Figures & data
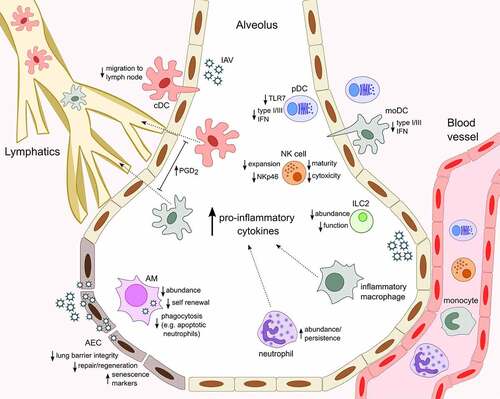
Figure 1. Age-associated changes in innate immune cell response to influenza infection.The heightened baseline inflammatory environment that corresponds with aging (inflammaging) influences innate immune cell responses, typically manifesting as altered activity and abundance within the infected lung and resulting in less efficient resolution and recovery from IAV infection in older organisms. With increased age, alveolar epithelial cells (AEC) appear more senescent, regenerate slower and secrete increased levels neutrophil-attracting chemokines upon IAV infection. AM are less numerous, poorly phagocytic and produce higher levels of CXCL8, favoring further recruitment and persistence of neutrophils in the airways. Similarly, elevated levels of CCL2 in the infected lungs facilitate increased entry of monocyte-derived Ly6Chi inflammatory macrophages from the circulation. Respiratory conventional and monocyte-derived dendritic cells (cDC and moDC) secrete cytokines in the lung and traffic antigen to draining lymph nodes via the lymphatics. Elevated levels of prostaglandin D2 (PGD2) in aged mice contributes to impaired cDC migration to the lymph node and T cell responses and moDC have an age-associated defect in type I and III IFN production. pDC display a similar defect in IFN production, which correlates with reduced expression of TLR7, a sensor of viral ssRNA. Aging is linked to reduced NK cell terminal differentiation, expansion, cytotoxicity and NKp46-mediated recognition of IAV-infected cells and fewer type 2 innate lymphoid cells (ILC2) populate the lungs in aged mice and are functionally impaired. In the context of IAV infection, ILC2 respond to the damage-associated molecular pattern IL-33 and can support lung tissue integrity, remodeling and repair
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
