Figures & data
Figure 1 Immune evasion or immunosuppressive strategies used by tumor cells.
Notes: Tumors use numerous strategies to evade immune responses.Citation18–Citation23 (A) Cancer cells can downregulate expression of MHC molecules that present tumor antigens to T-cells, and suppress tumor antigen presentation by professional APC, thereby avoiding recognition by T-cells. (B) Tumors create an immunosuppressive environment by recruitment and retention of suppressive Tregs and MDSCs, or (C) by secretion of immune-regulating or suppressive cytokines (IL-4, IL-5, IL-6, IL-10, and IL-13 and transforming growth factor-beta) and mediators (prostaglandins, indoleamine 2,3-dioxygenase. (D) Dysregulation of T-cell checkpoint pathways, including expression of PD-L1 by tumors, sends negative signals to tumor-specific T cells, causing T cell inactivation.
Abbreviations: APC, antigen-presenting cells; IL, interleukin; MDSCs, myeloid-derived suppressor cells; MHC, major histocompatibility complex; Tregs, T-regulatory cells.
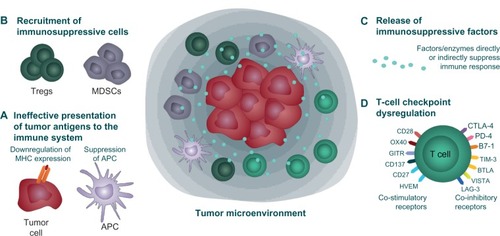
Figure 2 Targeted therapy approaches in NSCLC. Targeted therapies work by inactivating proteins essential for tumor growth and survival. Both EGF receptor tyrosine kinase and ALK can be mutated and overactive in some patients with NSCLC, although not typically in the same patients. Erlotinib and afatinib inhibit the tyrosine kinase on the intracellular region of the EGF receptor and prevent growth signaling. Crizotinib inhibits the kinase activity of ALK, located in the cell cytoplasm, to prevent growth signaling. Bevacizumab binds and inactivates vascular endothelial growth factor (VEGF) secreted by the tumor into the intracellular space, thereby limiting blood vessel formation to the tumor.
Abbreviations: ALK, anaplastic lymphoma kinase; EGF, epidermal growth factor; NSCLC, non-small cell lung cancer.
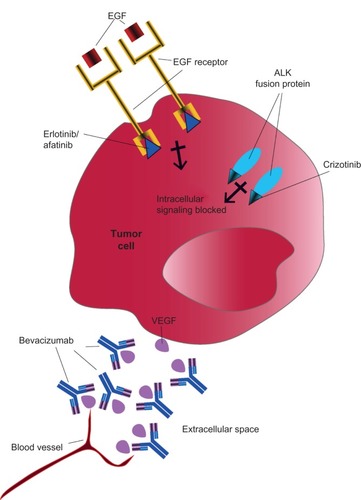
Table 1 Clinical results of ipilimumab in combination with chemotherapy in patients with chemotherapy-naïve advanced (stage 3b or 4) NSCLC
Figure 3 Concept of immunotherapy in NSCLC. (A) APCs display tumor antigens and B7 (CD80/CD86) molecules to CD8+ T-cells. CTLA-4 and CD28 are expressed on T-cells and compete for binding to B7. CTLA-4 has a higher affinity for B7 and CTLA-4:B7 binding leads to T-cell deactivation. (B) Anti-CTLA-4 antibodies prevent CTLA-4:B7 binding and allow CD28:B7 binding leading to T-cell activation. (C) Binding of PD-1 on T-cells to PD-L1 (or PD-L2; not depicted) on tumor cells causes T-cell deactivation. (D) Anti-PD-1 antibodies (or anti-PD-L1 antibodies, not shown) prevent PD-1:PD-L1 binding and restore T-cell activation and killing of tumor cells via release of cytolytic molecules.
Abbreviations: APCs, antigen-presenting cells; MHC, major histocompatibility complex; NSCLC, non-small cell lung cancer; CTLA4, cytotoxic T-lymphocyte-associated antigen-4.
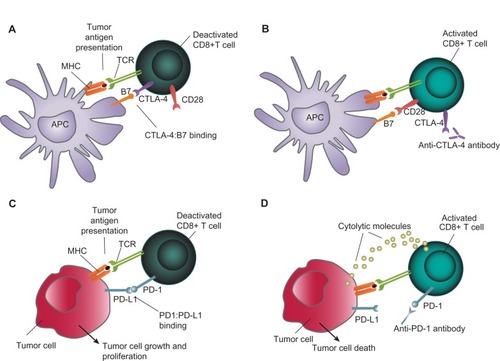
Table 2 Initial Phase I efficacy results for nivolumab monotherapy in evaluable patients with NSCLC
Table 3 Examples of select adverse events reported with immune checkpoint inhibitorsCitation12,Citation13,Citation25,Citation62,Citation65,Citation72,Citation73,Citation75,Citation76,Citation85,Citation86
