Figures & data
Figure 1 Effects of anti-CD52 on immune system. Administration of anti-CD52 causes depletion of circulating CD52+ cells, which are T cells, B cells, and immature myeloid dendritic cells (DCs). Depletion is due to complement-dependent cytolysis (CDC) and antibody-dependent cellular cytotoxicity (ADCC). In the periphery, after CD52+-cell depletion, a transient increase in TNFα and IFNγ is observed. Repopulation of depleted cells occurs from the thymus and bone-marrow population of cells, taking in human 3–6 months for B cells and up to 61 months for T cells. Fast repopulation of regulatory T and B cells is observed, which creates an immunotolerant environment. After depletion in the periphery, CD52+-cell infiltration into the CNS is decreased. This further decreases cell aggregates in the CNS and increases levels of anti-inflammatory cytokines, and decreased levels of proinflammatory cytokines are observed. Increased levels of neurotrophic factors are also noted.
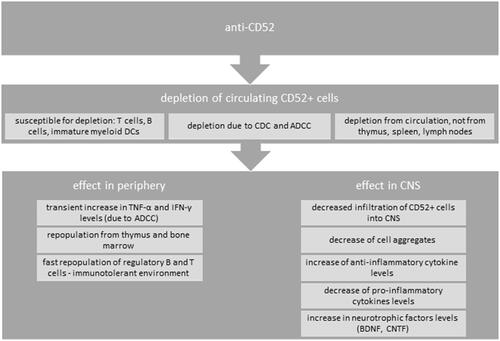
Table 1 Alemtuzumab treated MS patients with COVID-19 described in the literature
