Figures & data
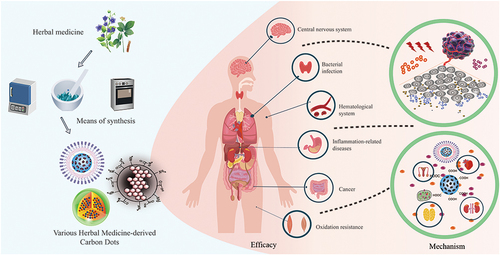
Table 1 The Comparative Summary of Synthesis Strategies for HM-CDs
Figure 1 Preparation methods of HM-CDs. (A) hydrothermal synthesis process; (B) pyrolysis synthesis process; (C) microwave carbonization synthesis process.
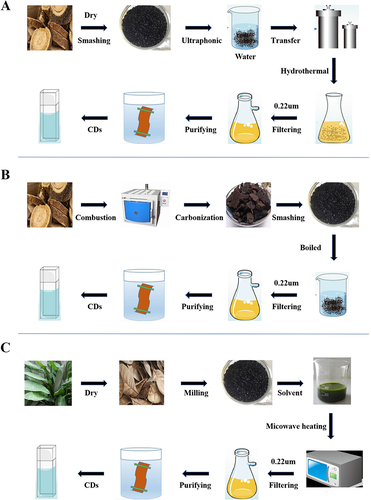
Table 2 HM-CDs Synthesized by Microwave Carbonization
Figure 2 HM-CDs significantly improved blood-brain barrier (BBB) permeability. HM-CD-1 has an ultra-tiny size and abundance surface functional groups. The covalent binding of HM-CD-2 to the drug facilitates passive transport of the drug. HM-CD-3 has a strong affinity for the BBB endothelial cell membrane.
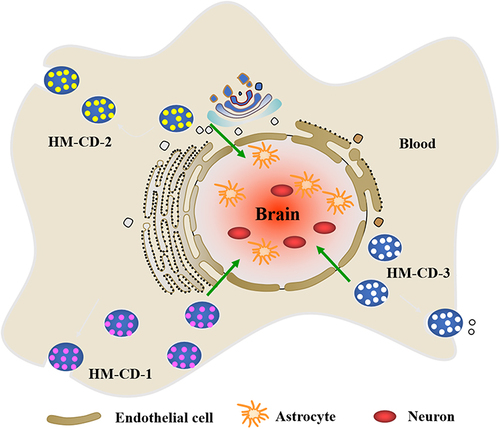
Figure 3 The current application of HM-CDs in disease treatment, including hematological system (hemostasis, hypoglycemic, and blood enrichment), bacterial infection, inflammation-related diseases (arthritis, epidermal inflammation, allergic inflammation, and organ damage inflammation), anticancer, diseases related to oxidative stress, other disease areas (menopausal syndrome, anxiolytic).
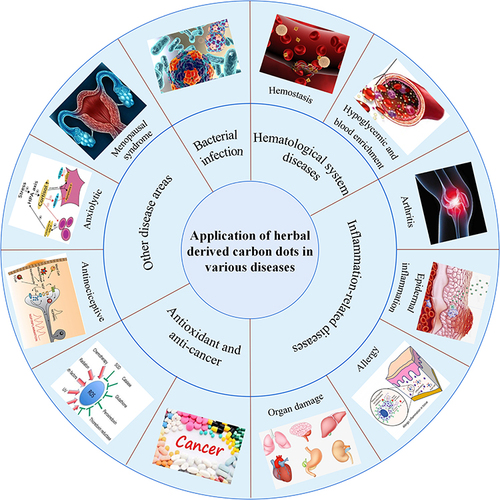
Table 3 HM-CDs as Potential Therapeutic Agents for Hematological Disorders
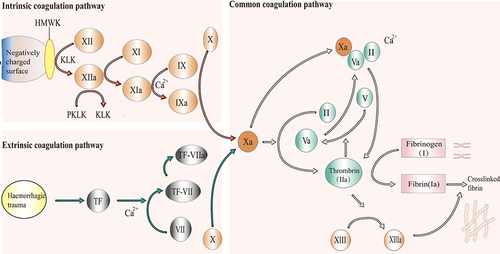
Figure 4 Mechanisms of hemostasis. Under the synergistic effect of platelet activation, coagulation factors undergo a complex coagulation cascade to produce thrombin (also known as activated factor II (IIa)), which converts fibrinogen (also known as factor (I) in adjacent plasma into fibrin (also known as factor Ia). The interwoven fibrin makes platelets clot and blood cells tangle into thrombi at the bleeding site. The coagulation cascade includes extrinsic and intrinsic pathways. The extrinsic pathway is initiated by the exposure of blood to tissue factor (TF) following tissue damage and eventually leads to the activation of factor X into factor Xa. For the intrinsic pathway, factor XII is activated when blood contacts a negatively charged surface, resulting in the downstream proteolytic activation of other coagulation factors until factor X is activated into factor Xa. The two pathways converge into a common pathway through factor Xa. Factor Xa cleaves prothrombin (also known as factor II) into thrombin in the presence of phospholipids and Ca2+, and thrombin converts fibrinogen into fibrin to achieve the main goal of haemostasis.