Figures & data
Figure 1 Diagram of regulatory mechanism of renin-angiotensin system (RAS). The classical RAS pathway begins with the conversion of angiotensinogen (AGT) to an inactive decapeptide precursor angiotensin I (Ang I) through the action of renin. Ang I is further recognized and cleaved by angiotensin converting enzyme (ACE) to produce active octapeptide angiotensin II (Ang II). Ang II is the key biological peptide of RAS which has various physiological regulatory effects. It acts mainly through the combination of type 1 angiotensin II receptor (AT1R) to constrict blood vessels, raise blood pressure, promote inflammation, and promote fibrosis and apoptosis. It can also bind to AT2, AT3, and AT4 receptors, and plays different physiological roles. In addition, angiotensin converting enzyme 2 (ACE2) can cleave Ang I C-terminal peptide to produce inactive Ang (1-9), then Ang (1-9) can be hydrolyzed by ACE and other peptidases to produce active Ang (1-7). ACE2 can also directly cleave Ang II to form Ang (1-7). Ang (1-7) binds to the Mas receptor (MasR) and exerts physiological functions that are contrary to Ang II, including vasodilation, lower blood pressure, anti-inflammation, anti-oxidative stress, anti-fibrosis, etc. These form two main functional axes of RAS. Ala-Ang (1-7) is produced when the aspartate at the amino terminal of Ang (1-7) is replaced by alanine. It can bind to the new receptor Mas-related G protein-coupled receptor D (MrgD) and protect against hypertension, inflammation, and lung damage. Furthermore, ACEI and ARB can protect against RAS imbalance by inhibiting the conversion of Ang I to Ang II and the binding of Ang II to the AT1R, respectively. We also showed that some viral infections can interfere with the function of RAS, leading to acute lung injury (ALI) and even acute respiratory distress syndrome (ARDS).
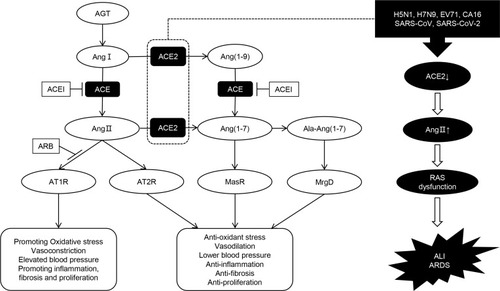
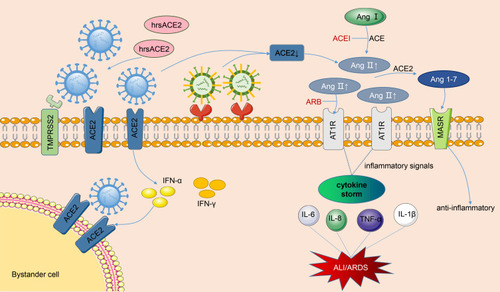
Figure 2 Pathogenesis of renin-angiotensin system in acute lung injury caused by viral infections. The SARS-CoV and SARS-CoV-2 bind to membranes angiotensin converting enzyme 2 (ACE2) of and employ type II transmembrane serine protease (TMPRSS2) for Spike protein priming, facilitating the fusion of viral and cellular membranes. After SARS-CoV-2 invades cells, it activates the natural antiviral pathway, prompts the infected cells to secrete interferon, stimulates bystanders to up-regulate ACE2 expression, and creates more targets for the entry of SARS-CoV-2. Occupation of ACE2 by the virus leads to the reduction of cell surface ACE2 levels. As the virus enters the cell, not limited to SARS-CoV and SARS-CoV-2, but also H5N1, H7N9 and EV71, the angiotensin II (Ang II) levels are significantly upregulated, a large amount of Ang II binds to the type 1 angiotensin II receptor (AT1R), then the inflammatory signaling pathways are overactivated, and then secrete various cytokines, resulting in cytokine storm and eventually lung injury. In the meantime, the ACE2 can cleave Ang II into Ang 1-7 which combines with Mas receptor (MasR) to fight against inflammation. ACEI and ARB can help restore the RAS balance after viral infections. Moreover, clinical-grade human soluble ACE2 (hrsACE2) can inhibit the coronavirus invasion by binding to coronavirus outside the cell. The blue virus in the figure represents coronaviruses, and the other one represents other viruses, such as H1N1, H7N9, and EV71.