Figures & data
Figure 1 The morphology of porous n-HA/PA66 composite.
Notes: (A) A porosity of 75%–85% and an average pore size of 500 microns; (B) A size of 4 × 2 × 2 mm3.
Abbreviation: n-HA/PA66, nano-hydroxyapatite/polyamide 66.
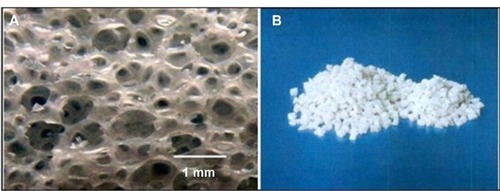
Table 1 Details of patients after implantation of the porous n-HA/PA66 composite
Figure 3 Figure showing how the amount of new bone and calcium crystals increased as the time goes on.
Notes: Bone and calcium crystals at (A) 2 weeks, (B) 8 weeks, (C) 12 weeks, and (D) 26 weeks. Masson staining was used, x200 magnification. After 26 weeks, interconnected porosity was filled completely with new bone tissue, which integrated into a whole.
Abbreviations: M, material; B, bone.

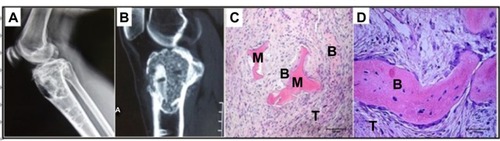
Figure 4 The SEM images (×2,000 magnification) of the porous n-HA/PA66 composite with implantation into the rabbit tibia.
Notes: The interface of material and bone at (A) 2 weeks, (B) 8 weeks, (C) 12 weeks, and (D) 26 weeks. After 26 weeks, the porous n-HA/PA66 composites integrated with host bone completely.
Abbreviations: SEM, scanning electron microscope; n-HA/PA66, nano-hydroxyapatite/polyamide 66; M, material; B, bone.
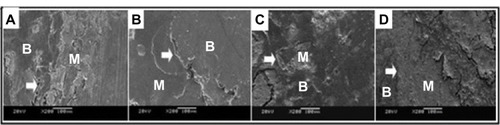
Table 2 Statistical data on 21 patients
Figure 5 A 20-year-old man suffering from fibrous dysplasia of the right proximal femur.
Notes: (A) The original image of the defect site. Periodic radiological assessments showed (B) during the period of 6 months, 50% of the grafting zones were replaced by new bones, and (C) fully occupied at 1.5 years after surgery. (D) With a more than 5 years follow-up, the porous n-HA/PA66 composite had been completely incorporated with the host bone. (E and F) grafting-to-non-lesion count ratio was 0.83, the patient was satisfied with the result, and the MSTS was 30.
Abbreviations: n-HA/PA66, nano-hydroxyapatite/polyamide 66; MSTS, Musculoskeletal Tumor Society score.
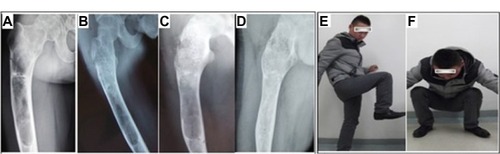
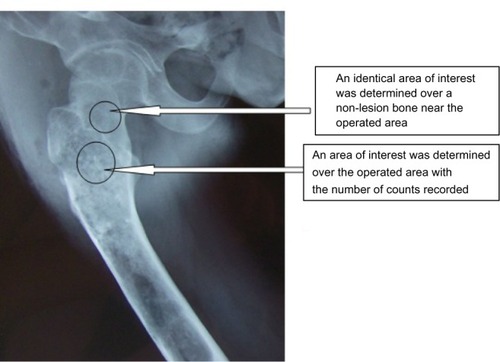
Figure 6 Images of a 47-year-old woman treated by a giant cell tumor resection and fixed with an internal steel plate after the porous n-HA/PA66 composite grafted in the right distal femur.
Notes: Periodic radiological assessments showed that the new bones developed and the porous n-HA/PA66 composite incorporated with the host bone gradually. The internal steel plate was still rigidly fixed and no joint surface subsidence occurred. (A) Preoperative; (B) a half-year after resection; (C) 1 year; and (D) 5 years later. The grafting-to-non-lesion count ratio was 0.78 and the MSTS score was 29 after 5 years follow-up (E and F).
Abbreviations: n-HA/PA66, nano-hydroxyapatite/polyamide 66; MSTS, Musculoskeletal Tumor Society score.

Figure 7 Comparing the G/N ratio between the metaphyseal and diaphyseal areas where the porous n-HA/PA66 composites were implanted after bone tumor resection.
Abbreviations: G/N ratio, grafting-to-non-lesion ratio; n-HA/PA66, nano-hydroxyapatite/polyamide 66.
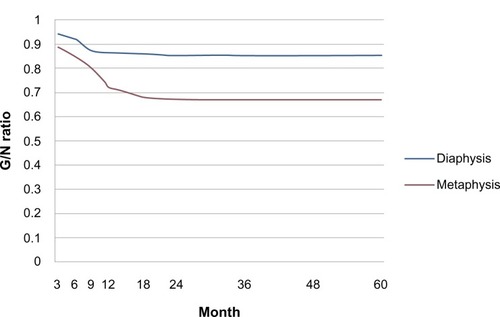
Figure 8 Images of the female patient that did not meet inclusion criteria due to recurring giant cell tumor.
Notes: A woman, 46 years, suffered from giant cell tumor of the right proximal tibia and had shown recurrence after a follow-up of 2 years. She received treatment by tumor resection and single implantation of the porous composite. (A and B) show the X-ray image and magnetic resonance image of GCT recurrence; (C and D) show the histological images of GCT recurrence, (C) HE ×100, (D) HE ×200).
Abbreviations: n-HA/PA66, nano-hydroxyapatite/polyamide 66; GCT, giant cell tumor; M, material; B, bone; T, tumor; HE, hematoxylin and eosin staining.