Abstract
Background and purpose Cup failure is a recognized problem in total trapeziometacarpal (TM) joint prostheses; it may be related to poor fixation, which can be revealed by radiostereometric analysis (RSA). We compared the early implant migration of cemented trapezium cups to that of uncemented screw cups.
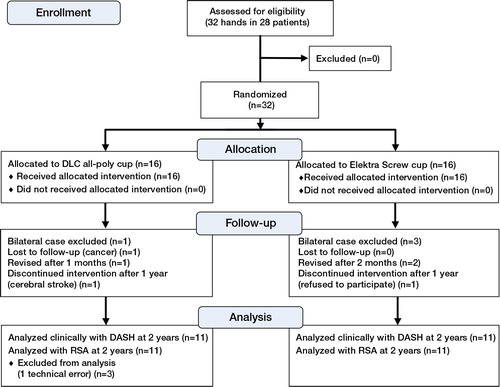
Patients and methods In a prospective, parallel-group, randomized patient-blinded clinical trial, we included 32 hands in 28 patients (5 males) with a mean age of 58 (40–77) years and with Eaton stage-2 or -3 osteoarthritis of the trapeziometacarpal joint. Patients were randomized to surgery with a cemented DLC all-polyethylene cup (C) (n = 16) or an uncemented hydroxyapatite-coated chrome-cobalt Elektra screw cup (UC) (n = 16). Uncemented cups were inserted without threading of the bone. Stereoradiographs for evaluation of cup migration (primary effect size) and DASH and pain scores were obtained during 2 years of follow-up.
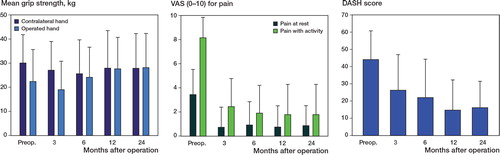
Results The 2-year total translation (TT) was similar (p = 0.2): 0.24 mm (SD 0.10) for the C (n = 11) and 0.19 mm (SD 0.16) for the UC (n = 11). Variances were similar (p = 0.4). Judged by RSA, 2 UC cups and 1 C cup became loose (TT > 1 mm). Both UC cups were found to be loose at revision. Grip strength, pain, and DASH scores were similar between groups at all measurement points.
Interpretation Early implant fixation and clinical outcome were equally good with both cup designs. This is the first clinical RSA study on trapezium cups, and the method appears to be clinically useful for detection of loose implants.
Total arthroplasty for trapeziometacarpal (TM) joint osteoarthritis, replacing the TM joint with a small ball and socket joint, has been used for more than 40 years (de la Caffiniere and Aucouturier Citation1979). Compared to trapeziectomy, total arthroplasty may result in faster rehabilitation and better grip strength after 1 year (Ulrich-Vinter et al. 2008), but high rates of loosening of TM arthroplasty components have been reported both in cemented and uncemented implants—especially of the trapezium component (Braun Citation1982, Cooney et al. Citation1987, Søndergaard et al. Citation1991, Wachtl et al. Citation1998, Van Capelle et al. Citation1999, Perez-Ubeda et al. Citation2003, Hansen and Snerum Citation2008, Hansen and Vainorious Citation2008, Hernandez-Cortez et al. 2012).
The fixation of uncemented implants relies on initial press-fit fixation until secondary bony anchorage into the microporous surface of the implant has been obtained. Loosening of uncemented implants within the first 2 years after surgery may be the result of failure of either the primary or the secondary fixation. The Elektra grit-blasted chrome-cobalt hydroxyapatite-coated trapezium screw cup (Regnard Citation2006) is a cone-shaped screw cup that is inserted using a press-fit fixation technique. 2 recent studies have have described a high rate of early loosening, indicating a possible problem with press-fit fixation of the screw cup (Hansen and Snerum Citation2008, Hernandez-Cortez et al. 2012). In an experimental study using RSA for evaluation of implant fixation, Hansen et al. (Citation2011) found that changing the bone preparation technique for the Elektra screw cup by alleviating threading of the trapezium bone before insertion of the implant improves the primary press-fit fixation. In the same study, the press-fit fixation of the uncemented Electra screw cup was found to be as good as with a cemented trapezium cup. The clinical importance of these findings is clinically unproven.
We hypothesized that the clinical fixation (primary effect parameter) of uncemented Elektra screw cups, when inserted without threading of the bone, would be comparable to fixation of cemented all-polyethylene trapezium cups (the gold standard for primary TM cup fixation).
Patients and methods
Between April 2008 and October 2009, 32 hands of 28 patients (5 males) with Eaton-Glickel stage-2 or -3 TM joint osteoarthritis (OA) were assessed for eligibility in this parallel-group, randomized patient-blinded clinical trial at our institution (Eaton and Glickel Citation1987). The trial was performed in accordance with the Helsinki Declaration of 1975, as revised in 2000. The reporting of data from this trial complies with the CONSORT statement. The study was approved by the Regional Committee of Biomedical Research Ethics (journal no. M-20080043; issue date April 14, 2008) and it was registered at Clinicaltrials.gov (NCT01554748). One author (TBH) enrolled the patients and all the patients who were eligible gave their informed consent to be participants in the study. Randomization was done by drawing labels from a box, and the labels were then concealed in 32 sequentially numbered closed envelopes. Just prior to the operation, an operating nurse chose an envelope, which randomized the patient to insertion of either a cemented DLC all-polyethylene cup or an uncemented Elektra chrome-cobalt grit-blasted hydroxyapatite-coated screw cup.
Sample size
Based on the standard deviation (SD) of the total translation (TT) of clinical double examinations (SD of DLC cup = 1.14 mm; SD of screw cup = 0.32 mm) from Hansen et al. (Citation2010), the sample size for the study was estimated to be 12 patients per group, considering a 1.0-mm difference in TT with a power of 80% and an alfa of 5%. To balance dropouts in the study and the risk of problems associated with analysis of small-scale RSA in a clinical setting, we included 2 groups with 16 hands in each.
Criteria
Inclusion criteria were Eaton-Glickel stage-2 or -3 TM joint OA in patients over 18 years of age where nonoperative treatment had failed. OA staging was based on a combination of conventional radiographs and CT scans evaluated by one observer (Hansen et al, Citation2012). Exclusion criteria were patients with known osteoporosis, scaphotrapeziotrapezoidal affection (judged by the CT scan), low functional demand, sequelae of carpal bone fracture, metabolic bone disease (i.e. rheumatoid arthritis or morbus Paget), cancer or chemotheraphy, younger females with a wish of pregnancy within the planned follow-up period, alcoholism, or severe psychiatric illness. In those cases, trapeziectomy was the recommended standard treatment in our department.
Components
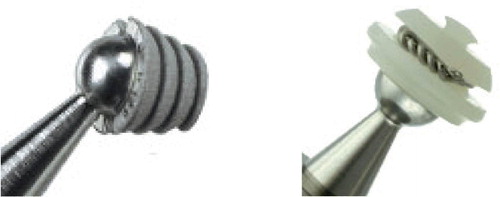
In all study patients, an uncemented Elektra grit-blasted titanium hydroxyapatite-coated metacarpal stem was used in combination with a 1-piece chrome-cobalt neck/head. The cups were either a cemented DLC all-polyethylene cup (C) or an uncemented Elektra chrome-cobalt grit-blasted hydroxyapatite-coated screw cup (UC) (Small Bone Innovations Inc., Les Bruyères, France) (). The articulation of the C was polyethylene-on-metal, whereas it was metal-on-metal with the UC.
Figure 1. The Elektra uncemented chrome-cobalt hydroxyapatite-coated screw cup (UC group) and the cemented DLC all-polyethylene cup (C group).
All the patients were operated by one surgeon (TBH) under general anesthesia using a tourniquet, and we used the standard technique described for insertion of the Elektra total joint arthroplasty (Regnard Citation2006, Hansen and Snerum Citation2008). However, we did not use the threading of the trapezium as recommended by the manufacturer before insertion of the screw cup; therefore, all Elektra screw cups were inserted without threading of the trapezium before insertion. For insertion of the DLC cup in the trapezium, a spherical drill was used to drill a cavity formed to the measured size of the cemented DLC cup using the standard DLC measuring instruments, and the cups were fixated with Palacos gentamycin bone cement (Haereus Medical, Hanau, Germany). As described by Hansen et al. (Citation2010), five 1.0-mm tantalum beads were inserted into the trapezium for RSA and evaluation of migration. All patients were treated prophylactically with a single dose of 1 g dicloxacilline intravenously. No pharmaceutical anti-thrombotic prophylaxis was used.
Clinical rehabilitation and follow-up
All the patients in both groups were immobilized in a plaster of Paris splint for 3 weeks after the operation. After 3 weeks, all of them were allowed to do light exercises. Unlimited use of the hand was allowed after 3 months. The patients did not receive any occupational therapy. Clinical follow-up with measurements of grip strength, VAS (0–10) at rest or with activity, and patient-reported outcome score (Disability of the Arm, Shoulder, and Hand (DASH) score) was done by an independent observer (a nurse from the outpatient clinic) with no knowledge of the type of implant used before surgery, and again at 3 months, 6 months, 12 months, and 24 months after the operation.
RSA
Stereoradiographs were obtained on the first postoperative day (the reference examination). Subsequent examinations were completed at 3 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years. Examinations were done with the patient sitting next to the stereoradiographic equipment at the foot-end of the stereoradiographic table with the operated hand positioned palm-down on the calibration box. The anatomical axis of the third metacarpal was parallel with the y-axis of the calibration box. The position and orientation of the global coordinate system in the reference examination defined the direction of implant migration in the follow-up examinations (Hansen et al. Citation2010). The radiographic setup and the analysis of the stereoradiographs with marker-based RSA for the DLC cups and model-based RSA for the Elektra cups (Medis Specials, Leiden, the Netherlands) was as described by Hansen et al. (Citation2010). The upper limit for mean-error rigid-body fitting (the stable marker model used for migration analysis) was 0.5 mm. The mean condition number (dispersion of the bone markers) in the trapezium was 95 (SD 32) and the mean condition number for the PC was 184 (SD 48). The mean difference in matching of the surface model to the Elektra screw cup radiographic contour (model pose estimation) in the radiograph was 0.07 mm (SD 0.02) (Kaptein et al Citation2003).
Analysis of all stereoradiographs was performed by one observer with the Model-Based RSA version 3.2 software (Medis Specials, Leiden, the Netherlands). Implant migration was evaluated using all 6 stereoradiographs with the postoperative stereoradiograph as the reference. The point of measurement was the center of gravity of the 3D surface model/marker model in relation to the bone markers as the fixed rigid-body reference. As we have reasoned previously, only the translations—and not the rotations—were interpreted (Hansen et al. Citation2010), and we calculated the summed migration vector of absolute migrations by use of Pythagoras’ theorem (TT = √(x2 + y2 + z2), where TT is the total translation).
Precision of RSA
Double-examination stereoradiographs were obtained in 20 patients as previously described (Hansen et al. Citation2010) and were used to document the clinical precision of small-scale marker-based and model-based RSA with these specific components, as recommended by Valstar et al. (Citation2005). The same team of 4 radiographers performed all RSA radiographs. The postoperative stereoradiograph was used as the reference in migration analysis of the double examinations, and the expected difference in displacement between the 2 calculations represents the systematic error of the RSA system (bias) and should (optimally) be zero. The standard deviation reflects the precision of the system ().
Table 1. Measurement error of RSA based on 20 double-examination stereo radiographs. The mean value represents the systematic error, or bias of the system, between 2 measurements taken on the same day. The standard deviation (SD) represents the precision of the system
Statistics
With the inclusion of 4 bilateral cases, we were challenged with non-independent observations in our final dataset (Bryant et al. Citation2006). It was unfortunately not possible to transform and normalize the dataset properly, in order to deal with the dependency problems by using a mixed-model statistical analysis. We therefore excluded 1 set of data from the bilateral cases (the data from the second hand that was operated) and used regular statistics for independent data. When the data followed a Gaussian function (checked by the Shapiro-Wilk test), the groups were then compared by Student’s t-test. When there were unequal variances (checked by an F-test), Satterthwaite’s t-test was used. When data did not follow a Gaussian function, non-parametric tests were used (Mann-Whitney U-test for unpaired data, Wilcoxon signed-rank test for paired data, and Fisher’s exact test (used for an expected cell count of 5 or less) for categorical data). Levene’s robust test was used to test equality of variances for non-normal data. For interpretational reasons, we present the mean (SD) of the total translations (TTs) numerically. The primary RSA endpoints were the total translations. The secondary RSA endpoints were the absolute individual migrations along the single axes. Statistical significance was assumed at p-values of < 0.05. Intercooled Stata version 11.0 (StataCorp, College Station, TX) was used for statistical computations.
Results
Clinical results
After excluding the data from the hand that was operated last in the 4 bilateral cases, 28 patients (28 hands, 4 male patients) were finally included in the study (). 1 patient (C group) was diagnosed as having an aggressive cancer in the days after surgery, and did not continue in the study. 2 patients were revised shortly after surgery; 1 patient (C group) had an intraoperative cementing failure necessitating revision (re-cementation) 1 month after primary surgery. Another patient (UC group) fell twice and first suffered a traumatic luxation of the head of the prosthesis 4 weeks after surgery that was treated with closed reduction, and at 8 weeks she suffered a traumatic fracture of the trapezium with cup loosening; she was revised with a trapeziectomy. 3 other patients did not complete the 2-year study period: 1 patient (C group) suffered a cerebral stroke after 1 year and was unable to attend the 2-year examination, and another patient (UC group) refused to attend the final 2-year examination. Neither of these 2 patients reported clinical symptoms of implant failure on oral interview at 2-year follow-up. In 1 patient (C group), we could not analyze the 2-year stereoradiographs because of occluded markers. A 63-year-old woman (UC group) had pain (VAS 7) at rest and with activity (VAS 10) at the 2-year follow-up, with clear cup loosening on radiographs and extreme cup migration (TT = 6 mm). She was revised to a cemented DLC cup just after the 2-year follow-up, and during the revision we found the cup to be loose, but the stem to be well-fixed. A 51-year-old woman (C group) had onset of pain at the 2-year follow-up, VAS 2 at rest, and VAS 7 with activity, with radiographic suspicion of loosening and cup migration of over 1 mm (TT = 1.61 mm), but she did not want a reoperation and is still functioning with the cup apparently in situ on regular radiographs. Thus, 22 hands (11 C group and 11 UC group) remained for clinical and radiographic evaluation at the 2-year follow-up.
Table 2. Patient demographics at the time of inclusion (preoperatively)
Apart from cup loosening, there were no other complications during the observation period. 2 cups were revised (1 C and 1 UC) during the study period, and another cup was revised just after our data collection. We did not find any statistically significant differences between groups regarding DASH score, grip strength, or VAS at rest or with activity, at any postoperative measure point ().
RSA results
At 2 years, 5 patients had left each study group (), leaving 11 patients in each group for the 2-year assessment. 3 cups, which we judged to be loose, had migrated more than 1 mm; 2 of these were revised (at 8 weeks and after 2 years) and they were intraoperatively confirmed to be loose (). One cemented cup clearly changed position between 3 and 6 months, as judged by the conventional radiographs and RSA (1 mm radial translation). 1 outlier/loose cup in the UC group with very large migration (Z-migration of 6.8 mm; TT = 6.9 mm) especially affected the results in these small study we decided to perform the statistical comparison of implant migration both with and without the 2 outliers (1 C and 1 UC) that remained in the dataset at 2 years follow-up (). 2 patients (C group) did not have their 6-week stereoradiographs because of a workers’ strike at the Department of Radiology. We had technical problems with occluded markers in 4 of 186 stereoradiographs (2 C and 2 UC), which we could not solve. 1 of these was a C-group patient who was excluded at the final follow-up because of loose reference markers (high rigid-body error). The numbers of stereoradiographs analyzed per follow-up are shown in .
Figure 5. Box-and-whisker plot of the total translations (TTs) showing the sample minimum, lower quartile, median, upper quartile, and the sample maximum. All patients are shown in the graph and 3 outliers are indicated by the dots above 1 mm TT. The numbers of stereo radiographs assessed for each follow-up are given under the lower whiskers.
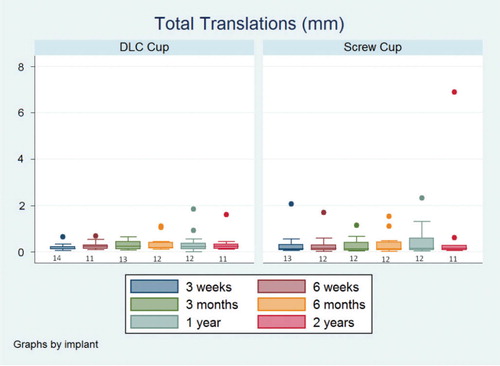
Figure 4. Line-and-scatter plot of the total translation (TT) for each individual patient with a screw cup (UC group; n = 13) or a DLC all-polyethylene cup (C group; n = 14). It is clear that 3 patients (all clinically symptomatic with a VAS score at rest of above 7) are outliers with cup migration above 1 mm. 2 of these cups (both UC) were revised and found to be completely loose in the trapezoid bone. One DLC cup seemed to migrate above 1 mm at the 6-month and 1 year follow-up and then return to previous levels at 2 years. The patient was asymptomatic, and RSA analysis in this case was difficult because of occluded markers at these to follow-up visits. We suspected that this was the explanation for the migration curve.
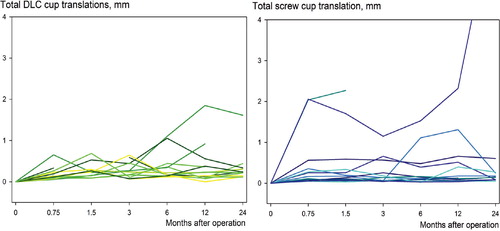
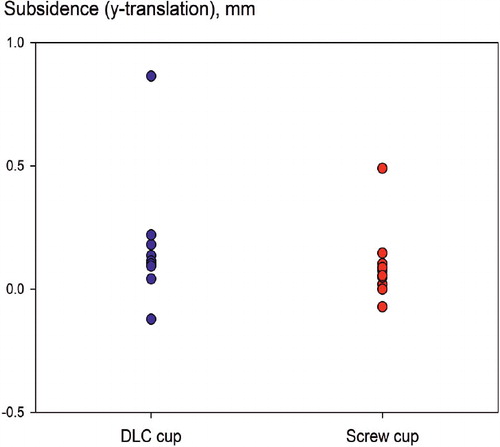
At 2 years, the UC cups (n = 11) had migrated by a mean TT of 0.80 mm (SD 2.0, 95% CI: –0.56 to 2.2) and the C cups (n = 11) had migrated by a mean TT of 0.36 mm (SD 0.43, 95% CI: 0.07–0.64). The difference in TT between groups was –0.44 mm (95% CI: –1.7 to 0.86), which was similar (rank sum test, p = 0.3). Using Levine’s robust test for equality of variances to test the SD of the TT, the SD in the 2 groups was similar at 2 years (p = 0.1). Since especially the 1 loose screw cup had migrated very much by 2 years, it biased the TT of the groups, and we therefore also present the TT group comparisons without the 2 loose cups remaining at 2 years follow-up (outliers with TT of more than 1 mm at 2 years of follow-up) ( and ). Excluding these 2 cups at the 2-year analysis, we found a similar TT (rank sum test, p = 0.2) between the groups with 0.24 mm (SD 0.10; 95%CI: 0.16–0.31) for the C group (n = 10) and 0.19 mm (SD 0.16; 95%CI: 0.07–0.31) for the UC group (n = 10). The SD was similar at 2 years in the 2 groups (p = 0.4) (again using Levine’s robust test for equality of variances to test the SD of the TT). TT was similar between the groups on all follow-up occasions (p > 0.2) (). We found no statistically significant difference in absolute translations along any of the 3 coordinate axes between the 2 groups at any follow-up. There was a significant difference (p = 0.003) in the segment motion (signed values) along the x-axis at 2-year follow-up with a mean of 0.09 (SD 0.06) in the C group and a mean of –0.03 (SD 0.09) in the UC group. There was no statistically significant difference between groups for the y- and z-coordinate axes at any follow-up. The results of the bilateral cases are presented in . Most cups seemed to subside (), but the values were below the precision limit for the UC component and there was no statistically significant difference between the groups (p = 0.5). Based on the double examinations, the precision of the method was acceptable (). All measurements during the follow-up time were below or at the precision limit of the system.
Table 3. Absolute translations (in mm) of the clinical RSA examinations at 2-year follow-up. There was no statistically significant difference between the groups (p > 0.2)
Table 4. Segment (signed) motion (mm) of the clinical RSA examinations at 2-year follow-up
Table 5. Total translation for the 4 bilateral cases at 2-year follow-up
Figure 6. Subsidence of the cups at 2 years (positive values indicate subsidence). 11 patients per group were available and there was no significant difference between groups (rank sum test; p = 0.5).
Judged by conventional radiographs and RSA, 1 C became loose between 3 and 6 months and settled in a different position (radial translation (x-axis) of 1 mm). The patient was asymptomatic and the cup was left in situ.
Discussion
To our knowledge, this is the first clinical study to use RSA for evaluation of implant fixation in TM total joint arthroplasty of the thumb, and the first randomized study to compare cemented and uncemented trapezium implants. The clinical results are comparable to those of other studies (Ulrich-Vinther et al. Citation2008, Klahn et al. Citation2012), but different survival rates have been presented for both cemented and uncemented trapezium implants, and no clear recommendation for the choice of cemented and uncemented implants has been published based on long-term evidence. With a high risk of revision both implant types, there is a theoretical and practical advantage in using uncemented trapezium implants because conversion of a failed uncemented trapezium cup to a cemented cup is easier and less bone stock is lost than with cementing of the the primary trapezium cup. Revision of primary cemented implants often results in a trapeziectomy, and even though the results of revision surgery with trapeziectomy appear to be quite good (Hansen and Homilius Citation2010), a revision to another trapezium implant may provide better function in high-demand patients. The high revision rates of 15–44% reported for uncemented implants (Wachtl et al. Citation1998, Hansen and Snerum Citation2008, Hansen and Vainorious Citation2008, Hernandez-Cortez et al. 2012, Klahn et al. Citation2012) indicate a problem with the bony fixation. Several reasons can be put forward such as poor bone quality in the trapezium preoperatively, smoking, implant material, implant design, implant coating, and surgical technique (Hansen Citation2011). Furthermore, substantial horizontal force in the joint is applied during pinch grip (Cooney and Chao Citation1977), which may contribute to the high risk of implant failure.
Modification of the surgical technique for the Elektra screw cup by alleviating threading of the bone before implant insertion appears to improve early press-fit fixation of the implant in an experimental setting, and may possibly prevent the previously reported high and early clinical failure rates (Hansen and Snerum Citation2008, Hernandez-Cortez et al. 2012). In the present study, the median migration of the uncemented Elektra cups during the first 2 years was comparable to the migration of cemented DLC cups. Our final patient numbers were smaller than what we had sampled for, and the measured difference between groups was also small; thus, the study carries the risk of type-II error. Only 1 very experienced surgeon operated the patients, and our results can be generalized only to implants inserted by experienced surgeons. Our RSA setup is standard in most other RSA laboratories and should be reproducible elsewhere based on our methodological descriptions.
Continuous implant migration and an appreciable amount of early implant migration have been predictive of longer-term implant failure of hip and knee prostheses (Kärrholm et al. Citation1994, Ryd et al. Citation1995, Nelissen et al. Citation2011). Measurements of implant migration during the first 2 years after surgery have validated RSA as a surrogate outcome measure of implant survival (Kärrholm et al. Citation1994, Ryd et al. Citation1995, Pijls et al. Citation2012a,Citationb). Due to the high precision of the method, a relatively low number of subjects is needed, e.g. 15–25 patients in each group in randomized studies (Valstar et al. Citation2005). Migration analysis with small implants in limited anatomic spaces (e.g. carpal bones) is less precise than with hip or knee implants (Valstar et al. Citation2005, Hansen et al. Citation2010). The condition number indicates the spatial limitations and a practical upper limit of 150 has been recommended (Valstar et al. Citation2005), but higher numbers have been used (Ryd et al. Citation2000). An increasing condition number indicates that the marker configuration approaches that of a straight line, which may have any direction, and the condition number has been shown to explain as much as 92% of the variation in overall rotation (Ryd et al. Citation2000). The accuracy of the rotation about the axis parallel to this “almost” straight line is poor (Ryd et al. Citation2000, Hansen et al. Citation2010); thus, we did not evaluate rotations.
In addition, the model-based RSA technique has its limitations in symmetrical implants, such as the Elektra screw cup, and makes rotational analysis about the symmetrical axis impossible. Based on double examinations, the precision of the translational measurements was acceptable and in the range of 0.4 mm along any axis or 0.6 mm in total translation, which is far better than the visual assessment of trapezium implant migration by conventional radiography. As with femoral stems in total hip arthoplasty, a clinically important measure for trapezium cups is subsidence. Most of the cups subsided (), but for the polyethylene cup, the values were below the precision limit () and we found no statistically significant difference between the groups. In both groups, we found that the implant was well-fixed without progressive/continuous migration during the total observation period, which indicates good long-term survival for both groups.
As this is the first RSA study on TMC joint implants, there are no recommendations for data dichotomy or a cutoff migration level above which the implants are likely to be loose (Aspenberg et al. Citation2008). We must therefore rely on the shape of the migration curves flattening out to illustrate implant fixation. The implants are different in both design and materials, but also concerning the method of bone fixation. Our data suggest that a migration of below 1 mm would be an acceptable cutoff for loose implants. Klahn et al. (Citation2012) recently published findings of progressive aseptic loosening of the Elektra cup after more than 2 years, but they used threading of the bone before insertion of the cup. In line with this, we found that 1 Elektra screw cup loosened symptomatically at 2 years. Based on a methodological study (Hansen et al. Citation2011), we found equally good fixation of cemented cups and screw cups inserted without threading of the bone, and we therefore hope that we will not encounter similar medium-term problems in our series. Also, based on our experimental results with press-fit fixation of Elektra screw cups (Hansen et al. Citation2011), we believe that it would be unethical to perform a clinical randomized study to test the implant fixation of Elektra implants inserted into threaded or non-threaded trapezium bone, as we expect that bone preparation by threading would increase the risk of implant failure. We will, however, follow the patients in our study—both clinically and with RSA—to exploit the expected clinical advantage of the non-threading surgical technique. We consider the cemented cup to be the “gold standard” of primary fixation since it has the longest track record on the market, even though the long-term results have not been good in all of the series published.
In conclusion, we have found comparably good fixation of the cemented all-polyethylene trapezium cup and uncemented Elektra screw cup. For practical reasons and due to anatomical limitations, RSA is challenging with small implants; however, and even though our learning curve with RSA for TM joint implants was included as part of this study, we found an acceptable clinical precision of a maximum of 0.4 mm translation along any axis, which is much better than the visual judgement of trapezium cup migration on conventional radiographs. We recommend that RSA be used as a standard safety parameter in the phased introduction of trapezium implants, as has been recommended for total knee implants (Nelissen et al. Citation2011). We did not prepare the trapezium bone by threading before insertion of the cup. Compared with the reported failures (Hansen and Snerum Citation2008, Hernandez-Cortez et al. 2012, Klahn et al. Citation2012), we expect that this may prevent early failure and improve primary fixation to the stability level of cemented DLC cups. However, further studies are needed to investigate the long-term survival of the uncemented Elektra trapezium cup and the potential benefits of alleviating bone threading. Also, the effect of metal-on-metal articulation of this implant should be investigated further.
TBH: design, data collection, and analysis. MS: design and data analysis. Both authors prepared the manuscript.
We thank Niels Trolle Andersen of the Department of Biostatistics, University of Aarhus, Denmark, for his highly valued statistical advice and comments during the final preparation of this paper.
No competing interests declared.
- Aspenberg P, Wagner P, Nilsson KG, Ranstam J. Fixed or loose? Dochotomy in RSA data for cemented cups. Acta Orthop 2008;79(4): 467-73.
- Braun RM. Total joint replacement at the base of the thumb – preliminary report. J Hand Surg Am 1982;7:245-51
- Bryant D, Havey TC, Roberts R, Guyatt G. How many patients? How many limbs? Analysis of patients or limbs in the orthopaedic literature: A systematic review. J Bone Joint Surg (Am) 2006;88(1): 41-5.
- Cooney WP, Chao EY. Biomechanical analysis of static forces in the thumb during hand function. J Bone Joint Surg (Am) 1977;59:27-36
- Cooney WP, Linscheid RP, Askew LJ. Total arthroplasty of the thumb trapeziometacarpal joint. Clin Orthop 1987;220:35-45
- de la Caffiniere JY, Aucouturier P. Trapezio-metacarpal arthroplasty by total prosthesis. Hand 1979;11:41-6
- Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin 1987;3:455-71
- Hansen TB. Elektra TM. Total joint prosthesis. In: Wrist and Hand Joint Replacements. FESSH Instructional Course 2011 (Ed Magne Røkkum).
- Hansen TB, Homilius M. Failed total carpometacarpal joint prosthesis of the thumb: results after resection arthroplasty. Scand J Plast Reconstr Surg Hand Surg 2010;44:171-4
- Hansen TB, Vainorius D. High loosening rate of the Moje Acamo prosthesis for treating osteoarthritis of the trapeziometacarpal joint. J Hand Surg Eur 2008;33:571-4
- Hansen TB, Snerum L. Elektra trapeziometacarpal prosthesis for treatment of osteoarthrosis of the basal joint of the thumb. Scand J Plastic Reconstr Hand Surg 2008;42:316-19
- Hansen TB, Larsen K, Bjergelund L, Stilling M. Trapeziometacarpal joint implants can be evaluated by roentgen stereophotogrammetric analysis. J Hand Surg Eur 2010;35:480-5
- Hansen TB, Meier M, Møller MC, . Primary cup fixation with different designs of trapeziometacarpal total joint trapezium components: a radiostereometric analysis in a pig bone model. J Hand Surg Eur 2011;36:285-90
- Hansen TB, Sørensen OG, Kirkeby L, . Computed tomography improves intra-observer reliability, but not the inter-observer reliability of the Eaton-Glickel classification. J Hand Surg Eur 2012, Epub ahead of print
- Hernández-Cortés P, Pajares-López M, Robles-Molina MJ, . Two-year outcomes of Elektra prosthesis for trapeziometacarpal osteoarthritis: a longitudinal cohort study. J Hand Surg Eur 2012;37:130-7
- Kaptein BL, Valstar ER, Stoel BC, . A new model-based RSA method validated using CAD models and models from reversed engineering. J Biomech 2003;36:873-82
- Klahn A, Nygaard M, Gvozdenovic R, Boeckstyns M EH. Elektra prosthesis for trapeziometacarpal osteoarthritis: a follow-up of 39 consecutive cases. J Hand Surg Eur 2012; Epub ahead of print
- Kärrholm J, Borssén B, Löwenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994;76:912-7.
- Nelissen RG, Pijls BG, Kärrholm J, . RSA and registries: the quest for phased introduction of new implants. J Bone Joint Surg (Am) (Suppl 3) 2011;21:93: 62-5.
- Perez-Ubeda MJ, Garcia-Lopez A, Martinez FM, . Results of the cemented SR trapeziometacarpal prosthesis in the treatment of thumb carpometacarpal osteoarthritis. J Hand Surg (Am) 2003;28:917-25
- Pijls BG, Nieuwenhuijse MJ, Fiocco M, . Early proximal migration of cups is associated with late revision in THA. A systematic review and meta-analysis of 26 RSA studies in 49 survival studies. Acta Orthop 2012a;83(6): 583-91.
- Pijls BG, Valstar ER, Nouta KA, . Early migration of tibial components is associated with late revision. A systematic review and meta-analysis of 21,000 knee arthroplasties. Acta Orthop 2012b;83(6): 614-24.
- Regnard PJ. Electra trapezio metacarpal prosthesis: Results of the first 100 cases. J Hand Surg Br 2006;31:621-8
- Ryd L, Albrektsson BE, Carlsson L, . Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995;77:377-83
- Ryd L, Yuan X, Löfgren H. Methods for determining the accuracy of radiostereometric analysis (RSA). Acta Orthop Scand 2000;71:403-8
- Søndergaard L, Konradsen L, Rechnagel K. Long-term follow-up of the cemented Caffiniere prosthesis for trapeziometacarpal arthroplasty. J Hand Surg Br 1991;16:428-30
- Ulrich-Vinther M, Puggaard H, Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg (Am) 2008;33:1369-77
- Wachtl SW, Guggenheim PR, Sennwald GR. Cemented and non-cemented replacement of the trapeziometacarpal joint. J Bone Joint Surg (Br) 1998;80:121-5
- Valstar ER, Gill R, Ryd L, . Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005;76:563-72
- Van Capelle H GJ, Elzenga P, van Horn JR. Long-term result and loosening analysis of de la Caffiniére replacement of the trapeziometacarpal joint. J Hand Surg (Am) 1999;24:476-82