Figures & data
Figure 1. Severe malaria pathogenesis: Both host and parasite factors contribute to the pathogenesis of severe malaria (SM). Key mechanisms include, sequestration of infected erythrocytes in the microvasculature of vital organs, hemolysis, inflammation, coagulopathy, endothelial activation, and microvascular injury. Each of these mechanisms may amplify another, leading to multi-organ failure and death.
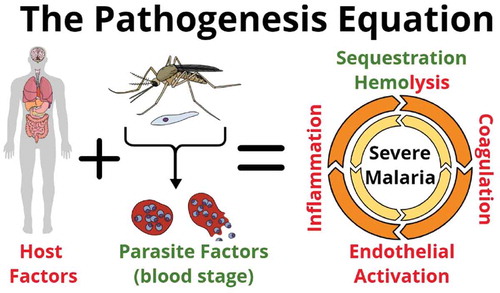
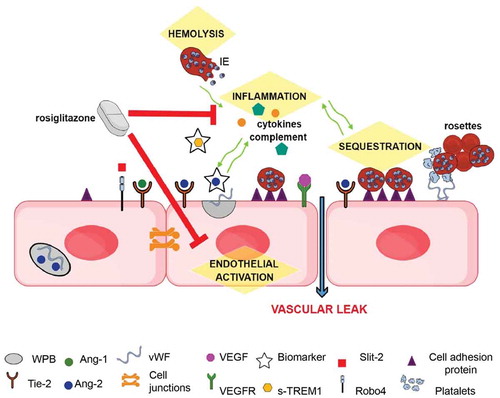
Figure 2. Schematic of mechanisms underlying SM pathology that represent potential sites for therapeutic intervention (highlighted in yellow): During quiescence, Ang-1 via Tie-2, and possibly Slit-2 via Robo4, promote endothelial integrity by stabilizing junctional proteins. During severe infections Weibel-Palade bodies (WPB) in the endothelial cell, stimulated by inflammatory responses, release Ang-2 and vWF. Ang-2 displaces Ang-1 and inhibits Tie-2 endothelial stabilizing effects. The expression of cell adhesion molecules, such as ICAM-1, are increased, leading to enhanced sequestration, and vWF released from WPB, promoting a pro-coagulatory state. These pathological mechanisms may interact and exacerbate each other (green arrows), leading to microvascular dysfunction. Circulating levels of Ang-2 and sTREM-1 are good prognostic markers of disease severity and outcome. Rosiglitazone is a promising putative adjunctive therapeutic as it acts upon several of the pathological mechanisms linked to the development of SM.