Figures & data
Figure 1. Trends in the incidence of various vestibular disorders in recent years. From 2017 to 2020 [Citation2,Citation3], the central vestibular diseases have been on the rise by the year and significantly surpassed their peripheral counterparts. In order to more vividly express the changes of diseases, we make a new comparison graph according to the two data from different years. BPPV, benign paroxysmal positional vertigo.
![Figure 1. Trends in the incidence of various vestibular disorders in recent years. From 2017 to 2020 [Citation2,Citation3], the central vestibular diseases have been on the rise by the year and significantly surpassed their peripheral counterparts. In order to more vividly express the changes of diseases, we make a new comparison graph according to the two data from different years. BPPV, benign paroxysmal positional vertigo.](/cms/asset/0777fa72-c037-48ea-ba26-80b3e3f9239a/iern_a_2106129_f0001_oc.jpg)
Figure 2. Diagnosis and treatment process of vestibular rehabilitation in central vestibular disorders and vestibular dysfunction. The diagnosis of central vestibular diseases mainly included history, assessment of vestibular function, psychophysiological, risk assessment and so on. Etiological therapy, symptomatic treatment, personalized rehabilitation especially VOR suppression, Memory VOR, Anti-Saccade, Memory saccades play the leading role. VOR, Vestibulo-Ocular Reflex; DHI, Dizziness Handicap Inventory; Hads, Hospital Anxiety Depression Scales; ABC, Activity-specific Balance Confidence Scale; SSS, Somatic Self-rating Scale.
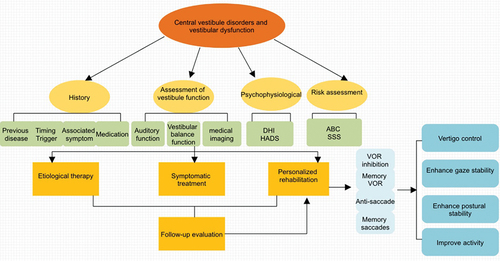
Figure 3. The treatment mechanism of vestibular migraine. Pathogenesis of vestibular migraine (VM) is still poorly understood and researchers fail to agree regarding whether its origin is predominantly central or peripheral. The factors involved in the pathogenesis of VM do not work separately but are intricately interwoven. Treatment options for VM patients include reducing or removing triggering factors, medications, physical rehabilitation therapies, and treatment of comorbidities.
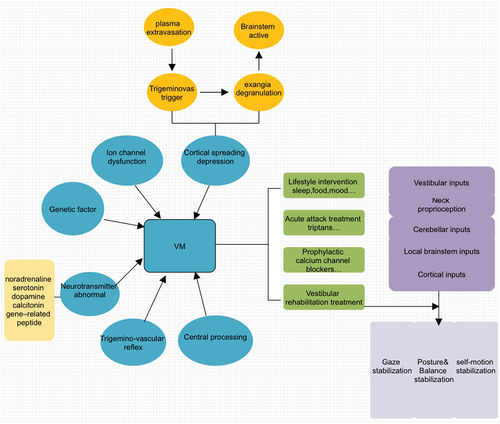
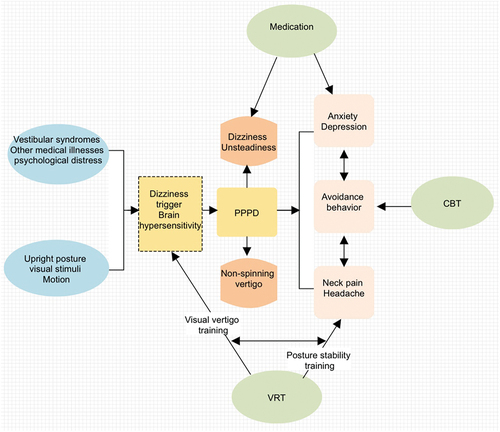
Figure 4. The brief introduction of PPPD. Affected individuals of PPPD feel worst when upright, exposed to moving or complex visual stimuli, and during active or passive head motion. These situations may not be equally provocative. Ingredients of treatment include (a) A clear positive diagnosis and explanation that you can work with; (b) Recognition during assessment of all the various component symptoms that may or may not be going along with your PPPD; (c) Physiotherapy/Desensitization of movement such as VRT. PPPD, persistent postural-perceptual dizziness; VRT, vestibular rehabilitation treatment; CBT, cognitive-behavioral therapy.