
The current investigation has the limitations common to all retrospective studies. Incomplete blood counts might have falsely elevated inflammatory marker values. In addition, C-reactive protein is not routinely measured at our center, and its association with cervical stromal involvement in endometrial cancer could not be analyzed in our study.
In conclusion, this report shows, for the first time, a relationship between systemic inflammatory markers and cervical stromal involvement in endometrial cancer. Preoperative NLR and PLR independently predict cervical stromal involvement in the disease, and may help select patients who should be especially evaluated for cervical stromal involvement.
Disclosure
The authors report no conflicts of interest in this work.
References
- DollAAbalMRigauMNovel molecular profiles of endometrial cancer – new light through old windowsJ Steroid Biochem Mol Biol20081083–522122918061438
- CornelisonTLTrimbleELKosaryCLSEER data, corpus uteri cancer: treatment trends versus survival for FIGO stage II, 1988–1994Gynecol Oncol199974335035510479492
- LarsonDMJohnsonKOlsonKAPelvic and paraaortic lymphadenectomy for surgical staging of endometrial cancer: morbidity and mortalityObstet Gynecol199279699810011579330
- FotiouSVlahosNKondi-PafitiAIntraoperative gross assessment of myometrial invasion and cervical stromal involvement in endometrial cancer: role of tumor grade and sizeGynecol Oncol2009112351752019117598
- LoKWCheungTHYimSFChungTKPreoperative hysteroscopic assessment of cervical invasion by endometrial carcinoma: a retrospective studyGynecol Oncol200182227928211531280
- HaldorsenISBergAWernerHMMagnetic resonance imaging performs better than endocervical curettage for preoperative prediction of cervical stromal invasion in endometrial carcinomasGynecol Oncol2012126341341822609110
- MantovaniAAllavenaPSicaACancer-related inflammationNature2008454720343644418650914
- KwonHCKimSHOhSYClinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancerBiomarkers201217321622222424597
- ZahorecRRatio of neutrophil to lymphocyte counts – rapid and simple parameter of systemic inflammation and stress in critically illBratisl Lek Listy2001102151411723675
- BhattiIPeacockOLloydGLarvinMHallRIPreoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus platelet-lymphocyte ratioAm J Surg2010200219720320122680
- SuhDHKimHSChungHHPre-operative systemic inflammatory response markers in predicting lymph node metastasis in endometrioid endometrial adenocarcinomaEur J Obstet Gynecol Reprod Biol2012162220621022445206
- MorrowCPBundyBNKurmanRJRelationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: a Gynecologic Oncology Group studyGynecol Oncol199140155651989916
- CohnDEWoesteEMCacchioSClinical and pathologic correlates in surgical stage II endometrial carcinomaObstet Gynecol200710951062106717470583
- AlmogBGutmanGLessingJBGrisaruDPrediction of cervical stromal involvement in endometrial cancer by hysteroscopyArch Gynecol Obstet20072751454816906402
- AkbayirOCorbaciogluANumanogluCPreoperative assessment of myometrial and cervical invasion in endometrial carcinoma by transvaginal ultrasoundGynecol Oncol2011122360060321700322
- KusumantoYHDamWAHospersGAMeijerCMulderNHPlatelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factorAngiogenesis20036428328715166496
- WorleyMJJrNitschmannCCShoniMThe significance of preoperative leukocytosis in endometrial carcinomaGynecol Oncol2012125356156522465698
- Tavares-MurtaBMMendoncaMAODuarteNLSystemic leukocyte alterations are associated with invasive uterine cervical cancerInt J Gynecol Cancer20102071154115921495217
- KlingerMHJelkmannWRole of blood platelets in infection and inflammationJ Interferon Cytokine Res200222991392212396713
- DossusLRinaldiSBeckerSObesity, inflammatory markers, and endometrial cancer risk: a prospective case-control studyEndocr Relat Cancer20101741007101920843938
- SchmidMSchneitterAHinterbergerSAssociation of elevated C-reactive protein levels with an impaired prognosis in patients with surgically treated endometrial cancerObstet Gynecol200711061231123618055714