Abstract
Purpose
Malnutrition and chronic inflammation in dialysis patients negatively impacts prognosis. However, intervening to correct this problem (through nutritional supplementation) is often hampered by poor compliance due to both medical and socioeconomic barriers. We have therefore performed a pilot study to investigate the technical feasibility of “directly observed treatment” of nutritional supplementation (protein and omega-3 fatty acids), administered during regular dialysis sessions. Secondary end points included observation of nutritional and inflammatory status of hypoalbuminemic patients undergoing hemodialysis.
Methods
Main inclusion criteria were serum albumin ≤ 3.9 g/dL (3 months prior to the study). Sixty-three eligible patients agreed to participate. Two intervention groups received 30 mL of a liquid protein supplement plus either 2.4 g omega-3 (1800 mg eicosapentaenoic acid + 600 mg docosahexaenoic acid) or a placebo, three times per week after their routine dialysis session for 6 months. Serum albumin, plasma lipids, and other indicators of nutritional and inflammatory status were measured.
Results
Directly observed nutritional supplementation resulted in a significant improvement in the low density lipoprotein cholesterol/high density lipoprotein cholesterol ratio in the omega-3 group as compared to the placebo group (P = 0.043). For the omega-3 group, serum albumin was also marginally higher after 6 months as compared to baseline (P = 0.07). The observed increase in C-reactive protein in the placebo group over 6 months was not apparent in the omega-3 group, although there was no significant difference between groups. Nuclear factor kappa B, malnutrition-inflammation score, normalized protein nitrogen appearance, body mass index, and hemoglobin were unaffected by the intervention.
Conclusion
“Directly observed treatment” with an omega-3 based supplement (as opposed to a pure protein supplement) showed beneficial effects on the lipid profile, and C-reactive protein levels. Further studies using a combination of outpatient and inpatient “directly observed treatment” of omega-3 based supplementation is warranted.
Introduction
Cardiovascular disease (CVD) represents the major source of morbidity and is a leading cause of death in uremic patients on chronic hemodialysis.Citation1 From nontraditional CVD risk factors in dialysis patients, a malnutrition-inflammation complex syndrome (MICS) has been postulated to play a role in the etiology of premature CVD in hemodialysis patients.Citation2 Thus, there is considerable interest in finding appropriate interventions for the MICS in this population.
Protein energy malnutrition is highly prevalent in dialysis patients which negatively impacts prognosis. Protein energy malnutrition is implicated in a complex syndrome caused by nutritional and non-nutritional factors such as deficient food ingestion secondary to uremia, dietary restriction, chronic inflammatory state, and increased catabolism related to treatment modalities, nutrients loss in dialysate, and metabolic acidosis.Citation3 Numerous studies have demonstrated that protein supplementation alone may improve protein metabolism and nutritional parameters and therefore improve clinical outcomes.Citation4–Citation6 Meanwhile, causes of inflammation are multifactorial including exposure of blood to dialyzer membranes or tubing, infection on vascular access, reduced antioxidants, and increased oxidative stress.Citation3,Citation7 Therefore, in order for a nutritional intervention to be most effective, it should be targeted at improving protein status and have anti-inflammatory properties.Citation8
There is a growing scientific interest in the application of omega-3 fatty acids as a means to prevent CVD in dialysis patients. Omega-3 fatty acids have been postulated to reduce pro-inflammatory response, confer antithrombotic properties, improve lipid levels (particularly triglycerides), and improve endothelial function.Citation9–Citation12 To date, there is no well-established recommendation on omega-3 fatty acid supplementation in the dialysis population despite the fact that these patients have lower omega-3 intakeCitation13 and plasma levels.Citation14 Some of the studies published used supraphysiological doses of omega-3 (>3 g/day) which required a high number of capsules and may have been difficult to consume long term.Citation15 Moreover, there may be barriers to compliance with this type of nutritional intervention, especially when the study population includes non-Caucasian races, low income groups, and the unemployed.Citation16 Some of the clinical studies relied only on subjective methods such as pill counting to measure compliance.Citation17,Citation18
Therefore, we performed a pilot study to investigate the technical feasibility of “directly observed treatment” of nutritional supplementation administered during regular dialysis sessions. Secondary outcomes included observations on nutritional and inflammatory status of hypoalbuminemic patients undergoing hemodialysis. We hypothesized that a combination of protein and omega-3 supplementation would be more effective than protein supplementation alone in improving nutritional and inflammatory status.
Methods
Patients
Patients who were undergoing routine hemodialysis treatment at the Great Lake Dialysis Clinic in Detroit, MI, were screened (n = 105). Selection criteria included serum albumin levels not meeting the outcome goal of the Kidney Disease Outcome Quality Initiative (KDOQI) guidelinesCitation19 (≤3.9 g/ dL), age greater than 18 years, and ongoing dialysis treatment for at least 3 months prior to the study. Patients who were residents of nursing homes, receiving intradialytic parenteral nutrition or tube feeding, undergoing 8 hours of dialysis treatment, undergoing nocturnal dialysis, serum albumin > 3.9 g/dL, or who had fish allergies were excluded.
Study design and procedures
The present study was approved by the Human Ethics Committee of Wayne State University and the Human Investigation Committee of Great Lakes Dialysis. Informed written consent was obtained from all patients. Eligible subjects (n = 63) were randomized into two groups; placebo + protein supplement (placebo, n = 32) and omega-3 + protein supplement (omega-3, n = 31). Patients, care givers, and investigators were blinded from group assignments. The study lasted 6 months.
Nutritional intervention and compliance
The nutritional intervention provided comprised two components. Both treatment groups received a blend of 30 mL liquid protein supplement (Proteinex®; Llorens Pharmaceuticals Inc, Miami, FL) in 60 mL of apple juice providing 100 kcal, 18 g protein, and 8 g carbohydrate (specifically, 30 mL of Proteinex provides 18 g of protein hydrolysate [72 kcals], with 1440 mg of L-arginine, 540 mg of L-leucine, 420 mg of L-phenylalanine, 132 mg of L-histidine, 780 mg of L-lysine, 360 mg of L-isoleucine, 132 mg of L-methionine, and 66 mg of L-tryptophan). Additionally, subjects were given four capsules of either omega-3 or placebo, formulated by Twin Rivers Technologies (Quincy, MA). Each of the omega-3 capsules contained 150 mg of docosahexaenoic acid (DHA) and 450 mg of eicosapentaenoic acid (EPA; total DHA 600 mg, total EPA 1800 mg), while the other capsule was a placebo comprised of olive oil. Analysis of omega-3 and placebo capsules is presented in . Both protein and capsules were given to the patients three times a week after their regular dialysis session for a total duration of 6 months. Compliance was ascertained by administering the supplements during the patients’ dialysis session with close monitoring by nurses. Tolerability and side effects of supplements were recorded by registered nurses and hospitalization rates were also monitored.
Table 1 Selected fatty acid composition of omega-3 and placebo capsule
Blood sampling and laboratory measures
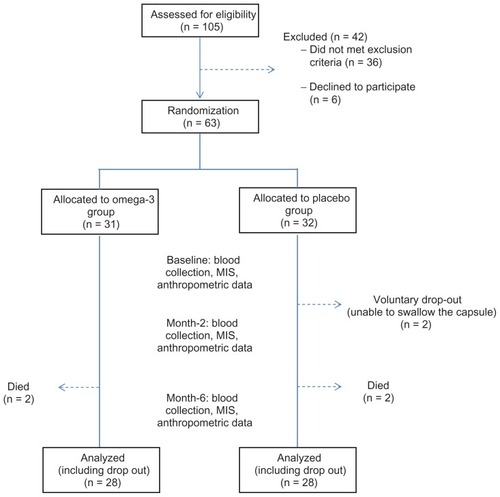
The study flow chart is shown in . Approximately 20 mL of fasting blood sample was taken prior to the dialysis session. Plasma samples intended for lipid analysis were isolated from blood by centrifugation at 3000 rpm for 20 minutes at 4°C and were kept at 4°C to be analyzed on the following day. Blood samples for nuclear factor kappa B (NFκB) were processed immediately to obtain mononuclear cell extract using the Ficoll-Paque methodCitation20 and the extract was kept at −80°C until further analysis. Serum samples for common renal profiles (serum albumin, blood-urea-nitrogen, creatinine, hemoglobin) were sent to Satellite Laboratory Services (Redwood City, CA) for analysis and were measured using standard automated laboratory techniques.
Figure 1 Study’s flow chart.
Abbreviation: MIS, malnutrition-inflammation score.
Lipids analysis
Total cholesterol, high density lipoprotein (HDL) cholesterol, and triacylglycerol (TAG) in the plasma were determined by enzymatic reaction using kits purchased from Pointe Scientific Inc (Canton, MI). Low density lipoprotein (LDL) cholesterol was calculated using the Friedwald equation (LDL-C = total cholesterol minus HDL-C minus TAG/5). LDL-C to HDL-C ratio was calculated by dividing LDL-C by HDL-C values.
Inflammatory markers
Serum C-reactive protein (CRP) was analyzed by an independent laboratory (DMC Laboratory, Detroit, MI) using an immunoturbidimetric method. Activated NFκB was measured from the nuclear extracts using a TransAm chemiluminescent (p65) kit purchased from Active Motif (Carlsbad, CA) using the procedure described by the manufacturer. Nutritional indicators Serum albumin was measured by the bromocresol green method using standard automated laboratory techniques. Normalized protein nitrogen appearance (nPNA) was calculated according to K/DOQI guidelines (2000).Citation19 The malnutrition-inflammation score (MIS) questionnaireCitation21 was also administered prior to (baseline), during (month 2) and at the end of the study (month 6). MIS is a quantitative scoring system that comprises ten components related to patients’ medical history, physical exam, body mass index (BMI), and laboratory parameters, which has been reported to be a useful tool to predict dialysis outcome, malnutrition, and inflammatory status.Citation22–Citation24 MIS was performed and calculated by a single person, a registered dietitian, to minimize interobserver variability.
Statistical analysis
The minimum sample size for each group was n = 31, which was estimated at a power of 80% and α = 0.05 for a two-arm parallel study to detect a 0.2 g/dL difference in serum albumin. Results were analyzed using intention to treat. All study participants were maintained in the treatment groups to which they were randomized regardless of post randomization withdrawal and any missing values reported accordingly. Categorical data are reported as number and percentage, while continuous data are reported as mean ± standard deviation (SD) or as otherwise stated. Independent t-test was used to determine differences in the variables of interest between the two groups at baseline. The difference between baseline and month 2 and between baseline and month 6 for each group were tested using a paired t-test. Data that were not normally distributed were tested using a nonparametric test. Statistical significance was set at α = 0.05. All statistical tests were performed using SPSS (v 16.0; IBM, Chicago, IL). As there was no significant difference between baseline and the 2-month values in any of the parameters measured, these are not discussed further (data not shown).
Results
Demographic profiles
The inclusion criteria were met by 69 patients and 63 agreed to participate. Subjects were randomized based on albumin levels, and with the exception of gender distribution, there were no significant differences in age, duration on dialysis, BMI, and prevalence of existing comorbidity (diabetes mellitus) or indicators of dialysis adequacy (Kt/v) between the two groups (). The study population was homogenously comprised of African-American ethnicities with no difference in income between groups.
Table 2 Clinical and demographic characteristics of the study population
Tolerability, side effects, and compliance
Over the course of the study, four patients died due to (a) cerebrovascular accident (placebo group, n = 1), (b) diabetic infection (omega-3 group, n = 1) and (c) CVD (one patient from each group). There were no other adverse events reported (ie, a life-threatening adverse effect, inpatient hospitalization or prolongation of existing hospitalization, or a persistent or significant disability/incapacity), over the course of the study. No discernible “fishy” smells were reported by any of the patients with regards to capsule assignment. Two patients complained they could not swallow the pills (placebo group) and withdrew from the study (). Twenty-one patients (33%) were able to take 100% of the supplements provided during the 6-month study period. Sixty-seven percent of the patients (n = 22 in the omega-3 group and n = 21 in the placebo group) were able to take greater than 80% of the supplements. The principal reason for lack of compliance was subjects who missed their scheduled dialysis sessions.
Effects on lipid profiles
One subject was excluded from the analysis due to high TAG levels (478 mg/dL) as the Friedwald equation for LDL-C estimation is not reliable when TAG levels exceed 400 mg/dL.Citation25 Total cholesterol was significantly reduced over the 6 months intervention in both groups (P < 0.001; ). At the end of 6 months, the reduction in total cholesterol in the omega-3 group (−37 ± 32 mg/dL) was approximately 50% greater than the reduction seen in the placebo group (−21 ± 26 mg/dL, P = 0.057). While HDL-C levels were increased at month-6 compared to baseline in both groups (t = −4.077, P = 0.000 and t = −3.410, P = 0.004, respectively), there was no significant difference between groups (P = 0.531). LDL-C was reduced in both groups (omega-3 group: t = 6.083, P = 0.000, placebo group: t = 4.200, P = 0.000) at month-6 compared to baseline, however, no significant differences between the two groups were noted at the end of the study (P = 0.092). The LDL-C/HDL-C ratios were significantly improved in both groups compared to baseline (omega-3 group: t = 5.875, P = 0.000, placebo group: t = 4.683, P = 0.000). After 6 months, the omega-3 group had a significantly larger reduction in LDL-C/HDL-C ratio compared to the placebo group (−1.3 ± 1.1 versus −0.7 ± 0.8, P = 0.043). Compared to baseline, TAG levels did not change significantly in the placebo group (P = 0.561), while there was a tendency for a decline in the omega-3 group (P = 0.064).
Table 3 Means and standard deviations of lipid profiles (TC, HDLC, LDLC, and TAG) at baseline and month-6
Effects on nutritional parameters
Serum albumin and other nutritional indices are presented in . Serum albumin at the end of the study was comparable to the values observed at baseline in both the omega-3 (t = −1.895, P = 0.070) and placebo (t = −0.314, P = 0.756) groups. Comparison between both groups showed no significant difference (P = 0.295). Similarly, no changes were observed in MIS score, nPNA, and BMI following the intervention within or between the groups. Additionally, hemoglobin levels were not changed following intervention in both groups (omega-3 group: t = 1.100, P = 0.282, placebo group: t = −0.731, P = 0.471).
Table 4 Means and standard deviations of nutritional status indicators (Ser alb, Hgb, MIS score, nPNA, and BMI) at baseline and month-6
Effects on inflammatory indicators
The NFκB levels observed after 6 months in the omega-3 and placebo groups were similar to baseline values (). Additionally, mean differences (month-6 minus baseline) between omega-3 and placebo groups were not significantly different (P = 0.134). With regards to CRP levels, mean values showed a significant elevation in the placebo group (t = −2.158, P = 0.040) but not the omega-3 group (t = −0.582, P = 0.565) over 6 months. However these differences were not apparent when median CRP values were compared. Additionally, there was a significant inverse association between CRP and albumin levels across both groups (r = −0.261, P = 0.049).
Table 5 Means and standard deviations of inflammatory indicators (NFκB, CRP) at baseline and month-6
Discussion
Our study tested the potential of a combination of protein and omega-3 supplementation to improve nutritional and inflammatory markers in chronic hemodialysis patients. To increase compliance the supplements were administered during patients’ routine dialysis session, three times per week (“directly observed treatment”). Directly observed treatment allowed for two-thirds of the subjects to receive more than 80% of the stated overall dose over a 6-month period. While compliance was excellent in patients who came in for regular dialysis sessions, the significant comorbidities within this patient population resulted in a large number of missed dialysis treatments (and hence missed supplementation).
We observed that serum albumin, one of the markers of nutritional status, was not improved significantly in either group following the intervention. This finding was in contrast to what has been reported in previous studies.Citation4–Citation6 This may be explained by the fact that only a small number of patients were able to take all of the supplements provided to them (no missing days) during the study course (n = 21, 33.3%). Patients missed days of supplementation mostly due to frequent hospitalization or because they failed to show up for their routine dialysis treatment, ranging from 1–44 days. Therefore, this could potentially upset the effect of omega-3 and protein supplementation per se. Further analysis on a pool of patients who substantially completed the supplementation course (ie, taking >80% of the supplements) showed marginal improvement in serum albumin at month-6 compared to baseline (3.6 ± 0.3 g/dL versus 3.7 ± 0.3 g/dL, P = 0.079) but no improvements were noted in those who took <80% of the supplements (3.7 ± 0.2 vs 3.7 ± 0.4, P = 0.939). Interestingly, nPNA, an indicator of protein intake, remained constant in both groups despite protein supplementation. A similar study by Moretti et alCitation26 also noted a similar trend, in which there were no changes in nPCR despite improvement in serum albumin in the protein group for the second 6 months.
Reduced protein intake and an increase in inflammatory response are two important factors that lead to a decrease in serum albumin.Citation27 However, Kaysen et alCitation28 had noted that low serum albumin in dialysis patients may be attributed to systemic inflammation rather than nutritional inadequacy as a causative factor per se. In relation to this, we also observed a significant inverse correlation between serum albumin and CRP which may indicate the influence of an inflammatory process on serum albumin levels. Friedman and FademCitation29 suggested that serum albumin should be taken as a marker of illnesses rather than nutrition. This is due to the fact that serum albumin has a strong ability to predict mortality but rather limited prediction for nutritional status due to significant influence of non-nutrition causes (such as inflammation).
Many of the omega-3 fatty acid supplementation studies in dialysis patients have described various potential outcomes such as attenuating dyslipidemia, inflammation, and providing a cardioprotective effect. Moreover, there is substantial evidence for reducing TAG levelsCitation30–Citation32 even at a dosage as low as 1.5 g/day.Citation33 As for plasma TAG, we saw a tendency for a reduction in TAG levels in both groups although in the omega-3 group statistical significance was marginal (P = 0.064). The large variation in the difference in TAG changes observed in the placebo group (−7 ± 61 mg/dL, P = 0.56, ) could be attributed to one subject with very high triglyceride concentrations. Upon removal of this subject the difference in TAG levels between the 6-month and baseline value was 1 ± 44 mg/dL, P = 0.89. Thus collectively these data suggest no change in TAG levels over 6 months in the placebo group, while there was a tendency for a reduction in TAG levels in the omega-3 group (−20 ± 44 mg/dL, P = 0.064). Previous studiesCitation18,Citation34 which administered a higher amount of omega-3 per week, with varying percentages of EPA/DHA but with a shorter duration (4–8 weeks), also reported no changes in TAG levels. However, Bouzidi et al reported that a supplementation of 2.1 g omega-3 daily for 3 months among chronic kidney disease patients reduced TAG levels by 48%.Citation35 However, it is important to note that the baseline TAG levels in their study were much higher than the current study (275 ± 58 mg/dL versus 123 ± 60 mg/dL in the omega-3 group). We postulate that, the baseline TAG levels (omega-3 group: 123 ± 60 mg/dL; placebo group: 104 ± 69 mg/dL) were within the normal levels and thus may not have been sufficiently elevated to achieve a significant reduction. Skulas-Ray et al reported that the extent of TAG lowering with omega-3 is a function of baseline TAG levels.Citation36 Omega-3 supplementation resulted in better improvement in LDL-C/HDL-C ratios as compared to placebo which appeared to be due to a greater improvement in non-HDL-C. As for inflammatory markers, our results for CRP were inconclusive. While mean values in the placebo group increased over the 6-month period, this was not the case in the omega-3 group, in which CRP levels stayed the same. Thus omega-3, if not effective in attenuating inflammation, may be beneficial in preventing further increases in inflammatory status. However when the data were evaluated using median CRP values, these differences were no longer apparent suggesting the need for a larger sample size to definitively resolve this issue. Only a small number of studies have investigated the effects of omega-3 on inflammatory markers in hemodialysis patients. It is important to note that most of these studies are not comparable due to differences in study design, supplement dosage, EPA/DHA ratios and study duration. Saifullah et al showed that a supplementation of 1.3 g of oral EPA and DHA daily over a period of 3 months could modestly reduce CRP levels.Citation37 However, a recent study using a larger dosage (2.08 g/day) but a shorter duration (10 weeks) showed no effects on serum systemic inflammatory markers (CRP, interleukin-6, tumor necrosis factor-α) and oxidative stress (malondialdehyde, total antioxidant capacity).Citation38 In a prospective cohort study by Noori et al, the authors showed that a lower omega-6 to omega-3 ratio (~6) was associated with decreased inflammation and overall mortality in hemodialysis patients which indicates the importance of n-6/3 polyunsaturated fatty acid ratios in the diet.Citation13 However, our study was not designed to investigate the effects of this ratio per se.
NFκB, a key player in pathogenesis of inflammation, is stimulated by pro-inflammatory agents such as cytokines and CRP. Studies have shown that NFκB activation and subsequent activation of mononuclear cells triggers a process that causes myocardial inflammatory damage in hemodialysis patients.Citation39,Citation40 Interestingly, our data for translocation of activated NFκB to the nucleus showed no significant changes following the intervention within and between both groups even though we saw an increase in CRP levels in the placebo group. The latter may have been due to the fact that the baseline CRP values in the placebo group were lower than those assigned to the omega-3 group.
Study limitations
We were restricted in our patient population to one dialysis clinic for this pilot study. While the lipid data suggested benefits of omega-3, the data for inflammatory markers was less clear cut. One plausible explanation for variation in inflammatory markers in the current study may be related to insufficient dosage/frequency of omega-3 supplementation as well as compliance (due to frequent hospitalization resulting in subjects missing dialysis sessions and therefore supplementation). There are several similar studies which also failed to report significant changes in inflammatory markers.Citation18,Citation41–Citation43 Studies which demonstrated a significant effect of omega-3 supplementation on inflammation indices are those with a higher dosage and more frequent administration of the supplement (9.1 to 21 g/week versus 7.2 g/week DHA + EPA in the current study) as well as reported higher patient compliance.Citation17,Citation44–Citation46 Another factor that could potentially explain the contradictory finding in our study with those studies is baseline levels of inflammatory markers. Omega-3 supplementation appears to be more effective in studies reporting higher baseline CRP (>13.8 mg/dL) than those that did not.Citation17,Citation38,Citation44
Notwithstanding some of the limitations discussed above, ours is one of the few studies to report on the use of “directly observed treatment” of oral nutritional supplementation with protein and omega-3 in a cohort of hemodialysis patients. Our results suggest that “directly observed treatment” is technically feasible in hemodialysis patients and does not disrupt the normal dialysis schedule. The relatively large number of missed dialysis sessions due to hospitalizations, however, suggests that “directly observed treatment” should be used in the setting of both outpatient and inpatient dialysis sessions in order to optimize compliance. In addition, while emphasizing the huge progressive inflammatory burden in hemodialysis patients over time; this pilot study suggests that “directly observed treatment” with a combination of omega-3 and protein-based supplement (as opposed to a pure protein supplement) could have some beneficial effects on lipid profile and CRP progression. Further studies using a combination of outpatient and inpatient “directly observed treatment” of fish oil based nutritional supplementation are warranted.
Acknowledgments
The authors express sincere gratitude to all participants and Great Lake Dialysis Clinic staff for their help and cooperation. The authors are also especially thankful to Janice Jackson, Mariam Beydoun, and Bryan Strouse from Wayne State University for the technical assistance. We are extremely grateful to Dr Prabir Roy-Chaudhury from the Division of Nephrology, University of Cincinnatti, for his critical and helpful comments on the manuscript.
Disclosures
Omega-3 and placebo capsules were formulated and donated by Twin Rivers Technologies Inc (Cincinnati, OH). The protein supplements were from Llorens Pharmaceuticals Inc (Miami, FL) including donation for 1 month. The authors declare no conflict of interest in this work.
References
- GirayBKanEBaliMHincalFBasaranNThe effect of vitamin E supplementation on antioxidant enzyme activities and lipid peroxidation levels in hemodialysis patientsClin Chim Acta20033381–2919814637272
- StenvinkelPHeimburgerOPaultreFStrong association between malnutrition, inflammation, and atherosclerosis in chronic renal failureKidney Int19995551899191110231453
- Kalantar-ZadehKIkizlerTABlockGAvramMMKoppleJDMalnutrition-inflammation complex syndrome in dialysis patients: causes and consequencesAm J Kidney Dis200342586488114582032
- StrattonRJBircherGFouqueDMultinutrient oral supplements and tube feeding in maintenance dialysis: a systematic review and meta-analysisAm J Kidney Dis200546338740516129200
- CanoNNutritional supplementation in adult patients on hemodialysisJ Ren Nutr200717110310517198944
- MeadeAProtein supplementation with sports protein bars in renal patientsJ Ren Nutr200717321421717462554
- RazeghiEOmatiHMaziarSKhashayarPMahdavi-MazdehMChronic inflammation increases risk in hemodialysis patientsSaudi J Kidney Dis Transpl200819578578918711296
- Kalantar-ZadehKBragliaAChowJAn anti-inflammatory and antioxidant nutritional supplement for hypoalbuminemic hemodialysis patients: a pilot/feasibility studyJ Ren Nutr200515331833116007562
- HarrisWSParkYIsleyWLCardiovascular disease and long-chain omega-3 fatty acidsCurr Opin Lipidol200314191412544655
- HuFBBronnerLWillettWCFish and omega-3 fatty acid intake and risk of coronary heart disease in womenJAMA2002287141815182111939867
- EgertSStehlePImpact of n-3 fatty acids on endothelial function: results from human interventions studiesCurr Opin Clin Nutr Metab Care201114212113121252652
- OlzaJMesaMDAguileraCMInfluence of an eicosapentaenoic and docosahexaenoic acid-enriched enteral nutrition formula on plasma fatty acid composition and biomarkers of insulin resistance in the elderlyClin Nutr2010291313719573960
- NooriNDukkipatiRKovesdyCPDietary omega-3 fatty acid, ratio of omega-6 to omega-3 Intake, inflammation, and survival in long-term hemodialysis patientsAm J Kidney Dis201158224825621658827
- MadsenTChristensenJHSvenssonMWittPMToftESchmidtEBMarine n-3 polyunsaturated fatty acids in patients with end-stage renal failure and in subjects without kidney disease: a comparative studyJ Ren Nutr201121216917520833075
- FriedmanAMoeSReview of the effects of omega-3 supplementation in dialysis patientsClin J Am Soc Nephrol20061218219217699207
- GriffithSA review of the factors associated with patient compliance and the taking of prescribed medicinesBr J Gen Pract1990403321141162112014
- BowdenRGWilsonRLDeikeEGentileMFish oil supplementation lowers C-reactive protein levels independent of triglyceride reduction in patients with end-stage renal diseaseNutr Clin Pract200924450851219461006
- PouliaKAPanagiotakosDBTourledeEOmega-3 fatty acids supplementation does not affect serum lipids in chronic hemodialysis patientsJ Ren Nutr201121647948421439849
- K/DOQIClinical practice guidelines for nutrition in chronic renal failure. K/DOQI, National Kidney FoundationAm J Kidney Dis2000356 Suppl 2S114010895784
- RuitenbergJJMulderCBMainoVCLandayALGhanekarSAVACUTAINER CPT and Ficoll density gradient separation perform equivalently in maintaining the quality and function of PBMC from HIV seropositive blood samplesBMC Immunol200671116725038
- Kalantar-ZadehKKoppleJDBlockGHumphreysMHA malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patientsAm J Kidney Dis20013861251126311728958
- PisetkulCChanchairujiraKChotipanvittayakulNOng-AjyoothLChanchairujiraTMalnutrition-inflammation score associated with atherosclerosis, inflammation and short-term outcome in hemodialysis patientsJ Med Assoc Thai201093Suppl 1S14715620364569
- HoLCWangHHChiangCKHungKYWuKDMalnutrition-inflammation score independently determined cardiovascular and infection risk in peritoneal dialysis patientsBlood Purif2010301162420588008
- RambodMBrossRZitterkophJAssociation of Malnutrition-Inflammation Score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort studyAm J Kidney Dis200953229830919070949
- FriedewaldWTLevyRIFredricksonDSEstimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifugeClin Chem19721864995024337382
- MorettiHDJohnsonAMKeeling-HathawayTJEffects of protein supplementation in chronic hemodialysis and peritoneal dialysis patientsJ Ren Nutr200919429830319539184
- MoshageHJJanssenJAFranssenJHHafkenscheidJCYapSHStudy of the molecular mechanism of decreased liver synthesis of albumin in inflammationJ Clin Invest1987796163516413584463
- KaysenGADubinJAMullerHGRosalesLLevinNWMitchWEInflammation and reduced albumin synthesis associated with stable decline in serum albumin in hemodialysis patientsKidney Int20046541408141515086482
- FriedmanANFademSZReassessment of albumin as a nutritional marker in kidney diseaseJ Am Soc Nephrol201021222323020075063
- AndoMSanakaTNiheiHEicosapentanoic acid reduces plasma levels of remnant lipoproteins and prevents in vivo peroxidation of LDL in dialysis patientsJ Am Soc Nephrol199910102177218410505695
- VegaGLChandaliaMSzczepaniakLSGrundySMEffects of N-3 fatty acids on hepatic triglyceride content in humansJ Investig Med2008565780785
- HauenschildABretzelRGSchnell-KretschmerHKloerHUHardtPDEwaldNSuccessful treatment of severe hypertriglyceridemia with a formula diet rich in omega-3 fatty acids and medium-chain triglyceridesAnn Nutr Metab201056317017520150726
- KhajehdehiPLipid-lowering effect of polyunsaturated fatty acids in hemodialysis patientsJ Ren Nutr200010419119511070146
- Perunicic-PekovicGBRasicZRPljesaSIEffect of n-3 fatty acids on nutritional status and inflammatory markers in haemodialysis patientsNephrology (Carlton)200712433133617635746
- BouzidiNMekkiKBoukaddoumADidaNKaddousABouchenakMEffects of omega-3 polyunsaturated fatty-acid supplementation on redox status in chronic renal failure patients with dyslipidemiaJ Ren Nutr201020532132820303788
- Skulas-RayACWestSGDavidsonMHKris-EthertonPMOmega-3 fatty acid concentrates in the treatment of moderate hypertriglyceridemiaExpert Opin Pharmacother2008971237124818422480
- SaifullahAWatkinsBASahaCLiYMoeSMFriedmanANOral fish oil supplementation raises blood omega-3 levels and lowers C-reactive protein in haemodialysis patients – a pilot studyNephrol Dial Transplant200722123561356717623719
- KooshkiATalebanFATabibiHHedayatiMEffects of marine omega-3 fatty acids on serum systemic and vascular inflammation markers and oxidative stress in hemodialysis patientsAnn Nutr Metab201158319720221757893
- RajDSBoivinMADominicEAHaemodialysis induces mitochondrial dysfunction and apoptosisEur J Clin Invest2007371297197718036031
- ShahVOFergusonJHunsakerLADeckLMVander JagtDLCardiac glycosides inhibit LPS-induced activation of pro-inflammatory cytokines in whole blood through and NF-kB-dependent mechanismInt J Appl Res Nat Prod2011411
- Szklarek-KubickaMFijalkowska-MorawskaJZaremba-DrobnikDUcinskiACzekalskiSNowickiMEffect of intradialytic intravenous administration of omega-3 fatty acids on nutritional status and inflammatory response in hemodialysis patients: a pilot studyJ Ren Nutr200919648749319616450
- VernaglioneLCristofanoCChimientiSOmega-3 polyunsaturated fatty acids and proxies of cardiovascular disease in hemodialysis: a prospective cohort studyJ Nephrol20082119910518264942
- FiedlerRMallMWandCOstenBShort-term administration of omega-3 fatty acids in hemodialysis patients with balanced lipid metabolismJ Ren Nutr200515225325615827899
- SaifullahAWatkinsBASahaCLiYMoeSMFriedmanANOral fish oil supplementation raises blood omega-3 levels and lowers C-reactive protein in haemodialysis patients – a pilot studyNephrol Dial Transplant200722123561356717623719
- Rasic-MilutinovicZPerunicicGPljesaSEffects of N-3 PUFAs supplementation on insulin resistance and inflammatory biomarkers in hemodialysis patientsRen Fail200729332132917497447
- EwersBRiserusUMarckmannPEffects of unsaturated fat dietary supplements on blood lipids, and on markers of malnutrition and inflammation in hemodialysis patientsJ Ren Nutr200919540141119541503