Abstract
Objectives:
To assess whether the detubularised isolated ureterosigmoidostomy (DIUS) technique is safe for urinary diversion after radical cystectomy.
Patients and methods:
The study included 10 patients (mean age 61.8 years) with invasive bladder tumour, operated at the Alexandria University, Egypt. The diversion in all patients was through a DIUS, with ureteric reimplantation by an antirefluxing procedure, using an embedded-nipple technique. The patients were evaluated before and after surgery using radiological and manometric studies, and the results analysed statistically using Student’s t-test.
Results:
Nine of the 10 patients could differentiate between urinary and stool sensation, and evacuate them separately. The mean (range) daytime frequency was 4.1 (3–5) and the mean night-time frequency was 0.5 (0–1). Before and after surgery, the respective mean resting anal pressure was 71 and 74 cmH2O (P = 0.004), the volume at first desire to defecate was 54 and 72 mL (P = 0.004) and the maximum tolerable volume was 140 and 160 mL (P < 0.001). The anorectal inhibitory reflex was lost in all patients after surgery. The mean (SD, range) basal pouch pressure was 5 (3.33, 0–10) cmH2O, and the end pressure was 13.2 (4.42, 9–20) cmH2O.
Conclusion:
Although the Mainz II pouch has a documented efficacy for urinary diversion after radical cystectomy, the modifications we applied to the DIUS improved that method of diversion, by separating urine and stool evacuation, maintaining continence, and with a low frequency and better protection of the upper urinary tracts, resulting in an improvement in the patients’ quality of life.
Introduction
Bladder cancer is the ninth most common cancer throughout the world [Citation1], and recent reports show that its incidence and mortality rates are decreasing in western countries, in contrast to some eastern European and developing countries [Citation2]. According to the Surveillance, Epidemiology and End Results database, ≈2.4% of men and women will be diagnosed with bladder cancer at some point during their lifetime [Citation3]. Bladder cancer is the most prevalent malignancy among Egyptian men (16%), resulting in >7900 deaths annually [Citation4].
Of patients with bladder cancer, 20–40% either present initially with invasive tumour or there is progression from a superficial disease [Citation5]. Radical cystectomy (RC) for recurrent non-muscle-invasive and invasive disease offers the best outcomes to patients, regardless of their age group, with recurrence-free survival rates at 5 and 10 years of 68% and 66%, respectively [Citation6,Citation7].
An assessment of the patient’s quality of life after RC is extremely important, as the procedure can affect body image, urinary, sexual, and social functions [Citation8]. Mohamed et al. [Citation9] reported that patients treated by RC and urinary diversion had many unmet psychological needs, in the form of depression and worries about their body image after surgery. European guidelines recommend that patients should be encouraged to actively participate in the decision-making for urinary diversion, and that continent diversion should be offered, unless there are specific contraindications [Citation10].
Singh et al. [Citation11] studied 164 patients managed by either an ileal neobladder or ileal conduit diversion after RC. They showed that an orthotopic neobladder is better in terms of physical, role and social functioning. Although an orthotopic bladder seems to be an ideal method of urinary diversion, studies showed that nocturnal enuresis is troublesome for most patients, for although diurnal continence was almost present in all, nocturnal continence was achieved in 44–66% [Citation12–Citation14]. We reported [Citation15] urodynamic criteria that can help urologists to predict the occurrence of diurnal and nocturnal continence after orthotopic bladder reconstruction.
Recently, many reports [Citation16–Citation20] showed that the Mainz pouch II was a safe and reproducible method of urinary diversion, and serves as a satisfactory method of continent urinary diversion in all age groups. We added a modification to the Mainz pouch II [Citation21], the detubularised isolated ureterosigmoidostomy (DIUS), and reported a novel simple technique for ureteric reimplantation using a nipple technique [Citation22]. In our modification the whole rectosigmoid colon is detubularised to 2.5 cm below the peritoneal reflection of the rectum. This anterior rectotomy aims to abolish the anorectal inhibitory reflex responsible for defecatory sensation and urge, in an attempt to improve bowel function after ureterosigmoidostomy. The improvement of rectal accommodation, and consequently a better bowel evacuation pattern, reduced the frequency, and absence of urgency and nocturnal wetting. The present study provided rectodynamic and radiological evidence for this improved function after DIUS.
Patients and methods
This was a prospective study of 10 patients (seven men and three women, mean age 61.8 years, range 45–72) with invasive bladder cancer, scheduled for RC and urinary diversion by the DIUS. All patients were assessed before and after surgery using anorectal manometric studies with the Andromeda urodynamic machine (Medizinische Systeme GmbH, Taufkirchen/Potzham, Germany) and included the following measurements.
Anal pressure
This was measured using an 8 F Nelaton catheter with four orifices at 90° between them and in the same plane at 5 cm from the catheter tip. The catheter was introduced through the anal canal into the rectum, identified when the pressure decreased to the basal rectal pressure. The catheter was infused with saline at 6 mL/min, with simultaneous pressure measurements while the catheter was gradually and continuously withdrawn to the outside at a near constant rate of 1 mm/s. The pressure was measured at regular points on the resulting curve and the mean was reported as the resting anal-canal pressure. The maximum rise on the curve was also recorded.
Rectal pressure
This was assessed using an 8 F Nelaton catheter with a balloon at one end, which was introduced into the rectum. The other end of the catheter was connected by a three-way stopcock to the pressure-measuring channel and to an infusion syringe. Repeated incremental volumes of 20 mL of saline were injected into the balloon, and the rectal pressure measured with each 20 mL increase. The pressures and volumes that stimulated the patient’s first desire to defecate, constant desire to defecate and maximum tolerated volume were recorded.
Anorectal inhibitory reflex
The pressure at the proximal part of the anal canal was measured in response to increasing the rectal pressure by distending the rectal balloon, to assess the anorectal inhibitory reflex.
All patients had a urinary diversion using the DIUS [Citation20], with a bilateral embedded ureteric reimplantation. At 3 months after surgery all patients were assessed using imaging studies, including ultrasonography of the abdomen to assess the upper urinary tracts, and a pouchogram, done using 20% diluted contrast medium mixed with streptomycin (1 g/100 mL), to assess the pouch capacity and morphology, and ureteric reflux or regurgitation of the contrast medium into the descending colon. In addition, a film was taken after evacuation to assess the residual amount of the injected dye. At the same time the manometric variables were assessed, including the anal pressure, rectal pressure and anorectal inhibitory reflex, and a ‘pouchometrograph’ was constructed by inserting two catheters into the new pouch, one for continuous infusion of saline at 50 mL/min and the other for pressure measurement. We recorded the basal pressure, end pressure and presence of contraction waves and their pressure.
Results
The follow-up assessments were made at 6 months after surgery. Nine patients could differentiate well between urine and stool, and were able to defecate and urinate separately. Only one patient could not differentiate between the sensations and was evacuating mixed urine and stool. The mean (range) daytime frequency was 4.1 (3–5) and the mean night-time frequency was 0.5 (0–1). Daytime and nocturnal continence was achieved in all patients. shows the ultrasonographic findings at 6 months after surgery.
Table 1 The findings on ultrasonography before and 6 months after surgery, from the pouchogram after DIUS, and the manometric findings before and after surgery.
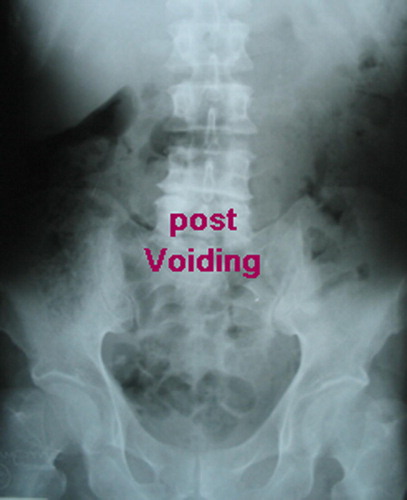
The pouchogram showed that nine patients had no reflux of the contrast medium, either to the descending colon or to the upper urinary tract, and films after evacuation showed complete emptying of the pouch, with no or minimal residual contrast medium. Only one patient had reflux to the descending colon that occurred at 500 mL, and in the postvoid film there was no residual contrast medium in the pouch or in the descending colon. also shows the findings of the pouchogram. shows a pouchogram done with 500 mL of infusion, and shows that there was no postvoid residual in the same patient.
The mean (SD, range) basal pouch pressure was 5 (3.33, 0–10) cmH2O, the mean end pressure was 13.2 (4.42, 9–20) cmH2O and contraction waves were found in one patient, with a pressure of up to 40 cmH2O. shows the manometric findings before and after surgery.
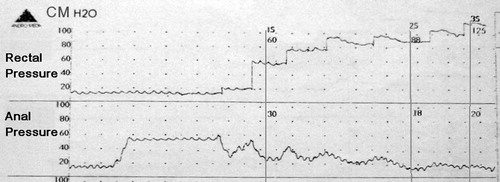
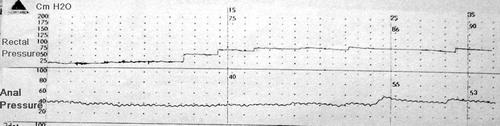
The anorectal inhibitory reflex was present in all patients before surgery, when the anal pressure at the proximal portion of the anal canal gradually decreased in response to gradual rectal distension (), while the reflex was absent in all patients after surgery, the anal pressure at that portion remaining constant in response to gradual rectal distension ().
Discussion
In the developed world urinary diversion has changed from ureterosigmoidostomy to an ileal conduit, orthotopic bladder or other forms of continent urinary diversion. This change is explained by the common complications caused by such a technique of diversion, including poor quality of urine control, ureteric stenosis and chronic pyelonephritis, leading to chronic renal insufficiency and an increased risk of secondary malignancy [Citation23–Citation25]. Physiologically an orthotopic neobladder is not an ideal method of diversion, as the neobladder lacks the voiding and guarding reflexes. During voiding the urethra does not open, the ileum does not contract and the patient has to strain or use the Crede manoeuvre. During storage the urethral sphincter does not contract in response to ileal contraction with higher pressure waves, and there is no guarding reflex, resulting in nocturnal wetting. Continence requires a reflex and not only a high pressure zone.
Detubularisation of the whole rectosigmoid colon allows the formation of a low-pressure high-capacity reservoir. The left colon is intussuscepted and fixed into the posterior wall of the rectal pouch, as low as possible, to be in continuity with the anal canal. Both ureters are implanted into the upper half of the reservoir. This allows a large urine reservoir, with no refluxing into the high-pressure left colon, and the left colon evacuates directly into the anal canal then to outside, with complete separation of urine and stool evacuation, and the ability to differentiate between them, as was the case in nine of our 10 patients.
This advantage was apparent during many years of using DIUS in our patients, and being able to distinguish urine and stool and evacuate them separately was a factor with a high psychological effect in our patients. This advantage is absent in all other methods of ureterosigmoidostomy diversion, including the Mainz pouch II. A study of the quality of life after using the Mainz II [Citation26] reported that evacuation of mixed stool and urine can lead to an altered sensation of diarrhoea, and results in cognitive and social functional impairment. In the present study there was one patient who was evacuating mixed urine and stool, and this was explained by an improper fixation of the left colon into the posterior wall of rectal ampulla. In DIUS both stool and urine are evacuated with preserved reflexes, while the abolition of the anorectal inhibitory reflex results in excellent high rectal compliance which can accommodate the new extra load of colonic content. This results in a satisfactory evacuation frequency with no defecatory urgency. In the present technique, wetting was reported only with gas passage, a situation which could be controlled with the use of anti-flatulence drugs.
In the present study daytime and nocturnal continence was achieved in all patients, and can be explained by two factors. First, including the rectum into the pouch created a large pouch with low pressure. Manometric studies showed that the mean (SD, range) basal pouch pressure was 5 (3.33, 0–10) cmH2O and the mean end pressure was 13.2 (4.42, 9–20) cmH2O. Second, rectal detubularisation interrupts the local myenteric nerve plexus that is responsible for the integrity of the anorectal inhibitory reflex, resulting in loss of that reflex. Patients were incontinent only while passing gas, and that could be averted simply by using anti-flatulence drugs.
D’elia et al. [Citation27] reported their 10-year experience with the Mainz II pouch and showed that the rate of postoperative incontinence was 3% and 5% during the day and night, respectively. The reported rate of nocturnal incontinence was 20% by Bastian et al. [Citation20] and 24% by Hadzi-Djokic et al. [Citation28]. A study [Citation29] on classical ureterosigmoidostomy reported a rate of day and night-time incontinence of 7% and 50%, respectively.
In the present study the mean day and night-time frequency was 4.1 (3–5) and 0.5 (0–1), respectively. Hadzi-Djokic et al. [Citation28] reported a mean diurnal frequency of 4.2, with 21% of patients voiding more than six times during the day, while the mean nocturnal frequency was 2.1, with 27% of patients voiding 3–6 times and 5% voiding more than six times at night. That high rate was consistent with the findings from other series [Citation26,Citation30,Citation31]. The present results can be also explained by the rectal detubularisation interrupting the local myenteric nerve plexus that is responsible for the integrity of the anorectal inhibitory reflex (in turn responsible for the defecatory urge), resulting in loss of that reflex. The anorectal inhibitory reflex is defined as a transient relaxation of the internal anal sphincter in response to rectal distension, with synchronous contraction of the external anal sphincter, and this is associated with the desire for defecation. The reflex is transitory, lasts for 1 min and is soon followed by a return of the tone of the intrinsic anal sphincter despite the continued rectal ampullary distension. If defecation is to be deferred there is a voluntary contraction of the external anal sphincter and levator ani muscles, resulting in rectal relaxation with better accommodation. However, with larger volumes the duration of the reflex inhibition becomes more prolonged and the recovery less complete. The reflex is lost at high rectal volumes (>400 mL). The reflex is hypothesised to serve as a ‘sampling reflex’, presenting the contents of the rectum, which is sensitive only to stretch to the upper anal canal, and which has all the sensations for faecal contents (solid, fluid or gas) and can discriminate between flatus and faecal material. Loss of that reflex using the DIUS technique allows pouch filling, with decreased frequency and urgency and improved continence.
In the present study, the mean basal pouch pressure was 5 cmH2O and the mean end pressure 13.2 cmH2O, with contraction waves found in one patient, with a pressure of up to 40 cmH2O. In 1994, Fisch et al. [Citation32] reported that the full reservoir pressure was 24 cmH2O and the maximum reservoir pressure 35 cmH2O. In 1996, Gilja et al. [Citation33] used the same technique and reported that the mean basal pouch pressure was 19.5 cmH2O. In 2000, Gumus et al. [Citation34] also used the same technique and reported that the mean basal pouch pressure was 6 cmH2O, with no contraction waves except in three patients, with pressures of 17–48 cmH2O. The end pressure (when the patient feels abdominal discomfort) was 13.8 cmH2O. The lower pouch pressure in the present study explains the low rate of reflux into the upper tracts in our patients, and the resulting low rate of pyelonephritis and renal insufficiency. Also, the resulting lower rate of reflux into the colon, with no residual volume, might be the cause of the low rate of electrolyte disturbances in our patients and the lower need for alkalinising agents.
The mean resting anal canal pressure was significantly higher after surgery and this increase might be explained as a compensatory mechanism of the anal sphincter to control urine, instead of controlling stool.
Although it was not an endpoint of the present study, over 15 years of using such diversion it is clear that during the long-term follow-up the technique is safe and does not significantly increase the risk of malignancy, as was shown in other studies of the Mainz II pouch and classical ureterosigmoidostomy [Citation35,Citation36]. This might be explained by the separation of urine and stool in our patients, as it was suggested that faecaluria [Citation37] and chronic irritation of the ureteric end [Citation38] with faecal matter is the leading factor for the increased rate of malignancy in such patients.
Stenosis in the uretero-intestinal anastomosis is a complication with different types of ureteric anastomosis. In the present patients, a uretero-intestinal anastomosis using a nipple technique was an easy and safe method of anastomosis, as the resulting ureteric orifice after construction will have an intact epithelium, resulting in a low rate of postoperative ureteric obstruction by oedema, and a low rate of the development of stricture during a long-term follow-up. Also, the everting suture reported previously [Citation22] allows easy nipple formation and reimplantation of a dilated, thick wall ureter.
In conclusion, although the Mainz II pouch has documented efficacy in diverting urine after RC, the modifications we have added in the DIUS technique improved that method of diversion, by separating urine and stool evacuation, maintaining continence, a low frequency and better protection of the upper urinary tracts, resulting in an improvement in the patients’ quality of life.
Conflict of interest
None.
Funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- D.M.ParkinF.BrayJ.FerlayP.PisaniGlobal cancer statistics, 2002CA Cancer J Clin55200574108
- Chavan S, Bray F, Lortet-Tieulent J, Goodman M, Jemal A. International variations in bladder cancer incidence and mortality. Eur Urol 2013 October 16; doi: 10.1016/j.eururo.2013.10.001. [Epub ahead of print].
- Anonymous. Surveillance, Epidemiology and End Results program. SEER stat fact sheets: bladder cancer. Available at <http://seer.cancer.gov/statfacts/html/urinb>.
- J.FerlayH.R.ShinF.BrayD.FormanC.MathersD.M.ParkinD.M.ParkinEstimates of worldwide burden of cancer in 2008. GLOBOCAN 2008Int J Cancer2010127200828932917
- H.KhaledSystematic management of bladder cancer in Egypt: revisitedJ Egypt Natl Cancer Inst172005127131
- Trulson JJ, Sharma P, Haden T, Kheterpal E, Pokala N. Comparative survival following different treatment modalities for stage T2 bladder cancer in octogenarians. World J Urol 2013 July 2. [Epub ahead of print].
- D.J.GallagherM.I.MilowskyBladder cancerCurr Treat Options Oncol102009205215
- J.P.SteinG.LieskovskyR.CoteS.GroshenA.C.FengS.Boydet alRadical cystectomy in the treatment of invasive bladder cancer: long-term results in 1054 patientsJ Clin Oncol192001666675
- N.E.MohamedP.Chaoprang HerreraS.HudsonT.A.RevensonC.T.LeeD.Z.Qualeet alMuscle invasive bladder cancer. Examining survivor burden and unmet needsJ Urol19120144853
- Witjes JA, Compérat E, Cowan NC, De Santis M, Gakis G, Lebret T, et al. EAU Guidelines on muscle-invasive and metastatic bladder cancer: Summary of the 2013 Guidelines. Eur Urol 2013 Dec 12. [Epub ahead of print]
- Singh V, Yadav R, Sinha RJ, Gupta DK. Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model. BJU Int 2013 September 5. [Epub ahead of print].
- J.E.MontieJ.E.PontesE.M.SmythSelection of the type of urinary diversion in conjunction with radical cystectomyJ Urol137198711541155
- D.A.ElmajianJ.P.SteinD.EsrigJ.A.FreemanE.C.SkinnerS.D.Boydet alThe Kock ileal neobladder: updated experience in 295 male patientsJ Urol1561996920
- R.E.HautmannR.de PetriconiH.W.GottfriedK.KleinschmidtR.MattesT.PaissThe ileal neobladder. Complications and functional results in 363 patients after 11 years of followupJ Urol1611999422
- M.M.KoraitimM.A.AttaM.K.FodaOrthotopic bladder substitution in men revisited. Identification of continence predictorsJ Urol176200620812084
- J.LeissnerR.SteinR.HohenfellnerRadical cystoprostatectomy combined with Mainz Pouch bladder substitution to the urethra: long-term resultsBJU Int831999964
- K.A.MtetaA.Y.Al-AmmaryModified ureterosigmoidostomy for malignant and non malignant conditionsEast Afr Med J852008334340
- I.IgnjatovicD.BasicModified Mainz pouch II (sigma rectum pouch) urinary diversion: 12 years experienceActa Chir Iugosl5420077377
- Z.DzamicJ.Hadzi DjokicM.AcimovicM.JovanovicJ.FilimonovicC.Tulicet alModified Mainz pouch II urinary diversion and quality of lifeActa Chir Iugosl5420075762
- P.J.BastianP.AlbersA.HaferkampS.SchumacherS.C.MullerModified ureterosigmoidostomy (Mainz pouch II) in different age groups and with different techniques of ureteric implantationBJU Int942004345349
- M.A.AttaDetubularized isolated ureterosigmoidostomy. Description of a new technique and preliminary resultsJ Urol1561996915919
- M.A.AttaThe everting suture: a new technical aid for ureteral nipple constructionJ Urol155199613721373
- S.B.FarnhamM.S.CooksonSurgical complications of urinary diversionWorld J Urol222004157167
- R.D.MillsU.E.StuderMetabolic consequences of continent urinary diversionJ Urol161199910571066
- M.AustenT.KalbleSecondary malignancies in different forms of urinary diversion using isolated gutJ Urol1722004831838
- P.J.BastianP.AlbersH.Hanitzschet alHealth related quality of life following modified ureterosigmoidostomy (Mainz pouch II) as continent urinary diversionEur Urol462004591597
- G.D’eliaS.PahernikM.FischR.HohenfellnerJ.W.ThüroffMainz pouch II technique: 10 years’ experienceBJU Int93200410371042
- J.B.Hadzi-DjokicD.T.BasicA modified sigma-rectum pouch (Mainz pouch II) technique. Analysis of outcomes and complications on 220 patientsBJU Int972006587591
- M.IshigookaT.HashimotoK.IzumiyaI.SasagawaT.NakadaIncidence of anal incontinence after long-term follow-up of patients treated with ureterosigmoidostomyInt Urol Nephrol251993455460
- C.ObekA.R.KuralS.AtausE.CoskunerO.DemirkesenA.Citçiet alComplications of the Mainz pouch II (sigma rectum pouch)Eur Urol392001204211
- C.R.WoodhouseM.ChristofidesModified ureterosigmoidostomy (Mainz II) technique and early resultsBr J Urol811998247252
- M.FischR.WammackS.C.MüllerR.HohenfellnerThe Mainz pouch IIEur Urol251994715
- I.GiljaM.KovacicM.RadejD.KosutaB.BakulaL.GolesThe sigmoidorectal pouch (Mainz pouch II)Eur Urol291996210215
- E.GumusC.MirogluL.SaportaG.BasaranK.HorasanliO.Tanriverdiet alRectodynamic and radiological assessment in modified Mainz pouch II casesEur Urol382000316322
- T.KälbleA.R.TrickerP.FriedlR.WaldherrJ.HoangG.Staehleret alUreterosigmoidostomy. Long-term results, risk of carcinoma and etiological factors for carcinogenesisJ Urol144199011101114
- R.F.GittesCarcinogenesis in ureterosigmoistomyUrol Clin N Am131986201
- M.M.CrisseyG.D.SteeleR.F.GittesRat model for carcinogenesis in ureterosigmoidostomyScience20719801079
- H.H.RobinovitchUreterosigmoidostomy in children – revival or demise?J Urol1241980552