Abstract
Anaplastic thyroid cancer represents 1%–2% of thyroid cancers. For its aggressiveness, it is considered a systemic disease at the time of diagnosis. Surgery remains the cornerstone of therapy in resectable tumor. Traditional chemotherapy has little effect on metastatic disease. A multimodality approach, incorporating cytoreductive surgical resection, chemoradiation, either concurrently or sequentially, and new promising target therapies is advisable. Doxorubicin is the most commonly used agent, with a response rate of 22%. Recently, other chemotherapy agents have been used, such as paclitaxel and gemcitabine, with superimposable activity and response rates of 10%–20%. However, survival of patients with anaplastic thyroid cancer has changed little in the past 50 years, despite more aggressive systemic and radiotherapies. Several new agents are currently under investigation. Some of them, such as sorafenib, imatinib, and axitinib have been tested in small clinical trials, showing promising disease control rates ranging from 35%–75%. Referral of patients for participation in clinical trials is needed.
Introduction
Anaplastic thyroid cancer (ATC) represents 1%–2% of all thyroid tumors and is characterized by aggressive, local invasion and common distant metastases. Histologically, ATC is characterized by elevated mitotic rate and lymphovascular invasion.Citation1
All patients with ATC are classified by the American Joint Committee on Cancer as having stage IV disease (IVa, intrathyroidal tumors; IVb, gross extrathyroidal; IVc, distant metastases). It affects prevalently the female sex; the ratio 3:1 is lower than the papillary or follicular histotypes.Citation1
The peak incidence occurs during the sixth to seventh decades of life. Anaplastic carcinoma has a poor 5-year survival rate (0–25%). Based on epidemiological studies derived from the Surveillance, Epidemiology and End Results Database, the incidence of ATC has held steady in the United States during the period between 1973 and 2002.Citation1
Clinically, patients refer with growing neck mass, dysphagia, cough, neck pain, and dyspnea. ATC is believed to occur from a terminal dedifferentiation of previously undetected long-standing thyroid carcinoma (eg, papillary, follicular).
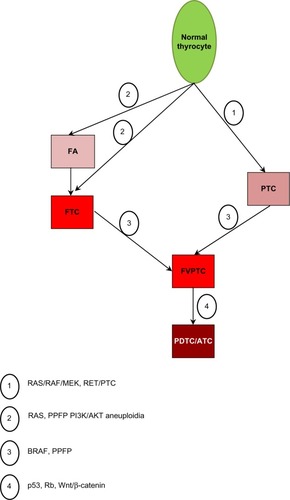
ATC has a genetic association with oncogenes C-myc, H-ras, and Nm23. Mutations in BRAF, RAS, catenin (cadherin-associated protein) beta 1, PIK3CA, TP53, AXIN1, PTEN, and APC genes have been found in ATC, and chromosomal abnormalities are common.Citation2,Citation3 summarizes the main route of tumor progression and dedifferentiation.
Figure 1 The main route of tumor progression and dedifferentiation.
Preoperative cervical ultrasonography can detect lymph node metastases. Cervical computed tomography scanning can be used to define the local spread of disease. Detection of distant metastases to the mediastinum, lung, liver, bone, and brain is also possible, via computed tomography scanning or MRI. Bone scanning can be used to determine the presence of bone metastases. Positron emission tomography with 18F-fluorodeoxyglucose can be successfully used in ATC to detect lymph node metastases, lung metastases, and other distant metastases. Fine needle aspiration often yields enough cytological information to allow diagnosis, but sometimes an open surgical biopsy is required. Grossly, ATC is a large, fleshy, off-white tumor. Infiltration of adjacent structures can be observed grossly and microscopically. Histologically, the tumor may contain regions of spontaneous necrosis and hemorrhage. Typically, vascular invasion is detectable.Citation1–Citation73
The main histological variants include spindle cell, giant cell (osteoclast-like), squamous, and pauci-cellular. The giant cell subtype typically exhibits local calcification with significant osteoid formation. The pauci-cellular subtype demonstrates rapid growth, intense fibrosis, focal infarction, diffuse calcification, and encroachment of adjacent vascular tissue by atypical spindle cells.Citation4
Thyroid lymphoma is the only curable condition that may be confused with ATC. It is fundamental to rule out lymphoma in the presence of a poorly differentiated large cell thyroid tumor. This investigation involves lymphoid tissue markers (eg, cytoplasm immunoglobulin, immunoglobulin receptors, and gene rearrangement studies). When the tumor is surgically resectable, a tracheostomy is often required because of compression of the trachea. Total thyroidectomy is effective in reducing local symptoms produced by the tumor mass. However, surgery alone is not able to control the disease, even in patients with small intrathyroidal masses.Citation1
Radiotherapy (RT) is used to improve loco-regional control (LRC), often with chemotherapy (CT). External RT, up to 65 Gy, may slow the progress of the disease but rarely controls it. ATC has a rapid course and early dissemination.Citation20 The most common sites of distant spread include, in descending order, the lung, bone, and brain. Metastases, particularly in the lung, are likely to be present at diagnosis more than fifty percent of the time.Citation73
CT is often added concurrently with RT but appears to have a limited effect on survival in most studies.Citation10,Citation21,Citation37
Some studies report better LRC when RT and CT are administered in a preoperative setting. Whether surgery should be given upfront or after neoadjuvant treatment is an open issue.
However, both the heterogeneity of retrospective series and the absence of randomized trials do not allow recommendation of a standard treatment. Recently, the publication of guidelines by the American Thyroid Association (ATA)Citation74 taskforce on ATC offered a significant direction in the management of this disease.
In the last few years, biologically targeted therapies for advanced thyroid carcinomas have been proposed on the basis of the recognition of key oncogenic mutations. New treatments are needed for this highly aggressive malignancy.
This review will analyze ATC molecular characteristics, preclinical studies results and clinical management, and discuss possible emerging therapies.
Material and methods
A comprehensive literature review was finalized in February, 2013. Medline® was used for research. Electronic search results were supplemented by hand searching of selected papers, expert consensus meeting notes, and reference lists from selected articles. The literature search was limited to articles in English and humans. The following medical subject heading terms were used in the search: thyroid cancer, emerging therapies, anaplastic thyroid carcinoma, chemotherapy, radiotherapy. We analyzed and discussed the literature, taking into account the previously reported reviews on this matter. In short, we analyzed data from: 29 preclinical studies on genetic ATC alterations and target therapies, 14 clinical reviews, and 38 clinical studies, of these only 17 were prospective studies (see and ).
Table 1 Treatment of anaplastic thyroid cancer
Table 2 Most significant trials on molecular target therapies used in anaplastic thyroid cancer treatment
Molecular characteristics
Anaplastic cells do not express thyroid-specific genes; they do not produce thyroglobulin, are unable to transport iodine; and thyrotropin receptors are not found on their plasma membranes.
ATC has a more complex and less distinct gene profile than papillary and follicular cancer, and molecular data suggests it may de-differentiate from well-differentiated thyroid cancer (WDTC). In about one-third of ATC cases, probably those arising from pre-existing papillary differentiated thyroid cancer (PTC), the BRAF(V600E) mutation (2–3) is present. It is also suggested that ATC might develop from RAS-mutated follicular thyroid cancer (FTC), since RAS mutation is also detected in 6%–50% of ATC.Citation2 The refractory nature of ATC to therapy may occur, at least in part, due to the presence of cancer stem cells, which have been identified in ATC cell lines.Citation63
In ATC, a mutation of PIK3CA gene causing AKT and ERK activation was reported.Citation3,Citation4,Citation68 Many of the genetic alterations found in ATC could potentially activate both the MAPK and PI3K/AKT pathways, including RTK gene copy gain, RET/PTC, and RAS mutations. schematizes some of the most important pathways.
Figure 2 Anaplastic thyroid cancer growth pathways.
Abbreviations: MAP, Mitogen-activated protein; ZO, zonula occludens; MAPK, MAP kinase; mTOR, mammalian target of rapamycin; ERK, extracellular signal-regulated kinase; PI3K, phosphoinositide 3 kinase; RET, rearranged during transfection; EGFR, epidermal growth factor receptor; RAS, rat sarcoma; RAF, rapidly accelerated fibrosarcoma; PIP, phosphatidylinositol phosphate; PTC, papillary thyroid cancer; AKT, alpha serine/threonine-protein kinase; PTEN, phosphatase and tensin homolog; P, phosphate; PCL, phospholipase C.
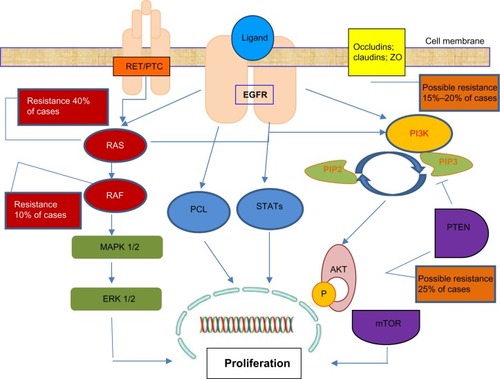
The BRAF mutation, which can activate the MAPK pathway, commonly coexisted with genetic alterations that could activate the PI3K/AKT pathway (eg, the PIK3CA copy gain) in ATC. AKT1 was activated in most ATC cases (85%–93%),Citation5,Citation6 and ERK was activated in 65%.Citation6 Phosphatase and tensin homology encoding chromosome 10 (PTEN) negatively regulates the PI3K pathway, and was mutated in 17% of 48 cases.Citation7,Citation8
Aurora kinases play an important role in cell division, and deregulation may result in aneuploidy. Aurora B is overexpressed in ATC cell lines,Citation9 and patient samples had a marked increase when compared with normal thyroid tissue or PTCs.Citation9 Like aurora B, aurora A is overexpressed at both the mRNA and protein levels in ATC cell lines, while aurora C is increased only at the protein level.Citation8
Genetic alterations or their combinations that could activate both the MAPK and PI3K/AKT pathways were found in up to 81% cases of ATC.Citation7
PIK3CA/AKT1 mutations and PIK3CA copy gain are frequently identified in ATC, as compared to well differentiated cancer, suggesting that PI3K/mTOR pathway activity is involved in the process of cancer de-differentiation.Citation70
Additional mutations frequently observed in ATC involve p53 and β-catenin. The tumor-suppressor gene p53 is fundamental for the progression from indolent to aggressive thyroid cancer. The inactivating p53 mutation, seldom detected in WDTC, is found in about 55% of PTC and ATC.Citation2 Membrane β-catenin expression is progressively reduced with loss of tumor differentiation, resulting in tumor invasiveness, and increasing metastatic potential.Citation5
Treatments
Treatment of ATC has ranged from surgery, radiotherapy, chemotherapy, or a combination of these regimens. Any modality used alone usually fails to control local disease, which is often the cause of death. Complete resection of ATC in the neck usually is not possible, but surgery can be an effective palliative modality. Extensive radical neck operations with en bloc adjacent organ resection are associated with high morbidity and are probably not warranted for this disease.Citation61 Postoperative RT, as well as palliative RT is widely used.
Agents used for chemotherapy usually include doxorubicin and analogs, but paclitaxel, cisplatin, carboplatinum, VP-16, cyclophosphamide, melphalan, and bleomycin are also used.
However, no standards of care for ATC are approved.
This depends on the lack of few statistically significant data in this population. Additionally, due to the rarity of the disease, few patients are enrolled in clinical trials. ATA recommends a comprehensive multimodality plan to establish treatment strategy.
Radiotherapy
Radiotherapy for ATC has changed from palliative low dose of standard RT to altered fractionation RT (hyper fractionation) and higher dose (>40 Gy). Since ATC is a rapidly dividing tumor, hyperfractionated RT or the combination of CRT minimizes tumor cell repopulation. External beam RT to the neck or mediastinum was administered to total doses ranging from 45–75 Gy.Citation1
Wang et al (2006) demonstrate the importance of a radical dose of radiotherapy: ie, patients with good performance status and no distant metastases who received radical radiotherapy (>40 Gy) versus [vs] those with poor performance status or distant metastases, had a median survival of 11.1 and 3.2 months, respectively.Citation20
High dose accelerated RT improves the response rate to RT but toxicity is hardly manageable. Hyperfractionated RT seems to be more effective for local control than conventional treatment.Citation27
Several authors have assessed the efficacy and feasibility of postoperative radiotherapy. Higher locoregional control is associated with accelerated RT and free surgical margins.Citation40
Chemotherapy and chemoradiotherapy
Doxorubicin was considered the most effective drug for ATC until a few years ago. In a randomized study of ECOG, the combination of cisplatin and doxorubicin was shown to be more effective than doxorubicin alone, with higher complete RR.
Combination chemotherapy with bleomycin, doxorubicin, and cisplatin resulted in a response rate of 40% in advanced thyroid cancer, producing considerable palliative effects. It is noteworthy that best responses to this regimen were observed often in patients with ATC.Citation11 Several other reports confirmed that a combination CT versus doxorubicin alone is more effective (RR 5% vs 18%).Citation17
Preclinical studies showed that paclitaxel inhibited growth in multiple ATC cell lines,Citation13 causing cell cycle arrest, apoptosis, and phosphorylation of multiple signaling kinases (JNK, ERK, AKT1).Citation12 Based on preclinical data, an open-label Phase II clinical trial of paclitaxel as a 96-hour infusion was conducted, achieving a favorable outcome: overall response rate (ORR) = 53%, disease progression (DP) = 42%, stable disease (SD) = 5%, partial regression (PR) = 47%, or complete regression (CR) = 5%; overall survival (OS) = 6 m, median survival (mOS) = 7 and 32 weeks in responders and non-responders respectively.Citation14
Long-term survivors were also reported among patients with stage IVb and IVc disease using weekly paclitaxel administration as induction CT,Citation15 while no significant OS difference was assessed among stage IVc patients.Citation13
The paclitaxel effects on apoptosis and tubulin acetylation are both enhanced by the histone deacetylase inhibitor, valproic acid.Citation16
Inhibition of cell cycle progression is an important strategy for reducing tumor growth: in ATC cell lines, gemcitabine, a nucleoside analog, induces G1/S arrest. The cytotoxic effect is additive if followed by cisplatin. Of interest, these drugs produce an antagonistic response when given in reverse order, as cisplatin inhibits gemcitabine incorporation into DNA.Citation12
Chemotherapy improved the effect of RT in locoregional and distant control. Weekly administration of low-dose doxorubicin concurrently with RT showed an acceptable toxicity and may be a therapeutic option for patients with ATC (2-y LRC: 68%; mOS: 1 y).Citation10
Haigh et alCitation21 reported the results of resected patients treated with CRT; with 8/26 patients being long survivors after postoperative CRT. In patients treated with potentially curative resection, median survival was 43 months compared with 3 months with palliative resection (P < 0.002).Citation21
No association was found between survival and age, prior goiter, prior thyroid carcinoma, adjacent differentiated carcinoma, or tumor size.
reports some of the most impressive studies using RT and CT therapies in ATC.
In Turin, Italy, 27 patients were treated in a 5-year period.Citation22 Surgery was performed initially (maximum debulking in 11 and palliative in 6). Chemotherapy (doxorubicin + cisplatin) was given during and after radiation. The approach in five patients was neoadjuvant CRT followed when possible by surgery, while five others had paclitaxel therapy alone. As in other series, surgical resection was the major contributor to patient responses. While median survival was only 3.9 months, those with maximal debulking had a 6-month survival of 58%; those with palliative or no surgery, only 10%.Citation22
Akaishi et al reported a retrospective series of 100 patients with ATC, treated between 1993 and 2009. Patients received surgery followed by RT with or without CT. Nineteen of the 100 patients survived for more than 1 year, and most of these underwent a complete resection, as opposed to debulking, followed by adjuvant radiotherapy with or without chemotherapy. However, the overall survival at 2 years remains dismal (12.3%).Citation37
Emerging therapies
There is a growing interest in target therapies and preclinical findings, in order to improve the dismal results obtained with conventional chemotherapy and chemoradiation in ATC.
Much has been learned about the genes, RNAs, and proteins deregulated. A lot of new drugs have been investigated but only few were demonstrated to be effective in both preclinical and clinical investigations.Citation79–Citation82
EGFR inhibitors
The frequent presence of endothelial growth factor receptor (EGFR) in ATC tumors and pleiotropy of its effects makes it an attractive target for drug development. Gefitinib, a tyrosine kinase inhibitor, slows down cell growth, although high doses are necessary in ATC cells. Early stage clinical trials have been performed in combination with docetaxel but results are dismal.Citation45,Citation46
The monoclonal antibody cetuximab should induce apoptosis but evidence for this is conflicting.Citation46,Citation47 In preclinical trials, Kim et alCitation85 observed that combination therapy with cetuximab/irinotecan inhibits the growth and progression of orthotopic ATC in nude mice.
An interesting dual inhibitor of EGFR and vascular EGFR (VEGFR), AEE788, was shown in ATC cells to increase apoptosis and inhibit both cell proliferation and the phosphorylation of multiple proteins.Citation44,Citation47 Kim et al (2005) showed that dual inhibition in combination with paclitaxel, is effective.Citation44
Multikinase inhibitors, mTOR inhibitors, MEK inhibitors, and other emerging therapies
Imatinib, another tyrosine kinase inhibitor with multiple targets, (eg, BCR-ABL1; c-KIT; PDGFR) has variable activity in ATC cell lines.Citation44–Citation46 However, imatinib does not achieve its effects at clinically achievable concentrations, although a recent clinical trial in 11 patients achieved a disease control rate in 6, with 6-month PFS = 27% and 6-month OS = 46%.Citation75
Other agents that have shown cytostatic effects in preclinical settings are in the clinical phase of investigation, such as plitidepsin, TP53-expressing adenovirus, mammalian target of rapamycin (mTOR) inhibitors and thiazolidinediones (TZDs), MEK inhibitors (AZD6244), tubulin-binding agents, and combretastatin A.Citation48–Citation50
Combretastatin A (CA4P) achieved satisfactory results in Phase II–III studies;Citation76 in the Phase III trial, its combination with carboplatin and paclitaxel showed a 35% reduction in the risk of death (1-y OS = 27% vs 9% with CT + CA4P vs CT respectively; P = 0.065).Citation83
Unsatisfactory results were obtained with axitinib and pazopanib monotherapy, even if an association of pazopanib and paclitaxel appears promising.Citation52,Citation53 Nevertheless, most of these trials with targeted agents were based on limited numbers of patients; therefore, all interesting results should be confirmed.
However, at the 2012 Italian Oncology Meeting, Spallanzani et al presented experience from Modena University Hospital with TKIs: 9 patients treated with sunitinib (7 patients) and sorafenib (2 patients) confirmed the efficacy and safety profile of TKIs in ATC.Citation58
A Phase II study of sorafenib in ATC patientsCitation71 and an international multicenter Phase III trial of sorafenib versus placebo in patients with iodine-refractory thyroid cancer (NCT00984282)Citation72 are ongoing.
Given the genomic instability of ATC, effective therapies may benefit from comprehensive microarray analysis or genome-wide screening to develop an individualized therapeutic regimen that maximally inhibits major pathways at multiple genetic and epigenetic levels. In addition, to more fully characterize the complex molecular profile, subsequent rapid in vitro screening assays of combinations of targeted therapies may further optimize a patient’s treatment plan. Finally, refinement may derive from evolving drug delivery systems such as nanoparticles.Citation63,Citation64
Recently valproic acid (VPA) was investigated in preclinical studies and showed highly efficacy in suppressing the growth of poorly differentiated thyroid cancer cell lines, inducing apoptosis and cell cycle. Its activity is limited in VPA monotherapy but it may be added to CT, as it enhances the cytotoxicity of doxorubicin and increases radiosensitivity.Citation16–Citation44
Panobinostat (LBH589) is a hydroxamic acid with potent inhibitory activity at low nanomolar concentrations against all classes of histone deacetylases (pan-deacetylases inhibitor).Citation55–Citation80
In vitro treatment with LBH589 resulted in impairment of cell viability, inhibition of colony formation, cell cycle arrest, and apoptosis induction. Recently, it has been reported that two histone deacetylase inhibitors, trichostatin A and vorinostat, induced miR-129-5p overexpression, histone acetylation, and cell death in papillary and anaplastic cancer cell lines, and in primary cultures of papillary thyroid cancer.
Disruption of the E-cadherin/catenin complex contributes to tumor metastasis, and decreased expression of E-cadherin is observed in advanced stage, poorly differentiated carcinomas, and is associated with the transformation of differentiated carcinomas. Loss of E-cadherin is associated with the transformation in ATC.Citation69
Wunderlich et alCitation57 reported that vandetanib inhibited tumor growth of the ATC cell lines in vivo (Hth83 and 8505C by 69.3% [P < 0.001] and 66.6% [P < 0.05], respectively), when compared to control. The authors concluded that the tremendous in vivo anti-tumor activity of vandetanib against ATC makes it an attractive candidate for further preclinical as well as clinical development for the treatment of this particularly virulent cancer, which remains effectively untreatable.Citation57
Inhibition of the proteasome pathway with bortezomib is also a strategy to evaluate in in-vivo experiments, as it showed proapoptotic activity on ATC.Citation58
Aurora kinases inhibitors (MLN8054) had proapoptotic and antiproliferative effects in ATC cells. The antitumoral activity is increased with the association of bortezomib.Citation83
Another critical serine-threonine protein kinase involved in the MAPK pathway that has been targeted to block its constitutive kinase activation is BRAF.Citation66,Citation67
BRAF mutation (V600E) is reported in 24% of papillary-derived ATC. Preclinical and clinical studies investigating combination therapy with agents such as selective (PLX4032) and potent (BAY 73-4506 and ARQ 736) small-molecule BRAF inhibitors, and MAP/ERK kinase inhibitors (AZD6244) hold great promise in the treatment of BRAF(V600E) ATC.Citation65,Citation66,Citation68
In a mouse model, the BRAF inhibitor PLX4720 suppressed growth of mutated human anaplastic thyroid cancer. A case report by Rosove et al was recently published in the New England Journal of Medicine.Citation59
PI3K/mTOR inhibitors are also under investigation at different levels of clinical studies. For example, BEZ235 reduces PI3K and mTOR kinase activity by competitive binding to the ATP-binding cleft of these enzymes.Citation67,Citation69,Citation70,Citation79
reports the most significant trials on molecular target therapies used in ATC treatment.
Conclusion
The outcome after treatment of ATC remains disappointing. However, knowledge about management of anaplastic tumors is increasing, and this information must be shared to improve outcomes. Indeed, this tumor was neglected by oncologists, and many doctors are still not informed about treatment options, in particular, drugs. The weakness of these studies on novel targeted agents is low accrual in clinical trials, also due to the rarity of the disease and its rapid evolution.
A multimodality approach should represent the standard treatment of choice in ATC, with surgery being the cornerstone of management of early stage patients. Notably, surgery remains the most important treatment modality when a complete resection may be obtained.
The role of preoperative or postoperative CRT remains controversial, although the use of both surgery and chemoradiation correlates with a better outcome.
A major concern of CRT is toxicity, which negatively impacts the completion of protocol. However, it improves both local and distant control, although it appears recommendable mostly for fit patients.
Because ATC management is very challenging, researchers look at emerging target therapies with a lot of interest. However, although there are promising results in preclinical development, only few studies on new molecules have been clinically confirmed. Clearly, a better understanding of the molecular pathogenesis driving the disease is required to define new therapeutic strategies. This knowledge might provide useful drugs to be used both alone or in combination with conventional methods. In short, the hope of a novel treatment strategy comes from unsatisfactory results from conventional therapies. An effort of every institution to allow clinical trials participation is required.
Confirmatory data from these new therapeutic strategies are needed.
Acknowledgments
The authors express thanks to Lawrence Preston for copy-editing, and Lega Italiana Tumori, Sezione di Cuneo for fundraising.
Disclosure
The authors report no conflicts of interest in this work.
References
- NagaiahGHossainAMooneyCJParmentierJRemickSCAnaplastic thyroid cancer: a review of epidemiology, pathogenesis, and treatmentJ Oncol2011201154235821772843
- NikiforovaMNNikiforovYEMolecular diagnostics and predictors in thyroid cancerThyroid200919121351136119895341
- SmallridgeRCMarlowLACoplandJAAnaplastic thyroid cancer: molecular pathogenesis and emerging therapiesEndocr Relat Cancer2009161174418987168
- BibleKCSmallridgeRCMorrisJCDevelopment of a multidisciplinary, multicampus subspecialty practice in endocrine cancersJ Oncol Pract20128Suppl 3e1se5s22942830
- XingMGenetic alterations in the phosphatidylinositol-3 kinase/Akt pathway in thyroid cancerThyroid201020769770620578891
- García-RostánGCostaAMPereira-CastroIMutation of the PIK3CA gene in anaplastic thyroid cancerCancer Res20056522101991020716288007
- SantarpiaLEl-NaggarAKCoteGJMyersJNShermanSIPhosphatidylinositol 3-kinase/akt and ras/raf-mitogen-activated protein kinase pathway mutations in anaplastic thyroid cancerJ Clin Endocrinol Metab200893127828417989125
- LiuDXingMPotent inhibition of thyroid cancer cells by the MEK inhibitor PD0325901 and its potentiation by suppression of the PI3K and NF-kappaB pathwaysThyroid200818885386418651802
- UlisseSDelcrosJGBaldiniETollerMExpression of Aurora genes kinases in human thyroid carcinoma cell lines and tissuesInt J Cancer2006119227528216477625
- KimJHLeeperRDTreatment of anaplastic giant and spindle cell carcinoma of the thyroid gland with combination adriamycin and radiation therapy. A new approachCancer19835269549576883279
- De BesiPBusnardoBTosoSCombined chemotherapy with bleomycin, adriamycin, and platinum in advanced thyroid cancerJ Endocrinol Invest19911464754801723086
- VoigtWBulankinAMullerTSchedule-dependent antagonism of gemcitabine and cisplatin in human anaplastic thyroid cancer cell linesClin Cancer Res2000652087209310815936
- PushkarevVMStarenkiDVSaenkoVAMolecular mechanisms of the effects of low concentrations of taxol in anaplastic thyroid cancer cellsEndocrinology200414573143315215044368
- AinKBEgorinMJDeSimonePATreatment of anaplastic thyroid carcinoma with paclitaxel: phase 2 trial using ninety-six-hour infusion. Collaborative Anaplastic Thyroid Cancer Health Intervention Trials (CATCHIT) GroupThyroid200010758759410958311
- HigashiyamaTItoYHirokawaMInduction chemotherapy with weekly paclitaxel administration for anaplastic thyroid carcinomaThyroid201020171420025538
- CatalanoMGPoliRPuglieseMFortunatiNBoccuzziGValproic acid enhances tubulin acetylation and apoptotic activity of paclitaxel on anaplastic thyroid cancer cell linesEndocr Relat Cancer200714383984517914112
- VoigtWKegelTWeissMMuellerTSimonHSchmollHJPotential activity of paclitaxel, vinorelbine and gemcitabine in anaplastic thyroid carcinomaJ Cancer Res Clin Oncol2005131958559016021466
- ShimaokaKSchoenfeldDADeWysWDCreechRHDeContiRA randomized trial of doxorubicin versus doxorubicin plus cisplatin in patients with advanced thyroid carcinomaCancer1985569215522213902203
- WangSLloydRVHutzlerMJSafranMSPatwardhanNAKhanAThe role of cell cycle regulatory protein, cyclin D1, in the progression of thyroid cancerMod Pathol200013888288710955455
- WangYTsangRAsaSDicksonBArenovichTBrierleyJClinical outcome of anaplastic thyroid carcinoma treated with radiotherapy of once- and twice-daily fractionation regimensCancer200610781786179216967442
- HaighPIItuartePHWuHSCompletely resected anaplastic thyroid carcinoma combined with adjuvant chemotherapy and irradiation is associated with prolonged survivalCancer200191122335234211413523
- BrignardelloEGalloMBaldiIAnaplastic thyroid carcinoma: clinical outcome of 30 consecutive patients referred to a single institution in the past 5 yearsEur J Endocrinol2007156442543017389456
- VoutilainenPEMultanenMHaapiainenRKLeppaniemiAKSivulaAHAnaplastic thyroid carcinoma survivalWorld J Surg1999239975978 discussion 978–979.10449831
- TanRKFinleyRKIIIDriscollDBakamjianVHicksWLJrSheddDPAnaplastic carcinoma of the thyroid: a 24-year experienceHead Neck1995114147 discussion 47–48.7883548
- VenessMJPorterGSMorganGJAnaplastic thyroid carcinoma: dismal outcome despite current treatment approachANZ J Surg200474755956215230790
- SchlumbergerMParmentierCDelisleMJCouetteJEDrozJPSarrazinDCombination therapy for anaplastic giant cell thyroid carcinomaCancer19916735645661985750
- MitchellGHuddartRHarmerCPhase II evaluation of high dose accelerated radiotherapy for anaplastic thyroid carcinomaRadiother Oncol1999501333810225555
- BesicNAuerspergMUs-KrasovecMGolouhRFrkovic-GrazioSVodnikAEffect of primary treatment on survival in anaplastic thyroid carcinomaEur J Surg Oncol200127326026411373102
- De CrevoisierRBaudinEBachelotACombined treatment of anaplastic thyroid carcinoma with surgery, chemotherapy, and hyperfractionated accelerated external radiotherapyInt J Radiat Oncol Biol Phys20046041137114315519785
- KobayashiTAsakawaHUmeshitaKTreatment of 37 patients with anaplastic carcinoma of the thyroidHead Neck199618136418774920
- Swaak-KragtenATde WiltJHSchmitzPIBontenbalMLevendagPCMultimodality treatment for anaplastic thyroid carcinoma – treatment outcome in 75 patientsRadiother Oncol200992110010419328572
- VrbicSPejcicIVrbicMFilipovicSTherapy of stage IV B anaplastic thyroid carcinoma: single institution experienceJ BUON2009141414419373945
- YauTLoCYEpsteinRJLamAKWanKYLangBHTreatment outcomes in anaplastic thyroid carcinoma: survival improvement in young patients with localized disease treated by combination of surgery and radiotherapyAnn Surg Oncol20081592500250518581185
- LimSMShinSJChungWYTreatment outcome of patients with anaplastic thyroid cancer: a single center experienceYonsei Med J201253235235722318823
- LeeJJFoukakisTHashemiJMolecular cytogenetic profiles of novel and established human anaplastic thyroid carcinoma modelsThyroid200717428930117465858
- McIverBHayIDGiuffridaDFAnaplastic thyroid carcinoma: a 50-year experience at a single institutionSurgery200113061028103411742333
- AkaishiJSuginoKKitagawaWPrognostic factors and treatment outcomes of 100 cases of anaplastic thyroid carcinomaThyroid201121111183118921936674
- HeronDEKarimpourSGrigsbyPWAnaplastic thyroid carcinoma: comparison of conventional radiotherapy and hyperfractionation chemoradiotherapy in two groupsAm J Clin Oncol200225544244612393980
- NilssonOLindebergJZedeniusJAnaplastic giant cell carcinoma of the thyroid gland: treatment and survival over a 25-year periodWorld J Surg19982277257309606289
- TennvallJLundellGWahlbergPAnaplastic thyroid carcinoma: three protocols combining doxorubicin, hyperfractionated radiotherapy and surgeryBr J Cancer200286121848185312085174
- JunorEJPaulJReedNSAnaplastic thyroid carcinoma: 91 patients treated by surgery and radiotherapyEur J Surg Oncol199218283881582515
- LevendagPCDe PorrePMvan PuttenWLAnaplastic carcinoma of the thyroid gland treated by radiation therapyIntl J Radiat Oncol Biol Phys199326125128
- DerbelOLimemSSégura-FerlayCResults of combined treatment of anaplastic thyroid carcinoma (ATC)BMC Cancer20111146922044775
- KimSSchiffBAYigitbasiOGTargeted molecular therapy of anaplastic thyroid carcinoma with AEE788Mol Cancer Ther20054463264015827337
- NobuharaYOnodaNYamashitaYEfficacy of epidermal growth factor receptor-targeted molecular therapy in anaplastic thyroid cancer cell linesBr J Cancer20059261110111615785737
- KurebayashiJOkuboSYamamotoYAdditive antitumor effects of gefitinib and imatinib on anaplastic thyroid cancer cellsCancer Chemother Pharmacol200658446047016435154
- HoffmannSBurchertAWunderlichADifferential effects of cetuximab and AEE 788 on epidermal growth factor receptor (EGF-R) and vascular endothelial growth factor receptor (VEGF-R) in thyroid cancer cell linesEndocrine20073110511317873319
- PodtchekoAOhtsuruATsudaSThe selective tyrosine kinase inhibitor, STI571, inhibits growth of anaplastic thyroid cancer cellsJ Clin Endocrinol Metab2003881889189612679488
- BlagosklonnyMVGiannakakouPWojtowiczMEffects of p53-expressing adenovirus on the chemosensitivity and differentiation of anaplastic thyroid cancer cellsJ Clin Endocrinol Metab199883251625229661637
- BonofiglioDQiHGabrieleSPeroxisome proliferator activated receptor γ inhibits follicular and anaplastic thyroid carcinoma cells growth by upregulating p21Cip1/WAF1 gene in a Sp1-dependent mannerEndocr Relat Cancer200815254555718509005
- FuryMGSolitDBSuYBA phase I trial of intermittent high-dose gefitinib and fixed-dose docetaxel in patients with advanced solid tumorsCancer Chemother Pharmacol20075946747516896930
- CohenEEWRosenLSVokesEEAxitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: results from a phase II studyJ Clin Oncol2008264708471318541897
- Gupta-AbramsonVTroxelABNelloreAPhase II trial of sorafenib in advanced thyroid cancerJ Clin Oncol200826294714471918541894
- ChoKWangXNieSChenZGShinDMTherapeutic nanoparticles for drug delivery in cancerClin Cancer Res2008141310131618316549
- AtadjaPDevelopment of the pan-DAC inhibitor panobinostat (LBH589): successes and challengesCancer Lett2009280223324119344997
- GuleMKChenYSanoDTargeted therapy of VEGFR2 and EGFR significantly inhibits growth of anaplastic thyroid cancer in an orthotopic murine modelClin Cancer Res20111782281229121220477
- WunderlichARothSRamaswamyACombined inhibition of cellular pathways as a future therapeutic option in fatal anaplastic thyroid cancerEndocrine201242363764622477151
- SpallanzaniABertoliniFDepenniRTyrosine kinase inhibitors (TKIs) in advanced thyroid cancer: a single institution reportSupplementi di Tumori2012133S99
- RosoveMHPeddiPFGlaspyJABRAF V600E inhibition in anaplastic thyroid cancerN Engl J Med2013368768468523406047
- NehsMANuceraCNagarkattiSSLate intervention with anti-BRAF(V600E) therapy induces tumor regression in an orthotopic mouse model of human anaplastic thyroid cancerEndocrinology201215398599422202162
- BrownRFDucicYAggressive surgical resection of anaplastic thyroid carcinoma may provide long-term survival in selected patientsOtolaryngol Head Neck Surg2013148456457123396588
- SunXSSunSRGuevaraNChemoradiation in anaplastic thyroid carcinomasCrit Rev Oncol Hematol201286329030123218594
- DeshpandeHARomanSSosaJANew targeted therapies and other advances in the management of anaplastic thyroid cancerCurr Opin Oncol2013251444923159847
- PaciniFCastagnaMGBrilliLPentheroudakisGESMO Guidelines Working GroupThyroid Cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-upAnn Oncol201223Suppl 7vii110vii11922997443
- XingMBRAF mutation in thyroid cancerEndocr Relat Cancer200512224526215947100
- HouPLiuDShanYGenetic alterations and their relationship in the phosphatidylinositol 3-kinase/Akt pathway in thyroid cancerClin Cancer Res20071341161117017317825
- LiuZHouPJiMGuanHHighly prevalent genetic alterations in receptor tyrosine kinases and phosphatidylinositol 3-kinase/akt and mitogen-activated protein kinase pathways in anaplastic and follicular thyroid cancersJ Clin Endocrinol Metab20089383106311618492751
- CaroniaLMPhayJEShahMHRole of BRAF in thyroid oncogenesisClin Cancer Res201117247511751721900390
- Ricarte-FilhoJCRyderMChitaleDAMutational profile of advanced primary and metastatic radioactive iodine-refractory thyroid cancers reveals distinct pathogenetic roles for BRAF, PIK3CA, and AKT1Cancer Res200969114885489319487299
- NehsMANagarkattiSNuceraCHodinRAParangiSThyroidectomy with neoadjuvant PLX4720 extends survival and decreases tumor burden in an orthotopic mouse model of anaplastic thyroid cancerSurgery2010148611541162 discussion 1162.21134546
- SavvidesPNagaiahGLavertuPNPhase II Trial of Sorafenib in patients with advanced anaplastic carcinoma of the thyroidThyroid201323560060423113752
- BayerNexavar® versus placebo in locally advanced/metastatic RAI-refractory differentiated thyroid cancer Available from: http://www.clinicaltrials.gov/ct2/show/NCT00984282. NLM identifier: NCT00984282. Available form: www.clinicaltrials.gov/ct2/show/NCT00984282Accessed July 20, 2013
- PerriFLorenzoGDScarpatiGDBuonerbaCAnaplastic thyroid carcinoma: a comprehensive review of current and future therapeutic optionsWorld J Clin Oncol20112315015721611089
- SmallridgeRCAinKBAsaSLAmerican Thyroid Association Anaplastic Thyroid Cancer Guidelines TaskforceThyroid201211221111043923130564
- CooneyMMvan HeeckerenWBhaktaSOrtizJRemickSCDrug insight: vascular disrupting agents and angiogenesis – novel approaches for drug deliveryNat Clin Pract Oncol200631268269217139319
- HaHTLeeJSUrbaSA phase II study of imatinib in patients with advanced anaplastic thyroid cancerThyroid201020997598020718683
- JinNJiangTRosenDMNelkinBDBallDWDual inhibition of mitogen-activated protein kinase kinase and mammalian target of rapamycin in differentiated and anaplastic thyroid cancerJ Clin Endocrinol Metab200994104107411219723757
- CatalanoMGFortunatiNPuglieseMHistone deacetylase inhibition modulates E-cadherin expression and suppresses migration and invasion of anaplastic thyroid cancer cellsJ Clin Endocrinol Metab2012977E1150E115922563106
- PapewalisCWuttkeMSchinnerSRole of the novel mTOR inhibitor RAD001 (everolimus) in anaplastic thyroid cancerHorm Metab Res2009411075275619513966
- O’NeillJPShahaARAnaplastic thyroid cancerOral Oncol201349770270623583302
- ItoKHanamuraTMurayamaKMultimodality therapeutic outcomes in anaplastic thyroid carcinoma: improved survival in subgroups of patients with localized primary tumorsHead Neck201234223023721500309
- GranataRLocatiLLicitraLTherapeutic strategies in the management of patients with metastatic anaplastic thyroid cancer: review of the current literatureCurr Opin Oncol201325322422823493194
- SosaJAEliseiRJarzabBA randomized phase II/III trial of a tumor vascular disrupting agent fosbretabulin tromethamine (CA4P) with carboplatin (C) and paclitaxel (P) in anaplastic thyroid cancer (ATC): final survival analysis for the FACT trialJ Clin Oncol201129Suppl Abstr 5502. Available from: http://meetinglibrary.asco.org/content/78227-102Accessed July 20, 2013
- PierieJPMuzikanskyAGazRDFaquinWCOttMJThe effect of surgery and radiotherapy on outcome of anaplastic thyroid carcinomaAnn Surg Oncol2002Jan-Feb91576411833496
- KimSPrichardCNYounesMNCetuximab and Irinotecan interact synergistically to inhibit the growth of orthotopic anaplastic thyroid carcinoma xenografts in nude miceClin Cancer Res2006115122600716428506