Abstract
One of the most important molecules mediating the proliferation, growth, and metastasis of cancer cells is insulin-like growth factor (IGF), with its receptor IGF-1R. Here, we describe the potential of an IGF-1R monoclonal antibody, HX-1162, on liver cancer apoptosis in vitro and in vivo. We found that HX-1162 could induce the apoptosis of cultured liver cancer cells. Additionally, HX-1162 treatment inhibited the tumor growth after cancer cell grafting and enhanced the cell apoptosis inside the tumor tissue. We conclude that IGF-1R targeting therapy provides a new avenue toward treating liver cancer.
Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of death due to cancer. In most patients, chronic inflammation or cirrhosis contributes to the exacerbation of the disease.Citation1–Citation3 One of the most important molecules mediating the proliferation, growth, and metastasis of cancer cells is insulin-like growth factor (IGF), with its main receptor type 1 insulin-like growth factor (IGF-1R).Citation4 IGF-1R signaling activates both mitogenic and anti-apoptotic pathways. In many tumor conditions, increased expression of IGF-1 and/or IGF-2, which are IGF-1R ligands, has been found. The specific blockade of IGF-1R could decrease tumor xenograft growth and cause apoptosis of tumor cells, suggesting it may be of high therapeutic value.
In recent years, different monoclonal antibodies for IGF-1R have been developed as an intervention tool for tumor treatments. For instance, MK-0646 (Merck, Whitehouse Station, NJ, USA) was shown to reduce IGF-1R activities and tumor cell proliferation,Citation5 while IMC-A12 (ImClone, New York, NY, USA) showed similar effects and inhibited tumor xenograft growth.Citation6,Citation7 Moreover, when combined with chemotherapy, CP-751871 (Pfizer, New York, NY, USA) demonstrated promising activities in Phase II and III trials.Citation8 All these results serve as the rationale for the use of IGF-1R monoclonal antibodies to treat cancer, including HCC.
In the study reported here, we examined the effects of a recently produced IGF-1R monoclonal antibody, HX-1162, on liver cancer apoptosis. We found that HX-1162 is highly effective in inducing cancer cell apoptosis in a short period. This result strongly argues for the application of IGF-1R-based therapies.
Materials and methods
Generation of HX-1162
HX-1162 was generated by ETSCSH Biotech (Shanghai, People’s Republic of China) in 2010. The purification, protein binding, and verification were undertaken by ETSCSH Biotech and SHENGi Biotech (Zhengzhou, People’s Republic of China).
Cell culture
Human liver cancer cell line (Hep G2) was obtained by SHENGi Biotech and cultured in Dulbecco’s modified Eagle medium with 100 mg/mL streptomycin, 100 mg/mL penicillin, and 10% fetal bovine serum at 37°C with a 5:95 O2 to CO2 air supply. All reagents were from Shanghai Shenggong Biotech (Shanghai, People’s Republic of China).
3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay
MTT assay was used to measure cell viability. Cells were plated in 96-well plates and incubated with and without HX-1162 for 24/48 hours. Then MTT solution (5 mg/mL in phosphate-buffered saline, 150 μL per well) was added and the plates were incubated for a further 2 hours. Finally, the supernatant was removed and discarded and formazan crystals dissolved in dimethyl sulfoxide were added (150 μL per well). The absorbance at 570/630 nm of each sample was measured using a special plate reader HZ320X (BIO-EER, Zhengzhou, People’s Republic of China). The experiments were repeated five times for each condition.
Caspase-3 and terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assays
Apoptotic activity was measured using either a caspase-3 activity kit (Merck, Darmstadt, Germany) or a TUNEL kit (Roche, Penzberg, Germany). Staining was performed according to the manufacturers’ directions. With fluorescence labeling, flow cytometry was performed for apoptotic cell sorting. In addition, cells at five random sites were counted at 40× magnification to determine positive rates of apoptotic staining.
Animal study
A total of 200 Kunming adult mice (normal mice) (male, aged 2–3 months old) were used in the animal study. Hep G2 cells (2 × 107) suspended in saline were injected subcutaneously (back skin) for xenograft development. Following this, each of three groups of ten mice were administered saline, HX-1162 10 mg/kg, or HX-1162 20 mg/kg every 2 days for 1 month (starting from the day of xenograft).
Finally, the animals were sacrificed at different time points (0, 5, 10, 15, 20, 25, and 30 days after the graft) and the tumor sizes were measured. Paraffin-embedded tissues were cut at 4 μm for TUNEL assay, and hematoxylin and eosin staining was also used to count the number of apoptotic cells.
The animal study was approved by the Animal Research Ethics Committee for the Use of Live Animals for Biomedical Research in The First Affiliated Hospital of Xinxiang Medical University.
Statistical analysis
Data are presented as mean ± standard deviation. Statistical analysis was performed using SPSS software (v 16.0; IBM, Armonk, NY, USA) and t-tests were used to compare differences between groups. P values < 0.05 were considered statistically significant.
Results
Effect of HX-1162 on cancer cell viability
We found that HX-1162 treatment significantly decreased cell viability, with the number of viable cells significantly decreasing after 24 and 48 hours (). After 24 hours, in the control group, 99.8% ± 0.1% of the cells were viable, while in the treated group, the percentage of viable cells was only 27.0% ± 9.4%. A further 48 hours after treatment, 99.7% ± 0.03% of the cells were still viable in the control group while only 18.6% ± 7.8% were viable in the treated group.
Table 1 Effect of HX-1162 on cancer cell viability
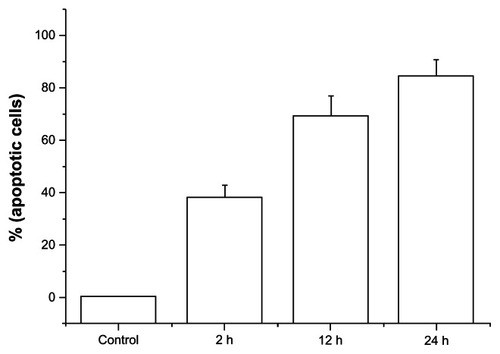
Effect of HX-1162 on cancer cell apoptosis in vitro
HX-1162 was found to lead to cancer cell apoptosis, as determined by TUNEL staining (). In the control group, only 0.2% ± 0.03% of cells were apoptotic, while in the HX-1162 groups, at 2 hours, 37.7% ± 5.1% of cells were apoptotic (P < 0.01); at 12 hours, 69.2% ± 7.7% of cells were apoptotic (P < 0.001); and at 24 hours, 84.1% ± 6.4% of cells were apoptotic (P < 0.001).
Effect of HX-1162 on cancer cell apoptosis in vivo
HX-1162 treatment significantly decreased tumor graft growth in vivo (). Additionally, within smaller tumors, the number of apoptotic cells was found to have increased. In tissues obtained at 30 days, the percentage of TUNEL-positive cells harvested from tumors in the mice was 1.7% ± 0.3% in the saline group, 29.5% ± 7.4% (P < 0.01) in the HX-1162 10 mg/kg group, and 36.4% ± 8.9% (P < 0.01) in the HX-1162 20 mg/kg group (). Similar changes were also found in tumor tissues harvested from other time points (data not shown).
Figure 2 Effect of HX-1162 on tumor growth in vivo.
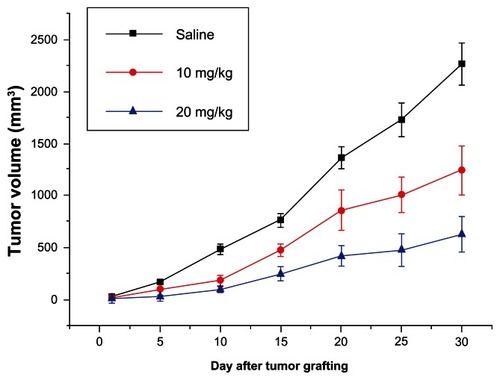
Table 2 HX-1162-induced cancer cell apoptosis in vivo (30 days)
Discussion
IGF-1R signaling activates both mitogenic and anti-apoptotic pathways in cancer cells. It has been shown that IGF-1R targeting therapy may eliminate the tumor progression in diverse types of cancer.Citation5–Citation8 However, the direct application of IGF-1R monoclonal antibodies on liver cancer cells has not been well investigated. The present study further verified the application of IGF-1R monoclonal antibodies on liver cancer, which is consistent with the fact that IGF-1R is involved in liver cancer development and progression.Citation2,Citation4,Citation5,Citation9–Citation11
Here, we found that the newly developed IGF-1R monoclonal antibody HX-1162 could induce apoptosis of cultured liver cancer cells. Additionally, HX-1162 treatment inhibited tumor growth after cancer cell grafting and enhanced cell apoptosis inside the tumor tissue. This is consistent with previous studies that have shown that antagonizing IGF-1R activities reduces tumor cell proliferationCitation5 and inhibits tumor xenograft growth.Citation6,Citation7 Moreover, IGF-1R monoclonal antibody treatment has been combined with chemotherapy in clinical trials with promising results.Citation8 The interruption was specific without adverse effects and no abnormal behaviors were observed in healthy mice receiving this antibody for a chronic period (2 weeks to 2 months) (data not shown).
Conclusion
IGF-1R targeting therapy offers a potential new method for treating liver cancer. We are planning to combine HX-1162 with other chemotherapy drugs in future studies. In addition, it will be necessary to examine the effects of HX-1162 on established tumors to validate this treatment as a therapy.
Acknowledgment
The authors were supported by The First Affiliated Hospital of Xinxiang Medical University.
Disclosure
The authors declare no conflicts of interest in this work.
References
- KleinJDawsonLAHepatocellular Carcinoma Radiation Therapy: Review of Evidence and Future OpportunitiesInt J Radiat Oncol Biol Phys Epub December 6, 2012
- AravalliRNCressmanENSteerCJCellular and molecular mechanisms of hepatocellular carcinoma: an updateArch Toxicol201387222724723007558
- Della CorteCColomboMSurveillance for hepatocellular carcinomaSemin Oncol201239438439822846857
- PsyrriAArkadopoulosNVassilakopoulouMSmyrniotisVDimitriadisGPathways and targets in hepatocellular carcinomaExpert Rev Anticancer Ther201212101347135723176622
- TovarVAlsinetCVillanuevaAIGF activation in a molecular subclass of hepatocellular carcinoma and pre-clinical efficacy of IGF-1R blockageJ Hepatol201052455055920206398
- RowinskyEKSchwartzJDZojwallaNBlockade of insulin-like growth factor type-1 receptor with cixutumumab (IMC-A12): a novel approach to treatment for multiple cancersCurr Drug Targets201112142016203321777192
- RowinskyEKYoussoufianHTonraJRSolomonPBurtrumDLudwigDLIMC-A12, a human IgG1 monoclonal antibody to the insulin-like growth factor I receptorClin Cancer Res20071318 Pt 25549s5555s17875788
- KarpDDPaz-AresLGNovelloSPhase II study of the anti-insulin-like growth factor type 1 receptor antibody CP-751,871 in combination with paclitaxel and carboplatin in previously untreated, locally advanced, or metastatic non-small-cell lung cancerJ Clin Oncol200927152516252219380445
- RubinJAyoubNKaldasFSaabSManagement of recurrent hepatocellular carcinoma in liver transplant recipients: a systematic reviewExp C lin Transplant2012106531543
- Abu El MakaremMAn overview of biomarkers for the diagnosis of hepatocellular carcinomaHepat Mon20121210 HCCe612223162601
- TanakaSAriiSMolecular targeted therapies in hepatocellular carcinomaSemin Oncol201239448649222846865