Figures & data
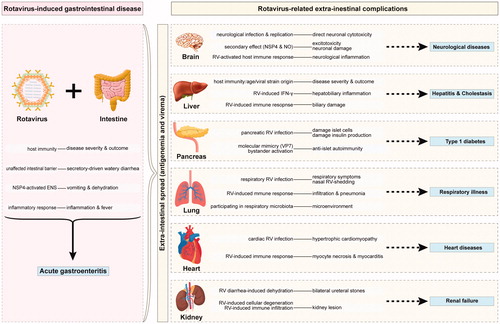
Table 1. Clinical manifestation and evidence summary of rotavirus-related systemic diseases.