Figures & data
Table 1. Baseline characteristics of included studies.
Figure 1. Combined analysis of HR of high versus low tumor mutation burden for OS in various cancer patients treated with or without immunotherapy, and immunotherapy versus chemotherapy in cancer patients with high tumor mutation burden. (a): Above, pooled HR for patients treated with immunotherapy. High tumor mutation burden is in favor of improved OS (n = 620, p< .01); Below, Pooled HR for patients without immunotherapy. High tumor mutation burden is associated with increased risk of death in these patients (n = 3286, p= .14). (b): Evaluating effects of immunotherapy versus chemotherapy on OS in cancer patients with high tumor mutation burden. OS was improved for patients from the immunotherapy group, compared to those in the chemotherapy group (n = 1462, p= .07).
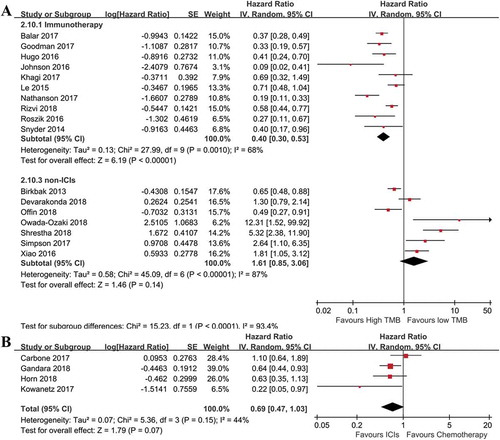
Figure 2. Subgroup analyses of factors that may affect the pooled HR for OS. (a): Subgroup analysis of OS in term of cancer types. The prognostic role of tumor mutation burden was independent of cancer types (n = 196 for melanoma, n = 240 for NSCLC, n = 1484 for multiple cancers. overall p< .01). (b): Subgroup analysis of OS with regard to detection methods of tumor mutation burden. The prognostic role of tumor mutation burden was independent of detection methods (p< .01).
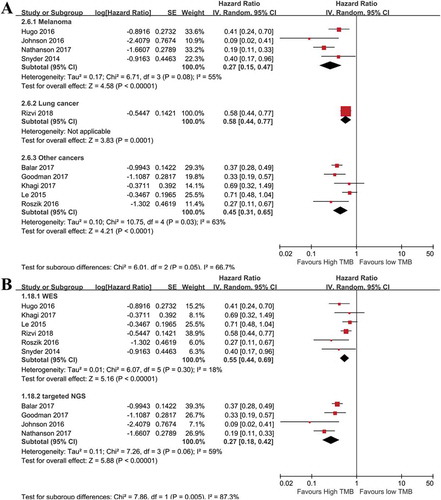
Figure 3. Combined analysis of HR of high versus low tumor mutation burden for PFS in various cancer patients treated with or without immunotherapy, and immunotherapy versus chemotherapy in cancer patients with high tumor mutation burden. (a): pooled HR of high versus low tumor mutation burden for patients treated with immunotherapy or not. High tumor mutation burden is in favor of improved OS (n = 440 for immunotherapy, p< .01), but associated with worse outcomes for patients treated without immunotherapy (n = 3480 for non-immunotherapy, p= .01). (b): Evaluating the effects of immunotherapy versus chemotherapy on PFS in cancer patients with high tumor mutation burden. PFS was significantly prolonged in patients receiving immunotherapy, compared to those with chemotherapy (n = 2078, p< .01).
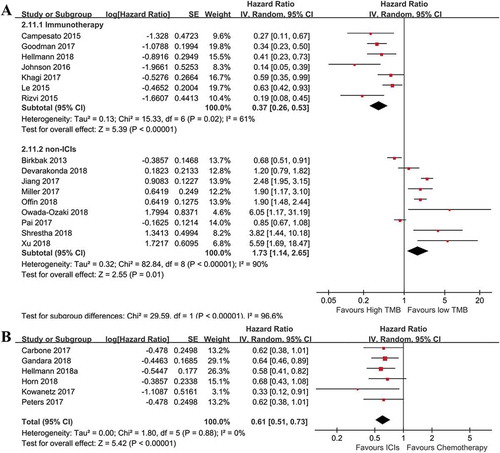
Figure 4. Subgroup analyses of PFS with regard to cancer types, and tumor mutation burden detection methods. (a): Subgroup analysis of OS in term of cancer types. The prognostic role of tumor mutation burden was similar in enrolled cancer types (n = 65 for melanoma, n = 2442 for NSCLC, n = 261 for multiple cancers. overall p< .01). (b): Subgroup analysis of PFS using different detection methods of tumor mutation burden. The prognostic role of tumor mutation burden was not significantly affected by detection methods (p< .05).
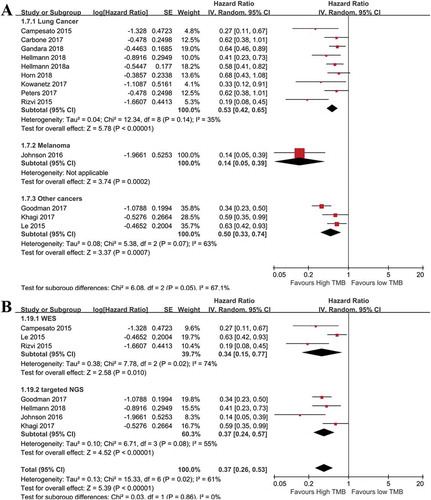
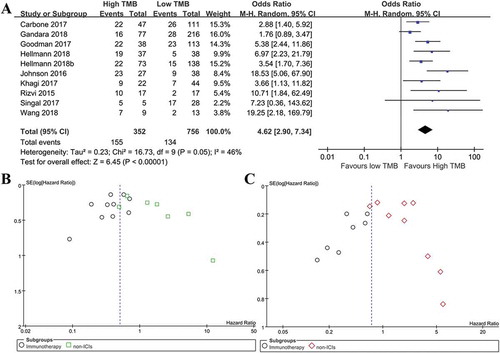
Figure 5. Meta-analysis of overall response rate in immunotherapy treated patients with high versus low tumor mutation burden, and publication bias assessment. (a): Meta-analysis of overall response rate in cancer patients with high versus low tumor mutation burden after immunotherapy (N = 1108, p< .01). (b): Funnel plot of OS from included studies. (c): Funnel plot of PFS from included studies.