Figures & data
Figure 1. Difference of viral cell entry between SARS-CoV-2 and influenza a virus.
The SARS-CoV-2 invade host cell via two pathways, the first form is endosomal entry (A). The virus uses the receptor binding domain (RBD) on S1 to bind to ACE2 with S1 “up” conformation, then internalized into infected cell. During endosome trafficking, viral S protein is cleaved at the S2ʹ site by cathepsin L, a furin-like proprotein convertase, and then uncoated viral RNA can be released into host cell. The second form is cell surface entry (B), SARS-CoV-2 bind with TMPRSS2 and ACE2 together, then TMPRSS2 activates the S protein for membrane fusion. Different to SARS-CoV-2, influenza A virus does not need the assistance of ACE2 or TMPRSS2 for cell entry. It infect host cell through receptor-mediated cell entry (C), which use RBD of HA on viral surface to connect with α2,6 sialic acid. Endocytosis occur and the following membrane fusion will be triggered in the acidic environment of endosomes.
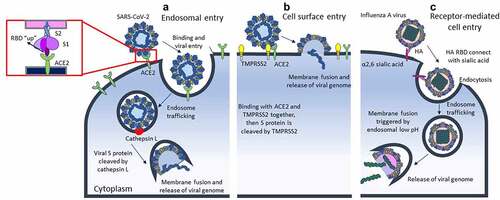
Table 1. Comparison between different respiratory viruses.
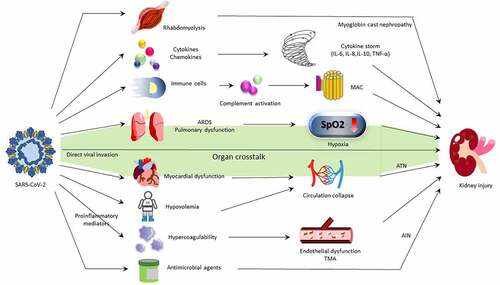
Figure 2. Mechanism of COVID-19-associated AKI.
AKI in COVID-19 patients is supposed to be multifocal; it may be caused by immune system dysregulation or complement activation, similar to other respiratory virus infection. Rhabdomyolysis occurs in several virus infection with severe illness, and the obstruction of renal tubules by myoglobin casts can also induce AKI. Proinflammatory mediators enhance blood coagulation and result in endothelial dysfunction or even thrombotic microangiopathy (TMA). Erythrocyte aggregates may induce obstruction of the capillary lumen and ischemic injury in the kidneys. Severe COVID-19 patients usually receive broad-spectrum antibiotics during acute-phase infection, so drug-induced acute interstitial nephritis should also be considered. SARS-CoV-2 infection can cause both pulmonary and myocardial dysfunction, and AKI may occur through these pathways of organ crosstalk. Finally, SARS-CoV-2 is found to have direct viral invasion to kidney, a unique pathophysiology of renal damage. There is no evidence that other respiratory virus has the same ability.