Figures & data
Table 1 Characteristics and results of pulmonary function test and arterial blood gas analysis in healthy elderly subjects (control group) and chronic lung disease patients with ventilatory disturbance with and without NOD (NOD group and non-NOD group, respectively), and who have been treated with LTOT (LTOT group)
Table 2 Results of nocturnal respiratory events, oxygen desaturation, and autonomic nerve function in healthy elderly subjects (control) and chronic lung disease patients with ventilatory disturbance with and without NOD (NOD group and non-NOD group, respectively), and who have been treated with LTOT (LTOT group)
Figure 1 Comparison of sympathetic (A) and parasympathetic (B) activity among healthy elderly subjects (control), CLD patients with NOD and without NOD (non-NOD), and CLD patients treated with LTOT.
Note: **P<0.01 vs control.
Abbreviations: LF, low frequency; HF, high frequency; LF/HF ratio, an index of sympathetic nerve activity; HF amplitude, an index of parasympathetic nerve activity; NOD, nocturnal oxygen desaturation; LTOT, long-term oxygen therapy; CLD, chronic lung disease.
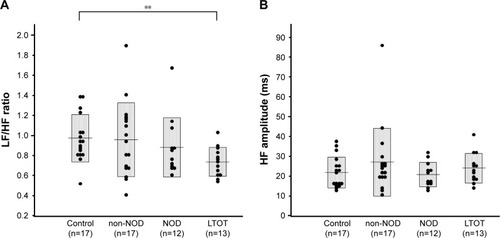
Figure 2 Comparison of indexes of stability of parasympathetic nerve function, %HF20sec (A) and %HF5min (B), among healthy elderly subjects (control), CLD patients with NOD and without NOD (non-NOD), and CLD patients treated with LTOT.
Notes: **P<0.01 vs control; ##P<0.01 vs non-NOD; §§P<0.01 vs NOD.
Abbreviations: %HF20sec and %HF5min, the relative times over which the same main high-frequency peak was sustained for at least 20 seconds and 5 minutes in total recording time (markers of stability of parasympathetic nerve function); CLD, chronic lung disease with irreversible pulmonary dysfunction and mild-to-moderate daytime hypoxemia; NOD, nocturnal oxygen desaturation defined as CT90 ≥3%; CT90, cumulative time with SpO2 <90%; LTOT, long-term oxygen therapy.
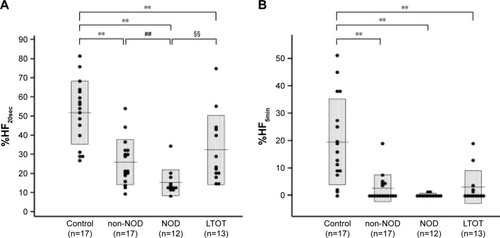
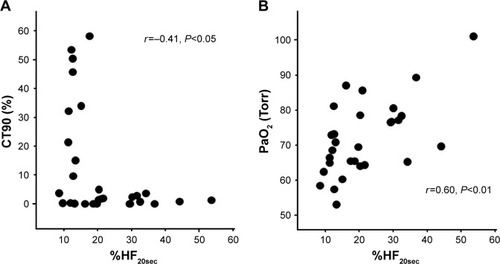
Figure 3 Relationship between %HF20sec, an index of stability of parasympathetic nerve function, and CT90 (A) or PaO2 (B).