Abstract
This study assessed the effect of Attention-Deficit Hyperactivity Disorder (ADHD) training on teachers’ knowledge and perception of the condition in Kano, Nigeria. It was a controlled trial of 200 primary schoolteachers from two Local Government Areas (LGAs). One LGA was randomly assigned to the intervention group and the other to a waitlist control (100 teachers per group). The intervention group received two training sessions on ADHD one week apart. The training was based on the Mental Health Gap Action Programme – Intervention Guide (mhGAP-IG). Participants completed the ADHD Knowledge Questionnaire, ADHD Attitude Scale, and Knowledge of Behavioral Intervention Questionnaire at baseline and one-week post-intervention. The participants ranged from 17 to 58 years (Mean = 34.1 years; SD = 8.7), comprising 112 females and 85 males. The intervention and control groups were broadly similar at baseline. Controlling for baseline scores and other differences (age, gender, duration of teaching experience, and if schools employed staff dedicated to helping children with mental health difficulties such as ADHD), the intervention group had significantly higher scores on Knowledge of ADHD and Knowledge of Behavioral Management of the condition, with effect sizes of 0.7 and 0.3, respectively. This intervention led to statistically significant improvements in the teachers’ knowledge of ADHD and behavioral intervention for ADHD. This provides further evidence of the feasibility and effectiveness of specific ADHD-training interventions for primary school teachers in Nigeria.
Introduction
Attention-Deficit Hyperactivity Disorder (ADHD) is the commonest neurodevelopmental disorder affecting 5% of children and adolescents (Polanczyk et al., Citation2014). It is associated with significant morbidity and disability, especially when untreated (Baranne and Falissard Citation2018; Belfer, Citation2008; Srinath et al., Citation2010). ADHD is particularly challenging for affected children in educational settings leading to academic underachievement, subsequent occupational dysfunction (Usami, Citation2016), and long-term socioeconomic burden (Galéra et al., Citation2012).
Teachers have a crucial role in recognizing and providing support for children affected by ADHD (Moldavsky et al., Citation2014). For example, teachers support the ADHD diagnostic assessment by providing evidence of impairment in educational settings, one of the diagnostic criteria (American Psychiatric Association, Citation2013). Studies show that teachers’ attitude toward ADHD therapeutic modalities significantly impacts the use of ADHD classroom management strategies and students’ behavioral outcomes (Sherman et al., Citation2008). Also, teachers with good knowledge of ADHD display a more positive attitude and behavior toward the condition (Ohan et al., Citation2008). Studies of children affected by ADHD show a desire for teachers to better understand their needs and their specific learning challenges to support them in achieving better educational outcomes (Kendall, Citation2016). These findings provide strong support for a continuing need for ADHD-focused psychoeducation for teachers.
A recent systematic review of ADHD-focused psychoeducational interventions for parents, teachers, and children and adolescents with ADHD found moderate to large effect sizes on outcomes such as improved knowledge about ADHD (Dahl et al., Citation2020). Another systematic review and meta-analysis demonstrated the effectiveness of ADHD teacher training interventions in improving teachers’ knowledge and pupils’ outcomes (Ward et al., Citation2022). However, despite this evidence, there are still limited studies of ADHD-focused teacher training programs in Africa. For example, of the 29 studies in the meta-analysis by Ward et al. (Citation2022), only four studies were from Africa, of which only one was from Nigeria. On the contrary, studies from Nigeria and other African countries continue to evidence teachers’ poor knowledge of ADHD and negative attitudes toward affected children and young people (Adeosun et al., Citation2013; Lasisi et al., Citation2017; Woyessa et al., Citation2019). For example, a study of Nigerian primary school teachers found that only 9% and 16% of participants endorsed that ADHD could be managed with medications and psychological therapies, respectively (Adeosun et al., Citation2013). Similarly, a recent study of Ethiopian primary school teachers found widespread misconceptions about ADHD, including 68% who suggested that affected students should be placed into part-time special education (Woyessa et al., Citation2019).
The persisting low levels of knowledge and poor attitude toward ADHD among teachers in Nigeria and other parts of Africa indicate a continuing need for ADHD-focused psychoeducation interventions in the region. Otherwise, children with ADHD will continue to go unrecognized and unsupported in school in these regions of the world. In some cases, children with ADHD may be subjected to corporal punishment in schools (Mohammed, Citation2018). Unfortunately, this is a practice that is still common in Nigeria (Alhassan, Citation2013) and other Low and Middle-Income Countries (LMICs) (Gershoff, Citation2017). Given that ADHD affects 5% of school-age children, this amounts to millions of children in the region who are at risk of unsatisfactory schooling experience due to their teachers’ poor knowledge and attitude toward ADHD. Education policymakers need replicable evidence of both the efficacy and feasibility of ADHD-focused teacher training programmes before adopting them as routine practice in Nigerian schools. To date, there has been only one previous study of an effective ADHD-focused teacher training programme in Nigeria (Lasisi et al Citation2017). The current study extends that work to another part of the country with a larger sample of teachers.
Methods
Study design and location
This was a parallel two-group controlled trial with an intervention and a wait-list control group. The study was conducted in Kano, one of Nigeria’s largest cities. Two Local Government Areas (LGAs) (Kumbotso and Ungoggo) that were furthest apart were purposively selected. Balloting was used to assign one LGA (Kumbotso) as intervention and the other (Ungoggo) as waiting list control. Eight public and 20 private primary schools with the highest populations of teachers in both LGAs, were selected for the study. Ethical approval was given by the Health Research Ethics Committee of the Kano State Ministry of Health. Permission was obtained from the Kano State Universal Basic Education Board, Kano State Private and Voluntary Institutions Board, and the Headteachers of the participating schools. Participating teachers gave written informed consent.
Participants
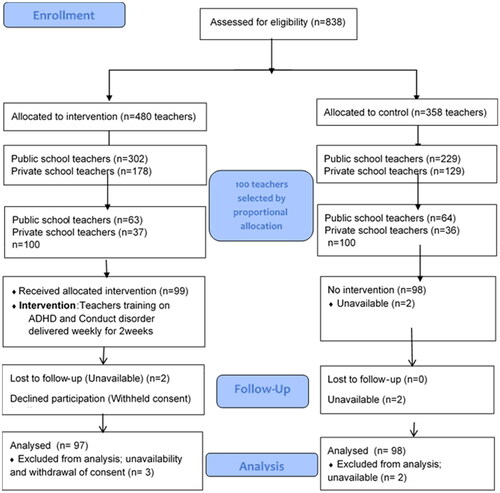
Participants were teachers currently teaching in the selected public and private primary schools. Primary schools in the intervention and control LGAs were stratified into public and private schools and by the population of teachers. The top 10% of public and private schools with the most population of teachers in each LGA were selected. This resulted in eight public and 20 private schools from each LGA. The sample size of 200 teachers (100 each from intervention and control LGAs) was selected based on the population of teachers in each school. Participants sampling was stratified by school type and teacher population to reduce the risk of selection bias, thereby allowing an adequate sample size per stratum to provide more precise estimations. This is especially relevant as Nigerian public and private schools have distinct profiles concerning size, operational quality, and opportunities for professional development. The individual participants from each school were selected by Computer Generated Random Numbers. Prior Power calculation identified that a sample of 63 in each group would be sufficient to identify a difference of 0.5 standard deviations in post-intervention ADHD knowledge scores between the intervention and control groups with 80% power and 5% two-sided alpha (Noordzij et al., Citation2010). The sample size was increased to 100 in each group to allow for attrition. One teacher in the intervention group declined to participate and two were lost to follow-up. Two teachers in the control group were unavailable at the follow-up ().
Procedures
The training manual was adapted from the behavioral module of the World Health Organization Mental Health Gap Action Programme Intervention Guide (mhGAP-IG)-Version 2.0 (WHO, Citation2016). The content on ADHD was modified to make it more readily accessible for primary school teachers in the setting, by removing pharmacological interventions and complex psychosocial intervention components. Special attention was paid to the “Advice for teachers” section of the training manual, emphasizing their powerful role in children’s life. Examples include, “Establish short, simple classroom rules, stating them in positive terms that convey what you want students to do”, “Make classroom activities consistent and predictable” and “Ask the child to sit at the front of the class”. The simplified version was reviewed by the investigators for face validity. The teachers were taught to recognize the symptoms of ADHD, as well as classroom strategies for managing children with ADHD. The training was delivered by the first author who is a psychiatrist and a certified trainer on the use of the mhGAP-IG. The training was delivered in two sessions one week apart, in large groups of 99 teachers in the first session and 97 teachers in the second session. Each session lasted three hours with regular breaks for refreshments. A large group approach was adopted to test the feasibility of large-scale delivery given the shortage of certified mhGAP-IG trainers in Nigeria. The sessions involved workshop-style interactive presentations and group discussions. It included a hypothetical vignette depicting a child with an ADHD diagnosis based on the DSM 5 criteria (American Psychiatric Association, Citation2013). The training was delivered in English and Hausa, as the trainer and all the teachers were fluent in both. Attrition was minimized by prompting participants through text messages and phone calls. The control group received no training during the study. The intervention and control groups completed the post-intervention outcome measures a week after the second intervention session. Upon establishing the intervention was helpful, the wait-list control was also given the same training package.
Outcome measures
Five instruments were used in this study, namely a sociodemographic questionnaire, an ADHD Knowledge Questionnaire and case vignettes, an ADHD Attitude Scale, a Knowledge of Behavioral Intervention for ADHD, and Client Satisfaction Questionnaire. The instruments were piloted among 100 teachers from nonparticipating schools in a different LGA, and their feedback was used to adjust the questionnaires.
Sociodemographic Questionnaire
This questionnaire elicited information about the participants’ personal characteristics as shown in . Information was also sought on the duration of their teaching experience and previous training on childhood mental disorders.
Table 1. Socio-demographic characteristics of participants in intervention and control groups.
ADHD Knowledge Questionnaire and case vignettes
This 27-item questionnaire evaluated the teachers’ knowledge of the symptoms, nature, causes, course, and outcome of ADHD (Kos, Citation2004). Participants responded to each question as “True”, “False”, or “Don’t Know”. The scoring was dichotomized such that correctly answered items were scored as “1” and summed to create a Knowledge Scale such that higher scores indicate better knowledge of ADHD (range 0–27). The scale showed good internal consistency (Kuder–Richardson 20 = 0.79) (Kuder & Richardson Citation1937).
In addition to the Knowledge questionnaire, participants were given two vignettes. The first was a child with difficulties matching the DSM 5 criteria for ADHD, and the second matched the requirements for a Conduct Disorder. At baseline, participants in both groups were asked to identify which of the two children presented with ADHD symptoms. This was repeated after the intervention.
ADHD Attitude Scale
The ADHD Attitude Scale was adapted from a 131-item multi-domain ADHD Questionnaire (Kos, Citation2004). Thirty items with good face validity for assessing attitudes toward ADHD were selected. Piloting led to 22 items being adopted for the study. Participants responded to each item on a 5-item Likert scale: “strongly disagree,” “disagree,” “not sure,” “agree,” and “strongly agree”. Responses (strongly disagree/disagree OR agree/strongly agree) that indicate a negative attitude toward ADHD were scored “1” and summed to create an Attitude Scale. Higher scores indicate a more negative attitude. The scale showed good internal consistency in this study (Cronbach’s alpha, 0.88).
Knowledge of behavioral intervention questionnaire
This 12-item questionnaire assessed the teachers’ knowledge of classroom behavioral interventions for children with ADHD (Lasisi et al., Citation2017). Participants responded to each item as “True”, “False”, or “Don’t Know”. The scores were dichotomized, so that correct answers were scored as “1” and summed so that higher scores indicate higher knowledge (range 0–12). The scale had acceptable internal consistency in the current study (Kuder-Richardson 20 = 0.7).
Client satisfaction questionnaire
Participants were asked to indicate to what extent they agreed or not with aspects of the program, including whether the workshop met their expectations, if the information was clearly presented, whether the workshop was valuable and whether the workshop increased their confidence in teaching students with ADHD. Participants rated these items on a five-point Likert scale from “Strongly agree” to “Strongly disagree”.
Data management
Data were analyzed with Statistical Package for the Social Sciences (SPSS) Version 23. Continuous variables are presented as Means and Standard Deviations, while categorical variables are described as frequencies and proportions. A per-protocol analysis was adopted for comparisons of outcome measures due to the minimal, random, and near-equal losses to follow-up in both groups (3 intervention and 2 control participants); more so in the context of sample sizes that were much larger (100 in each group) than was required from the Power calculation (63 in each group). Between-group comparisons of intervention and control groups were made with student t-tests for continuous variables and a Chi-square test for categorical variables. The treatment effect was assessed with an analysis of covariance (ANCOVA) of post-intervention scores on outcome measures controlling for the respective baseline scores. Pre-post-intervention change in correct classification of the ADHD case vignette was assessed with the Chi-Square test. Effect sizes were calculated as Cohen’s d with 0.2, 0.5 and 0.8 considered small, medium and large, respectively (Cohen, Citation1988). The level of significance was set at 0.05 two-tailed for all tests. Qualitative comments in the client satisfaction questionnaire were analyzed thematically.
Results
Demographic characteristics of the study participants
The participants consisted of 112 (56.9%) females and 85 (43.1%) males. Their age ranged from 17 to 58 years (Mean = 34.1 years; SD = 8.7). shows that the intervention and control groups had similar socio-demographic characteristics except that the intervention group were significantly younger, had more females, had been teaching for fewer years, and were more likely to have staff employed to help children with ADHD or other mental health problems.
Baseline scores on outcome measures
shows that the intervention and control groups had similar baseline scores on the ADHD Knowledge Questionnaire {(Mean = 13.64; SD = 3.65) vs (Mean = 13.48; SD = 3.52), t = −0.31, df 193, p = .756}, and Knowledge of Behavioral Intervention for ADHD {(Mean = 6.96; SD = 1.77) vs (Mean = 6.66; SD = 1.62), t = −1.22, df 193, p = .226}. However, the control group scored significantly higher (more negative attitude) on the ADHD Attitude Scale than the intervention group {(Mean = 68.17; SD = 8.04) vs (Mean = 65.16; SD = 7.81), t = 2.65, df 193, p = .009}. At baseline, 22% of the intervention group correctly recognized the ADHD case vignette compared with 30% of the control group (X2 = 0.68, df 1, p = .409).
Table 2. Between-group comparison of baseline scores on outcome measures.
Effects of the intervention
Between-group comparison of post-intervention scores on the outcome measures showed that the intervention group had significantly higher ADHD Knowledge {(Mean = 17.85; SD = 3.30) vs (Mean = 13.21; SD = 3.81), t = −9.08, df 193, p = .001}, and higher Knowledge of Behavioral Intervention for ADHD {(Mean = 7.64; SD = 2.00) vs (Mean = 6.60; SD = 2.03), t = −3.59, df 193, p = .001}. However, the intervention group also had significantly higher score on the ADHD Attitude Scale (more negative attitude) than the control group (less negative attitude) {(Mean = 69.85; SD = 8.80) vs (Mean = 67.09; SD = 8.17), t = −2.27, df 193, p = .025} (). Post-intervention 54.9% of the intervention group correctly recognized the ADHD case vignette compared with 35.7% of the control group (X2 = 4.08, df 1, p = .043).
Table 3. Between-group comparison of post-intervention scores on outcome measures.
Analysis of covariance (ANCOVA) () showed that after controlling for their respective pre-intervention scores (along with other demographic differences between the groups), the intervention was associated with statistically significant improvement in the treatment group’s Knowledge of ADHD {F (1, 188) = 68.7, p < .001, Cohen’s effect size (d) = 0.7}, and Knowledge of Behavioral Intervention for ADHD {F (1, 187) = 7.19, p < .001, Cohen’s effect size (d) = 0.3}. However, the intervention was also associated with a significant increase in the treatment group’s ADHD Attitude Scale score (more negative attitude) {F (1, 188) = 4.6, p = .033}.
Table 4. Analysis of covariance (ANCOVA) results and effect sizes.
Participants’ level of satisfaction with the intervention (N = 98)
The intervention group indicated high levels of satisfaction with the training program. The vast majority (96.9%) of the participants endorsed that the workshop met their expectations. Almost all indicated that attending the workshop was valuable (99%) and that the workshop had increased their confidence in teaching pupils with ADHD (98%). For example, a participant reported, “We are now well-armed with knowledge of how to deal with these children.” Others commented, “The workshop has increased our confidence to deal with children with ADHD” and “I understand how to care for pupils with ADHD and that beating doesn’t solve the problem.” A participant who was not fully satisfied noted that they would like autism and intellectual disability to be considered in future training.
Discussion
This controlled intervention study of the effectiveness of a training program for improving the knowledge and perception of ADHD among primary school teachers in Kano–Nigeria found significantly improved knowledge of ADHD. Post-intervention, 54.9% of the treatment group correctly identified the ADHD case vignette compared with 35.7% of the control group. The intervention group also had a significant improvement in their knowledge of behavioral intervention for ADHD. Despite the short duration, large group format, and low intensity of the intervention, statistically significant beneficial effects were found in these two knowledge outcome measures.
These findings are consistent with studies of similar programs in other parts of the world. For example, a recent systematic review of psychoeducational interventions for parents, teachers, and children and adolescents with ADHD reported improved knowledge of ADHD for all groups (Dahl et al., Citation2020). Similarly, a meta-analysis of ADHD teacher training interventions found improved teachers’ knowledge and pupils’ outcomes (Ward et al., Citation2022). The effect sizes for improved ADHD knowledge and Knowledge of Behavioral Intervention in the current study (0.7 and 0.3, respectively) are similar to a recent study among Nigerian primary school teachers (Lasisi et al., Citation2017).
However, the current training program was associated with an increase in the intervention group’s negative attitude toward ADHD. It could be that the intervention group’s increased awareness of the potential difficulties associated with ADHD might have led to an increased negative attitude toward the condition. This suggests that future intervention studies aimed at improving knowledge of ADHD should specifically and proactively include components to address negative attitudes toward the condition. One potential strategy based on “contact theory” is for the training to include actual contact and interaction with a person affected by ADHD. It has been argued that contact-based education is one of the more effective interventions for reducing negative attitudes toward mental illness (Stuart et al., Citation2014; Thornicroft et al., Citation2016).
Unlike Lasisi et al., where 39.5% and 60.5% of the intervention and control participants, respectively, reported having had previous training on ADHD, in our sample, the figures were 12.4% and 15.3%. Thus, it is possible that in the study by Lasisi and colleagues, the participants’ high prior exposure to ADHD led to a more in-depth understanding and more favorable attitudes toward the condition following their re-exposure to information about the condition. On the contrary, most participants in our study had not had previous exposure to ADHD. Thus, their becoming aware for the first time about the potential difficultes related to the condition may have increased their negative attitudes before they could internalize the additional information such as that the condition is treatable and a negative outcome is not inevitable. Furthermore, in Lasisi et al’s study, the participating teachers were selected by their headteacher, so it was possible that the headteachers selected teachers who had already shown interest in the condition and were more favorably disposed to it. This is in contrast to our study where participants were randomly selected.
The improvement in the teachers’ Knowledge of the Behavioral management of ADHD is important. Teachers’ behavior management strategies in Nigerian schools are still predominantly based on corporal punishment (Alhassan, Citation2013; Gershoff, Citation2017). This practice remains widespread in the country despite the large body of evidence of the deleterious effects on children (Alhassan, Citation2013; Ani and Grantham-McGregor, Citation1998; Fakunmoju & Bammeke, Citation2015). The core symptoms of ADHD such as hyperactivity and impulsivity increase the likelihood that affected children may infringe on class rules due to a low level of behavior regulation. Therefore, such children are more likely to receive harsh disciplinary practices, including corporal punishment. Thus, increasing the teacher’s recognition of ADHD and improving their knowledge of alternative, effective and nonphysical strategies for managing the children’s behavior could have a positive effect on affected children’s schooling experience.
The finding of positive intervention effects on ADHD knowledge, and Knowledge of Behavioral intervention for ADHD with this short intervention (2 sessions of 3 hours one week apart) suggests that a similar programme could be readily integrated into ongoing continuing development courses for teachers as well as incorporated into trainee-teachers curriculum with minimal extra resources. This is particularly pertinent given that most of the teachers in both groups indicated limited prior exposure to training about ADHD.
The findings of this study should be interpreted in light of the following limitations. First, the teachers were not individually randomly allocated to the intervention or control groups. This could have introduced bias resulting in, for example, unbalanced groups in terms of the employment of staff to help children with ADHD. Thus, a better study design could have been a cluster randomized controlled trial with the schools as the unit of randomization as opposed to the teachers. However, this design was not feasible due to limited resources.
Secondly, the post-intervention outcome measures were obtained once, a week after the last training session. This means that the sustainability of the improvement in knowledge is uncertain. Thus future studies should assess the long-term sustainability of the intervention by including longer-term follow-up assessment at multiple time points. Third, our use of the same case vignettes at baseline and post-test may have introduced some test re-test bias, although this would have been the case for both the intervention and control groups. Finally, the use of a waitlist control group is known to increase the apparent effect of interventions (Cunningham et al., Citation2013).
In conclusion, this training program on ADHD improved the teachers’ knowledge of ADHD and their Knowledge of Behavior management of the condition. The intervention was well-received, and the findings strengthen the local evidence base for its efficacy and feasibility. Thus, consideration should be given to including similar training on ADHD for teachers’ continuous development programmes and in teacher training Colleges. However, future training programmes on ADHD knowledge should consist of a specific component such as actual contact with a person with ADHD to also improve the teachers’ attitude toward students with ADHD.
Acknowledgement
The authors would like to thank the schoolteachers for participating in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article.
Additional information
Funding
References
- Adeosun, I., Ogun, O., Fatiregun, O., & Adeyemo, S. (2013). The attitude of Nigerian primary school teachers to children with attention deficit hyperactivity disorder. European Psychiatry, 28, 1. https://doi.org/10.1016/S0924-9338(13)76428-9
- Alhassan, A. B. (2013). School corporal punishment in Ghana and Nigeria as a method of discipline: A psychological examination of policy and practice. Journal of Education and Practice, 4(27), 137–147.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). APA. https://doi.org/10.1176/appi.books.9780890425596
- Ani, C. C., & Grantham-McGregor, S. (1998). Family and personal characteristics of aggressive Nigerian boys: Differences from and similarities with Western findings. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 23(5), 311–317. https://doi.org/10.1016/s1054-139x(98)00031-79814393
- Baranne, M. L., & Falissard, B. (2018). Global burden of mental disorders among children aged 5-14 years. Child and Adolescent Psychiatry and Mental Health, 12(1), 19. https://doi.org/10.1186/s13034-018-0225-4
- Belfer, M. L. (2008). Child and adolescent mental disorders: The magnitude of the problem across the globe. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 49(3), 226–236. https://doi.org/10.1111/j.1469-7610.2007.01855.x
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates.
- Cunningham, J. A., Kypri, K., & McCambridge, J. (2013). Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Medical Research Methodology, 13(1), 150. https://doi.org/10.1186/1471-2288-13-150
- Dahl, V., Ramakrishnan, A., Spears, A. P., Jorge, A., Lu, J., Bigio, N. A., & Chacko, A. (2020). Psychoeducation interventions for parents and teachers of children and adolescents with ADHD: A systematic review of the literature. Journal of Developmental and Physical Disabilities, 32(2), 257–292. https://doi.org/10.1007/s10882-019-09691-3
- Fakunmoju, S. B., & Bammeke, F. O. (2015). Anxiety disorders and depression among high school adolescents and youths in Nigeria: Understanding differential effects of physical abuse at home and school. Journal of Adolescence, 42(1), 1–10. https://doi.org/10.1016/j.adolescence.2015.03.012
- Galéra, C., Bouvard, M. P., Lagarde, E., Michel, G., Touchette, E., Fombonne, E., & Melchior, M. (2012). Childhood attention problems and socioeconomic status in adulthood: 18-Year follow-up. The British Journal of Psychiatry, 201(1), 20–25. https://doi.org/10.1192/bjp.bp.111.102491
- Gershoff, E. T. (2017). School corporal punishment in global perspective: prevalence, outcomes, and efforts at intervention. Psychology, Health & Medicine, 22(Suppl 1), 224–239. https://doi.org/10.1080/13548506.2016.1271955
- Kendall, L. (2016). The teacher said I’m thick! Experiences of children with attention deficit hyperactivity disorder within a school setting. Support for Learning, 31(2), 122–137. https://doi.org/10.1111/1467-9604.12121
- Kos, J. M. (2004). Primary school teachers’ knowledge, attitudes and behaviours toward children with attention-deficit/hyperactivity disorder. RMIT University.
- Kuder, G. F., & Richardson, M. W. (1937). The theory of the estimation of test reliability. Psychometrika, 2(3), 151–160. https://doi.org/10.1007/BF02288391
- Lasisi, D., Ani, C., Lasebikan, V., Sheikh, L., & Omigbodun, O. (2017). Effect of attention-deficit-hyperactivity-disorder training program on the knowledge and attitudes of primary school teachers in Kaduna, North-Western Nigeria. Child and Adolescent Psychiatry and Mental Health, 11(1), 15. https://doi.org/10.1186/s13034-017-0153-8
- Mohammed, F. (2018). Effects of a tailored incredible years teacher classroom management programme on on-task behaviour of school children with ADHD in Addis Ababa. Journal of International Special Needs Education, 21(1), 1–13. https://doi.org/10.9782/15-00055R2
- Moldavsky, M., Pass, S., & Sayal, K. (2014). Primary school teachers’ attitudes about children with attention-deficit/hyperactivity disorder and the role of pharmacological treatment. Clinical Child Psychology and Psychiatry, 19(2), 202–216. https://doi.org/10.1177/1359104513485083
- Noordzij, M., Tripepi, G., Dekker, F. W., Zoccali, C., Tanck, M. W., & Jager, K. J. (2010). Sample size calculations: Basic principles and common pitfalls. Nephrology, Dialysis, Transplantation, 25(5), 1388–1393. https://doi.org/10.1093/ndt/gfp732
- Ohan, J. L., Cormier, N., Hepp, S. L., Visser, T. A. W., & Strain, M. C. (2008). Does knowledge about attention-deficit/hyperactivity disorder impact teachers’ reported behaviors and perceptions? School Psychology Quarterly, 23(3), 436–449. https://doi.org/10.1037/1045-3830.23.3.436
- Polanczyk, G. V., Willcutt, E. G., Salum, G. A., Kieling, C., & Rohde, L. A. (2014). ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. International Journal of Epidemiology, 43(2), 434–442. https://doi.org/10.1093/ije/dyt261
- Sherman, J., Rasmussen, C., & Baydala, L. (2008). The impact of teacher factors on achievement and behavioural outcomes of children with attention-deficit/hyperactivity disorder (ADHD): A review of the literature. Educational Research, 50(4), 347–360. https://doi.org/10.1080/00131880802499803
- Srinath, S., Kandasamy, P., & Golhar, T. S. (2010). Epidemiology of child and adolescent mental health disorders in Asia. Current Opinion in Psychiatry, 23(4), 330–336. https://doi.org/10.1097/YCO.0b013e32833aa0c1
- Stuart, H., Chen, S.-P., Christie, R., Dobson, K., Kirsh, B., Knaak, S., Koller, M., Krupa, T., Lauria-Horner, B., Luong, D., Modgill, G., Patten, S. B., Pietrus, M., Szeto, A., & Whitley, R. (2014). Opening minds in Canada: Targeting change. Canadian Journal of Psychiatry, 59(10 Suppl 1), S13–S18. https://doi.org/10.1177/070674371405901s05
- Thornicroft, G., Mehta, N., Clement, S., Evans-Lacko, S., Doherty, M., Rose, D., Koschorke, M., Shidhaye, R., O'Reilly, C., & Henderson, C. (2016). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet, 387(10023), 1123–1132. https://doi.org/10.1016/S0140-6736(15)00298-6
- Usami, M. (2016). Functional consequences of attention-deficit hyperactivity disorder on children and their families. Psychiatry and Clinical Neurosciences, 70(8), 303–317. https://doi.org/10.1111/pcn.12393
- Ward, R. J., Bristow, S. J., Kovshoff, H., Cortese, S., & Kreppner, J. (2022). The effects of ADHD teacher training programs on teachers and pupils: A systematic review and meta-analysis. Journal of Attention Disorders, 26(2), 225–244. https://doi.org/10.1177/1087054720972801
- World Health Organization. (2016). mhGAP intervention guide mental health gap action programme version 2.0 for mental, neurological and substance use disorders in non-specialized health settings (pp. 1–173). WHO.
- Woyessa, A. H., Tharmalingadevar, T. P., Upashe, S. P., & Diriba, D. C. (2019). Primary school teachers’ misconceptions about attention-deficit/hyperactivity disorder in Nekemte town, Oromia region, Western Ethiopia. BMC Research Notes, 12(1), 524. https://doi.org/10.1186/s13104-019-4573-9