 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Studies show that body mass index during early adulthood (‘early BMI’) predicts the transition to first birth, but early childbearers tend to be omitted from such studies. This sample selection distorts the prevalence of childlessness, and particularly the racial/ethnic heterogeneity therein, because first birth timing differs by race/ethnicity. We imputed pre-parenthood early BMI for a larger sample, including early childbearers, for the same United States NLSY79 data used in a previous study and simulated differences in the probability of childlessness at age 40+ using posterior distributions based on the Bayesian framework. Obesity was consistently associated with higher childlessness across racial/ethnic groups in both sexes, but only among obese women were first births delayed until after early adulthood. The overall lower childlessness among the underweight women appeared largely driven by Black women. Our findings on the intersectionality of race/ethnicity and sex in the BMI–childlessness pathways encourage research on the underlying mechanisms and on more recent cohorts across different societies.
Introduction and background
Body mass index (BMI = weight [kg] divided by height [m, squared]) is one indicator of adiposity that has received extensive attention in the medical literature, in relation to health as well as fertility (Gesink Law et al. Citation2006; Ramlau-Hansen et al. Citation2007; Gaskins et al. Citation2015). Studies have shown higher chances of experiencing negative birth outcomes or reduced fecundity among underweight (Derbyshire Citation2014; Boutari et al. Citation2020) and obese individuals (Nguyen et al. Citation2007; Luke et al. Citation2011; Sermondade et al. Citation2013; Kawwass et al. Citation2016; Cavalcante et al. Citation2019; Crean and Senior Citation2019) of both sexes. Moreover, BMI may shape the social process of partnering, for example by influencing an individual’s self-esteem and self-perceived attractiveness (Kallen and Doughty Citation1984; La Rocque and Cioe Citation2011), attractiveness to potential mates (Swami Citation2006), and chances of experiencing discrimination in education and the labour market (Puhl and Brownell Citation2001; Spahlholz et al. Citation2016), all of which can affect their standing in mating markets. As yet, studies on the connection between BMI and fertility have typically been concentrated in either the clinical literature on infertility or the social sciences literature examining mating dynamics, leaving the association between BMI and completed fertility largely unaddressed from a demographic perspective.
A handful of existing studies conducted in Finland, Sweden, and the United States (US) have suggested that BMI measured during early adulthood (‘early BMI’) influences lifetime fertility with a BMI higher than the range for healthy weight (18.5–24.9) tend to have fewer children and are more likely to remain childless (i.e. zero biological children) at the end of their peak reproductive years. Additionally, in men, a BMI lower than the healthy range is associated with lower fertility. These patterns appear to be independent of socio-economic status (Jokela et al. Citation2007; Barclay and Kolk Citation2020). Understanding the long-term consequences of early BMI for lifetime fertility is important, given important secular trends in contemporary populations: the growing social and health disparities by early BMI (Frederick et al. Citation2014) and the increasing prevalence of delayed first births and childlessness (Kreyenfeld and Konietzka Citation2017; Ombelet and Goossens Citation2017).
Less is known about the extent to which the pathways linking early BMI to lifetime childlessness differ by race/ethnicity, a major axis along which disparities develop in terms of both BMI (Clarke et al. Citation2009; Yang et al. Citation2021) and childbearing (Darabi and Ortiz Citation1987; Sweeney and Raley Citation2014; Torres and Parrado Citation2022). Although previous work examining the BMI–fertility relationship using the National Longitudinal Study of Youth 1979 (NLSY79 Cohort) from the United States (US) did consider race/ethnicity as a statistical control, heterogeneity by race/ethnicity was not examined in detail (Jokela et al. Citation2008). This is unfortunate, given that the NLSY79 is one of the only data sources that can be used to examine the longitudinal association between early BMI and lifetime fertility by race/ethnicity. With the growing evidence that pathways into childlessness are gendered (Keizer et al. Citation2008; Fiori et al. Citation2017; Trimarchi and Van Bavel Citation2017; Chudnovskaya Citation2019; Saarela and Skirbekk Citation2020), there is a further need to study the intersectionality between race/ethnicity and sex in the BMI–childlessness association.
From early BMI to childlessness: Possible racial/ethnic differences
In this study, we examine whether the association between early BMI and lifetime fertility is consistent across race/ethnicity and how potential differences between racial/ethnic groups may interact with sex. Despite the well-known racial/ethnic disparities in early BMI (Cali and Caprio Citation2008) and in childlessness (Boyd Citation1989; Lundquist et al. Citation2009; Stulp et al. Citation2016) in the US context, BMI, childlessness, and race/ethnicity have rarely been studied in a combined framework. The pathways linking early BMI to childlessness may differ by race/ethnicity for several reasons that are not mutually exclusive.
Racial/ethnic differences in BMI
First, the pathways may differ because BMI differs by race/ethnicity. Evidence suggests that racial/ethnic disparities in BMI emerge early in life (Dixon et al. Citation2012; Rossen and Schoendorf Citation2012; Krueger et al. Citation2014; Krueger and Reither Citation2015; Menigoz et al. Citation2016). On the one hand, if the higher childlessness among those who are obese during early adulthood is driven by an ethnic group with a particularly high prevalence of obesity, this would suggest that the racial/ethnic disparity in obesity could exacerbate racial/ethnic disparities in lifetime fertility. On the other hand, if the relationship between early BMI and childlessness is relatively consistent across race/ethnicity despite some racial/ethnic differences in BMI, the degree of such consistency might allow us to gauge the physiological or behavioural significance of BMI in mediating lifetime fertility outcomes.
Racial/ethnic differences in preferred BMI
The way BMI is associated with perceived attractiveness may also differ by race/ethnicity and sex (Swami Citation2006), giving rise to heterogeneous BMI–childlessness relationships if perceived attractiveness influences the chances of partnering and eventually childlessness. Marriage or co-residential union formation, and their timing, have remained one of the strongest predictors of lifetime childlessness in recent US cohorts, including the NLSY79 sample cohort (Hayford Citation2013; Nitsche and Hayford Citation2020). Previous studies have highlighted marriage (or partnership in general) as a key mediator by which early BMI is associated with lifetime fertility (Jokela et al. Citation2007, Citation2008; Barclay and Kolk Citation2020). As such, to the extent that the probability of partnering is influenced by early BMI, any racial/ethnic differences in preferred BMI may lead to racial/ethnic heterogeneity in the relationship between early BMI and childlessness.
For instance, it has been suggested that ethnic minority women may be ‘buffered’ from the socio-cultural pressure to conform to a slender body type, given that the thin body ideal is largely associated with western, White-majority culture (Powell and Kahn Citation1995). In studies conducted in the US, Black men reported preferring a heavier body weight for women compared with their White counterparts, and Black women rated slightly heavier body weight to be ideal as well (Flynn and Fitzgibbon Citation1998). Black women also reported more satisfaction with their body weight despite being heavier than their White counterparts (Miller et al. Citation2000; Chithambo and Huey Citation2013). However, ethnic minority women had a similar or even higher tendency to report negative body esteem (Grabe and Hyde Citation2006; Sotiriou and Awad Citation2020; Frayon et al. Citation2021), suggesting that women in non-White groups may nevertheless be susceptible to the slender body ideal. Preferred BMI, as perceived by self and others, may be associated with reproductive behaviours and fertility in various ways, and testing these is beyond the scope of this study. Here we focus on whether lifetime fertility in the NLSY79 sample is less affected by deviations from healthy BMI among Black and Hispanic women compared with White women, as implied by the buffering hypothesis.
In men, although body shape (e.g. waist-to-chest ratio) tends to contribute more to perceived bodily attractiveness than does body size (e.g. BMI) (Tovée et al. Citation1999), BMI still appears to be a significant factor influencing family formation (Swami Citation2006). The significance of men’s BMI on perceived attractiveness might depend on the context. For example, while Greek and British women have reported preferring men of healthy BMI range, Greek women preferred men with a slightly thinner physique, presumably because what was perceived as ‘healthy’ body size differed in Greek society, where men’s obesity is among the highest in Europe (Swami et al. Citation2007). In general, there appears to be a preference for heavier weight (to the extent that it suggests greater strength) for men. In support, evidence suggests that men tend to underestimate their body weight due to a presumably higher preference for being larger, whereas the opposite is true for women (McCreary and Sasse Citation2000; McCreary and Sadava Citation2001; McCreary Citation2002); other research found that male undergraduate students in the US aspired to a large, muscular body shape ideal (Mintz and Kashubeck Citation1999). Such aspirations and related body esteem do not seem to differ by race/ethnicity (Mintz and Kashubeck Citation1999; Franzoi and Chang Citation2002). This evidence suggests that there may be no buffering from the influence of body size ideals for ethnic minority men, in contrast to that expected in women. Nevertheless, racial/ethnic differences in the perception of bodily attractiveness in men, and more generally their possible role in family formation processes, remain less studied for men.
Discrimination and intersectionality
Studies have indicated that discrimination based on weight occurs, particularly in terms of obesity. Obese individuals face discrimination in the labour market, in access to and support for education, and in the housing market (Puhl and Brownell Citation2001; Flint et al. Citation2016; Spahlholz et al. Citation2016). Moreover, obesity appears to interact with other individual characteristics, such as sex, in affecting the chance of experiencing discrimination across the life course. For instance, studies have shown that obese women, but not obese men, face discrimination in job recruitment (Campos-Vazquez and Gonzalez Citation2020) and that obese girls, but not boys, are less likely to enrol in college than peers of ‘normal’ weight (Crosnoe Citation2007). Weight discrimination has also been shown to accumulate with other forms of discrimination, such as race/ethnicity-based discrimination (Pearl et al. Citation2018). This intersectionality between body weight, sex, and race/ethnicity may place obese or underweight individuals from racial/ethnic minority groups in a position of exacerbated disadvantage in the mating market, in terms of having access to potential partners, union formation processes, and/or union stability.
Present study
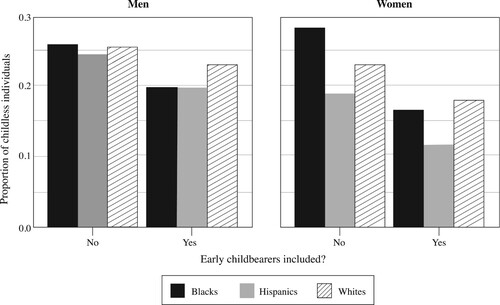
Here, we revisit the NLSY79 data and compare childlessness by early BMI among Hispanics, Blacks, and Whites within each sex. We address one limitation in the NLSY79 data for studying the relationship between early BMI and childlessness, which is that early BMI was measured during young adulthood (on average at age 20) when more than a quarter of the sample had already transitioned to first parenthood or would do so within the next year. This condition led the previous study on the same NLSY79 data (Jokela et al. Citation2008) to exclude early childbearers: defined here as those who already had biological children by 1981 (the first year in which BMI was measured in the NLSY79 sample) and those with a first birth before age 17 (see supplementary material, section S1). The purpose of excluding early childbearers was to avoid contamination of the early BMI and fertility relationship by the known reverse impact of parenthood on BMI (Corder et al. Citation2020). However, doing so inevitably overestimates the prevalence of childlessness and potentially distorts racial/ethnic differences in childlessness by early BMI in multiple ways. For example, under this sampling strategy, the median age at first birth in our study sample was seven years younger among early childbearers (19 years) than non-early childbearers (26 years) in both sexes, and there were more early childbearers among women (33.5 per cent) than men (20.3 per cent). Among women whose fertility information at age 40+ was available, the prevalence of childlessness was 15.5, 11.5, and 18.1 per cent for Blacks, Hispanics, and Whites, respectively, but was 27.8, 19.3, and 23.3 per cent after excluding early childbearers. In other words, using this strategy, significantly larger proportions of Black and Hispanic mothers will be excluded compared with White mothers (), introducing bias by race/ethnicity in the sample for the prospective analyses.
Figure 1 Racial differences in the proportion of individuals remaining childless at age 40+: men and women from the US NLSY79 Cohort
Notes: Calculations are based on the 10,571 individuals (men = 5,346; women = 5,225) whose BMI was measured during early adulthood. When early childbearers are excluded from the sample, the average proportion of childless individuals is overestimated and its racial/ethnic distribution changes, especially in women. The proportions are 0.26, 0.24, and 0.25 for Black, Hispanic, and White men respectively, and 0.28, 0.19, and 0.23 for Black, Hispanic, and White women, respectively, if early childbearers are excluded. The proportions become lower if early childbearers are included, to 0.20, 0.20, and 0.19 for Black, Hispanic, and White men, respectively, and 0.17, 0.11, and 0.18 for Black, Hispanic, and White women, respectively.
Source: Authors’ analysis of data from the NLSY79 Cohort.
Excluding the dynamics of early childbearing also leaves unknown when the delayed transition to first parenthood associated with BMI manifests. In light of the previous findings that suggested higher childlessness among those with too low or too high a BMI (Jokela et al. Citation2007, Citation2008; Barclay and Kolk Citation2020), we might expect that those who become parents early are more likely to exhibit a healthy BMI. But it is also possible that the implications of healthy BMI on accelerating the transition to parenthood depend on age, to the extent that healthy BMI exerts its effect on lifetime fertility via selection into partner markets, as considered in the earlier subsection on racial/ethnic difference in preferred BMI. If so, we would expect the association between healthy BMI and accelerated transition to parenthood to begin to appear only after young adulthood (i.e. when women reach typical marital age). Such temporal dynamics in the effect of early BMI may further differ by racial/ethnic group, if there are racial/ethnic differences in preferred BMI.
Thus, incorporating early childbearers into the analysis is crucial to understanding the extent to which the influence of early BMI on childlessness differs by race/ethnicity. We achieve this goal by imputing pre-parenthood BMI at a fixed age, so that early childbearers—who are more likely to be non-Whites and were omitted in the previous study that used the same NLSY79 data (Jokela et al. Citation2008)—can be incorporated into the analyses. Using the expanded data set, with 37 per cent more individuals made available via the imputation of early BMI and the incorporation of the latest NLSY79 data from 2018, we seek to answer the following research questions:
Study 1: Does early BMI predict childlessness at age 40+, and are there differences by race/ethnicity and sex?
Study 2: How does the pace of transition to first birth differ by early BMI, and are there differences by race/ethnicity and sex?
We address these questions separately for each sex. In Study 1, we compare childlessness between Blacks, Hispanics, and Whites by early BMI. To gauge the significance of racial/ethnic differences in the relationship between early BMI and lifetime childlessness, we conduct probabilistic model comparisons using information criteria and estimate the relative quality of predictive accuracy of a model that assumes race/ethnicity interaction in the BMI–childlessness association. In Study 2, we analyse time to first birth by early BMI, and further by race/ethnicity, and describe patterns based on survival curves and hazard rate differences between early BMI groups. Because the previous study compared time to first birth by early BMI too (Jokela et al. Citation2008), we are also interested in to what extent the findings regarding the impact of early BMI will change once we incorporate in the analyses both early childbearers and a larger sample of the NLSY79 Cohort that is more representative in terms of racial/ethnic differences in both timing and quantum of first births.
Data and methods
NLSY79 Cohort
The NLSY79 Cohort is a longitudinal project that follows the lives of the cohort born in the US between 1957 and 1964, comprising the younger portion of the baby boom generation (Hogan et al. Citation2008). The survey started in 1979, when the recruited subjects were aged 14–22, was repeated annually until 1994, and has been run biennially since, with the most recent survey conducted in 2018. Response rates are high in the sample: for example, after excluding those deceased, 89 per cent of those from 1979 were followed through to 2014 (Rothstein et al. Citation2019). Studies have found no evidence that attrition has biased estimated models of employment and wages (MaCurdy et al. Citation1998) or the relationship between educational attainment and labour market outcomes (Aughinbaugh et al. Citation2017).
Outcome variable: Childlessness
We studied childlessness by examining both whether the index person was childless by age 40+ (Study 1) and time to first parenthood, if any (Study 2). We used the ‘number of children ever born’ (NUMKID_XRND) variable to code whether a respondent was childless when their last interview was at age 40+. The median (and mean) age at which completed fertility was assessed in the studied sample was 53 years, with an inter-quartile range of 52–55 years. We used the ‘age of respondent at first birth’ (AGE1B_XRND) variable for those who had ever had a child and age at last interview for those who had never had a child or were censored before the birth of a first child.
Independent variables
Early BMI
We used BMI information available from the 1981, 1982, and 1985 surveys, when the NLSY79 participants were aged 16–28. In the original NLSY79 sample (n = 12,686), there were 3,415 individuals (28.2 per cent) whose BMI was known only after their transition to parenthood, of whom 67.1 per cent were females. To be able to incorporate these individuals into our study, we predicted their early BMI before becoming a parent, as follows.
First, we selected 34,995 BMI measurements from 12,599 individuals (6,194 females and 6,405 males). This was after excluding 87 individuals whose parenthood status at BMI measurement was unknown, as this condition would not allow us to predict pre-parenthood BMI. Among the 12,599 individuals, BMI was measured three times for 83 per cent, twice for 15 per cent, and only once for 2 per cent.
Second, within each sex, we estimated a model for predicting early BMI. To reflect the data structure of repeated BMI measures within individuals, and thus retain between-individual variance when predicting BMI, a mixed-effects model (aka multilevel model) was specified as:
(1)
(1) where observations of BMI
are clustered within individuals
;
is each observed BMI measurement; and
represents the individual intercepts (random effects) assumed to follow a normal distribution. The notation
denotes a matrix of fixed effects specific to BMI (age at BMI measurement, to whether a BMI was measured at or after the transition to parenthood), and to individual background (age at recruitment to the NLSY79 sample, NLSY79 subsample membership, race/ethnicity, parents’ highest level of education, religion during upbringing, residence [urban/rural/farm], and with whom a respondent resided).
Third, we used the estimated coefficients, including individual intercepts, to construct for each individual a model to predict BMI at age 16 (before the transition to parenthood), while setting the variables on individual background at each respondent’s observed values. The choice of age 16 was to measure early adulthood BMI more than three years before the average age at first birth for both sexes across racial/ethnic groups, so that a prospective design could be retained. Section S2 of the supplementary material provides more details on the modelling and validation of this method.
Lastly, we categorized the predicted BMI values into underweight (<18.5), healthy (18.5–24.9), overweight (25.0–29.9), and obese (≥30.0) following the standard clinical classification of BMI. We used the categorical instead of the continuous variable to allow for easier interpretation of the interaction between BMI and race/ethnicity.
Race/ethnicity
We used three categories of race/ethnicity—Blacks, Hispanics, and Whites—based on the information assessed during the household screening conducted by NORC in 1978, when interviewers were instructed to code the race/ethnicity information using a set of guidelines. Respondents were also asked during the first interviews in 1979 to name the racial/ethnic origins with which they identified, from a listing of almost 30 categories. Among those who identified themselves as neither Blacks nor Hispanics, we selected those who identified themselves as of European origin (68 per cent) to create a group of respondents operationally defined as Whites. Within our study sample, there were 2,926 Blacks (27.7 per cent), 1,648 Hispanics (15.6 per cent), and 5,997 Whites (56.7 per cent). The higher representation of Blacks and Hispanics in our sample compared with that at the population level during the early 1980s (Smelser et al. Citation2001) allowed an opportunity to examine heterogeneity by race/ethnicity better.
Study sample
From the original NLSY79 sample of 12,686 respondents, our study sample was 10,571 respondents. We used three non-mutually exclusive inclusion criteria. We included individuals who belonged to any one of the racial/ethnic groups Blacks, Hispanics, and Whites (n = 1,744 excluded) and had non-missing information on age at first childbirth (not due to childlessness; n = 29 excluded). We also excluded those whose reported age at first birth was under 16 (n = 185) because: (1) too young a reported age at first birth could indicate reporting error; and (2) incorporating them into the analyses would require the predicted BMI to be set at age 10, given that the youngest reported age at first birth was 11.
Statistical analysis
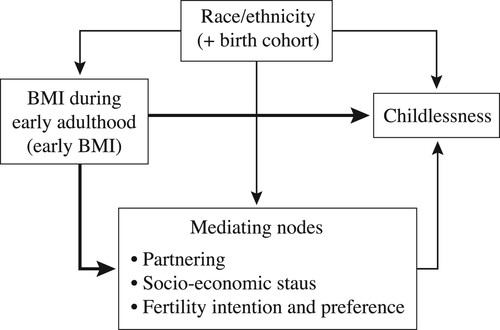
We estimated models within each sex, based on the causal diagram where the estimand is the effect of early BMI on childlessness (). We modelled a causal process in which race/ethnicity underlies the variations in both early BMI and childlessness (i.e. it is a confounder), and behaviours that we expect to be affected in part by early BMI—such as union formation, variables directly related to socio-economic status, or fertility desire—lie on the causal path between early BMI and childlessness (i.e. they are mediators). As such, only race/ethnicity comprises biasing paths that are necessary and sufficient to be adjusted to estimate the total effect of early BMI on childlessness to avoid overcontrol bias (Textor et al. Citation2017; Rohrer Citation2018) and to examine how the total effect differs by race/ethnicity. In this regard, we did not adjust for mediating variables in the statistical models estimated for this study. The NLSY79 sample was recruited at ages 14–21, and such within-sample differences in yearly birth cohort can potentially influence both early BMI and childlessness. As such, yearly birth cohort is another confounder that could potentially compete with race/ethnicity to bias the path from early BMI to childlessness. We thus adjusted for yearly birth cohort in all models but do not interpret their estimates.
Figure 2 A directed acyclic graph describing the expected causal process linking race/ethnicity, early BMI, and childlessness in our study
Notes: In our proposed causal framework, causal paths (thick lines) exist between exposure (early BMI) and outcome (childlessness), as well as between exposure and mediators. The rest are biasing paths (thin lines). Race/ethnicity and birth cohort are confounders, because they affect both exposure and outcome. To estimate the total effect of early BMI on childlessness, adjustment of confounders is necessary and sufficient, because adjustment of mediators would ‘take away’ the weight of effects exerted through the causal path between early BMI and mediators. In this study, we are interested in the total effect that combines the direct and indirect effects of early BMI, and as such, only race/ethnicity (and birth cohort as a potentially competing confounder) are adjusted for in the models.
Source: Authors’ own.
For Study 1, on early BMI and childlessness and racial/ethnic differences therein, our sample was individuals whose childlessness information was known at age 40+ (n = 7,531). We modelled within each sex a binary indicator, , of whether a respondent i remained childless at age 40+ as a function of early BMI category (
) and race/ethnicity category (
):
(2)
(2) where the inverse logit (or log odds) of
, that is,
, is the predicted proportion of childless individuals in the reference group (Whites with healthy BMI at age 16), and the inverse logits of
and
are the proportions childless in the non-healthy BMI groups and non-White groups, respectively. To be able to represent the degree of uncertainty around estimates fully, we used a Bayesian framework with the Markov chain Monte Carlo (MCMC) algorithm—specifically Hamiltonian Monte Carlo—as our simulation technique and made use of the posterior predictive distribution generated from the posterior distribution of estimates. Using the posterior predictive distribution is recommended over summarizing results based on the posterior distribution of estimates, because the former takes into account variance not only in estimates (estimation uncertainty) but also in their distribution per se (sampling uncertainty) (McElreath Citation2020).
To obtain the posterior predictive distribution of probability that underweight Hispanic women remain childless, we randomly drew 4,000 predicted binary outcomes (childless or not) from the sampling distribution of estimates by setting early BMI at underweight and race/ethnicity at Hispanics, then took an average over the 4,000 draws to find the predicted proportion of childlessness. Finally, we repeated this process 10,000 times to obtain the distribution of the predicted proportion of childlessness. We interpret the proportion as the probability of remaining childless for respective groups. To understand the overall significance of racial/ethnic differences in the BMI to childlessness pathway, we compared models that either allowed or did not allow interaction between early BMI and race/ethnicity. Specifically, we performed efficient, approximate leave-one-out cross-validation (LOO-CV) for Bayesian models using Pareto smoothed importance sampling, to assess if inclusion of the interaction term improved predictive accuracy for a model relative to a simpler model without the interaction term (Vehtari et al. Citation2017).
For Study 2, on the pace of transition to first parenthood by early BMI and racial/ethnic differences therein, we used the whole study sample (n = 10,571). We conducted survival analyses and modelled age at first birth as waiting time until transition to first parenthood. Using the proportional hazard model, the expected hazard of transitioning to first birth at age is assumed to be a function of early BMI category (
) of respondent
:
(3)
(3) where
is the baseline hazard rate and represents the probability that the transition to first parenthood occurs if such transition has not occurred up to age
for the reference group (healthy BMI at age 16); and
represents the hazard rate of a BMI group relative to that of the healthy BMI group. Because we tested the significance of the interaction between early BMI and race/ethnicity in Study 1, our focus in Study 2 was to describe and test differences in transition rates to first birth by early BMI categories within each race/ethnicity and sex. As such, we ran models within each sex and then further within each racial/ethnic group, without testing the interaction between early BMI and race/ethnicity.
We used R version 4.1.0 (R Core Team Citation2021) for data processing, statistical analysis of both Study 1 and Study 2, and visualization. We used the R packages ‘rstanarm’ (Goodrich et al. Citation2020) for fitting and diagnosing MCMC models, as well as ‘bayestestR’ (Makowski et al. Citation2019) and ‘bayesplot’ (Gabry and Mahr Citation2017) for processing model outputs. Every model was run for four chains, each with 5,000 iterations (including a burn-in period of 1,000 iterations which are discarded); we examined if the chains converged well by checking split (<1.1) and trace plots (Muth et al. Citation2018). More details on modelling results are presented in the supplementary material (sections 3 and 4).
In the Results section, we report medians of posterior samples as point estimates and 90 per cent credible intervals (CIs) in brackets to express uncertainty around each point estimate. For the CIs, we computed the lower and higher values comprising the 90 per cent quantile of a given distribution. Point estimates and CIs were calculated based on sampling from the posterior predictive distribution of estimates for Study 1 and from the posterior distribution of estimates for Study 2. Whenever a comparison is made, the 90 per cent indicates the estimated differences expected at 90 per cent chance; if the interval does not overlap with zero, it means there is a smaller than 5 per cent chance that the difference is the opposite direction.
Results
Study 1. Does early BMI predict childlessness at age 40+, and are there differences by race/ethnicity and sex?
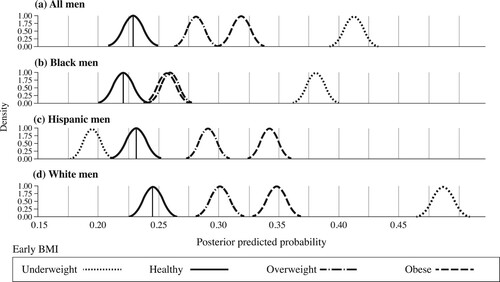
The chance of remaining childless at age 40+ differed by early BMI ((a) for women; (a) for men). In both sexes, being obese during early adulthood was associated with a higher probability of childlessness compared with healthy BMI counterparts, by a larger degree in women (0.14 [90 per cent CI: 0.13–0.16]) than in men (0.09 [0.07–0.11]). Being underweight had different implications for men and women: although being underweight during early adulthood was associated with an average 0.19 [0.17–0.21] increase in the probability of childlessness compared with healthy BMI counterparts for men, it was associated with on average a 0.03 [0.02–0.04] decrease for women. Being overweight during early adulthood was also associated with higher childlessness (in men 0.05 [0.03–0.07]; in women 0.02 [0.01–0.04]) relative to healthy BMI counterparts, but the magnitude of the difference relative to the healthy BMI group was smaller than for either the underweight or obese. Whether the relationship between early BMI and childlessness differed by race/ethnicity was dependent on sex, as we discuss next.
Figure 3 Probability of remaining childless at age 40+ by early BMI and race/ethnicity: women in the US NLSY79 Cohort who were last interviewed at age 40+ (n = 3,765)
Note: Early BMI is pre-parenthood BMI at age 16. The average points of distributions for individuals of healthy BMI are indicated by dashed lines to help gauge relative distances to the distributions of other BMI groups.
Source: As for .
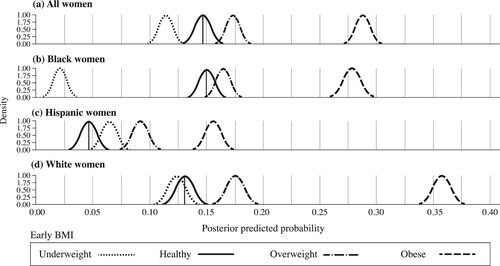
Figure 4 Probability of remaining childless at age 40+ by early BMI and race/ethnicity: men in the US NLSY79 Cohort who were last interviewed at age 40+ (n = 3,766)
Note: Early BMI is pre-parenthood BMI at age 16. The average points of distributions for individuals of healthy BMI are indicated by dashed lines to help gauge relative distances to the distributions of other BMI groups.
Source: As for .
Findings for women
Among women, the racial/ethnic differences were most evident for the association between being underweight and childlessness ((b)–(d), dot-dash lines). The lower childlessness associated with underweight was driven predominantly by the pattern in Black women, where the probability of childlessness was lower than that of healthy BMI counterparts by 0.13 [0.12–0.14]. Indeed, underweight Black women were predicted to be the least likely to remain childless ((b), dot-dash line). In contrast, being underweight during early adulthood was associated with slightly higher childlessness for Hispanic women ([0.00–0.03]; (c)), and the chance of remaining childless compared with healthy BMI counterparts was not distinguishable for White women ([−0.02–0.01]; (d)). As indicated by the inclusion of 0 in the 90 per cent CI, certainty around the difference between the underweight and healthy BMI groups was lower for Hispanic and White women. This is also shown by some large overlap in the posterior estimates of the probability of childlessness for underweight women (, light dot-dash lines) and healthy BMI women (, solid lines), especially among Whites.
Racial/ethnic differences were less pronounced among obese or overweight women. Across racial/ethnic groups, childlessness was consistently higher among the obese compared with their healthy BMI counterparts. The difference was largest among White women (0.20 [0.18–0.21]), followed by Blacks (0.13 [0.11–0.14]) and Hispanics (0.08 [0.07–0.10]). The degree to which being overweight was associated with higher childlessness was consistently small across racial/ethnic groups, with 0.03 [0.02–0.04] for Hispanic women, 0.05 [0.03–0.06] for White women, and 0.01 [0.00–0.03] for Black women (where the difference in childlessness between overweight and healthy BMI women was the smallest and least certain, given the inclusion of zero in the 90 per cent CI).
This racial/ethnic contrast, mostly among underweight women, likely explains the relatively small support we found for the model allowing the interaction between race/ethnicity and childlessness, according to model selection. The model with the interaction between race/ethnicity and early BMI had expected log predictive density (ELPD) that was higher by 0.9 (standard error [SE] of the difference = 3.3) compared with the model without the interaction. Given that the SE of the difference was larger than the difference itself, we interpret this model comparison result as evidence of marginally better accuracy of the model with the interaction term.
Findings for men
Among men, the model without the interaction between race/ethnicity and early BMI exhibited higher accuracy than the model with the interaction: the ELPD was higher by 4.4 (SE = 2.2). This model comparison result contrasts with the slightly higher accuracy seen in the model with the interaction term for women and thus suggests that evidence of racial/ethnic heterogeneity in the BMI–childlessness relationship is clearly weaker in men than in women. This conclusion is supported by the general pattern that deviations from healthy BMI were all associated with a higher predicted probability of childlessness compared with that of the healthy BMI counterparts in men across racial/ethnic groups (). One visible exception was among underweight Hispanic men (panel (c)), whose probability of remaining childless was lower by 0.03 [0.02–0.05] compared with their healthy BMI counterparts. The opposite was true for underweight Black and White men (panels (b) and (d)), where the predicted probabilities of childlessness jumped up by 0.16 [0.14–0.18] and 0.25 [0.23–0.26], in turn, compared with the respective racial/ethnic group’s healthy BMI counterparts. Because the increase in childlessness was much larger for underweight Blacks and Whites than for underweight Hispanic men (0.03), the pattern for underweight Hispanic men would be ‘masked’ if average patterns across race/ethnicity were examined (, dot-dash line in panel (a), compared with panels (b)–(d)).
Study 2. How does the pace of transition to first birth differ by early BMI, and are there racial/ethnic differences by race/ethnicity and sex?
Tracing the impact of early BMI on transitions to first birth showed that the impact may depend not only on race/ethnicity but also on age for women. We did not find similar evidence for men.
Findings for women
Among women, the average rate of first births at a given age was higher for those who were underweight ((a), All women) and lower for those who were obese at age 16 ((c), All women) compared with that of the healthy BMI group (, left-hand side).
Figure 5 Survival curves for time to first parenthood by BMI, relative to healthy BMI counterparts, and by race/ethnicity: women in the US NLSY79 Cohort (n = 5,225)
Notes: Survival curves show probability of remaining childless over time. Comparison groups are based on pre-parenthood BMI estimated at age 16. Age at which 50 per cent of women have transitioned to first parenthood is indicated by dashed lines in the panels for All women. Shading shows 95 per cent credible intervals.
Source: As for .
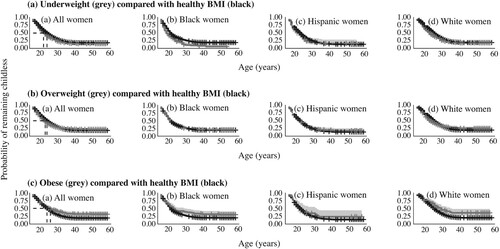
Table 1 Hazard ratio of first birth by early BMI group (relative to healthy BMI): women in the US NLSY79 Cohort
When further examined by race/ethnicity, differences were most pronounced for underweight women. In line with the findings from Study 1, the faster transitions to first birth in underweight women compared with women of healthy BMI was a pattern most visible in Blacks ((a), Black women). There was evidence that underweight White women made faster transitions to first birth but only during their early 20s ((a), White women). This would explain why lifetime childlessness in underweight women and those of healthy BMI was not distinguishable for Whites in Study 1. In Hispanics, nearly 23 per cent of the posterior estimates lay on the negative side ((b)), suggesting some degree of uncertainty in the degree to which underweight Hispanic women made faster transitions to first birth compared with their healthy BMI counterparts ((a), Hispanic women).
Figure 6 Hazard rate of becoming a parent by BMI, relative to healthy BMI counterparts, and by race/ethnicity: women in the US NLSY79 Cohort (n = 5,225)
Notes: Vertical dashed lines represent the hazard rate for women of healthy BMI. Posterior distributions of estimates were used to calculate hazard rate differences. Negative values indicate a lower hazard rate (i.e. slower transition to first birth) than for those with healthy BMI. Difference in the distribution of estimates reflects the degree of uncertainty around the estimated hazard rate for that BMI group relative to that of the healthy BMI group.
Source: As for .
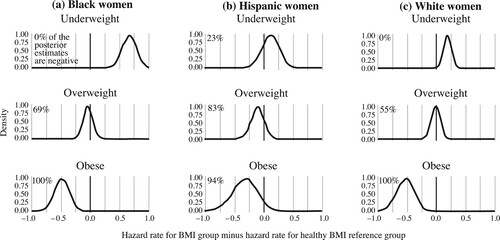
In contrast to such racial/ethnic heterogeneity for underweight women, the delayed transition to first parenthood among obese women compared with women of healthy BMI was a pattern most consistently and clearly visible across racial/ethnic groups ((c), , lower row).
The relative rate of overweight women becoming a parent was not clearly distinguishable from that of the healthy BMI group ((b), All women; ), and this observation remained similar across racial/ethnic groups (, middle row). The lower certainty appears to be due to the differential impact of being overweight depending on age (faster transition during early adulthood, slower transition in late adulthood), rather than to similarity with the healthy BMI group. In particular among White women, there was evidence that being overweight ‘switches’ its direction of impact from positive to negative, such that being overweight accelerates the transition to first parenthood during early adulthood and then delays the transition after age 30, compared with the rate of transition for those of healthy BMI ((b), White women). This pattern likely explains why the distribution for differences in posterior estimates is distributed fairly evenly below and above zero in overweight White women ((c), middle row).
Due to the differential impacts of early BMI by age, particularly during early adulthood, we reached a different conclusion about the relationship between early BMI and transition to first birth depending on whether early childbearers were included (, left-hand side) or excluded from the analyses (, right-hand side). Specifically, after including early childbearers we found that: (1) the relative acceleration in transition to first parenthood among underweight women became stronger and more evident; while (2) the relatively slower transition to first parenthood among overweight/obese women became weaker, because overweight/obese women were not necessarily delayed in the transition during early adulthood. Section S5 of the supplementary material provides a direct comparison between findings when early childbearers are included vs excluded.
Findings for men
Among men, the impact of early BMI on the rate of transition to first birth did not depend strongly on age. The faster rate of transition in individuals with healthy BMI was visible from early adulthood, most notably compared with underweight ((a)) or obese ((c)) men and less so in overweight men ((b)). This was in contrast to women, where the advantage of a healthy BMI was not apparent during early adulthood. As such, for men, the relationship between early BMI and fertility did not differ significantly depending on whether early childbearers were included (, left-hand side) or excluded from the analyses (, right-hand side). In further contrast to women, the pace of transitioning to first parenthood by early BMI was not strongly patterned by race/ethnicity in men. For each of underweight, overweight, and obese groups, the hazard rate difference from the healthy BMI group was similar across racial/ethnic groups (). The large uncertainty around the degree of differences for underweight men (as shown by the wide distributions in ) is mostly due to the low number of underweight men in the sample, but the overall negative differences are in line with on average slower transitions among underweight men compared with their healthy BMI counterparts.
Figure 7 Survival curves for time to first parenthood by BMI, relative to healthy BMI counterparts, and by race/ethnicity: men in the US NLSY79 Cohort (n = 5,346)
Notes: Survival curves show probability of remaining childless over time. Comparison groups are based on pre-parenthood BMI estimated at age 16. Age at which 50 per cent of men have transitioned to first parenthood is indicated by dashed lines in the panels for All men. Shading shows 95 per cent credible intervals.
Source: As for .
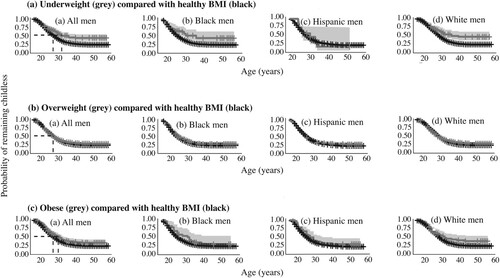
Figure 8 Hazard rate of becoming a parent by BMI, relative to healthy BMI counterparts, and by race/ethnicity: men in the US NLSY79 Cohort (n = 5,346)
Notes: Vertical dashed lines represent the hazard rate for men of healthy BMI. Posterior distributions of estimates were used to calculate hazard rate differences. Negative values indicate a lower hazard rate (i.e. slower transition to first birth) than for those with healthy BMI. Difference in the distribution of estimates reflects the degree of uncertainty around the estimated hazard rate for that BMI group relative to that of the healthy BMI group.
Source: As for .
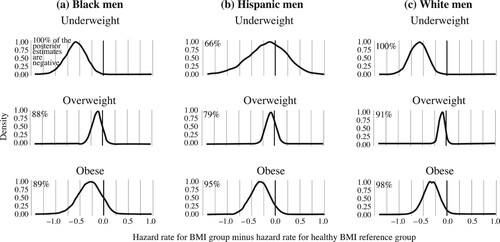
Table 2 Hazard ratio of first birth by early BMI group (relative to healthy BMI): men in the US NLSY79 Cohort
Discussion
Although previous scholarship has established significant differences in transition to first birth by BMI in NLSY79 data, ∼28 per cent of the sample who had had a first child before the assessment of early BMI needed to be excluded in the study by (Jokela et al. Citation2008) to avoid confounding by the reverse causality. In this study, we revisited the same data and used pre-parenthood BMI imputed for a larger sample that included early childbearers, thereby assessing the impact of early BMI on childlessness in a sample more representative in terms of racial/ethnic differences in the timing of first parenthood. We also made a methodological contribution by using posterior distributions of estimated difference to simulate the distribution of differences between subgroups. Doing so helped to address the challenge of interpreting differences between subgroups with insufficient data, and we communicated uncertainty around the estimates without relying on p-values, for example by assessing the degree of overlap with zero or departure from the distribution of other subgroups.
Our results highlight both similarity and heterogeneity by race/ethnicity in the BMI–childlessness relationship and in how race/ethnicity intersects with sex. First, we found that overall racial/ethnic heterogeneity may be small, due to the strong influence of obesity across racial/ethnic groups in both sexes. Within each race/ethnicity, the gap in childlessness between obese and healthy BMI was consistently larger in women than in men. Second, some racial/ethnic heterogeneity was detectable, especially in terms of underweight. Among women, the average lower childlessness associated with being underweight was driven almost solely by Black women (). Third, our new approach of incorporating early childbearers into the analyses offered additional evidence that the slower transitions to first birth among overweight/obese women did not manifest until their mid-20s. We discuss these three findings in turn.
The first finding, of higher childlessness among obese individuals across race/ethnicity and sex, suggests that there are some shared mechanisms underlying the association between obesity and fertility. For instance, endocrinological mechanisms by which obesity increases or exacerbates infertility have been widely described in the epidemiological, clinical, genetic, epigenetic, and non-human animal literature (Pasquali et al. Citation2007; Talmor and Dunphy Citation2015; Craig et al. Citation2017). To the extent that this body of evidence is generalizable to different population subgroups, and that early BMI levels persist into later life (Yang et al. Citation2021), we can consider higher infecundity as one reason why childlessness is higher among obese individuals regardless of sex and race/ethnicity. The physiological impact of obesity on infertility could be larger, given that individuals tend to partner with those with similar BMI (Ajslev et al. Citation2012).
Our finding could also suggest that behavioural mechanisms underlying the obesity–childlessness relationship have become similar across Blacks, Hispanics, and Whites, at least in the US birth cohorts represented by the NLSY79 sample. The behavioural mechanisms are likely manifold, rooted in physiological or psychological factors that interact with mating dynamics, as well as in structural inequalities, such as obesity stigma. We might expect these complex behavioural processes to exhibit heterogeneity by sex and race/ethnicity, depending on how social preference for certain body type differs along those social axes. We find no evidence of heterogeneity by race/ethnicity, and within each racial/ethnic group, obesity confers consistently higher childlessness in women than in men. These findings suggest that the socio-behavioural implications of obesity in the family formation process, which tend to be more consequential for women, perhaps due to the slender body ideal, have to some degree converged across racial/ethnic groups in the US. Alternatively, it could be that different mechanisms are at play across the groups but combine to produce similar patterns that link obesity to childlessness. It thus remains for future studies to explore the trajectory connecting early adulthood obesity and later-life fertility by race/ethnicity within each sex and to examine possible physiological and behavioural pathways in detail.
With obesity stigma, in addition to obesity itself, becoming a global health challenge (Brewis et al. Citation2018), future studies are needed beyond the racial/ethnic groups examined in this study and beyond the US context, especially in countries at different stages of socio-economic development, where structural factors such as weight-based discrimination might operate differently. Cross-cultural studies have shown that being obese itself might not be stigmatized in some countries (Sohn Citation2016), for example if large body size is socially valued (Cohen et al. Citation2018, Citation2019; Bosire et al. Citation2020). It is also possible that the importance of BMI in family formation is contingent on the prevalence of extreme BMI types: for example, with increased obesity, the obesity ‘penalty’ in the mating context might become smaller via multiple mechanisms, for example increased weight-based assortative mating (Ajslev et al. Citation2012). Such differences in socio-cultural norms or obesity prevalence may partly explain why the relationship between BMI and lifetime fertility differs across countries (Sear and Marlowe Citation2009; Butovskaya et al. Citation2017).
Our second finding provides evidence of lower childlessness among underweight women but only among Blacks. The difference between underweight and healthy BMI women in terms of lifetime childlessness was minimal for Hispanics and Whites. As this study focused on testing for the presence of racial/ethnic differences, underlying mechanisms remain to be explored in future research. One mechanism likely in play is the socio-economic disadvantage experienced by young Black women. It is well known that age at first birth is lower among Black women, who, at least between the 1970s and 1990s, were also more likely than other ethnic/racial groups to experience teenage pregnancies that were unwanted, mistimed, or outside marriage (Ventura and Bachrach Citation2000; Musick et al. Citation2009; Sweeney and Raley Citation2014). If being underweight is one indicator of socio-economic disadvantage via increased risk of food insecurity (Myers and Painter Citation2017; Burke et al. Citation2018; Moradi et al. Citation2019), we can expect a stronger association between being underweight and faster transition to first birth in more disadvantaged racial/ethnic groups, as we observed among Black women. Within this broader context of socio-economic disadvantage, behavioural and physiological mechanisms could play a further role.
For instance, it is possible that preferences for slender body type in women have been particularly strong among Blacks, a point that is further corroborated by the contrary pattern of higher childlessness among obese Black women. Such preferences, in turn, would underlie higher rates of union formation starting early in life and could be a mechanism that links underweight to lower childlessness among Black women. Under this scenario, the impact of BMI-related selection in the mating context may be even more pronounced in women of non-White ethnicities. Literature has suggested that women in non-White groups may be as susceptible to the thin body ideal as Whites (meta-analysis by Grabe and Hyde Citation2006). Moreover, qualitative evidence has indicated that slender body type represents a means to social status (Kwan Citation2009), especially for ethnic-minority women in the US (Cheney Citation2011). From this perspective, our finding of lower childlessness among underweight Black women may partly reflect an increasing impact of weight-based mate choice on the lifetime fertility of Black women. For example, the sharp decline in marriage among the early 1960s US birth cohorts (to which the NLSY79 sample belongs) was most pronounced in Black women (Raley et al. Citation2015; Frejka Citation2017). This has been explained by the limited overall pool of mates available for Black women, due to many factors including higher incarceration rates and higher interethnic marriage rates among Black men, and lower numbers of Black men with educational levels matching those of Black women (Frejka Citation2017). Within this context, Black women might have experienced greater selection in mate choice, one route in which BMI acted as a criterion.
Another possibility is that the lower childlessness among underweight Black women is due to physiological conditions in favour of fertility (e.g. higher conception rates, better pregnancy outcomes). Given that clinical research has so far given less attention to how reproductive biology by BMI differs by race/ethnicity, it is difficult to assess whether the physiological implications of being underweight differ in Black women. Some studies have suggested that eating disorders may be more prevalent among White than Black women, in part due to higher endorsement of slim body type among White women (Gray et al. Citation1987; Powell and Kahn Citation1995; Neff et al. Citation1997). The intersection of BMI, health, and race and its association with reproductive behaviours and processes may be promising avenues for future research to explore.
Our third finding is that after incorporating early childbearers into the analyses of first birth transitions, the hazard ratios for overweight and obese women are closer to 1.0 (i.e. differences compared with the healthy BMI group reduce). This is because obese women do not appear to be delayed in their transition to first birth, and overweight women even appear to make the transition faster than their healthy BMI counterparts, at least during early adulthood. As such, the overall delayed first births among obese and overweight individuals are less pronounced than implied from the previous study. We also find that the hazard ratios for underweight women are further away from 1.0 (i.e. differences compared with the healthy BMI group increase). This is because the faster rate of first births among underweight women is evident from early adulthood, allowing the higher chance of underweight women having at least one child to be detected, unlike in the previous study.
Our findings thus suggest that the impact of overweight and obesity on fertility might be age dependent, with different mechanisms involved across the lifespan. For instance, during adolescence, excess weight and higher body fat are associated with earlier sexual maturity (Elizondo-Montemayor et al. Citation2017; Barros et al. Citation2019; Żurawiecka and Wronka Citation2021) and even risky sexual behaviour (Leech and Dias Citation2012; Gordon et al. Citation2016; but see also Averett et al. Citation2013). This could potentially explain why the rate of transition to first birth among obese women seems to be indistinguishable from that of their healthy BMI counterparts, and the rate for overweight women in our study sample is even faster at these youngest ages. However, such adolescence-specific effects might fade when sexual maturation is complete and once the implications of overweight and obesity in partnering or infecundity become more dominant. Further research is needed to clarify whether and where exactly change points in the impact of early BMI exist, using more targeted methods (e.g. a piecewise hazard rate), and what mechanisms might explain heterogeneity over time.
To conclude, this study provides evidence of both similarity and heterogeneity in the association between early BMI and childlessness by race/ethnicity and in its intersection with sex. The patterns described in this study prompt two lines of future study. First, studies should explore the underlying mechanisms of this heterogeneity, which possibly involve physiological, psychological, and behavioural mechanisms that interact with social environments where weight-based perception and structural discrimination affect both the chances of reproduction (e.g. via partnering) and intentions to reproduce (e.g. fertility expectation or desire). We have made the early BMI data generated from this study publicly available (see Note 3) for future studies on mechanisms in the NLSY79 Cohort. Second, it remains to be seen whether our findings from the NLSY79 Cohort can be extended to more recent US cohorts or to other countries where secular trends in childlessness and BMI are both rapidly changing. For the more recent birth cohorts, it is possible that BMI is affecting childlessness and fertility in a different way, given the increasing prevalence of overweight and obesity and how that may affect norms and expectations around how body type and body image influence partnership formation and fertility processes.
Supplemental Material
Download PDF (841.8 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Notes
1 Please direct all correspondence to Susie Lee, Max Planck Institute for Demographic Research, Konrad-Zuse Straße 1, 18057 Rostock, Germany; or by Email: [email protected]
2 Acknowledgments: The authors would like to thank the discussant, the session chair, and audiences in the ‘Delayed Fertility and Childlessness’ session at the 2021 Annual Meeting of the Population Association of America (PAA) for helpful comments and discussion. The authors are grateful for the feedback provided by the editor and the two anonymous reviewers on the initial manuscript. Kieron Barclay was supported by the Bank of Sweden Tercentenary Foundation (Riksbankens Jubileumsfond) through a Pro Futura Scientia XIV fellowship.
3 Availability of data and code: The data that support the findings of this study are available to registered users of the NLS Investigator website (https://www.nlsinfo.org/investigator/pages/login). The new data on early BMI generated from this study are available at figshare (https://doi.org/10.6084/m9.figshare.19697815.v1>). All R code for statistical analyses and visualizations are available at Github (https://github.com/DSusieLee/NLSY79_BMI_childlessness/tree/master/Scripts).
References
- Ajslev, Teresa Adeltoft, Lars Ängquist, Karri Silventoinen, Michael Gamborg, David B. Allison, Jennifer L. Baker, and Thorkild I. A. Sørensen. 2012. Assortative marriages by body mass index have increased simultaneously with the obesity epidemic, Frontiers in Genetics 3. https://doi.org/10.3389/fgene.2012.00125
- Aughinbaugh, Alison, Charles R. Pierret, and Donna S. Rothstein. 2017. Attrition and Its Implications in the National Longitudinal Survey of Youth 1979. JSM Proceedings. Alexandria, VA: American Statistical Association.
- Averett, Susan, Hope Corman, and Nancy E. Reichman. 2013. Effects of overweight on risky sexual behavior of adolescent girls, Economic Inquiry 51(1): 605–619. https://doi.org/10.1111/j.1465-7295.2011.00396.x
- Barclay, Kieron, and Martin Kolk. 2020. The influence of health in early adulthood on male fertility, Population and Development Review 46(4): 757–785. https://doi.org/10.1111/padr.12357
- Barros, Bruna de Siqueira, Maria Cristina Maria Caetano Kuschnir, Katia Vergetti Bloch, and Thiago Luiz Nogueira da Silva. 2019. ERICA: age at menarche and its association with nutritional status, Jornal de Pediatria 95: 106–111. https://doi.org/10.1016/j.jped.2017.12.004
- Bosire, Edna N., Emmanuel Cohen, Agnes Erzse, Susan J. Goldstein, Karen J. Hofman, and Shane A. Norris. 2020. ‘I’d say I’m fat, I’m not obese’: Obesity normalisation in urban-poor South Africa, Public Health Nutrition 23(9): 1515–1526. https://doi.org/10.1017/S1368980019004440
- Boutari, Chrysoula, Panagiotis D. Pappas, Gesthimani Mintziori, Meletios P. Nigdelis, Loukas Athanasiadis, Dimitrios G. Goulis, and Christos S. Mantzoros. 2020. The effect of underweight on female and male reproduction, Metabolism 107: 154229. https://doi.org/10.1016/j.metabol.2020.154229
- Boyd, Robert L. 1989. Racial differences in childlessness: A centennial review, Sociological Perspectives 32(2): 183–199. https://doi.org/10.2307/1389096
- Brewis, Alexandra, Cindi SturtzSreetharan, and Amber Wutich. 2018. Obesity stigma as a globalizing health challenge, Globalization and Health 14(1): 20. https://doi.org/10.1186/s12992-018-0337-x
- Burke, Michael P., Sonya J. Jones, Edward A. Frongillo, Maryah S. Fram, Christine E. Blake, and Darcy A. Freedman. 2018. Severity of household food insecurity and lifetime racial discrimination among African-American households in South Carolina, Ethnicity & Health 23(3): 276–292. https://doi.org/10.1080/13557858.2016.1263286
- Butovskaya, M., A. Sorokowska, M. Karwowski, A. Sabiniewicz, J. Fedenok, D. Dronova, M. Negasheva, et al. 2017. Waist-to-hip ratio, body-mass index, age and number of children in seven traditional societies, Scientific Reports 7(1): 1622. https://doi.org/10.1038/s41598-017-01916-9
- Cali, Anna M. G., and Sonia Caprio. 2008. Obesity in children and adolescents, The Journal of Clinical Endocrinology & Metabolism 93(11_supplement_1): s31–s36. https://doi.org/10.1210/jc.2008-1363
- Campos-Vazquez, Raymundo M., and Eva Gonzalez. 2020. Obesity and hiring discrimination, Economics & Human Biology 37: 100850. https://doi.org/10.1016/j.ehb.2020.100850
- Cavalcante, Marcelo B., Manoel Sarno, Alberto B. Peixoto, Edward Araujo Junior, and Ricardo Barini. 2019. Obesity and recurrent miscarriage: A systematic review and meta-analysis, Journal of Obstetrics and Gynaecology Research 45(1): 30–38. https://doi.org/10.1111/jog.13799
- Cheney, Ann M. 2011. “Most girls want to be skinny”: Body (dis)satisfaction among ethnically diverse women, Qualitative Health Research 21(10): 1347–1359. https://doi.org/10.1177/1049732310392592
- Chithambo, Taona P., and Stanley J. Huey. 2013. Black/white differences in perceived weight and attractiveness among overweight women, Journal of Obesity 2013: e320326. https://doi.org/10.1155/2013/320326
- Chudnovskaya, Margarita. 2019. Trends in childlessness among highly educated men in Sweden, European Journal of Population 35(5): 939–958. https://doi.org/10.1007/s10680-018-9511-3
- Clarke, Philippa, Patrick M. O’Malley, Lloyd D. Johnston, and John E. Schulenberg. 2009. Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986–2004, International Journal of Epidemiology 38(2): 499–509. https://doi.org/10.1093/ije/dyn214
- Cohen, E., A. Ndao, B. Faye, S. Ndiaye, E. H. M. Ndiaye, G. Ezan, L. Gueye, et al. 2018. Large body size as a socially valued factor determining excess weight and obesity in the context of the nutritional transition in Senegal, Bulletins et Mémoires de La Société D’Anthropologie de Paris 30(1–2): 59–69. https://doi.org/10.1007/s13219-017-0198-5
- Cohen, Emmanuel, Philippe Jean-Luc Gradidge, Amadou Ndao, Priscilla Duboz, Enguerran Macia, Lamine Gueye, Gilles Boëtsch, et al. 2019. Biocultural determinants of overweight and obesity in the context of nutrition transition in Senegal: A holistic anthropological approach, Journal of Biosocial Science 51(4): 469–490. https://doi.org/10.1017/S0021932018000287
- Corder, Kirsten, Eleanor M. Winpenny, Campbell Foubister, Justin M. Guagliano, Xenia M. Hartwig, Rebecca Love, Chloe Clifford Astbury, et al. 2020. Becoming a parent: A systematic review and meta-analysis of changes in BMI, diet, and physical activity, Obesity Reviews 21(4): e12959. https://doi.org/10.1111/obr.12959
- Craig, James R., Timothy G. Jenkins, Douglas T. Carrell, and James M. Hotaling. 2017. Obesity, male infertility, and the sperm epigenome, Fertility and Sterility 107(4): 848–859. https://doi.org/10.1016/j.fertnstert.2017.02.115
- Crean, Angela J., and Alistair M. Senior. 2019. High-fat diets reduce male reproductive success in animal models: A systematic review and meta-analysis, Obesity Reviews 20(6): 921–933. https://doi.org/10.1111/obr.12827
- Crosnoe, Robert. 2007. Gender, obesity, and education, Sociology of Education 80(3): 241–260. https://doi.org/10.1177/003804070708000303
- Darabi, K. F. and V. Ortiz. 1987. Childbearing among young Latino women in the United States, American Journal of Public Health 77(1): 25–28. https://doi.org/10.2105/AJPH.77.1.25
- Derbyshire, E. 2014. 19. Lower fertility associated with periconceptional obesity and underweight, in Human Health Handbooks: Vol. 7. Handbook of Diet and Nutrition in the Menstrual Cycle, Periconception and Fertility, Vol. 7, pp. 313–326. https://doi.org/10.3920/978-90-8686-767-7_19
- Dixon, Brittany, Michelle-Marie Peña, and Elsie M. Taveras. 2012. Lifecourse approach to racial/ethnic disparities in childhood obesity, Advances in Nutrition 3(1): 73–82. https://doi.org/10.3945/an.111.000919
- Elizondo-Montemayor, Leticia, Claudia Hernández-Escobar, Eduardo Lara-Torre, Bianca Nieblas, and Merith Gómez-Carmona. 2017. Gynecologic and obstetric consequences of obesity in adolescent girls, Journal of Pediatric and Adolescent Gynecology 30(2): 156–168. https://doi.org/10.1016/j.jpag.2016.02.007
- Fiori, Francesca, Francesca Rinesi, and Elspeth Graham. 2017. Choosing to remain childless? A comparative study of fertility intentions among women and men in Italy and Britain, European Journal of Population 33(3): 319–350. https://doi.org/10.1007/s10680-016-9404-2
- Flint, Stuart W., Martin Čadek, Sonia C. Codreanu, Vanja Ivić, Colene Zomer, and Amalia Gomoiu. 2016. Obesity discrimination in the recruitment process: “You’re not hired!”, Frontiers in Psychology 7: 647. https://doi.org/10.3389/fpsyg.2016.00647
- Flynn, Kristin J., and Marian Fitzgibbon. 1998. Body images and obesity risk among black females: A review of the literature, Annals of Behavioral Medicine 20(1): 13–24. https://doi.org/10.1007/BF02893804
- Franzoi, Stephen L., and Zoua Chang. 2002. The body esteem of Hmong and Caucasian young adults, Psychology of Women Quarterly 26(1): 89–91. https://doi.org/10.1111/1471-6402.00046
- Frayon, Stéphane, Viren Swami, Guillaume Wattelez, Jennifer Todd, and Olivier Galy. 2021. Associations between weight status, body satisfaction, ethnic identity and self-esteem in Oceanian adolescents, Pediatric Obesity 16(12): e12824. https://doi.org/10.1111/ijpo.12824
- Frederick, Carl B., Kaisa Snellman, and Robert D. Putnam. 2014. Increasing socioeconomic disparities in adolescent obesity, Proceedings of the National Academy of Sciences 111(4): 1338–1342. https://doi.org/10.1073/pnas.1321355110
- Frejka, Tomas. 2017. Childlessness in the United States, in Michaela Kreyenfeld and Dirk Konietzka (eds), Childlessness in Europe: Contexts, Causes, and Consequences, pp. 159–179. Retrieved from http://library.oapen.org/handle/20.500.12657/29707
- Gabry, Jonah, and Tristan Mahr. 2017. bayesplot: Plotting for Bayesian models. R Package Version, 1.0.
- Gaskins, Audrey J., Janet W. Rich-Edwards, Stacey A. Missmer, Bernard Rosner, and Jorge E. Chavarro. 2015. Association of fecundity with changes in adult female weight, Obstetrics & Gynecology 126(4): 850–858. https://doi.org/10.1097/AOG.0000000000001030
- Gesink Law, D. C., Richard F. Maclehose, and Matthew P. Longnecker. 2006. Obesity and time to pregnancy, Human Reproduction 22(2): 414–420. https://doi.org/10.1093/humrep/del400
- Goodrich, Ben, Jonah Gabry, Imad Ali, and Sam Brilleman. 2020. rstanarm: Bayesian applied regression modeling via Stan. Retrieved from https://mc-stan.org/rstanarm
- Gordon, Lonna P., Angela Diaz, Christine Soghomonian, Anne T. Nucci-Sack, Jocelyn M. Weiss, Howard D. Strickler, Robert D. Burk, et al. 2016. Increased body mass index associated with increased risky sexual behaviors, Journal of Pediatric and Adolescent Gynecology 29(1): 42–47. https://doi.org/10.1016/j.jpag.2015.06.003
- Grabe, Shelly, and Janet Shibley Hyde. 2006. Ethnicity and body dissatisfaction among women in the United States: A meta-analysis, Psychological Bulletin 132(4): 622–640. https://doi.org/10.1037/0033-2909.132.4.622
- Gray, James J., Kathryn Ford, and Lily M. Kelly. 1987. The prevalence of bulimia in a black college population, International Journal of Eating Disorders 6(6): 733–740. https://doi.org/10.1002/1098-108X(198711)6:6<733::AID-EAT2260060606>3.0.CO;2-U
- Hayford, Sarah R. 2013. Marriage (still) matters: The contribution of demographic change to trends in childlessness in the United States, Demography 50(5): 1641–1661. https://doi.org/10.1007/s13524-013-0215-3
- Hogan, Howard, Deborah Perez, and William Bell. 2008. Who (Really) are the First Baby Boomers? 1009–1016. Alexandria, VA: American Statistical Association: Joint Statistical Meetings Proceedings, Social Statistics Section.
- Jokela, Markus, Marko Elovainio, and Mika Kivimäki. 2008. Lower fertility associated with obesity and underweight: The US National Longitudinal Survey of Youth, The American Journal of Clinical Nutrition 88(4): 886–893. https://doi.org/10.1093/ajcn/88.4.886
- Jokela, Markus, Mika Kivimäki, Marko Elovainio, Jorma Viikari, Olli T. Raitakari, and Liisa Keltikangas-Järvinen. 2007. Body mass index in adolescence and number of children in adulthood, Epidemiology 18: 599–606. https://doi.org/10.1097/EDE.0b013e3181257158
- Kallen, David, and Andrea Doughty. 1984. The relationship of weight, the self perception of weight and self esteem with courtship behavior, Marriage & Family Review 7(1–2): 93–114. https://doi.org/10.1300/J002v07n01_09
- Kawwass, Jennifer F., Aniket D. Kulkarni, Heather S. Hipp, Sara Crawford, Dmitry M. Kissin, and Denise J. Jamieson. 2016. Extremities of body mass index and their association with pregnancy outcomes in women undergoing in vitro fertilization in the United States, Fertility and Sterility 106(7): 1742–1750. https://doi.org/10.1016/j.fertnstert.2016.08.028
- Keizer, Renske, Pearl A. Dykstra, and Miranda D. Jansen. 2008. Pathways into childlessness: Evidence of gendered life course dynamics, Journal of Biosocial Science 40(6): 863–878. https://doi.org/10.1017/S0021932007002660
- Kreyenfeld, Michaela, and Dirk Konietzka. 2017. Childlessness in Europe: Contexts, Causes, and Consequences. Cham: Springer Nature.
- Krueger, Patrick M., Kate Coleman-Minahan, and Ronica N. Rooks. 2014. Race/ethnicity, nativity and trends in BMI among U.S. adults, Obesity 22(7): 1739–1746. https://doi.org/10.1002/oby.20744
- Krueger, Patrick M., and Eric N. Reither. 2015. Mind the gap: Race/ethnic and socioeconomic disparities in obesity, Current Diabetes Reports 15(11): 95. https://doi.org/10.1007/s11892-015-0666-6
- Kwan, Samantha. 2009. Competing motivational discourses for weight loss: Means to ends and the nexus of beauty and health, Qualitative Health Research 19(9): 1223–1233. https://doi.org/10.1177/1049732309343952
- La Rocque, Cherie L., and Jan Cioe. 2011. An evaluation of the relationship between body image and sexual avoidance, Journal of Sex Research 48(4): 397–408. https://doi.org/10.1080/00224499.2010.499522
- Leech, Tamara G. J., and Janice Johnson Dias. 2012. Risky sexual behavior: A race-specific social consequence of obesity, Journal of Youth and Adolescence 41(1): 41–52. https://doi.org/10.1007/s10964-011-9670-6
- Luke, Barbara, Morton B. Brown, Stacey A. Missmer, Orhan Bukulmez, Richard Leach, and Judy E. Stern. 2011. The effect of increasing obesity on the response to and outcome of assisted reproductive technology: A national study, Fertility and Sterility 96(4): 820–825. https://doi.org/10.1016/j.fertnstert.2011.07.1100
- Lundquist, Jennifer Hickes, Michelle J. Budig, and Anna Curtis. 2009. Race and childlessness in America, 1988–2002, Journal of Marriage and Family 71(3): 741–755. https://doi.org/10.1111/j.1741-3737.2009.00630.x
- MaCurdy, Thomas, Thomas Mroz, and R. Mark Gritz. 1998. An evaluation of the national longitudinal survey on youth, The Journal of Human Resources 33(2): 345–436. https://doi.org/10.2307/146435
- Makowski, Dominique, Mattan S. Ben-Shachar, and Daniel Lüdecke. 2019. Bayestestr: Describing effects and their uncertainty, existence and significance within the Bayesian framework, Journal of Open Source Software 4(40): 1541. https://doi.org/10.21105/joss.01541
- McCreary, Donald R., and Doris K. Sasse. 2000. An exploration of the drive for muscularity in adolescent boys and girls, Journal of American College Health 48(6): 297–304. https://doi.org/10.1080/07448480009596271
- McCreary, Donald R., and Stanley W. Sadava. 2001. Gender differences in relationships among perceived attractiveness, life satisfaction, and health in adults as a function of body mass index and perceived weight, Psychology of Men & Masculinity 2(2): 108–116. https://doi.org/10.1037/1524-9220.2.2.108
- McCreary, Donald R. 2002. Gender and age differences in the relationship between body mass index and perceived weight: Exploring the paradox, International Journal of Men's Health 1(1): 31–42. https://doi.org/10.3149/jmh.0101.31
- McElreath, Richard. 2020. Statistical Rethinking: A Bayesian Course with Examples in R and STAN, 2nd ed. London: Chapman & Hall.
- Menigoz, Karen, Andrea Nathan, and Gavin Turrell. 2016. Ethnic differences in overweight and obesity and the influence of acculturation on immigrant bodyweight: Evidence from a national sample of Australian adults, BMC Public Health 16(1): 932. https://doi.org/10.1186/s12889-016-3608-6
- Miller, Katherine J., David H. Gleaves, Tera G. Hirsch, Bradley A. Green, Alicia C. Snow, and Chanda C. Corbett. 2000. Comparisons of body image dimensions by race/ethnicity and gender in a university population, International Journal of Eating Disorders 27(3): 310–316. https://doi.org/10.1002/(sici)1098-108x(200004)27:3<310::aid-eat8>3.0.co;2-q
- Mintz, Laurie B., and Susan Kashubeck. 1999. Body image and disordered eating among Asian American and Caucasian College students: An examination of race and gender differences, Psychology of Women Quarterly 23(4): 781–796. https://doi.org/10.1111/j.1471-6402.1999.tb00397.x
- Moradi, Sajjad, Atieh Mirzababaei, Hamed Mohammadi, Seyedeh Parisa Moosavian, Arman Arab, Behrooz Jannat, and Khadijeh Mirzaei. 2019. Food insecurity and the risk of undernutrition complications among children and adolescents: A systematic review and meta-analysis, Nutrition 62: 52–60. https://doi.org/10.1016/j.nut.2018.11.029
- Musick, Kelly, Paula England, Sarah Edgington, and Nicole Kangas. 2009. Education differences in intended and unintended fertility, Social Forces 88(2): 543–572. https://doi.org/10.1353/sof.0.0278
- Muth, Chelsea, Zita Oravecz, and Jonah Gabry. 2018. User-friendly Bayesian regression modeling: A tutorial with rstanarm and shinystan, The Quantitative Methods for Psychology 14(2): 99–119. https://doi.org/10.20982/tqmp.14.2.p099
- Myers, Ana McCormick, and Matthew A. Painter. 2017. Food insecurity in the United States of America: An examination of race/ethnicity and nativity, Food Security 9(6): 1419–1432. https://doi.org/10.1007/s12571-017-0733-8
- Neff, Linda J., Roger G. Sargent, Robert E. McKeown, Kirby L. Jackson, and Robert F. Valois. 1997. Black–White differences in body size perceptions and weight management practices among adolescent females, Journal of Adolescent Health 20(6): 459–465. https://doi.org/10.1016/S1054-139X(96)00273-X
- Nguyen, Ruby H. N., Allen J. Wilcox, Rolv Skjærven, and Donna D. Baird. 2007. Men’s body mass index and infertility, Human Reproduction 22(9): 2488–2493. https://doi.org/10.1093/humrep/dem139
- Nitsche, Natalie, and Sarah R. Hayford. 2020. Preferences, partners, and parenthood: Linking early fertility desires, marriage timing, and achieved fertility, Demography 57: 1975–2001. https://doi.org/10.1007/s13524-020-00927-y
- Ombelet, W., and J. Goossens. 2017. Global reproductive health – Why do we persist in neglecting the undeniable problem of childlessness in resource-poor countries?, Facts, Views & Vision in ObGyn 9(1): 1–3.
- Pasquali, Renato, Laura Patton, and Alessandra Gambineri. 2007. Obesity and infertility. Current Opinion in Endocrinology, Diabetes and Obesity 14(6): 482–487. https://doi.org/10.1097/MED.0b013e3282f1d6cb
- Pearl, Rebecca L., Thomas A. Wadden, J. Shaw Tronieri, Ariana M. Chao, Naji Alamuddin, and Robert I. Berkowitz. 2018. Everyday discrimination in a racially diverse sample of patients with obesity, Clinical Obesity 8(2): 140–146. https://doi.org/10.1111/cob.12235
- Powell, Andrea D., and Arnold S. Kahn. 1995. Racial differences in women’s desires to be thin, International Journal of Eating Disorders 17(2): 191–195. https://doi.org/10.1002/1098-108x(199503)17:2<191::aid-eat2260170213>3.0.co;2-z
- Puhl, Rebecca, and Kelly D. Brownell. 2001. Bias, discrimination, and obesity, Obesity Research 9(12): 788–805. https://doi.org/10.1038/oby.2001.108
- Raley, R. Kelly, Megan M. Sweeney, and Danielle Wondra. 2015. The growing racial and ethnic divide in U.S. marriage patterns, The Future of Children 25(2): 89–109. https://doi.org/10.1353/foc.2015.0014
- Ramlau-Hansen, Cecilia H., Ane Marie Thulstrup, E. A. Nohr, Jens Peter Bonde, T. I. A. Sørensen, and Jørn Olsen. 2007. Subfecundity in overweight and obese couples, Human Reproduction 22(6): 1634–1637. https://doi.org/10.1093/humrep/dem035
- R Core Team. 2021. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Retrieved from https://www.R-project.org/.
- Rohrer, Julia M. 2018. Thinking clearly about correlations and causation: Graphical causal models for observational data, Advances in Methods and Practices in Psychological Science 1(1): 27–42. https://doi.org/10.1177/2515245917745629
- Rossen, Lauren M., and Kenneth C. Schoendorf. 2012. Measuring health disparities: Trends in racial−ethnic and socioeconomic disparities in obesity among 2- to 18-year old youth in the United States, 2001–2010, Annals of Epidemiology 22(10): 698–704. https://doi.org/10.1016/j.annepidem.2012.07.005
- Rothstein, Donna S., Deborah Carr, and Elizabeth Cooksey. 2019. Cohort profile: The National Longitudinal Survey of Youth 1979 (NLSY79), International Journal of Epidemiology 48(1): 22–22e. https://doi.org/10.1093/ije/dyy133
- Saarela, Jan and Vegard Skirbekk. 2020. Childlessness and union histories: Evidence from Finnish population register data, Journal of Biosocial Science 52(1): 78–96. https://doi.org/10.1017/S0021932019000257
- Sear, Rebecca and Frank W. Marlowe. 2009. How universal are human mate choices? Size does not matter when Hadza foragers are choosing a mate, Biology Letters 5(5): 606–609. https://doi.org/10.1098/rsbl.2009.0342
- Sermondade, N., C. Faure, L. Fezeu, A. G. Shayeb, J. P. Bonde, T. K. Jensen, M. Van Wely, et al. 2013. BMI in relation to sperm count: An updated systematic review and collaborative meta-analysis, Human Reproduction Update 19(3): 221–231. https://doi.org/10.1093/humupd/dms050
- Smelser, Neil J., William Julius Wilson, and Faith Mitchell. 2001. America Becoming: Racial Trends and Their Consequences, Volume 1. Washington, DC: National Academies Press.
- Sohn, Kitae. 2016. The fatter are happier in Indonesia, Quality of Life Research 2(26): 393–402. https://doi.org/10.1007/s11136-016-1403-6
- Sotiriou, Elysia G. and Germine H. Awad. 2020. Cultural influences on body image and body esteem, in Diane F. Halpern and Fanny M. Cheung (eds), The Cambridge Handbook of the International Psychology of Women, pp. 190–204. Retrieved from https://www.cambridge.org/core/books/cambridge-handbook-of-the-international-psychology-of-women/cultural-influences-on-body-image-and-body-esteem/131A8E030BA6DDA68F64DE625350F364
- Spahlholz, J., N. Baer, H.-H. König, S. G. Riedel-Heller, and C. Luck-Sikorski. 2016. Obesity and discrimination - A systematic review and meta-analysis of observational studies, Obesity Reviews 17(1): 43–55. https://doi.org/10.1111/obr.12343
- Stulp, Gert, Rebecca Sear, Susan B. Schaffnit, Melinda C. Mills, and Louise Barrett. 2016. The reproductive ecology of industrial societies, part II, Human Nature 27(4): 445–470. https://doi.org/10.1007/s12110-016-9272-9
- Swami, Viren. 2006. The influence of body weight and shape in determining female and male physical attractiveness. In Advances in Psychology Research Vol. 55, edited by A. Columbus, 195–220. Nova Science Publishers.
- Swami, Viren, Jan Smith, Athena Tsiokris, Chrissa Georgiades, Yolanda Sangareau, Martin J. Tovée, and Adrian Furnham. 2007. Male physical attractiveness in Britain and Greece: A cross-cultural study, The Journal of Social Psychology 147(1): 15–26. https://doi.org/10.3200/SOCP.147.1.15-26
- Sweeney, Megan M., and R. Kelly Raley. 2014. Race, ethnicity, and the changing context of childbearing in the United States, Annual Review of Sociology 40(1): 539–558. https://doi.org/10.1146/annurev-soc-071913-043342
- Talmor, Alon and Bruce Dunphy. 2015. Female obesity and infertility, Best Practice & Research Clinical Obstetrics & Gynaecology 29(4): 498–506. https://doi.org/10.1016/j.bpobgyn.2014.10.014
- Textor, Johannes, Benito van der Zander, Mark S. Gilthorpe, Maciej Liśkiewicz, and George T. H. Ellison. 2017. Robust causal inference using directed acyclic graphs: The R package ‘dagitty’, International Journal of Epidemiology 45(6): 1887–1894. https://doi.org/10.1093/ije/dyw341
- Torres, Andrés F. Castro, and Emilio Alberto Parrado. 2022. Nativity differentials in first births in the United States: Patterns by race and ethnicity, Demographic Research 46: 37–64. https://doi.org/10.4054/DemRes.2022.46.2
- Tovée, Martin J., Douglas S. Maisey, Ellen L. E. Vale, and Piers L. Cornelissen. 1999. Characteristics of male attractiveness for women, The Lancet 353(9163): 1500. https://doi.org/10.1016/S0140-6736(99)00438-9
- Trimarchi, Alessandra and Jan Van Bavel. 2017. Education and the transition to fatherhood: The role of selection into union, Demography 54(1): 119–144. https://doi.org/10.1007/s13524-016-0533-3
- Vehtari, Aki, Andrew Gelman, and Jonah Gabry. 2017. Practical Bayesian model evaluation using leave-one-out cross-validation and WAIC, Statistics and Computing 27(5): 1413–1432. https://doi.org/10.1007/s11222-016-9696-4
- Ventura, Stephanie J. and Christine A. Bachrach. 2000. Nonmarital childbearing in the United States, 1940-99. No. 48–16: 46. ERIC.
- Yang, Yang Claire, Christine E. Walsh, Moira P. Johnson, Daniel W. Belsky, Max Reason, Patrick Curran, Allison E. Aiello, et al. 2021. Life-course trajectories of body mass index from adolescence to old age: Racial and educational disparities, Proceedings of the National Academy of Sciences 118(17). https://doi.org/10.1073/pnas.2020167118
- Żurawiecka, Martyna and Iwona Wronka. 2021. Association between age at menarche and body mass index, waist circumference, waist to hip ratio, and waist to height ratio in adult women, American Journal of Human Biology 33(6): e23523. https://doi.org/10.1002/ajhb.23523
