Abstract
Aim
To describe parental perceptions of general health, oral health and received dental health care in Swedish children with Down syndrome (DS).
Methods
Online questionnaire, quantitative data analysis (Chi-square test).
Results
Parents of 101 children with DS (52 boys, 49 girls, mean age: 9.6 years) participated. Seventy percent rated their child’s general health and 74% their child’s oral health as good or very good. Parents, who rated their child’s oral health as poor (8%), also reported that dental procedures were difficult. Children received dental care at general (55%) and specialist clinics (53%). Ninety-four percent of parents of children receiving specialist dental health care were satisfied compared to 70% of parents with children in general clinics. The parents most valued characteristics of dental professionals were patience (63%) and their ability to engage the child (68%). Parents wanted multidisciplinary collaboration.
Conclusion
Most parents rated their child’s general and oral health as good or very good. Children with poor oral health were also reported to have difficulties coping with dental procedures. Parents wanted dental care to be tailored to meet their child’s unique needs. They wanted dental professionals to have knowledge about children with a need for special care. Lastly, they requested multidisciplinary collaboration.
Introduction
In Sweden, about 140 children with Down syndrome (DS) are born every year and constitute about 0.16% of all children in the country [Citation1]. Most children with DS have intellectual disabilities and increased risk of different medical problems. Congenital heart defect, visual impairment, hearing problems, increased susceptibility to infections, autoimmune diseases, thyroid diseases and leukaemia are common [Citation2–4]. Oral health may also be affected [Citation5–8]. Anatomical and developmental differences in the middle third of the face may cause functional problems [Citation9]. Low muscle tone in the lips and tongue, as well as difficulties with chewing, swallowing, speech and other orofacial functions, may affect feeding ability during infancy [Citation10]. An underdeveloped maxilla, hypodontia, narrow airways, hypotonic muscles and tongue protrusion can increase the development of malocclusions [Citation11–14]. The risk of obstructive sleep apnoea syndrome and respiratory tract infections is high in children with DS compared to typically developing children [Citation15]. Individuals with DS, including children, have a higher risk for periodontitis due to several factors, such as impaired immune response and difficulties in oral hygiene [Citation16]. Oral candidiasis is common, and an increased frequency of tooth wear has been noted with a multifactorial aetiology in children and young adults with DS [Citation7,Citation17,Citation18].
It remains unclear whether individuals with DS have an increased risk for caries or not compared to individuals without DS. However, risk factors for caries in children with DS are more frequent, such as reduced salivary function, food impaction and difficulties maintaining suitable oral hygiene [Citation19,Citation20].
In Sweden, dental health care for all children and adolescents up to 23 years of age is free of charge for the individual [Citation21]. All 21 Swedish regions are responsible for organizing dental health care for their inhabitants. In some regions, there is limited access to paediatric dental specialists while other regions have well-established specialist clinics [Citation22]. Measures for prevention of oral diseases for each child are planned after individual risk assessment. Information, hygiene instructions, food intake recommendations and fluorides are given at regular recall visits, usually by a dental hygienist or by a dental nurse [Citation23]. In Sweden, dentists or dental hygienists examine children at child-specific intervals based on perceived risk of oral health problems and at some orthodontic key stages. According to the Swedish national medical guidelines for children with DS, established contact with dental health care, including oral hygiene follow-ups if necessary, is recommended from around one year of age [Citation24].
It is not uncommon for children with DS to also have an autism spectrum disorder (ASD), which may impair the child’s ability to maintain good oral health habits, as well as making communication an additional barrier during dental health care visits. Children who find it difficult to interact with people outside of the family have a greater need for customized dental care [Citation25,Citation26]. Therefore, these children often meet specialists in paediatric dentistry [Citation27].
It is always important for parents to support their child to keep an overall good oral health and even more so if the child has a disability. In comparison to parents of typically developed children, parents of children with DS often need to support their child more [Citation28]. It is also well known that the oral health behaviour of the parents often affects their children’s oral health [Citation29,Citation30]. Other parental factors potentially influencing a child’s oral health are level of education, ethnicity, and socioeconomic status [Citation31]. In a study from Brazil, mothers of children with DS expressed difficulties supporting their children in daily oral hygiene. They also reported that their financial situation influenced the possibility for professional dental health care [Citation32]. It is also reported that parents of children with disabilities often prioritize treatment and management of medical problems over dental needs [29,Citation33].
In a Belgian survey with 100 parents of children with DS, 53% rated their child's oral health as ‘quite good’ and 31% as ‘very good’. According to these parental reports, 66% of the children had been to a dentist in the previous six months and 23% in the past year. Eighty-three percent were satisfied with their child’s dentist; however, about 20% of the children had not received any specific oral hygiene instructions and many brushed their teeth only once a day [Citation34]. Whether this is similar in Swedish children and adolescents with DS is not known.
In Sweden, most children with DS live with their biological family. In other countries, the living arrangements for children with DS can differ. The form of living can affect the support to maintain oral hygiene [Citation26]. Also, the utilization of society’s different types of general support to children corresponds to which type of school the child attends. Children with DS can go to either elementary schools or special schools for children with intellectual disabilities. In Sweden, it is reported that families with a child with mild developmental disabilities who attend special classes more often utilize different types of support and interventions than those who attend elementary schools [Citation35]. Whether this also applies to dental services is, however, unclear.
The aim of this study was to describe Swedish parents’ perceptions of the oral and general health of their children with Down syndrome as well as the dental health care their children are receiving using the following research questions:
What are the parents’ perceptions of their child’s oral and general health?
What are the parents’ perceptions about the child’s dental health care?
Material and methods
A cross-sectional quantitative design was used. The questionnaire selected for this study was developed, validated and used in the previously mentioned Belgian study of oral health in children with DS [Citation34]. The Belgian questionnaire used questions from other internationally available questionnaires on a similar topic [Citation36–39].
Information about the study was posted on the Swedish Down Syndrome Society website (www.svenskadownforeningen.se) and their Facebook page. The society has approximately 480 members. Parents of a child with DS between 0 and 18 years of age were eligible to participate. They were informed that study participation was voluntary, and that the data would be handled with strict confidentiality. By answering the questionnaire, parents consented to participate in the study. Ethical approval was obtained from the Regional Ethics Committee for Human Research at Linköping University, Sweden 2016/425-31, in complete accordance with the World Medical Association Declaration of Helsinki.
Questionnaire
The original questionnaire was translated from English into Swedish by an authorized language examiner. The translation and back-translation were performed in several stages and reviewed until the consistency was achieved [Citation40]. To adapt to the Swedish context, some of the questions regarding dental treatment were modified and questions about dental visits to dental hygienists were added. To test the face validity of the questions, a first draft was proofread by five parents, who afterwards were interviewed about the content and layout of the questionnaire. Based on their suggestions, the questionnaire was revised with minor changes, e.g. different school settings and living conditions. These parents’ answers were excluded from the responses in the final study group. The questionnaire consisted of five parts and was available as a web survey. Part one included demographic data with socioeconomic and medical factors. Part two included questions about the child's dental health care visits, interactions between children and the dentist/dental hygienist and between the parent and the dentist/dental hygienist. The third part contained questions about oral hygiene. Part four included questions about oral problems based on a validated OADS (Oral Assessment in Down Syndrome) questionnaire [Citation36]. The parents’ rating of their child’s oral health from very poor to very good was also included. Lastly, the fifth part of the questionnaire concerned sociodemographic factors and the parents’ own oral health. The respondents had the opportunity to expand their answers through open questions related to the main questions. These answers will be analyzed using content analysis in another study by the authors of the present study.
Statistical analysis
All items had to be answered for the questionnaire to be considered valid. To make this feasible, a possible answer was always ‘I don’t know’. Data were analysed using the Statistical Package for the Social Sciences software program SPSS ver. 25.0 (SPSS Inc., Chicago, IL, USA). Chi-squared tests were used to test the association with categorical dependent variables. The level of significance was set as p < .05. Not significant p value was expressed as NS.
Results
Demographic factors
The questionnaire was completed by 101 parents of children with DS. 89% were completed by mothers and 11% by fathers. The parents’ age range was 28–58 years, mean age 42.8 (SD: 6.58). All 21 regions (counties) in Sweden were represented, although most of the children lived in the middle or south, which are also the most populated parts of the country. In these regions, there are about 3,550 public dental health clinics, including 40 paediatric dental specialist clinics. About 70% of the parents had a university/college degree. There were 52 boys and 49 girls and the children’s ages ranged between 1 and 19 years old (mean age: 9.6/SD: 4.7 years). The majority (87%) lived with both of their parents. About half of the children attended special schools, followed by 35% attending elementary schools while 16% were under school age. Almost all parents (94%) used the Swedish language to communicate with their children. Twenty percent also used signs or pictures as communication support.
Parents’ perceptions of their child’s general and oral health
The most common parent-reported medical conditions of the children with DS are listed in . Twenty percent (20%) had been referred to a hospital during the previous 12 months. The reasons for this varied, but pneumonia or planned surgery were the most common reasons.
Table 1. Medical problems in children with DS reported by their parents (n = 101).
The parents’ ratings of their children’s general and oral health are listed in . When comparing general health with oral health, most parents who reported their children to have good general health, also reported them to have good oral health or quite good oral health. Parents who reported that their children had poor or very poor oral health (8%), also reported that dental examinations and dental treatment were difficult procedures.
Table 2. General and oral health in children with DS as rated by their parents (n = 101).
Most parents indicated that they assisted their child with toothbrushing, and this parental assistance decreased as the child got older. Toothbrushing habits are presented in . Children who received their treatment at specialist dental clinics had more support in daily toothbrushing than children treated at general dental clinics, 77% and 68%, respectively (NS). Some parents (17%) reported that their children avoided specific hard food textures, such as carrots and apples. Moreover, difficulties sucking when being breast or bottle fed (52%) were reported. Difficulties drinking from a mug or choking while drinking or eating were reported by 7% and 9%, respectively.
Table 3. Toothbrushing habits of children with DS as reported by their parents (n = 101).
Parents’ perceptions of their child’s dental health care
Most children had seen a dentist during the previous 6 months (73%) or during the previous year (17%). Only one child had never been to a dental clinic, as the parents considered their child to be too young to cooperate. The main reason for children with DS having a dental appointment were oral examination, other common reasons were introduction and training for the child to participate in dental examinations and dental treatment (). Most children received their dental health care at public general dental health care (55%) and paediatric specialist clinics (53%). Only one child went to a private general dental clinic. There was no significant difference between children attending special schools and elementary schools related to utilization of specialist dental health care.
Table 4. Reasons for last dental visit, reported by parents of children with DS (n = 101). Other reasons for dental visits included introduction to and training in dental treatment, orthodontic and periodontal treatment. Respondents could give more than one reason.
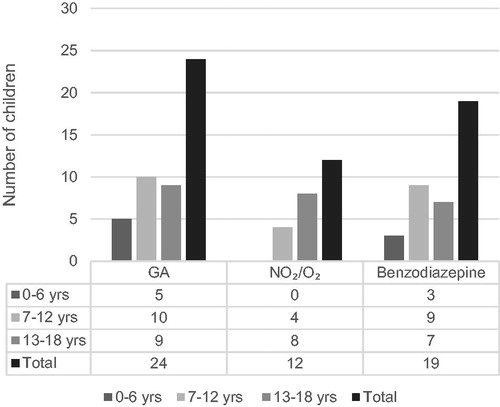
All children rated as having poor general health and those with ASD went to paediatric specialist dental clinics. In 35% of the families, the child with DS went to the same dentist as their siblings. Difficulties with dental examination were reported in 27% and dental treatment in 36% of the children. The number of children who had experienced dental treatment under sedation, by general anaesthesia (GA), N2O/O2 or Benzodiazepine, is presented in . The most common dental procedures performed under GA were dental examinations and scaling. Within the same GA session, 17% of the children had other health care interventions combined with dental treatment, e.g. blood samples, medical surgery and ear-nose-throat examination.
Figure 1. Number of children with DS who received dental treatment (DT) with sedation by General Anaesthesia (GA), N2O/O2 inhalation sedation or oral/rectal Benzodiazepine (n = 101).
Fifty-four percent (54%) of the parents indicated that they had received specific information about oral hygiene for their child from their dentist; 61% from a dental hygienist and 13% from other parents of children with DS. Other sources of information were family, friends, school and speech and language therapists. Information given in connection with a dental visit concerned oral hygiene (81%), recommendations about fluoride supplements (57%), dietary advice (31%) and information about tooth agenesis (30%).
Most parents (84%) were generally satisfied with their child’s dentist or dental hygienist. Among parents of children receiving dental health care in specialist clinics, 94% were satisfied compared to 70% in public general dental health care, p < .05. All parents had some experience of visiting a paediatric specialist dental clinic. The parents’ listing of what they wanted from their child’s dentist and dental hygienist is presented in . Parents who were not satisfied (7%) reported that the dentist or dental hygienist only spoke to them without involving the child (53%), lacked patience (40%), did not allow the child extra time if needed (37%) and did not explain the dental procedures (27%). Some parents highlighted the importance of the child being treated by the same dentist or dental hygienist over time. One parent suggested that the dental professional should contact the parents prior to every dental visit to agree on a suitable strategy. Children reported by their parents as having good oral health also had no or minor problems interacting with other people. There was no significant relation between having received dental treatment under GA and having difficulties interacting with people outside the family. Among children who had received paediatric dental specialist care, there was no significant difference between those who attended special schools (n = 49), elementary/secondary school (n = 35) or did not yet attend school (n = 16). Neither was any statistical difference found between school settings and how the parents rated their child’s general or oral health. Parents’ background factors, such as age, ethnicity, oral hygiene habits and education, did not affect how they rated their child's oral health, except for gender, where all the fathers (n = 10) who answered the questionnaire rated their child’s oral health as poor.
Table 5. Parents’ listings of what they want from a good dentist or dental hygienist treating their child with DS (n = 101). Respondents could select more than one option.
Discussion
Swedish children with DS received their dental health care at both general and specialist clinics. A majority of the parents rated their child’s general and oral health as good or very good. Those who rated their child’s oral health as poor, also reported that their child had difficulties with dental procedures. Most parents were satisfied with their child’s dentist/dental hygienist. However, parents of children in specialist dental clinics were more satisfied than those in general dental health care. Patience and engaging the child during treatment were the most appreciated qualities in dental professionals. Parents also highlighted the need for multidisciplinary collaboration and care coordination.
Limited access to dental professionals who specialize in children with disabilities may be a barrier to dental health care for this population [Citation22,Citation41]. In this study, however, about half of the children received their dental health care at paediatric dental specialist clinics and it is not known if access to specialist clinics was difficult or not. Since most of the children lived in parts of Sweden where paediatric specialist dental care is well organized, accessibility should not have been an issue. Also, all parents had some experience of visiting a paediatric specialist dental clinic. This is in line with the Swedish national medical guidelines for children with DS, which state that paediatricians should send an early referral to a dentist already when the child is 6 months old. Referrals from medical health care are usually directed to specialist dental clinics. The guidelines also emphasize the value of cooperation between specialist and general dental health care [Citation24].
In this study, no difference in specialist dental health care between those attending special schools or those in elementary schools was found. This finding is in contrast with findings by Olsson et al., where children attending special schools often utilized different types of support [Citation35]. That study did not, however, specifically address dental health care. The Belgian study by Descamps and Marks showed that it was common for children with DS to receive dental health care at a private clinic. Consequently, they were also more likely to meet the same dentist as their siblings than Swedish children with DS [Citation34]. Parents of children with DS in France reported problems accessing any dental health care and medical services. Thus, children with DS did not receive dental services to the same degree as their siblings without DS [Citation28]. These differences between countries likely reflect the differences in how dental health care is organized for children with disabilities.
Most parents also rated their child’s oral health as good in the study of Descamps and Marks [Citation34]. Most parents assisted their younger children with toothbrushing twice a day. Since children with DS, compared to other children, continue to need support with oral hygiene as they get older, their parents need to be informed [Citation28]. It is therefore satisfying that most parents in this study had received this information from dental professionals. Children within specialist dental health care had more support in daily toothbrushing than children treated at general dental clinics. This can be explained by the simple fact that dentists and dental hygienists working in paediatric specialist dental health care have extended experience and knowledge of functioning and oral health in children with disabilities.
In this study, most parents reported their child to have good general health, which is in line with what has been called the ‘disability paradox’ – good quality of life despite medical diagnoses [Citation42]. The same was seen by Faulks et al., where almost 90% of 218 studied children from four different countries had a significant medical diagnosis and still, almost 80% were reported by their parents as having good or very good physical health [Citation26]. The most common medical conditions reported in our study, visual and hearing problems, are conditions well known in individuals with DS. Children with ASD were also represented in this study. ASD as well as visual and hearing impairments together with intellectual disability can have a negative impact on communication [Citation26,Citation40].
In the present study, all children with ASD as an additional diagnosis were treated at paediatric specialist dental clinics, where alternative forms of supporting communication are used. However, all dental professionals would benefit from education in alternative communication, which is useful when communicating with children with disabilities as well as with children with dental fear, language difficulties and children in younger age groups [Citation43]. Alternative Augmentative Communication (AAC) covers all forms of nonverbal communication and includes facial expressions and gestures as well as the use of images, symbols, sounds or written text. For children with communication difficulties, AAC tools can be used to supplement or replace speech [Citation44,Citation45]. In addition to alternative communication, dental professionals benefit from having other strategic skills to help them interact with children with DS. Enhancing parental presence is one such strategy; however, it is important that communication is not done solely with the parent. Another strategy is the tell-show-do technique. The tell-show-do technique involves demonstration, explaining and practising each separate step of the examination or treatment [Citation46]. The willingness to allow extra time, to explain and involve the child in the dental procedure, along with patience, were in the parents’ views the most important qualities for a dentist or dental hygienist to have. These are also factors that are well known in paediatric specialist dental care and since dental treatment of children with DS often requires additional skills from the professionals [Citation25], it is not surprising that almost all parents of' children in paediatric specialist dental health care were satisfied. Thus, dental professionals need to know the spectrum of health problems and developmental differences commonly associated with DS and how they may influence oral health and dental health care [Citation26,Citation47]. It is also important to be aware that the diagnosis alone does not provide an accurate understanding of each individual child’s unique needs. Even if children with DS run an increased risk for oral diseases, they can maintain good oral health if preventive care starts early in life. Dental professionals in general dental health care also need to know when, and if, it is time to refer a child with DS to a specialist. It is reported that more than 60% of general dentists neither felt comfortable nor were prepared to treat patients with special needs [Citation48]. This is supported by a study which included 356 dentists in Belgium, where a representative sample of general dentists did not feel comfortable treating children with DS and often referred them to a specialist. The majority stated that they had not been instructed in how to treat children with DS during their dental educational training. About 50% indicated that additional training and education would be desirable [Citation25].
The UN Convention on the Rights of the Child states that all children have the same right to good oral health and dental health care [Citation21,Citation49]. To ensure that a child with DS has the same access to good oral health as other children, dental health care has to be adapted to meet the needs of the individual child and family [Citation50]. With person-centred care, interaction with each child is highlighted – regardless of communicative difficulties and other barriers – and is a prerequisite for optimal participation in dental health care procedures [Citation51].
The importance of meeting each child’s needs is made clear by many of the parents’ statements in this study. One of these, the wish for multidisciplinary collaboration and care coordination, depended a great deal on the organization of care in the region where the family lives. Health care interventions under GA combined with dental treatment are an example of collaboration that benefits the overall care of a child. The availability of dental GA is important in order to give children with DS the same prerequisites for good dental health care as other children [Citation26,Citation33]. Hallberg and Klingberg reported that oral health is not fully integrated into the medical care of children with disabilities. They also reported that dental and medical health care professionals as well as parents and individuals with a disability perceive that no one seems to take overriding responsibility for oral health in young adults with disabilities [Citation47]. Furthermore, inclusion of oral health within health care and supporting cooperation with other professionals may not only benefit the child and their parents but also society, e.g. fewer dental visits and increased school attendance [Citation26]. The economic perspective is important for both families and the broader health care system [Citation52]. In order to highlight the impact of general health on oral health in children with need of special care, on different levels, interprofessional collaboration should be integrated into educational programs for both dental and health care professionals.
Parents who rated their child’s oral health as poor also reported that their child had difficulty with dental examinations and dental treatment. In a study by Norderyd et al., children with limitations in their interpersonal interactions and relationships were more likely to have had dental treatment under GA. In the present study, however, no such relation was found. The reason for this may be that in the study by Norderyd et al., only about 25% of the children with disabilities had DS [Citation27].
Findings from this study support the need to include individuals with DS and their families in future research projects concerning oral health in children with DS. Parents’ expertise and knowledge about oral health and dental health care in general and in children with DS in particular, needs to be acknowledged and valued. To make parents’ and children’s voices heard, we suggest that future research takes an inclusive approach. In inclusive research design, children with DS and their care providers are involved in all steps of the research process from designing the data collection to interpreting data and disseminating results [Citation53].
Limitations of the study
Differences in cultural context, country-specific organization of dental health care, access to paediatric dental specialist clinics and different study methods [Citation28,Citation29,Citation32,Citation34,Citation41] make our results on parents’ perception of dental health care for their children with DS difficult to compare with findings from other studies. Distributing a questionnaire online to collect data enables contact with participants in distant locations and enables efficient use of research time and effort. The disadvantages of this type of data collection include uncertainty regarding data validity and sampling issues [Citation54]. One important limitation is the study sample. Participants were recruited by the Swedish Down Syndrome Society website (www.svenskadownforeningen.se) or by their Facebook page. Parents that are members of the Society are likely informed and motivated and probably, prioritize participation in research. The collected data can therefore not be seen as representative for all parents to children with DS in Sweden and the findings can, thus, not be generalized. If detailed demographic information about socioeconomic factors had been collected, it could have been used to explain the data, as it is well known that socioeconomic factors impact both general and oral health [Citation55,Citation56]. However, findings in this study may, despite its limitations, display useful results and information. To make future studies more representative, we suggest a larger number of participants and detailed demographic data to be collected.
Conclusion
Most parents rated both the general and the oral health of their child with DS as good to very good. Children with oral health rated as poor were also reported to have difficulties participating in dental examination and treatment. Patience, willingness to spend extra time, and to explain and include the child in conversations were the abilities in dental health care professionals that were most highly valued by the parents. They also preferred their child to receive dental health care from professionals who specialized in children with disabilities. Dental professionals who adapt their care to fit the unique needs of each child with DS are likely to provide higher quality care and to enable better oral health for these children.
Acknowledgements
The authors are grateful to all parents, to Sazan Lindh for her contribution to the work with the questionnaire and Erjona Halitaj for her help with the data collection.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Socialstyrelsen, Fosterskador och kromosomavvikelser [Internet]. 2014. [cited 2020 Feb 14]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2016.
- Aldossary M. Down syndrome: a review for the dental professionals. IOSR JDMS. 2017;16(07):61–66.
- Lewis MP, Bell EB, Evans AK. A comparison of tympanometry with 226 Hz and 1000 Hz probe tones in children with Down syndrome. Int J Pediatr Otorhinolaryngol. 2011;75(12):1492–1495.
- Söderman L, Nordlund M, Lindahl H. Utvecklingsstörning/funktionshinder. Stockholm: Liber; 2005.
- Durhan MA, Agrali OB, Kiyan E, et al. Does obstructive sleep apnea affect oral and periodontal health in children with Down syndrome? A preliminary study. Niger J Clin Pract. 2019;22(9):1175–1179.
- Ghaith B, Al Halabi M, Khamis A, et al. Oral health status among children with Down Syndrome in Dubai, United Arab Emirates. J Int Soc Prevent Communit Dent. 2019;9(3):232–239.
- Hyder M, Tanboga I, Kalyoncu I, et al. Are Down syndrome children more vulnerable to tooth wear?. J Intellect Disabil Res. 2019; 63(11):1324–1333.
- Areias C, Sampaio-Maia B, Macho V, et al. Oral health in Down syndrome, health problems in Down syndrome. In: Dey S, editor. Prenatal diagnosis and screening for Down syndrome. London: IntechOpen; 2015. p. 45–68.
- Macho V, Coelho A, Areias C, et al. Craniofacial features and specific oral characteristics of Down syndrome children. Oral Health Dent Manag. 2014; 13(2):408–411.
- Anil MA, Shabnam S, Narayanan S. Feeding and swallowing difficulties in children with Down syndrome. J Intellect Disabil Res. 2019;63(8):992–1014.
- Diéguez-Pérez M, de Nova-Garcia MJ, Mourelle-Martinez MR, et al. Oral health in children with physical (Cerebral Palsy) and intellectual (Down syndrome) disabilities: systematic review 1. Clin Exp Dent. 2016;8(3):337–343.
- Doriguêtto P, Carrada CF, Scalioni F, et al. Malocclusion in children and adolescents with Down syndrome: a systematic review and meta-analysis. Int J Paediatr Dent. 2019;29(4):524–541.
- Marques LS, Alcântara CEP, Pereira LJ, et al. Down syndrome: a risk factor for malocclusion severity. Braz Oral Res. 2015;29:44–47.
- Bauer D, Evans CA, Begole E, et al. Severity of occlusal disharmonies in Down syndrome. Int J Dent. 2012;2012(1):872367. Epub 2012 Aug 15.
- Lee CF, Lee CH, Hsueh WY, et al. Prevalence of obstructive sleep apnea in children with Down syndrome: a meta-analysis. J. Clin Sleep Med. 2018;14(05):867–875.
- Amaral Loureiro AC, Oliveira Costa F, Eustáquio da Costa J. The impact of periodontal disease on the quality of life of individuals with Down syndrome. Downs Syndr Res Pract. 2007;12(1):50–54.
- Mohiddin G, Narayanaswamy AB, Masthan KMK, et al. Oral candidal and streptococcal carriage in Down syndrome patients. J Nat Sci Biol Med. 2015;6(2):300–305.
- Marro F, Fernandez C, Martens L, et al. Erosive tooth wear in special Olympic athletes with intellectual disabilities. BMC Oral Health. 2019;19(1):37.
- Deps T, Angelo G, Martins C, et al. Association between dental caries and Down syndrome: a systematic review and meta-analyses. PLoS One. 2015;10(6):e0127484.
- Hennequin M, Faulks D, Veyrune JL, et al. Significance of oral health in persons with Down syndrome: a literature review. Dev Med Child Neurol. 1999;41(4):275–283.
- SFS. 1985. National Dental Service Act [Tandvårdslag]. Stockholm: Socialdepartementet; 1985. p. 125.
- Klingberg G, Andersson-Wenckert I, Grindefjord M, et al. Specialist paediatric dentistry in Sweden 2008 – a 25-year perspective. Int J Paediatr Dent. 2010;20(5):313–321.
- Koch G, Poulsen S, Twetman S. Caries prevention. Pediatric dentistry: a clinical approach. Chichester: Wiley-Blackwell; 2017. p. 114–129.
- Annerén G, Wester Oxelgren K, Jahnke, et al. Downs syndrome: medical guidelines for children 0-18 years. 2013;(3):5–6. [In Swedish]
- Norderyd J, Lillvist A, Klingberg G, et al. Oral health, medical diagnoses, and functioning profiles in children with disabilities receiving paediatric specialist dental care - a study using the ICF-CY. Disabil Rehabil. 2015;37(16):1431–1438.
- Norderyd J, Klingberg G, Faulks D, et al. Specialised dental care for children with complex disabilities focusing on child's functioning and need for general anaesthesia. Disabil Rehabil. 2017;39(24):2484–2491.
- Descamps I, Fernandez C, Van Cleynenbreugel D, et al. Dental care in children with Down syndrome: a questionnaire for Belgian dentists. Med Oral. 2019;24(3):e385.
- Scalioni F, Carrada CF, Abreu L, et al. Perception of parents/caregivers on the oral health of children/adolescents with Down syndrome. Spec Care Dentist. 2018;38(6):382–390.
- Case A, Paxson C. Parental behavior and child health. Health Aff (Millwood). 2002;21(2):164–178.
- Skeie M, Espelid P, Riordan PJ, et al. Caries increment in children aged 3-5 years in relation to parents' dental attitudes: Oslo, Norway 2002 to 2004. Community Dent Oral Epidemiol. 2008;36(5):441–450.
- Kramer A, Hakeberg M, Petzold M, et al. Demographic factors and dental health of Swedish children and adolescents. Acta Odontol Scand. 2016;74(3):178–185.
- Oliveira A, Pordeus I, Luz C, et al. Mothers' perceptions concerning oral health of children and adolescents with Down syndrome: a qualitative approach. Eur J Paediatr Dent. 2010;11(1):27–30.
- Randell D, Harth S, Seow W. Preventive dental health practices of non-institutionalized Down syndrome children: a controlled study. I. Clin Pediatr Dent. 1992;16(3):225–229.
- Descamps I, Marks L. Oral health in children with Down syndrome: Parents’ views on dental care in Flanders (Belgium). Eur J Paediatr Dent. 2015;16(2):163–168.
- Olsson LM, Elgmark Andersson E, Granlund M, et al. Social service utilisation patterns among children with mild intellectual disability–differences between children integrated into mainstream classes and children in self-contained classes. Eur J Special Needs Educ. 2015;30(2):220–236.
- Allison PJ, Hennequin M. The oral assesment in Down syndrome questionnaire (OADS) Development of an instrument to evaluate oral health problems in individuals with Down syndrome. Community Dent Health. 2000;17(3):172–179.
- Collado V, Faulks D, Hennequin M. A survey of the difficulties encountered during routine hygiene and health care by persons with special needs. Disabil Rehabil. 2008;30(14):1047–1054.
- Kaye PL, Fiske J, Bower EJ, et al. Views and experiences of parents and siblings of adults with Down syndrome regarding oral healthcare: a qualitative and quantitative study. Br Dent J. 2005;198(9):571–578.
- Allison PJ, Hennequin M, Faulks D. Dental care access among individuals with Down syndrome in France. Spec Care Dentist. 2000;20(1):28–34.
- Streiner D, Norman G, Cairney J. Health measurement scales: a practical guide to their development and use. USA: Oxford University Press; 2015.
- Norderyd J, Faulks D, Molina G, et al. Which factors most influence referral for restorative dental treatment under sedation and general anaesthesia in children with complex disabilities: caries severity, child functioning, or dental service organisation? Int J Paediatr Dent. 2018;28(1):71–82.
- Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 1999;48(8):977–988.
- Espinoza KM, Heaton L, Baylor C. Communication with children with special healthcare needs in dental practice. Dental Care for Children with Special Needs. Cham: Springer; 2019. p. 51–75.
- Beukelman DR, Mirenda P. Augmentative and alternative communication: supporting children and adults with complex communication needs. Baltimore: Paul H. Brookes Pub; 2013.
- Grewal N, Sethi T, Grewal S. Widening horizons through alternative and augmentative communication systems for managing children with special health care needs in a pediatric dental setup. Spec Care Dentist. 2015;35(3):114–119.
- Adair SM. Behavior management conference panel I report - rationale for behavior management techniques in pediatric dentistry. Pediatr Dent. 2004; 26(2):167–170.
- Hallberg U, Klingberg G. Medical health care professionals' assessments of oral health needs in children with disabilities: a qualitative study. Eur J Oral Sci. 2005;113(5):363–368.
- Dao L, Zwetchkenbaum S, Inglehart M. General dentists and special needs patients: does dental education matter? J Dent Educ. 2005;69(10):1107–1115.
- UNCRC. United Nations Convention on the Rights of the Child. Office of the United Nations High Commissioner for Human Rights. [Internet]. 1989. [cited 2020 Feb 5]. Available from: https://www.ohchr.org/en/professionalinterest/pages/crc.aspx.
- Nilsson S, Bjorkman B, Almqvist AL, et al. Children's voices differentiating a child perspective from a child's perspective. Dev Neurorehabil. 2015;18(3):162–168.
- Cardiff S, McCormack B, McCance T. Person-centred leadership: a relational approach to leadership derived through action research. J Clin Nurs. 2018;27(15-16):3056–3069.
- Peres MA, Macpherson LM, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–260.
- Nind M. The practical wisdom of inclusive research. Qual Res. 2017;17(3):278–288.
- Wright KB. Researching Internet-based populations: advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. J Comput Mediated Commun. 2006;10(3):00–00.
- Schwendicke F, Dörfer CE, Schlattmann P, et al. Socioeconomic inequality and caries: a systematic review and meta-analysis. J Dent Res. 2015;94(1):10–18.
- Allen L, Williams J, Townsend N, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5(3):e277.
