Abstract
Pectus excavatum (PEx) is one of the most common congenital chest wall deformities. Depending on the severity, presentation of PEx may range from minor cosmetic issues to disabling cardiopulmonary symptoms. The effect of PEx on adult patients has not been extensively studied. Symptoms may not occur until the patient ages, and they may worsen over the years. More recent publications have implied that PEx may have significant cardiopulmonary implications and repair is of medical benefit. Adults presenting for PEx repair can undergo a successful repair with a minimally invasive “Nuss” approach. Resolution of symptoms, improved quality of life, and satisfying results are reported.
Background
Pectus excavatum (PEx) is the most common congenital chest wall anomaly.Citation1–Citation4 The deformity is reported to occur more frequently in males than females; however, diagnosis in females may often be missed if obscured with breast tissue.Citation5–Citation7 Depending on the severity, presentation of PEx may range from a minor cosmetic issue to disabling cardiopulmonary symptoms.Citation8–Citation10 The internally displaced sternum can cause right-side heart compression and restrictive deficits.Citation8,Citation9 As the patient advances in age, the chest wall can become less flexible as a result of increased calcium accumulation in cartilage attachments of the anterior chest wall.Citation11,Citation12 Symptoms may occur or show progression as the patient ages.Citation11–Citation13 Kragten et alCitation12 reported development of symptoms in the fourth and fifth decade in nearly half of their adult patients with significant improvement after surgical repair. The optimal surgical procedure for adult PEx patients has been controversial, and some surgeons recommend limiting the Nuss procedure to pediatrics and adolescents.Citation14,Citation15 We present a review of adult patients with PEx including outcomes after repair with Nuss (“Nuss”) or a minimally invasive repair of pectus excavatum (MIRPEx).
Cardiopulmonary outcomes
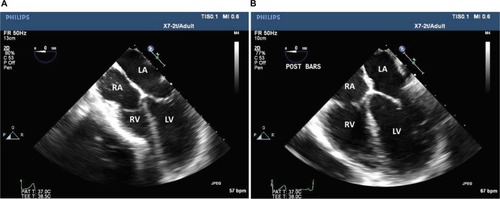
The cardiopulmonary effects of PEx have been debated for years, Citation16–Citation18 and there is a paucity of reports evaluating adult patients.Citation19,Citation20 The inward deformity of the anterior chest wall has a negative cardiopulmonary consequence on patients with PEx, as supported by the most recent data.Citation9,Citation21 This can cause displacement of the heart into the left chest and varying degrees of heart compression (). Decrease in atrial filling and venous return can result in diastolic dysfunction and reduction in cardiac output with significant compression to the chambers of the right heart.Citation9,Citation20–Citation22 Mocchegiani et alCitation23 reported that the right ventricular outflow tract in PEx patients was significantly narrower and right ventricle (RV) end-diastolic and-systolic areas were significantly smaller. Surgical correction of the PEx has been shown to relieve compression, allowing for a significant increase in right heart chamber size, increased flow velocities, and improved cardiac outputCitation9,Citation21,Citation24 (). Krueger et alCitation25 also noted significant improvement in post-repair cardiac outputs that increased to 66.2% vs 58.4% and the end-diastolic RV volume that increased to a mean of 40.8 mL vs 21.7 mL preoperatively. There may be a greater impact on cardiac function and symptoms in patients over 30 years of age.Citation12,Citation24 In post-repair PEx patients ≥30 years, a mean increase in right ventricular output of 65% was documented by intraoperative transesophageal echocardiogram.Citation24 Neviere et alCitation26 found that PEx deformity was associated with reduction in the strength of the inspiratory muscle as evident by reduction in the maximal static respiratory pressure (PImax) and sniff nasal inspiratory pressure (SNIP) with significant increase of these values postoperatively which was reflected in enhanced efficacy of the respiratory pump and the cardiovascular function improvement.
Figure 1 Computerized tomographic scan of a patient with severe pectus excavatum and Haller index of 24.6. Sternal deformity with compression of the right heart and inflow are seen (arrow).

Figure 2 Transesophageal echocardiographic images show preoperative effect (A) of pectus excavatum with compression on the right ventricle due to the inward sternal deformity and relief of the compression following surgical repair (B).
Long-term follow-up of corrected PEx patients and correlations between physiologic impact and symptoms are lacking.Citation8,Citation27–Citation30 reviews some of the major publications reporting cardiopulmonary impairments and postsurgical results. Only six of these represented a mean age of 18 years and older.Citation9,Citation19,Citation25,Citation26,Citation31,Citation32 Cardiopulmonary exercise testing has been used to assess exercise capacity and limitations in peak oxygen uptake and O2 pulse which can result as a consequence of the pectus deformity.Citation18,Citation19,Citation33,Citation34 Publications as to the benefits of surgical correction have varied.Citation8,Citation19,Citation31,Citation35 Several studies have reported that the cardiopulmonary function has improved significantly with increase in the oxygen consumption (VO2) and O2 pulse after surgical repair of PEx.Citation8,Citation19 Maagaard et alCitation35 previously reported normalization of the decreased cardiopulmonary function in teenagers with PEx at 3 years following surgical repair; however, in a more recent evaluation of adult patients by Udholm et alCitation31 (≥21 years), a significant improvement in the maximum oxygen consumption (VO2 max) was not seen 1 year after PEx repair. These results did show a trend of increased improvement in the VO2 max which could be more evident with a longer period of follow-up. Adult patients may also differ in their ability to return to normal after PEx repair. During assessment, the patient’s baseline exercise history must be considered. Cardiac output and deconditioning can occur with postoperative inactivity;Citation36 therefore, the patient’s exercise history can affect the measurements of VO2 and may cause more impact on short-term testing results.Citation34
Table 1 Review of major publications reporting cardiopulmonary outcomes and postsurgical results
Quality of life and patient satisfaction
Both the exercise limitations and the cosmetic disfigurement with PEx may cause a decrease in quality of life and alteration of social behavior.Citation37,Citation40–Citation44 There has been a greater recognition of the physiologic and psychologic impact of these patients.Citation45 Lack of self-confidence, poor body image, avoidance of social activities, and emotional difficulties are noted in PEx patients. Feelings of anxiety, depression, sadness, and frustration are also reported.Citation40 The importance of corrective surgery for improvement in psychological distress, quality of life, and exercise tolerance has been documented in the literature.Citation37,Citation41–Citation44 The majority of these studies report a mixed population of children and adolescents with few adults; therefore, it is difficult to make broad-based assumptions as to their application to the adult population.Citation46–Citation50 reviews some of the major publicationsCitation44,Citation48–Citation50,Citation53,Citation54 reporting postsurgical quality of life and symptom outcomes.
Table 2 Review of major publications from 2006–2016 reporting quality of life and patient satisfaction after pectus excavatum repair
Kelly et alCitation10 reported on 264 child patients and 291 parents from multiple centers using a validated Pectus Excavatum Evaluation Questionnaire. Children noted a dramatic improvement in the body image and physical difficulties after surgery. Parents also noticed an improvement in the child’s emotional, physical difficulties and social self- consciousness.Citation10 Patient’s satisfaction with the chest appearance was found to be very good, with excellent to good results reported in over 95% of patients at the time of bar removal.Citation51
In a 2016 study performed by Lomholt et al,Citation49 107 patients and 106 parents completed the generic health-related quality-of-life measure. The Child Health Questionnaire was assessed preoperatively and at 3, 6 months following PEx repair. A control group of 183 school children completed the same measure on one occasion. In the postoperative study, patients and parents reported improved emotional well-being and self-esteem. Additionally, patients at both 3 and 6 months postoperatively reported increased physical and social activities.
There are very few major publications that documented symptoms and quality-of-life improvement after Nuss repair in adult patients. Kragten et alCitation12 reported on symptomatic seniors with PEx. He found that in 45% of the patients with “serious and sometimes invalidating complaints”, symptoms did not start until the fourth or fifth decade of life and were often labeled as “unexplained cardiovascular complaints”. All patients that underwent surgery were repaired by the open Ravitch procedure and reported substantial or complete resolution of the symptoms postoperatively. Tikka et alCitation52 used the Brompton’s single-step questionnaire (SSQ) to assess the postoperative patient satisfaction and confirmed that Nuss operation had positively impacted the psychological and physical status of their patients along with overall quality-of-life improvement. They reported that their pectus patient information website improved, additionally, their patient’s satisfaction and recovery after surgery.
Krasopoulos et alCitation43 proposed the two-step Nuss Questionnaire modified for Adults (NQ-mA) and a SSQ. These questionnaires measured the disease-specific quality-of-life changes after surgery and assessed the effect of surgery on the physical and psychological well-being of postoperative patients. They noted that patients’ self-esteem, social functioning, and level of satisfaction were significantly improved following Nuss procedure. Their questionnaire also included the impact of surgical wounds/scars on the overall cosmetic result, consciousness of the presence of metallic bar, the decision to have the operation again, and questions about postoperative pain which may have limited the patient satisfaction after surgery. It was evident from the study that most of the patients were very satisfied with their scars and almost all of them were conscious of the presence of bar, but none of them considered that to be a major inconvenience. Pain was also noted as a concern in the immediate postoperative period; however, it decreased significantly after several weeks. By 4–5 months after surgery, no patient was still requiring analgesics.
Other surgeons have subsequently utilized this modified survey for assessing the patients postoperatively.Citation48,Citation50,Citation53 Hoksch et alCitation50 performed a prospective study to evaluate the long-term results of Nuss in adults using NQ-mA and SSQ in a shorter and modified format. Initially, a large adult cohort (n = 129) was included, but only19 patients were observed for >10 years after surgery. This has been the only study reporting outcomes for an adult population for more than 10 years after surgery. The results obtained initially after surgery were in the follow-up period of 3, 12 and 36 months showed high levels of satisfaction respectively reported at 97.6%, 97.2%, and 95.7%. Better or much better quality of life was reported at 3, 12, and 36 months in 88%, 89%, and increased to 92.5%, respectively, in the follow-up period. Even after observation for >10 years, continued improvement in quality of life was confirmed in 57.9% of patients. Surgical recommendation for Nuss was given by nearly 95% of patients. Mild pain occurring during specific bodily movements was reported in 31.6%, and 63.2% of patients had no pain.
Sacco Casamassima et alCitation53 in 2016 reported long-term results of adults using modified SSQ. Satisfaction with the chest wall appearance was reported in 89% out of 43.8% of responders. Improvement in social interaction was reported by 84% of responders. About 94% of patients obtained overall satisfaction with the results post-bar removal. They also highlighted that the dissatisfaction observed by some patients was due to severe postoperative chest pain (that necessitates more aggressive analgesic regimen) and surgical scars. Willingness to have the operation again was reported by 79% of responders. Generalized conclusions cannot be drawn from this study as it is limited by small sample size. There is a compelling need for a large number of similar studies commenting on the long-term results in adults to identify the benefits of surgery in this group.
Hanna et alCitation41 studied the midterm results in young adults who underwent Nuss repair and used the single-step quality-of-life survey for evaluation. With a 73% response rate, they noticed an improvement in both self-esteem and social life. Satisfaction with the cosmetic result was achieved in 80% and recommendation for the surgery was given by 96% of their patients. About 92% reported subjective improvement in the chest wall appearance. As stated by other authors, in-hospital pain despite aggressive analgesic usage was a major concern in the immediate postoperative period; however, in the follow-up it was significantly decreased, with almost all patients reporting minimal or no pain.
Most of the data available suggest that patients who had undergone Nuss showed an overall satisfaction with the cosmetic result, had a significant improvement in self-image, and felt that the surgery had a positive impact on their ability to exercise and well-being.
Surgical approaches and outcomes
The Nuss procedure or “MIRPEx” has become the standard of care for PEx repair in children and adolescents.Citation64 There is an ongoing discussion in the literature regarding the success of this surgery in adults with PEx. Initial reports of Nuss procedure in adults were criticized due to higher complication rates vs the open Ravitch technique with most being related to bar migration, postoperative pain, and recurrences. Citation65–Citation67 The recommendations of some surgeons were to limit the procedure to pediatrics and adolescents; however, their publications have been replaced with numerous series of successful repairs using a modified MIRPEx approach.Citation24,Citation68,Citation69 reviews publications reporting on 70 or more adults repaired using an MIRPEx procedure since 2008. The majority of authors considered patients aged 18 years and older as adults. Citation28,Citation51,Citation57,Citation63,Citation70,Citation71 Several papers have stratified their results to differentiate younger vs older patients.Citation24,Citation30 There is evidence that older patients are more difficult to treat and the risk of complications may be greater.Citation14 Despite this, excellent results are achieved with an MIRPEx approach even in older adult pat ientsCitation15,Citation24,Citation28–Citation30,Citation43,Citation63,Citation68,Citation69,Citation71–Citation73 ().
Figure 3 Clinical photographs of a 22-year-old man with severe pectus excavatum are shown before surgery (A, B) and after (C) minimally invasive repair of pectus excavatum, with placement of three Nuss bars as shown in the chest roentgenogram (D).
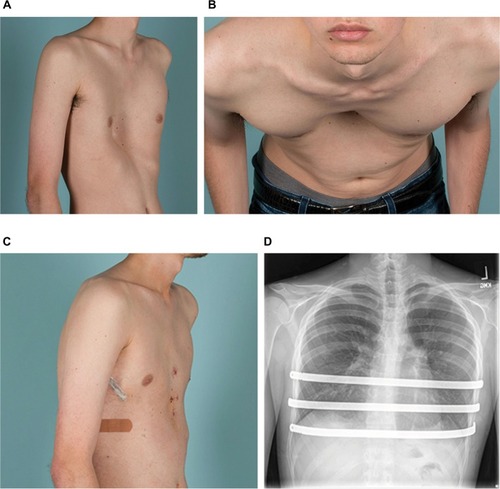
Table 3 Review of some of the recent studies and reported results from 2008–2016 after Nuss procedure for pectus excavatum repair in adults
Since the introduction of the original Nuss technique for children in 1998,Citation64 several changes have been made in the surgical technique and methods of bar stabilization which have improved the success of the procedure in adult patients.Citation24,Citation28,Citation72,Citation74–Citation78 Important modifications include the use of forced sternal elevation,Citation78 multiple support bars,Citation24,Citation77 and improved fixation methods to secure the bars and prevent rotation.Citation24,Citation28,Citation72,Citation74–Citation78 These technical refinements enabled successful MIRPEx repair of older patients and are reviewed in .
Table 4 Review of several technical modifications reported for minimally invasive repair of pectus excavatum in adults
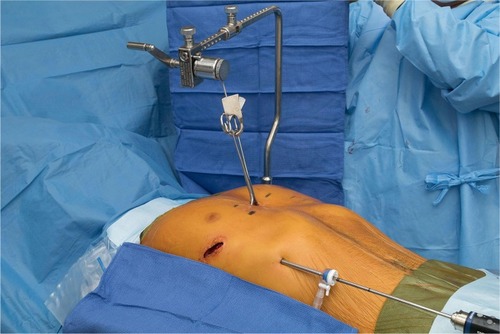
The use of forced sternal elevation may help reduce the force required to insert and rotate bars (). This may lessen, but not eliminate, lateral stripping of the intercostal muscles of the more rigid chest wall.Citation69,Citation78,Citation79,Citation81,Citation82,Citation84 Several techniques have been proposed for the forceful elevation of sternum. Park et alCitation79 reported his Crane technique and discussed the benefits of its use in adult patients with heavier chests and severely asymmetric deformities including prevention of intercostal muscle tear and bar displacement. Similar variations of this technique have been reported by others with similar beneficial results.Citation69,Citation78,Citation81,Citation82,Citation84 A more simplified aspect of handheld retractors can also be utilized, depending on the severity and rigidity of the defect.Citation80,Citation83
Figure 4 The Rultract retractor can be utilized to forcefully elevate the sternum when attached by a bone clamp.
Multiple bars may balance the increased pressure of the chest wall and in older patients, the use of two or more bars is frequently reported.Citation24,Citation70,Citation77,Citation90 The risk of bar rotation and malposition may also be decreased by distributing the pressure of a more rigid chest wall.Citation70,Citation77,Citation90 PilegaardCitation68 reported that 70% of his patients over 30 years of age required two or more bars. In our own practice, two or more bars were utilized in 99% of patients over age 18 years,Citation24 with 40% of patients over 30 years receiving three bars to achieve complete repair. Others have reported decreased risk of bar migration and the need of reoperation when multiple bars were utilized.Citation70,Citation77,Citation90 In a study of PEx repair in 44 late adolescent and adult patients, 11.5% of those with single-bar repairs required reoperation for incomplete correction or bar rotation compared with 0% who had a double-bar repair. Double bar also decreases the postoperative pain as described by Nagaso et al.Citation89 The risk of bar rotation may be lowered by the use of shorter bars as reported by several surgeons.Citation93,Citation94 In a publication reporting Nuss revision after procedure failure, too long bars were noted to be a factor related to failure.Citation95
The biggest challenge in adult patients continues to be bar fixation. A higher rate of bar displacement is reported in older patients.Citation14,Citation24 There are multiple successful ways reported for securing of bars. Medial fixation with a hinge reinforcement plate,Citation85 medially placed stabilizers,Citation75 multipoint fixation,Citation24,Citation69,Citation77 and the Bridge technique, which was more recently published,Citation61 have all been successful methods for bar fixation in adult patients.Citation72,Citation79,Citation87,Citation96
Chondroplasty or open osteotomy may still be necessary to achieve adequate repair in some adult patients. Patients with complex combined deformities, extensively calcified chest walls, and significant asymmetry may require an open repair for optimal correction. The requirement for osteotomy or cartilage resection is more commonly reported in older patients.Citation24,Citation91,Citation97,Citation98 In our experience, over 88% of the patients ≥30 years were successfully repaired with MIRPEx; however, some required an osteotomy or open resection for fracture. Postoperative pain may also be reduced by scoring of deformed cartilages as illustrated by Nagasao et al.Citation92 The use of a hybrid procedure may also be considered and is our procedure of choice for these more difficult deformities.Citation24 Both surgical principles are utilized by incorporating osteotomy cuts and external fixation as well as pectus support bars. Achieving adequate postoperative pain control remains a concern for adults undergoing Nuss.Citation99 Various analgesic regimens have been discussed by several authors.Citation100 Perioperative pain can be well managed by current techniques.Citation101 These include the use of thoracic epidurals, intravenous on-demand patient-administrated narcotics, local paravertebral blocks, and subcutaneous continuous flow catheters.Citation102–Citation106 We have had excellent results using a protocol including gabapentin, ibuprofen, acetaminophen, and narcotics along with subcutaneous continuous flow catheters for postoperative pain control.Citation24,Citation102,Citation107 Adjuvant medications for postoperative pain management have included the use of ketorolac, diazepam, and gabapentin.Citation103–Citation106 Intraoperative use of methadone can also be advantageous.Citation24,Citation102
Discussion
The extension of the Nuss procedure to repair adults with PEx has been controversial in the past.Citation14,Citation65–Citation67 There are now multiple publications that report successful repair of adults even beyond 50 years of age.Citation9,Citation12,Citation24,Citation55 The difficulty of repair and risk of complications do, however, increase with age.Citation14,Citation24,Citation53 Adequate surgical experience with the Nuss procedure in younger patients that are easier to repair is critical prior to attempting the more difficult adult deformity. Bar rotation and migration can be a significant issue and techniques to minimize intercostal stripping, such as reinforcement of intercostal spacesCitation24,Citation59,Citation87 and medially placed stabilizers, may be of benefit in reducing the risks.Citation75 The use of forced sternal elevation can also decrease the forces required for bar insertion and positioning.Citation69,Citation78–Citation84 The adult chest wall has additional complexities due to the decrease in flexibility and increase in weight. Multiple bars have been noted to decrease the weight supported by an individual bar and decrease the risk of rotation.Citation24,Citation70,Citation88–Citation90 Adequate stabilization of bars is also critical due to these factors, and medial and/or multipoint fixation has been shown to reduce bar displacement.Citation24,Citation28,Citation51,Citation59,Citation61,Citation69,Citation75,Citation86,Citation87 We did not intend this publication to be an intensive review of surgical techniques in adult patients, and the majority of information presented was based on a larger case series which reported on primary Nuss repair in the adult population. Extension of the Nuss procedure to more complex repairs, such as patients with prior sternotomy or cardiac surgery, is beyond the scope of this paper and can be associated with catastrophic complications.Citation55,Citation108
Conclusion
MIRPEx can be extended to repair the majority of older adult patients. Although adults undergoing Nuss procedure may have a higher rate of complications, continuous technical refinements have significantly reduced the complication rates and contributed to the success of the procedure. As there is increased difficulty in performing this procedure in adult patients, the experience and expertise of surgeons at specialized centers is critical for successful outcomes. There is enough evidence to validate repair of adults with PEx. Published data support the benefits of repair with good outcomes and improvement of symptoms.
Disclosure
The authors report no conflicts of interest in this work.
References
- FokinAASteuerwaldNMAhrensWAAllenKEAnatomical, histologic, and genetic characteristics of congenital chest wall deformitiesSemin Thorac Cardiovasc Surg2009211445719632563
- SchererLRArnPHDresselDAPyeritzRMHallerJAJrSurgical management of children and young adults with Marfan syndrome and pectus excavatumJ Pediatr Surg19882312116911723236181
- CobbenJMOostraRJvan DijkFSPectus excavatum and carinatumEur J Med Genet201457841441724821303
- ChungCSMyrianthopoulosNCFactors affecting risks of congenital malformations. I. Analysis of epidemiologic factors in congenital malformations. Report from the Collaborative Perinatal ProjectBirth Defects Orig Artic Ser19751110122
- FonkalsrudEWManagement of pectus chest deformities in female patientsAm J Surg2004187219219714769303
- MaITRebeccaAMNotricaDMMcMahonLEJaroszewskiDEPectus excavatum in adult women: repair and the impact of prior or concurrent breast augmentationPlast Reconstr Surg20151352303e312e
- ParkHJGuJHJangJCDhongESYoonESCorrection of pectus excavatum with breast hypoplasia using simultaneous pectus bar procedure and augmentation mammoplastyAnn Plast Surg201473219019523486122
- SigaletDLMontgomeryMHarderJWongVKravarusicDAlassiriALong term cardiopulmonary effects of closed repair of pectus excavatumPediatr Surg Int200723549349717252283
- ChaoCJJaroszewskiDEKumarPNSurgical repair of pectus excavatum relieves right heart chamber compression and improves cardiac output in adult patients – an intraoperative transesophageal echocardiographic studyAm J Surg201521061118112426499055
- KellyREJrCashTFShambergerRCSurgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter studyPediatrics200812261218122219047237
- JaroszewskiDEFonkalsrudEWRepair of pectus chest deformities in 320 adult patients: 21 year experienceAnn Thorac Surg200784242943317643611
- KragtenHASiebengaJHoppenerPFVerburgRViskerNSymptomatic pectus excavatum in seniors (SPES): a cardiovascular problem?: a prospective cardiological study of 42 senior patients with a symptomatic pectus excavatumNeth Heart J2011192737822020944
- JaroszewskiDSteidleyEGalindoAArabiaFTreating heart failure and dyspnea in a 78-year-old man with surgical correction of pectus excavatumAnn Thorac Surg20098831008101019699946
- Kim doHHwangJJLeeMKLeeDYPaikHCAnalysis of the Nuss procedure for pectus excavatum in different age groupsAnn Thorac Surg20058031073107716122489
- EstevesEPaivaKCCalcagno-SilvaMChagasCCBarbosa-FilhoHTreatment of pectus excavatum in patients over 20 years of ageJ Laparoendosc Adv Surg Tech A2011211939621214363
- KaguraokaHOhnukiTItaokaTKeiJYokoyamaMNittaSDegree of severity of pectus excavatum and pulmonary function in preoperative and postoperative periodsJ Thorac Cardiovasc Surg19921045148314881434732
- MorshuisWJFolgeringHTBarentszJOCoxALvan LierHJLacquetLKExercise cardiorespiratory function before and one year after operation for pectus excavatumJ Thorac Cardiovasc Surg19941076140314098196380
- HallerJAJrLoughlinGMCardiorespiratory function is significantly improved following corrective surgery for severe pectus excavatum. Proposed treatment guidelinesJ Cardiovasc Surg (Torino)2000411125130
- NeviereRMontaigneDBenhamedLCardiopulmonary response following surgical repair of pectus excavatum in adult patientsEur J Cardiothorac Surg2011402e77e8221570313
- MalekMHFonkalsrudEWCooperCBVentilatory and cardiovascular responses to exercise in patients with pectus excavatumChest2003124387088212970011
- GurkanUAydemirBAksoySEchocardiographic assessment of right ventricular function before and after surgery in patients with pectus excavatum and right ventricular compressionThorac Cardiovasc Surg201462323123523619591
- ColnECarrascoJColnDDemonstrating relief of cardiac compression with the Nuss minimally invasive repair for pectus excavatumJ Pediatr Surg2006414683686 discussion 683–68616567176
- MocchegianiRBadanoLLestuzziCNicolosiGLZanuttiniDRelation of right ventricular morphology and function in pectus excavatum to the severity of the chest wall deformityAm J Cardiol199576129419467484836
- JaroszewskiDEEwaisMMChaoCJSuccess of minimally invasive pectus excavatum procedures (modified Nuss) in adult patients (±=30 years)Ann Thorac Surg20161023993100327283111
- KruegerTChassotPGChristodoulouMChengCRisHBMagnussonLCardiac function assessed by transesophageal echocardiography during pectus excavatum repairAnn Thorac Surg201089124024320103244
- NeviereRBenhamedLDuva PentiahAWurtzAPectus excavatum repair improves respiratory pump efficacy and cardiovascular function at exerciseJ Thorac Cardiovasc Surg2013145260560622929222
- KellyREJrMellinsRBShambergerRCMulticenter study of pectus excavatum, final report: complications, static/exercise pulmonary function, and anatomic outcomesJ Am Coll Surg201321761080108924246622
- HebraAJacobsJPFelizAArenasJMooreCBLarsonSMinimally invasive repair of pectus excavatum in adult patientsAm Surg200672983784216986397
- AronsonDCBosgraafRPvan der HorstCEkkelkampSNuss procedure: pediatric surgical solution for adults with pectus excavatumWorld J Surg20073112629 discussion 3017180569
- ChengYLLeeSCHuangTWWuCTEfficacy and safety of modified bilateral thoracoscopy-assisted Nuss procedure in adult patients with pectus excavatumEur J Cardiothorac Surg20083451057106118774724
- UdholmSMaagaardMPilegaardHHjortdalVCardiac function in adults following minimally invasive repair of pectus excavatumInteract Cardiovasc Thorac Surg201622552552926860899
- TopperAPolleichtnerSZagrosekAImpact of surgical correction of pectus excavatum on cardiac function: insights on the right ventricle. A cardiovascular magnetic resonance studydaggerInteract Cardiovasc Thorac Surg2016221384626487434
- AlbouainiKEgredMAlahmarAWrightDJCardiopulmonary exercise testing and its applicationHeart200793101285129217890705
- MalekMHCoburnJWStrategies for cardiopulmonary exercise testing of pectus excavatum patientsClinics (Sao Paulo)200863224525418438580
- MaagaardMTangMRinggaardSNormalized cardiopulmonary exercise function in patients with pectus excavatum three years after operationAnn Thorac Surg201396127227823684487
- PerhonenMAFrancoFLaneLDCardiac atrophy after bed rest and spaceflightJ Appl Physiol 1985200191264565311457776
- O’KeefeJByrneRMontgomeryMHarderJRobertsDSigaletDLLonger term effects of closed repair of pectus excavatum on cardiopulmonary statusJ Pediatr Surg20134851049105423701781
- TangMNielsenHHLesboMImproved cardiopulmonary exercise function after modified Nuss operation for pectus excavatumEur J Cardiothorac Surg20124151063106722219453
- BawazirOAMontgomeryMHarderJSigaletDLMidterm evaluation of cardiopulmonary effects of closed repair for pectus excavatumJ Pediatr Surg200540586386715937832
- JaroszewskiDNotricaDMcMahonLSteidleyDEDeschampsCCurrent management of pectus excavatum: a review and update of therapy and treatment recommendationsJ Am Board Fam Med201023223023920207934
- HannaWCKoMABlitzMShargallYCompeauCGThoracoscopic Nuss procedure for young adults with pectus excavatum: excellent midterm results and patient satisfactionAnn Thorac Surg201396310331036 discussion 1037–103823810179
- JacobsenEBThastumMJeppesenJHPilegaardHKHealth-related quality of life in children and adolescents undergoing surgery for pectus excavatumEur J Pediatr Surg2010202859120112187
- KrasopoulosGDusmetMLadasGGoldstrawPNuss procedure improves the quality of life in young male adults with pectus excavatum deformityEur J Cardiothorac Surg20062911516337131
- KuruPBostanciKErmerakNOBahadirATAfacanCYukselMQuality of life improves after minimally invasive repair of pectus excavatumAsian Cardiovasc Thorac Ann201523330230725293414
- SteinmannCKrilleSMuellerAWeberPReingruberBMartinAPectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: a control group comparison of psychological characteristics prior to surgical correctionEur J Cardiothorac Surg20114051138114521440452
- KellyREJrPectus excavatum: historical background, clinical picture, preoperative evaluation and criteria for operationSemin Pediatr Surg200817318119318582824
- KrasopoulosGGoldstrawPMinimally invasive repair of pectus excavatum deformityEur J Cardiothorac Surg201139214915820739187
- MetzelderMLKueblerJFLeonhardtJUreBMPetersenCSelf and parental assessment after minimally invasive repair of pectus excavatum: lasting satisfaction after bar removalAnn Thorac Surg20078351844184917462410
- LomholtJJJacobsenEBThastumMPilegaardHA prospective study on quality of life in youths after pectus excavatum correctionAnn Cardiothorac Surg20165545646527747179
- HokschBKocherGVollmarPPrazFSchmidRANuss procedure for pectus excavatum in adults: long-term results in a prospective observational studyEur J Cardiothorac Surg201650593493927126132
- KellyREGoretskyMJObermeyerRTwenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patientsAnn Surg201025261072108121107118
- TikkaTKalkatMSBishayESteynRSRajeshPBNaiduBA 20-year review of pectus surgery: an analysis of factors predictive of recurrence and outcomesInteract Cardiovasc Thorac Surg201623690891327521175
- Sacco CasamassimaMGGauseCGoldsteinSDPatient satisfaction after minimally invasive repair of pectus excavatum in adults: long-term results of Nuss procedure in adultsAnn Thorac Surg201610141338134526794892
- TikkaTWebbJAgostiniPPectus patient information website has improved access to care and patient reported outcomesJ Cardiothorac Surg20161116927114076
- PilegaardHKSingle centre experience on short bar technique for pectus excavatumAnn Cardiothorac Surg20165545045527747178
- PawlakKGasiorowskiLGabryelPGaleckiBZielinskiPDyszkiewiczWEarly and late results of the Nuss procedure in surgical treatment of pectus excavatum in different age groupsAnn Thorac Surg201610251711171627373189
- ErsenEDemirkayaAKilicBMinimally invasive repair of pectus excavatum (MIRPE) in adults: is it a proper choice?Wideochir Inne Tech Maloinwazyjne20161129810427458490
- FiblaJJMolinsLMoradiellosJExperience with the Nuss technique for the treatment of pectus excavatum in Spanish thoracic surgery departmentsCir Esp2016941384326546550
- ParkHJKimKSLeeSJeonHWA next-generation pectus excavatum repair technique: new devices make a differenceAnn Thorac Surg201599245546125488621
- ZhangDKTangJMBenXSSurgical correction of 639 pectus excavatum cases via the Nuss procedureJ Thorac Dis2015791595160526543607
- ParkHJKimKSMoonYKLeeSThe bridge technique for pectus bar fixation: a method to make the bar un-rotatableJ Pediatr Surg20155081320132225783318
- RokitanskyAMStanekRModified minimally invasive pectus repair in children, adolescents and adults: an analysis of 262 patientsPneumologia201362422423124734356
- OlbrechtVAArnoldMANabaweesiRLorenz bar repair of pectus excavatum in the adult population: should it be done?Ann Thorac Surg2008862402408 discussion 408–40918640305
- NussDKellyREJrCroitoruDPKatzMEA 10-year review of a minimally invasive technique for the correction of pectus excavatumJ Pediatr Surg19983345455529574749
- JohnsonWRFedorDSinghalSSystematic review of surgical treatment techniques for adult and pediatric patients with pectus excavatumJ Cardiothorac Surg201492524506826
- HebraASwovelandBEgbertMOutcome analysis of minimally invasive repair of pectus excavatum: review of 251 casesJ Pediatr Surg2000352252257 discussion 257–25810693675
- KanagaratnamAPhanSTchantchaleishviliVPhanKRavitch versus Nuss procedure for pectus excavatum: systematic review and meta-analysisAnn Cardiothorac Surg20165540942127747174
- PilegaardHKExtending the use of Nuss procedure in patients older than 30 yearsEur J Cardiothorac Surg201140233433721232968
- YoonYSKimHKChoiYSKimKShimYMKimJA modified Nuss procedure for late adolescent and adult pectus excavatumWorld J Surg20103471475148020221599
- PilegaardHKLichtPBRoutine use of minimally invasive surgery for pectus excavatum in adultsAnn Thorac Surg200886395295618721589
- SchalamonJPokallSWindhaberJHoellwarthMEMinimally invasive correction of pectus excavatum in adult patientsJ Thorac Cardiovasc Surg2006132352452916935105
- ParkHJJeongJYJoWMMinimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approachJ Thorac Cardiovasc Surg2010139237938620106400
- MansourKAThouraniVHOdesseyEADurhamMMMillerJIJrMillerDLThirty-year experience with repair of pectus deformities in adultsAnn Thorac Surg2003762391395 discussion 39512902071
- McMahonLEJohnsonKNJaroszewskiDEExperience with FiberWire for pectus bar attachmentJ Pediatr Surg20144981259126325092086
- PilegaardHKNuss technique in pectus excavatum: a mono-institutional experienceJ Thorac Dis20157Suppl 2S172S17625984364
- MolikKAEngumSARescorlaFJWestKWSchererLRGrosfeldJLPectus excavatum repair: experience with standard and minimal invasive techniquesJ Pediatr Surg200136232432811172426
- ParkHJLeeSYLeeCSYoumWLeeKRThe Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patientsAnn Thorac Surg200477128929514726081
- JaroszewskiDEJohnsonKMcMahonLNotricaDSternal elevation before passing bars: a technique for improving visualization and facilitating minimally invasive pectus excavatum repair in adult patientsJ Thorac Cardiovasc Surg201414731093109524237886
- ParkHJChungWJLeeISKimKTMechanism of bar displacement and corresponding bar fixation techniques in minimally invasive repair of pectus excavatumJ Pediatr Surg2008431747818206459
- TeddeMLde CamposJRWihlmJMJateneFBThe Nuss procedure made safer: an effective and simple sternal elevation manoeuvreEur J Cardiothorac Surg201242589089122833539
- TakagiSOyamaTTomokazuNKinoshitaKMakinoTOhjimiHA new sternum elevator reduces severe complications during minimally invasive repair of the pectus excavatumPediatr Surg Int201228662362622526549
- HaeckerFMSesiaSBIntraoperative use of the vacuum bell for elevating the sternum during the Nuss procedureJ Laparoendosc Adv Surg Tech A201222993493623137116
- JohnsonWRFedorDSinghalSA novel approach to eliminate cardiac perforation in the nuss procedureAnn Thorac Surg20139531109111123438552
- KimDIdowuOPalmerBKimSAnterior chest wall elevation using a T-fastener suture technique during a nuss procedureAnn Thorac Surg201498273473625087810
- ParkHJJeongJYKimKTChoiYHHinge reinforcement plate for adult pectus excavatum repair: a novel tool for the prevention of intercostal muscle stripInteract Cardiovasc Thorac Surg201112568769121343158
- Del FrariBSchwabeggerAHHow to avoid pectus bar dislocation in the MIRPE or MOVARPE technique: results of 12 years’ experienceAnn Plast Surg2014721757923241769
- NussDObermeyerRJKellyRENuss bar procedure: past, present and futureAnn Cardiothorac Surg20165542243327747175
- NussDMinimally invasive surgical repair of pectus excavatumSemin Pediatr Surg200817320921718582827
- NagasoTMiyamotoJKokajiKDouble-bar application decreases postoperative pain after the Nuss procedureJ Thorac Cardiovasc Surg20101401394444.e1220363484
- StanfillABDiSommaNHenriquesSMWallaceLJVeguntaRKPearlRHNuss procedure: decrease in bar movement requiring reoperation with primary placement of two barsJ Laparoendosc Adv Surg Tech A201222441241522577811
- DzielickiJKorlackiWJanickaIDzielickaEDifficulties and limitations in minimally invasive repair of pectus excavatum – 6 years experiences with Nuss techniqueEur J Cardiothorac Surg200630580180416982197
- NagasaoTHamamotoYTamaiMScoring of deformed costal cartilages reduces postoperative pain after Nuss procedure for pectus excavatumThorac Cardiovasc Surg2016641626926166292
- PilegaardHKShort Nuss bar procedureAnn Cardiothorac Surg20165551351827747185
- GhionzoliMCiutiGRicottiLIs a shorter bar an effective solution to avoid bar dislocation in a Nuss procedure?Ann Thorac Surg20149731022102724480262
- CroitoruDPKellyREJrGoretskyMJGustinTKeeverRNussDThe minimally invasive Nuss technique for recurrent or failed pectus excavatum repair in 50 patientsJ Pediatr Surg2005401181186 discussion 186–18715868582
- FallonSCSlaterBJNuchternJGComplications related to the Nuss procedure: minimizing risk with operative techniqueJ Pediatr Surg20134851044104823701780
- Al-AssiriAKravarusicDWongVDickenBMilbrandtKSigaletDLOperative innovation to the “Nuss” procedure for pectus excavatum: operative and functional effectsJ Pediatr Surg200944588889219433163
- RavenniGActis DatoGMZingarelliEFloccoRCasabonaRNuss procedure in adult pectus excavatum: a simple artifice to reduce sternal tensionInteract Cardiovasc Thorac Surg2013171232523575757
- PapicJCFinnellSMHowensteinAMBrecklerFLeysCMPostoperative opioid analgesic use after Nuss versus Ravitch pectus excavatum repairJ Pediatr Surg2014496919923 discussion 92324888835
- MuhlyWTMaxwellLGCraveroJPPain management following the Nuss procedure: a survey of practice and reviewActa Anaesthesiol Scand20145891134113925087774
- KellyREJrShambergerRCMellinsRBProspective multicenter study of surgical correction of pectus excavatum: design, perioperative complications, pain, and baseline pulmonary function facilitated by internet-based data collectionJ Am Coll Surg2007205220521617660066
- JaroszewskiDETemkitMEwaisMMRandomized trial of epidural vs. subcutaneous catheters for managing pain after modified Nuss in adultsJ Thorac Dis2016882102211027621865
- GebhardtRMehranRJSolizJCataJPSmallwoodAKFeeleyTWEpidural versus ON-Q local anesthetic-infiltrating catheter for post-thoracotomy pain controlJ Cardiothorac Vasc Anesth201327342342623672860
- RiedMSchillingCPotzgerTProspective, comparative study of the On-Q(R) PainBuster(R) postoperative pain relief system and thoracic epidural analgesia after thoracic surgeryJ Cardiothorac Vasc Anesth2014284985990
- WeberTMatzlJRokitanskyAKlimschaWNeumannKDeuschESuperior postoperative pain relief with thoracic epidural analgesia versus intravenous patient-controlled analgesia after minimally invasive pectus excavatum repairJ Thorac Cardiovasc Surg2007134486587017903498
- FutagawaKSuwaIOkudaTAnesthetic management for the minimally invasive Nuss procedure in 21 patients with pectus excavatumJ Anesth2006201485016421678
- Hall BurtonDMBoretskyKRA comparison of paravertebral nerve block catheters and thoracic epidural catheters for postoperative analgesia following the Nuss procedure for pectus excavatum repairPaediatr Anaesth201424551652024612096
- JaroszewskiDEGustinPJHaeckerF-MPectus excavatum repair after sternotomy: the Chest Wall International Group experience with substernal Nuss barsEuropean Journal of Cardio-Thoracic Surgery201752471071729156016
