Figures & data
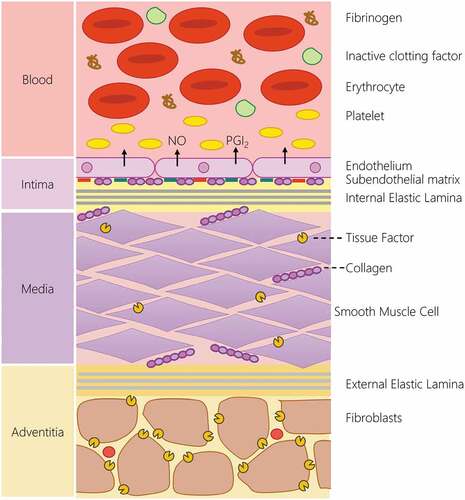
Figure 1. The structure of the blood-arterial wall interface is the key regulator of hemostatic response. In the uninjured blood vessel, the hemostatic system is kept quiescent by the physical and chemical barrier produced by the endothelial lining. The endothelial lining produces a range of endogenous inhibitors of platelets and the coagulation cascade to prevent activation of the hemostatic system. The intimal layer also physically separates blood from the pro-thrombotic constituents of the medial and adventitial layer of the artery. This includes the presence of pro-aggregatory molecules such as collagen, fibronectin and laminin in the subendothelial matrix, and the production of tissue factor by smooth muscle cells in the medial layer as well as adventitial fibroblasts. These systems help prevent the unwanted activation of the hemostatic system. In the event of vascular damage, the loss of the endothelial lining locally removes the inhibitory effect of this lining and allows blood to interact with the pro-aggregatory and pro-coagulant component of the arterial wall to initiate thrombus formation.