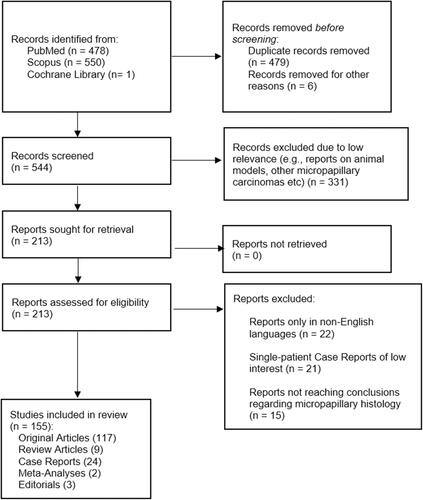
Figures & data
Figure 1 (A–D) In low magnification, through an atrophic mammary gland a neoplastic population is recognized, infiltrating the remaining ducts (A). The cells are organized in clusters, forming small-sized glandular structures and nests, arranged in a micropapillary pattern (B). Occasionally, a small proportion of them acquire a central lumina. Fibrovascular cores are absent. (C) The neoplastic cells have a moderate amount of eosinophilic cytoplasm and small round nuclei with condensed chromatin and intermediate pleomorphism. (D). In another slide of this lesion, a lymphovascular emboli is recognized (D). The morphology is highly suggestive of invasive micropapillary carcinoma, so immunohistochemical markers are performed to establish the diagnosis.
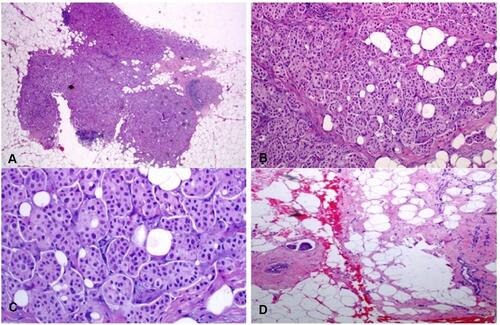
Table 1 Data on Tumor Size, Tumor Grade, Nodal Status and LVI from Included Studies
Table 2 Data on Hormone Receptor and HER-2 Status of IMPC Patients from Included Studies
Figure 3 (A) Preoperative and pre-treatment MRI image of IMPC. White arrow indicates the central mass of the lesion along with mass and non-mass enhancement. (B) MRI findings post-PST consistent with complete pathologic response. White arrow indicates local scarring in the mass area after PST. Although imaging indicated complete pathological response, residual disease was still found in the scarring area when examined under a microscope, and complete mastectomy was deemed appropriate.
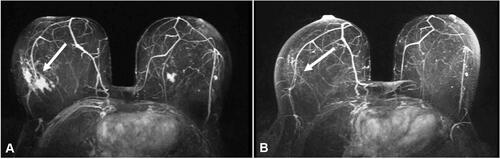
Table 3 Data on Local Recurrence, Distant Metastasis, and Survival from the Included Studies