Figures & data
Figure 1. Service pathway for the HabITec Lab. PWD = person with disability; ESM = scheduling and reporting system; MDT = multidisciplinary team. [image re-used with permission from the Hopkins Centre].
Overview of the HabITec Lab service pathway for a patient in the hospital to their home. A person wanting to explore technology is referred and can receive a quick response, or complex prescribing which involves specialist assessment, intervention, and outreach to the home.
The HabITec Lab service pathway for a patient in the hospital to their home consists of 2 main stages. First, a person wanting to explore technology is referred to The HabITec and is triaged to receive a quick response, or complex prescribing. A quick response appointment consists of education and/or link to other services. Complex prescribing involves specialist assessment (including goal setting, planning and outcome measures), intervention (assess existing technology use and need for bespoke solution, determine learning and training needs, provision and adjustment of technology-based solutions), and outreach to the home (including education and training around existing technologies, co-creation of bespoke solutions, linking to other services, and education).
![Figure 1. Service pathway for the HabITec Lab. PWD = person with disability; ESM = scheduling and reporting system; MDT = multidisciplinary team. [image re-used with permission from the Hopkins Centre].Overview of the HabITec Lab service pathway for a patient in the hospital to their home. A person wanting to explore technology is referred and can receive a quick response, or complex prescribing which involves specialist assessment, intervention, and outreach to the home.The HabITec Lab service pathway for a patient in the hospital to their home consists of 2 main stages. First, a person wanting to explore technology is referred to The HabITec and is triaged to receive a quick response, or complex prescribing. A quick response appointment consists of education and/or link to other services. Complex prescribing involves specialist assessment (including goal setting, planning and outcome measures), intervention (assess existing technology use and need for bespoke solution, determine learning and training needs, provision and adjustment of technology-based solutions), and outreach to the home (including education and training around existing technologies, co-creation of bespoke solutions, linking to other services, and education).](/cms/asset/3493f9ed-083a-4c9a-aa3e-950004c75e52/iidt_a_2244001_f0001_c.jpg)
Figure 2. Referral and administrative data for all 25 participants. SCI: spinal cord injury, TBI: traumatic brain injury, MCA: middle cerebral artery stroke, OT: occupational therapist, PT: physiotherapist, LT: leisure therapist.
Bar graphs indicating 9 participant demographic and referral characteristics: gender, diagnosis, date of injury, postcode, in/outpatient status, employment history, employment status, living situation and referring discipline.
Bar graphs indicating 9 demographic and referral characteristics of the 25 participants. Gender: 22 participants were male, 3 were female. Diagnosis: 23 participants had an SCI, 1 had a TBI, 1 had a stroke. Date of injury: 4 were before 2019, 21 were on or after 2019. Postcode: 18 participants were from metropolitan areas, 6 from regional or rural areas, and 1 interstate. In/outpatient status: 20 were inpatients, 5 were outpatients. Employment history: 18 participants were employed at the time of injury, 3 were unemployed, and 4 were retired. Employment status: 3 participants were unemployed at the time of attending The HabITec Lab, 22 were unemployed. Living situation: 18 participants lived with family and 7 lived alone. Referring discipline: 19 participants were referred by occupational therapy, 3 by vocational rehabilitation, 1 by physiotherapy, 1 by leisure therapist and 1 was self-referred.
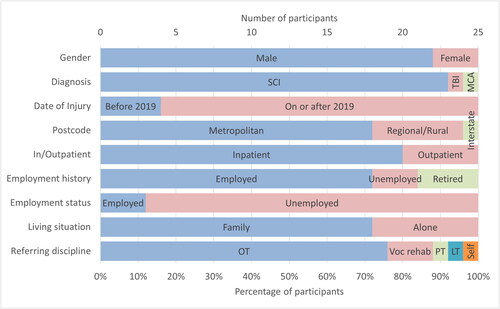
Figure 3. Number of individuals that received each type of intervention by in/outpatient setting.
Bar plots of the total number of intervention sessions per intervention type and participant’s inpatient/outpatient status. Inpatient repetitive practice was by far the most common session.
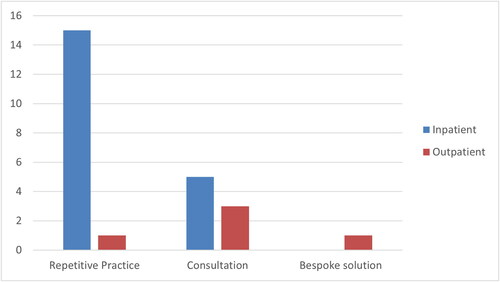
Table 1. Goals identified by the 25 individuals that attended the HabITec Lab: number by types of goals, with examples.
Figure 4. Referral and administrative data for participants that completed MGAMs pre- and post-intervention.
Bar graphs indicating 9 participant demographic and referral characteristics: gender, diagnosis, date of injury, postcode, in/outpatient status, employment history, employment status, living situation and referring discipline.
Bar graphs indicating 9 demographic and referral characteristics of the 12 participants. Gender: 75% of participants were male. Diagnosis: 11 participants had an SCI, 1 had a stroke. Date of injury: all incidents were on or after 2019. Postcode: 7 participants were from metropolitan areas, 4 from regional or rural areas, and 1 interstate. In/outpatient status: 11 were inpatients. Employment history: 7 participants were employed at the time of injury, 1 was unemployed, 4 were retired. Employment status: all participants were unemployed at the time of attending The HabITec Lab. Living situation: 9 participants lived with family and 3 lived alone. Referring discipline: 11 participants were referred by occupational therapists, 1 by leisure therapist.
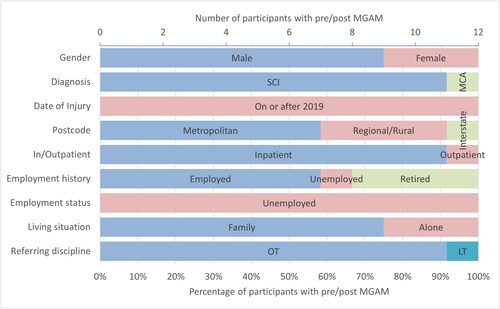
Figure 5. MGAM scores pre (Left) and post (right) attending the HabITec Lab for: (a) performance and (b) satisfaction. Scores within individual are connected by lines.
Individual scores and across-participant descriptive statistics boxplots of MGAM Performance scores pre and post attending the HabITec Lab. All individuals scores increased.
Individual scores and across-participant descriptive statistics boxplots of MGAM Satisfaction scores pre and post attending the HabITec Lab. All individuals scores increased.
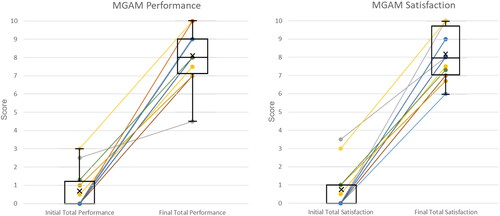
Table 2. Demographic information of the 12 interview participants.
