Figures & data
Table 1. Comparison of Mandeville et al. and SUN working group clinical criteria for TINU.
Figure 1. Proposed pathogenesis of TINU. A foreign antigen, such as an infectious agent, may prime T-cells against ocular and kidney tissues with subsequent development of autoantibodies leading to continued chronic inflammation. Image created in BioRender.
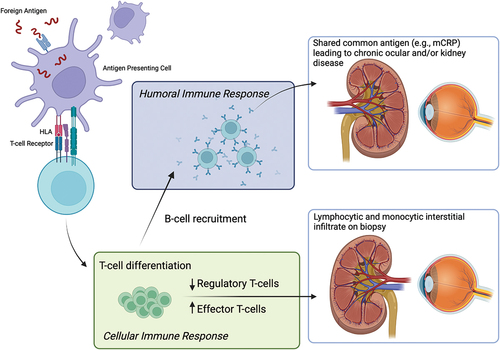
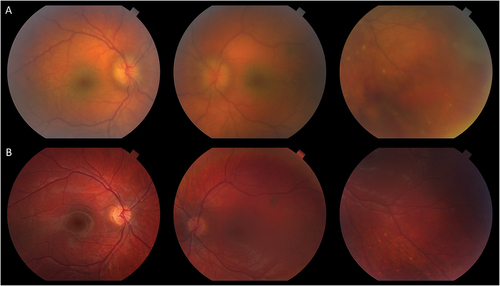
Figure 2. Choroidal inflammation in TINU. A 16-year-old male was referred after three months of bilateral anterior uveitis following a febrile illness. On first visit to the uveitis clinic, he had 2+ anterior chamber (AC) and 2+ vitreous cell with few snowballs in the right eye. Posterior examination showed areas of subtle small choroidal lesions throughout both eyes (A) with few small pigmented atrophic choroidal lesions inferiorly. ICGA demonstrated many small hypofluorescent spots throughout both eyes more prominent than seen clinically. Workup was only notable for elevated urine beta-2 microglobulin; sarcoidosis workup was unrevealing. In addition to topical prednisolone, the patient was treated with a course of oral prednisone and transitioned to adalimumab with quiescence of disease. Follow-up ICGA (B) nine months after starting adalimumab showed resolution of hypofluorescent lesions.
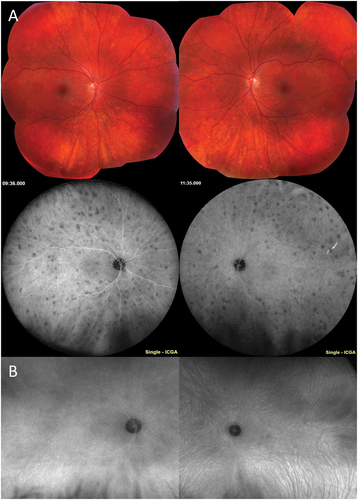
Figure 3. Retinal vascular inflammation in TINU. A 15-year-old male was referred for anterior and intermediate uveitis for six months, treated with topical prednisolone and intravitreal triamcinolone. The patient noted upper respiratory tract infection one month prior to ocular symptoms. On first visit at the uveitis clinic, the patient had 3+ anterior chamber cell and 2+ anterior vitreous cell, 1+ haze, and snowballs in both eyes. The posterior examination was notable for hyperemic optic nerves and few pigmented small choroidal lesions. Fluorescein angiography demonstrated diffuse small vessel vasculitis, angiographic cystoid macular edema, and disc leakage (A). Workup was notable for elevated urine beta-2 microglobulin. Work up for sarcoidosis (ACE, lysozyme, chest x-ray) was unremarkable. The patient was treated with a course of prednisone and transitioned to adalimumab with quiescence of inflammation and resolution of vasculitis (B).
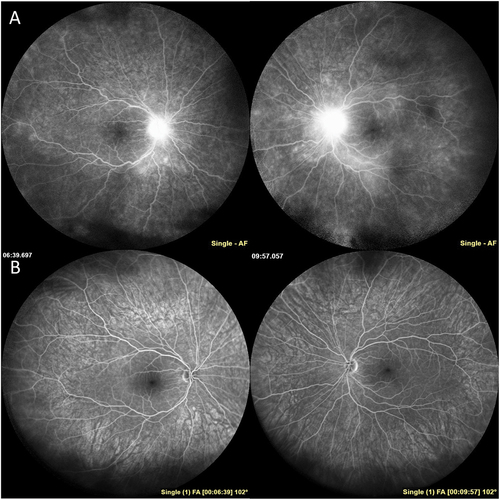
Figure 4. Inflammatory neovascularization of the disc in TINU. A 10-year-old boy was referred for anterior uveitis that developed three months after biopsy proven severe tubulointerstitial nephritis. On first examination at the uveitis clinic, the patient had 4+ anterior chamber cell, 3+ anterior vitreous cell, and 2+ haze with snowballs in both eyes. The optic nerves were edematous with fine neovascularization of both nerves (A). There were small chorioretinal lesions in the periphery of both eyes and vitreous hemorrhage in the left eye (A). The patient was treated with a course of oral prednisone and transitioned to methotrexate and adalimumab therapy with improvement in inflammation and resolution of inflammatory neovascularization and disc edema (B).