Figures & data
Table 1. Diagnosis of asthma.
Figure 1. Diagnosis algorithm for children 1 to 5 years of age.
aDocumentation by a physician or trained health care practitioner.bEpisodes of wheezing with/without difficulty breathing.cSeverity of an exacerbation documented by clinical assessment of signs of airflow obstruction, preferably with the addition of objective measures such oxygen saturation and respiratory rate, and/or validated score such as the Pediatric Respiratory Assessment Measure (PRAM) score.dBased on marked improvement in signs of airflow obstruction before and after therapy or a reduction of ≥ 3 points on the PRAM score, recognizing the expected time response to therapy.eA conclusive therapeutic trial hinges on adequate dose of asthma medication, adequate inhalation technique, diligent documentation of the signs and/or symptoms, and timely medical reassessment; if these conditions are not met, consider repeating the treatment or therapeutic trial.fThe diagnosis of asthma is based on recurrent (≥ 2) episodes of asthma-like exacerbations (documented signs) and/or symptoms. In case of a first occurrence of exacerbation with no previous asthma-like symptoms, the diagnostic of asthma is suspected and can be confirmed with re-occurrence of asthma-like symptoms or exacerbations with response to asthma therapy.g>8 days/month with asthma-like symptoms.hSevere exacerbations require any of the following: systemic steroids, hospitalization; or an emergency department visit.IIn this age group, the diagnostic accuracy of parental report of a short-term response to as-needed short-acting β2-agonist (SABA) may be unreliable due to misperception and/or spontaneous improvement of another condition. Documentation of airflow obstruction and reversibility when symptomatic, by a physician or trained health care practitioner, is preferred.jBased on 50% fewer severe exacerbations, shorter and milder exacerbations, and fewer, milder symptoms between episodes.
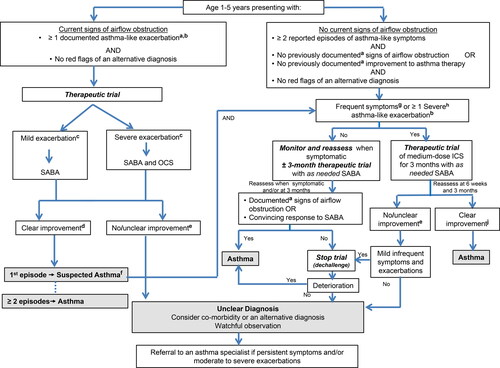
Figure 2. 2021 Asthma continuum.
Management relies on an accurate diagnosis of asthma and regular reassessment of control and risk of exacerbation. All individuals with asthma should be provided with self-management education, including a written action plan. Adherence to treatment, inhaler technique, exposure to environmental triggers, and the presence of comorbidities should be reassessed at each visit and optimized.
Individuals with well controlled asthma on no medication or PRN SABA at lower risk of exacerbation can use PRN SABA, daily ICS + PRN SABA, and if ≥ 12 years of age PRN bud/form*.
Individuals at higher risk of exacerbation even if well-controlled on PRN SABA or no medication, and those with poorly-controlled asthma on PRN SABA or no medication should be started on daily ICS + PRN SABA. In individuals ≥ 12 years old with poor adherence despite substantial asthma education and support, PRN bud/form* can be considered. LTRA are second-line monotherapy for asthma. If asthma is not adequately controlled by daily low doses of ICS with good technique and adherence, additional therapy should be considered. In children 1-11 years old, ICS should be increased to medium dose and if still not controlled in children 6-11 years old, the addition of a LABA or LTRA should be considered. In individuals 12 years of age and over, a LABA in the same inhaler as an ICS is first line adjunct therapy. If still not controlled, the addition of a LTRA or tiotropium should be considered.
In children who are not well-controlled on medium dose ICS, a referral to an asthma specialist is recommended. After achieving asthma control, including no severe exacerbations, for at least 3-6 months, medication should be reduced to the minimum necessary dose to maintain asthma control and prevent future exacerbations.
HFA, hydrofluoroalkane; SABA, short-acting beta-agonist, LABA, long-acting beta-agonist, ICS, inhaled corticosteroid, LTRA, leukotriene receptor antagonist, bud/form: budesonide-formoterol in a single inhaler
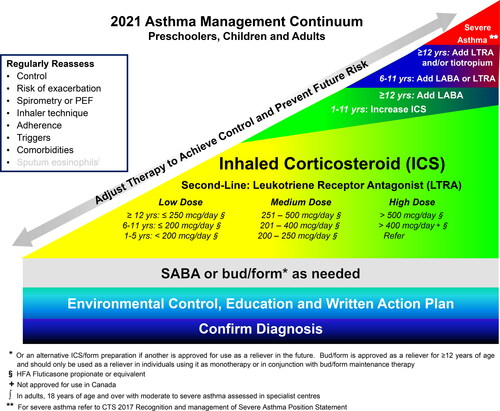
Table 2. Well-controlled asthma criteria.
Table 3. Assessing risk for severe exacerbation.
Table 4. Risk factors associated with severe asthma exacerbations.
Table 5. Risk factors associated with near-fatal or fatal asthma.Citation 19 ,Citation 20
Table 6. Components of an asthma education program.
Table 7. Recommendations for asthma devices by age.Citation 37
Table 8. Comparative inhaled corticosteroids (ICS) dosing categories in preschoolers, children and adults.
Table 9. Yellow Zone action plan recommendations based on age and maintenance controller therapy.
Table 10. Severity classification.

