ABSTRACT
Background: Precise terminology and definitions are important components of scientific language. Although the terms “hard drugs” and “soft drugs” are used widely by professionals, neither the International Classification of Diseases nor the Diagnostic and Statistical Manual classify psychoactive substances into the categories “hard” and “soft.”
Objectives: To analyze the occurrence of the terms “hard drugs” and “soft drugs” in recent scientific literature and to establish the degree of consensus in labeling psychoactive substances as “hard” or “soft.”
Methods: A critical review of scientific papers listed in PubMed and Scopus between 2011 and 2015. Three hundred thirty-four articles were initially identified as potentially relevant for review, 132 of which were included in the final analysis.
Results: One hundred twenty-four articles used the term “hard drugs” and 84.7% provided examples of substances considered “hard.” Forty-four articles used the term “soft drugs” and 90.9% provided examples of substances considered “soft.” Citations of relevant articles supporting categorization as “hard” or “soft” were not given in 90% of the articles. The authors often provided no or only very sparse information on their reasons for considering specific drugs as “hard” or “soft.”
Conclusions: Although it initially appeared that there is substantial agreement as to which psychoactive substances should be regarded as “hard” and “soft,” closer inspection shows that the dividing line is blurred without clear criteria for categorization. At this time, it remains uncertain whether these terms should persist in the scientific literature. We therefore recommend these terms should be avoided or, if used, be clearly and precisely defined.
Introduction
Precise terminology and definitions are important components of scientific language. If their meaning is clear, they help in understanding research findings, avoiding confusion and risks, and communicating results to healthcare professionals in clinical practice.
However, the terminology in the field of drug addiction is often unclear since the terms used are often confusing or contradictory. Several attempts have been made to standardize usage and to reduce misunderstandings and confusion, but many challenges still remain, such as the blurred dividing lines between popular and scientific definitions of key terms (Citation1). Popular terms are used in scientific presentations, and scientific terms gradually undergo a process of popularization. A few examples that illustrate such overlaps may be pointed out with marijuana (e.g., “grass” vs. cannabis in public vs. research communication, respectively) (Citation2), amphetamine-type stimulants (“ecstasy” vs. MDMA) (Citation3), or newer synthetic drugs (“bath salts” vs. synthetic cathinones) (Citation4).
The terms “hard drugs” and “soft drugs” are popular in both lay language and the media. They also appear in respectful international multimedia news agencies (Citation5), which, conversely, may have an impact on disseminating the terms in the public. In addition, these terms have been used in the medical literature since at least 1968 (Citation6), and they are even found in current systematic reviews (Citation7). We believe Denise Kandel’s work in the 1970s had a significant influence on this terminology although she did not explicitly use the terms (Citation8), namely by initiation of the “gateway hypothesis” in which certain drugs (e.g., alcohol or tobacco cigarettes) tend to serve as a gateway for the use of other substances (e.g., cannabinoids) which itself tends to precede the use of other illicit drugs (Citation9). Finally, the origins of the terms can be traced back to specific national legislative documents (Citation10–Citation12). In the Netherlands, for example, the regulations on drugs are laid down in the Opium Act (Citation10), which, according to some authors, implicitly draws a distinction between “hard drugs” and “soft drugs” by separating the market and allowing controlled use of specified substances while possession of others is a crime (Citation13).
Although they are used widely by professionals, the terms “hard” and “soft” have not been standardized. Neither the International Classification of Diseases (ICD-10) nor the Diagnostic and Statistical Manual (DSM-5) classify psychoactive substances into the categories “hard” and “soft” (Citation14,Citation15). It is generally assumed that the terms are ambiguous and that a scientific basis for such a classification is lacking (Citation16).
Addictive behaviors can be viewed as a social phenomenon, and their definitions and classifications as social constructs (Citation17). Social constructs can be indifferent or interactive (Citation18). Indifferent constructs do not affect the object of conceptualization, but this might be applied to the “neutral” classification of psychoactive substances using the ICD-10 and DSM-5 criteria. The terms “hard drugs” and “soft drugs” are, however, interactive because they are used by people and influence the experience of those taking them, i.e., “hard drug” and “soft drug” users, as well as those who interact with them in different ways. Furthermore, the usage of these terms may have an impact on public perception, interpretation of research findings, and management of substance-use disorders.
The crucial question is how and why authors use the terms “hard drugs” and “soft drugs” in the current scientific literature, in what contexts, and what they actually mean by them. To our knowledge, no systematic review has yet been conducted in this area.
Aims
The aim of this review was to analyze the occurrence patterns of the terms “hard drugs” and “soft drugs” in the current scientific literature to establish the degree of consensus in labeling specific psychoactive substances with these terms.
Methods
Quantitative content analysis of selected scientific papers published from 2011 to 2015 was performed to analyze the occurrence of the terms and the patterns of their use for the categorization of psychoactive substances.
Literature search
To generate data for the analysis, we conducted literature searches in PubMed and Scopus in September 2016. The search included the keywords “hard drug*” OR “soft drug*” in the title or abstract of the articles published in extenso or online between January 1, 2011 and December 31, 2015. The search period of the past five years was chosen for depiction of the most recent approach to the categorization. After the initial search, titles and abstracts were screened, followed by review of the full text of the remaining articles. All the articles were independently reviewed by two authors and discrepancies were resolved by consensus.
Papers were excluded if they did not use the keywords in the context of psychoactive substances. Full texts using the keywords but not providing examples of specific drugs and articles with unclear conclusions on the labeling of specific substances were also excluded. Since we intended to obtain a broad spectrum of different authors’ views on categorization, only the first published articles from series of articles were included. No language limitations were applied.
Three hundred thirty-four articles were initially identified as potentially relevant for the review. Based on the search criteria and after additional review of the abstracts, 132 of the articles were included in the final analysis ( and ) (Citation19–Citation150).
Table 1. Final sample of publications.
Analysis of terms
To analyze the terminology, we recorded all substances identified by authors as “hard drugs” or “soft drugs” either explicitly by labeling specific substances or implicitly by direct assignment as opposed to labeled substances. To obtain a more precise delineation between the many substances identified, we allocated them into 10 groups following the ICD-10 and DSM-5 classifications: alcohol, caffeine, tobacco/nicotine, anxiolytics/hypnotics, opioids, cannabinoids, cocaine, amphetamine stimulants, hallucinogens, and volatiles (Citation14,Citation15). Unexplained groups of substances identified in articles such as “illicit drugs,” “injection drugs,” “stimulants,” and “depressants” were analyzed separately.
Results
Based on our selection criteria, all 132 articles listed at least one example of “hard” or “soft” drugs. Only 44 (33.3%) articles provided examples of both “hard” and “soft” drugs. The term “hard drugs” was used in 124 (93.9%) articles, 84.7% of which provided any example of substances considered as “hard.” Only 44 (33.3%) articles used the term “soft drugs,” 90.9% of which provided any example of substances considered “soft.”
shows the occurrence of major substance groups categorized by examples of specific substances as either as “hard” or “soft” drugs in the final sample of articles. Only 17 (12.9%) of the 132 articles covered more than half of the major substance groups in their categorization of specific substances, and 53.0% of the articles categorized specific substances from three major groups of substances or fewer.
Table 2. Occurrence of categorized substance groups in the final sample of articles.
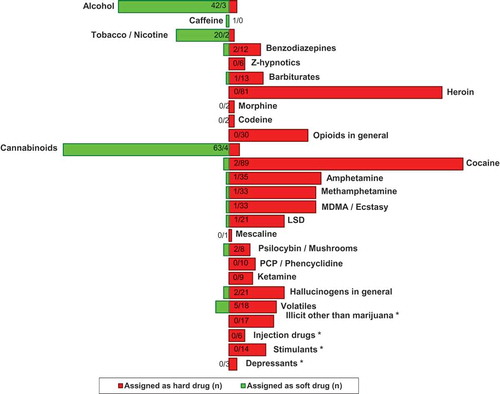
shows, by major substance group, the categorization of specific substances into “hard” or “soft” drugs as assigned by authors in the 132 articles. Newly discovered drugs (e.g., benzylpiperazine or mephedrone) were not mentioned in any of the articles, although gammahydroxy-butyrate (GHB) appeared in 13 articles and was categorized exclusively as a “hard drug.” Only 13 (9.8%) of the articles referred to an external bibliographic source that supported their categorization of substances and only 24 (18.2%) of the articles provided any specific rationale for categorization as such.
Figure 2. Assignment of specific substances as “soft” or “hard” drugs in the final sample of articles. Numbers in the bars are the number of articles in which the substance was identified as a “soft” or “hard” drug, respectively. For example, 63/4 in the cannabinoids bar means that marijuana or hashish was categorized as “soft” in 63 articles and as “hard” in 4 articles. *No further explanation or examples of specific substances given by authors.
Discussion
The occurrence of the terms “hard drug” and “soft drug” in a sample of 132 scientific articles concerned with the use of psychoactive substances published between 2011 and 2015 shows that these terms are in common use.
Most authors used the term “hard drug” for opioids, anxiolytics/hypnotics, amphetamines, cocaine, hallucinogens, volatiles, and GHB. The term “soft drug” was primarily used for cannabinoids, alcohol, and tobacco.
An incomplete list of substances for a particular category (“hard” or “soft”) and insufficient categorization of all major substance classes according to ICD-10 or DSM-5 was found in most of the studied articles. This is underlined by the finding that 36 (27.3%) articles categorized vaguely defined groups of substances, such as illicit or injection drugs, stimulants, and depressants, as “hard drugs” without offering any specific examples. Notably, authors of 17 (12.8%) of the articles merely distinguished other illicit drugs from marijuana when speaking about “hard drugs.”
The reason for categorizing substances was not clear in most of the articles, and authors often gave no or only little information on how they reached their decision that a drug is “hard” or “soft.” Citations of relevant articles supporting categorization were not given in 90% of the articles. Moreover, 103 (78.0%) of the articles provided neither citations nor rationale for what they meant by “hard” or “soft” drugs. Finally, 23 (17.4%) of the articles included the terms in quotations which possibly showed the authors had no intention to mislead readers and implied their agreement that the terms were somewhat ambiguous. We think that these findings may indicate the uncertainty of the authors themselves within the categorization of substances into “hard” and “soft.”
Caffeine was considered in only one article and was labeled as a “soft drug” (Citation62). Although caffeine addiction (caffeine substance-use disorder) is not classified in DSM-5, it is still classified in ICD-10) (Citation14,Citation15). Its use is very prevalent (Citation151) and may have complications such as intoxication and a withdrawal state (Citation15). From this point of view, it is not clear why it was hardly ever categorized in any of the 132 articles we reviewed.
In the articles where alcohol was mentioned, it was labeled as “soft drug” by most authors (93.3%). This is surprising especially when comparing alcohol with benzodiazepines, which were categorized as “hard drugs” in 85.7% of the articles where they were mentioned. It is of note that in another study using a card sorting test in a sample of university students, both alcohol and benzodiazepines were substances with no consensus on categorization as “hard” or “soft” (Citation62). Many experts see alcohol as a most harmful drug, and benzodiazepines are perceived as far less harmful (Citation152). Alcohol, like the benzodiazepines, acts on the GABA-A (γ-aminobutyric acid) receptors in the brain (Citation153,Citation154) and both demonstrate significant clinical parallels in addiction and addictive potential (Citation153,Citation155). We feel that the difference between alcohol and benzodiazepines with regard to categorization as “hard” or “soft” in our review may possibly be due to inadequate differentiation from other substances and also partly due to the social acceptance of alcohol. Alcohol was not categorized in seven of the 12 articles where benzodiazepines were categorized, and benzodiazepines were not categorized in 40 of the 45 articles where alcohol was categorized. In the remaining five articles where both were categorized, alcohol was labeled as a “hard drug.”
Heroin was mentioned in 61.4% of the articles and was labeled exclusively as “hard drug.” However, only eight of the articles gave any specific rationale for categorization such as:
Monshouwer et al. (2011): “…hard drugs […] are considered to pose an unacceptable risk to public health, such as heroin…” (Citation39).
Tennsted and Saint-Remy (2011): “cannabis, which is traditionally recognized as a soft drug (as it entails no physical addiction nor death from overdose), as opposed to hard drugs such as heroin […]…” (Citation43).
Blomqvist et al. (2012): “…addiction to what has in this study been classified as “hard” drugs (heroin […]), is seen as a ‘disease’ that the individual user is struck by, and which she/he cannot resolve, at least not without professional help […] ‘hard’ drugs […] are perceived as a very large threat to society…” (Citation46).
Palamar et al. (2012): “harder, more dangerous drugs […] appear to remain associated with higher levels of stigma […] drugs that are more harmful and addicting, such as heroin…” (Citation60).
Wouters et al. (2012): “…hard drugs (heroin […]), which are viewed as more hazardous to health…” (Citation73).
Samuelsson et al. (2013): “…hard narcotic drugs, that is, heroin […] which are judged to be very dangerous to society, highly addictive and very difficult to quit…” (Citation92).
Vos et al. (2013): “Soft drugs […] are regarded to pose fewer risks to public health than hard drugs such as heroin…” (Citation97).
Kelly and Rasul (2014): “…hard drugs, known as ‘Class-A’ drugs in England (intended to indicate increasing potential harm to users) include […] heroin…” (Citation111).
Even in this very small sample of eight publications, the authors use at least five different aspects to arrive at the categorization as a “hard drug”: (1) addictive potential; (2) physical addiction with physical withdrawal state; (3) assumed harm to user; (4) poor prognosis of addiction remission; and (5) assumed harm to public health and society.
Our critical review of 132 articles raises important questions with regard to the categorization of psychoactive substances as “hard” or “soft” drugs. The terms are often used in the literature but explanations for categorization as “hard” or “soft” are rarely given. “Hardness” or “softness” may refer to different aspects of psychoactive substances and can be perceived differently when comparing only two or a small number of specific drugs rather than the entire spectrum of substances. The authors’ decisions seem to be often––but not exclusively––based on subjective clinical impressions that result in statistical uncertainty into scientific publications, which in turn brings confusion into evidence-based medicine (Citation98).
Inconsistencies in the published terminology may lead to confusion in clinical practice when specific substances are perceived differently with regard to their relationship with etiology, clinical picture and course, and the influence these considerations have on diagnostics, therapy and prognosis of different disorders. Furthermore, vague or inadequate usage of the terms by the media might have a negative impact on the views of public on the problems related to psychoactive substances. Critical analysis of terminology would be therefore needed to enhance the internal consistency of scientific publishing and to improve the application of research results in clinical practice. For example, much discussion and debate was required before more standardized terminology for the area of “quality of life” research was achieved (Citation156). We would need a similar approach if we wanted to arrive at more standardized criteria for the categorization of substances as “hard” and “soft” drugs and to consolidate scientific language in addiction research and avoid confusion and associated risks. From our point of view, the acceptable and correct use of the categorization in research, publishing, and clinical practice currently remains an unresolved issue.
Limitations
Our review focused on a quantitative analysis of the terms “hard drugs” and “soft drugs” in the literature. Because only a small number of articles we selected provided reasons for assignment to these categories, we were unable to perform systematic qualitative review. Moreover, with a few exceptions, individual articles did not directly compare specific substances within the selected categories (“hard” or “soft”) as this was not part of their aims. Our findings should therefore be viewed more as a collection of opinions than a measure of consensus.
Conclusion
The terms “hard” and “soft” drugs have been widely used in the scientific literature over the past five years. Although it initially appears that there is substantial agreement as to which psychoactive substances should be regarded as “hard” and “soft” drugs in the 132 articles we reviewed, closer inspection shows that the dividing line is often blurred. Authors often used only partial lists of known substances in different categories and did not categorize all of the main substance classes according to ICD or DSM. Authors also gave insufficient information regarding their criteria for deciding whether a drug was “hard” or “soft,” and citations supporting categorization were missing in 90% of the articles.
Based on our results, the distinction between “hard” and “soft” drugs in the published literature remains unclear for at least three reasons. First, consensus has not yet been reached on the complete range of substances requiring categorization. Second, grouping of substances into specific “hard” or “soft” category within their relation to other drugs is hardly ever considered. Third, thoroughly discussed and precisely defined criteria of “hardness” and “softness” are currently missing.
To avoid confusion in the future, we recommend not using the terms “hard drugs” and “soft drugs” in scientific publications unless adequately clarified and precisely specified by authors. In addition, the question whether there is a place for these terms in scientific literature at all is also relevant and should be a subject of a broader scientific discourse. Therefore, we suggest that editors and reviewers are cautious when they encounter these terms within the publishing process.
Acknowledgments
Language revision of the manuscript was done by A. Reeves of Ascribe, Wiesbaden, Germany.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- Babor TF, Hall W. Standardizing terminology in addiction science: to achieve the impossible dream. Addiction (Abingdon) 2007;102:1015–1018.
- Curran HV, Freeman TP, Mokrysz C, Lewis DA, Morgan CJA, Parsons LH. Keep off the grass? Cannabis, cognition and addiction. Nat Rev Neurosci 2016;17:293–306.
- Golding JF, Groome DH, Rycroft N, Denton Z. Cognitive performance in light current users and ex-users of ecstasy (MDMA) and controls. Am J Drug Alcohol Abuse 2007;33:301–307.
- Banks ML, Worst TJ, Rusyniak DE, Sprague JE. Synthetic cathinones (“bath salts”). J Emerg Med 2014;46:632–642.
- Emery G. Like regular cigarettes, e-cigs a gateway to harder drugs – study. Reuters 2014. [cited 2016 Sept 15]. Available from: http://www.reuters.com/article/heatlh-nicotine-ecigarettes-idUSL1N0R42P220140903.
- Klein J, Phillips DL. From hard to soft drugs: temporal and substantive changes in drug usage among gangs in a working-class community. J Health Soc Behav 1968;9:139–145.
- Faggiano F, Minozzi S, Versino E, Buscemi D. Universal school-based prevention for illicit drug use. Cochrane Database Syst Rev 2014;12:CD003020.
- Kandel D. Stages in adolescent involvement in drug use. Science 1975;190:912–914.
- Kandel D, Kandel E. The Gateway Hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatr (Oslo, Norway) 2015;104:130–137.
- European Monitoring Centre for Drugs and Drug Addiction. EMCDDA Country legal profile – The Netherlands [Internet]. EMCDDA 2012. [cited 2016 Sept 15]. Available from: http://www.emcdda.europa.eu/html.cfm/index5174EN.html?pluginMethod=eldd.countryprofiles&country=NL.
- European Monitoring Centre for Drugs and Drug Addiction. EMCDDA Country legal profile – United Kingdom [Internet]. EMCDDA 2012. [cited 2016 Sept 15]. Available from: http://www.emcdda.europa.eu/html.cfm/index5174EN.html?pluginMethod=eldd.countryprofiles&country=UK.
- U.S. Department of Justice. Title 21 United States Code Controlled Substances Act [Internet]. 2012. [ cited 2016 Sept 15]. Available from: http://www.deadiversion.usdoj.gov/21cfr/21usc/.
- van Ours JC. Is cannabis a stepping-stone for cocaine? J Health Econ 2003;22:539–554.
- World Health Organization. The ICD-10 Classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993. 248 p.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Fifth Edition. Washington: American Psychiatric Association; 2013. 991 p.
- Marion NE, Oliver WM. Drugs in American society: an encyclopedia of history, politics, culture, and the law: an encyclopedia of history, politics, culture, and the Law. ABC-CLIO; 2014. 1163 p.
- Hellman M, Einstein S. Encoding and decoding substance use and addictive behaviors––the roles of cultural images. Subst Use Misuse 2015;50:415–418.
- Hacking I. The social construction of what? Cambridge: Harvard University Press; 1999. 272 p.
- Amundsen EJ, Bretteville-Jensen AL, Kraus L. A method to estimate total entry to hard drug use: the case of intravenous drug use in Norway. Eur Addict Res 2011;17:129–135.
- Bekele AB, van Aken MAG, Dubas JS. Sexual violence victimization among female secondary school students in eastern Ethiopia. Violence Vict 2011;26:608–630.
- Branstetter SA, Low S, Furman W. The Influence of Parents and Friends on Adolescent Substance Use: A Multidimensional Approach. J Subst Use 2011;16:150–160.
- Bretteville-Jensen AL, Jacobi L. Climbing the drug staircase: a Bayesian analysis of the initiation of hard drug use. J Appl Econom. 2011;26:1157–1186.
- Cohn SE, Jiang H, McCutchan JA, Koletar SL, Murphy RL, Robertson KR, et al. Association of ongoing drug and alcohol use with non-adherence to antiretroviral therapy and higher risk of AIDS and death: results from ACTG 362. AIDS Care 2011;23:775–785.
- Dabbaghian V, Spicer V, Singh SK, Borwein P, Brantingham P. The social impact in a high-risk community: a cellular automata model. J Comput Sci 2011;2:238–246.
- Feldstein E, Venner KL, Mead HK, Bryan AD. Exploring racial/ethnic differences in substance use: a preliminary theory-based investigation with juvenile justice-involved youth. BMC Pediatr 2011;11:71.
- Flynn RJ, Tessier NG. Promotive and risk factors as concurrent predictors of educational outcomes in supported transitional living: extended care and maintenance in Ontario, Canada. Child Youth Serv Rev 2011;33:2498–2503.
- Freeman P, Walker BC, Harris DR, Garofalo R, Willard N, Ellen JM, et al. Methamphetamine use and risk for HIV among young men who have sex with men in 8 US cities. Arch Pediatr Adolesc Med 2011;165:736–740.
- Friedman SR, Pouget ER, Chatterjee S, Cleland CM, Tempalski B, Brady JE, et al. Drug arrests and injection drug deterrence. Am J Publ Health 2011;101:344–349.
- Glover M, Kira A, Min S, Scragg R, Nosa V, McCool J, et al. Smoking is rank! But, not as rank as other drugs and bullying say New Zealand parents of pre-adolescent children. Health Promot J Aust 2011;22:223–237.
- Grella CE, Rodriguez L. Motivation for treatment among women offenders in prison-based treatment and longitudinal outcomes among those who participate in community aftercare. J Psychoactive Drugs 2011:58–67.
- Huemer HP, Lassnig C, Bernhard D, Sturm S, Nowotny N, Kitchen M, et al. Cannabinoids lead to enhanced virulence of the smallpox vaccine (vaccinia) virus. Immunobiology 2011;216:670–677.
- Hunt K, Sweeting H, Sargent J, Lewars H, Young R, West P. Is there an association between seeing incidents of alcohol or drug use in films and young Scottish adults’ own alcohol or drug use? A cross sectional study. BMC Publ Health 2011;11:259.
- Christensen BS, Grønbaek M, Pedersen BV, Graugaard C, Frisch M. Associations of unhealthy lifestyle factors with sexual inactivity and sexual dysfunctions in Denmark. J Sex Med 2011;8:1903–1916.
- Järvinen M, Demant J. The normalisation of cannabis use among young people: symbolic boundary work in focus groups. Health Risk Soc 2011;13:165–182.
- Jenness SM, Neaigus A, Murrill CS, Gelpi-Acosta C, Wendel T, Hagan H. Recruitment-adjusted estimates of HIV prevalence and risk among men who have sex with men: effects of weighting venue-based sampling data. Publ Health Rep 2011;126:635–642.
- Johnson JE, Friedmann PD, Green TC, Harrington M, Taxman FS. Gender and treatment response in substance use treatment-mandated parolees. J Subst Abuse Treat 2011;40:313–321.
- McCart MR, Zajac K, Danielson CK, Strachan M, Ruggiero KJ, Smith DW, et al. Interpersonal victimization, posttraumatic stress disorder, and change in adolescent substance use prevalence over a ten-year period. J Clin Child Adolesc Psychol 2011;40:136–143.
- Menéndez RG. [Taxonomic criterium for the alcohol consumption patterns]. Rev Cuba Salud Publica 2011;37:132–143.
- Monshouwer K, Van Laar M, Vollebergh WA. Buying cannabis in “coffee shops”. Drug Alcohol Rev 2011;30:148–156.
- Nijhof KS, Vermulst A, Scholte RHJ, van Dam C, Veerman JW, Engels RCME. Psychopathic traits of Dutch adolescents in residential care: identifying subgroups. J Abnorm Child Psychol 2011;39:59–70.
- O’Cathail SM, O’Connell OJ, Long N, Morgan M, Eustace JA, Plant BJ, et al. Association of cigarette smoking with drug use and risk taking behaviour in Irish teenagers. Addict Behav 2011;36:547–550.
- Shook JJ, Vaughn M, Goodkind S, Johnson H. An empirical portrait of youthful offenders who sell drugs. J Crim Justice 2011;39:224–231.
- Tennstedt D, Saint-Remy A. Cannabis and skin diseases. Eur J Dermatol 2011;21:5–11.
- Vinkers DJ, de Beurs E, Barendregt M, Rinne T, Hoek HW. The relationship between mental disorders and different types of crime. Crim Behav Ment Health 2011;21:307–320.
- Akiibinu MO, Ogundahunsi OA, Ogunyemi EO. Inter-relationship of plasma markers of oxidative stress and thyroid hormones in schizophrenics. BMC Res Notes 2012;5:169.
- Blomqvist J. Perceptions of addiction and recovery in Sweden: the influence of respondent characteristics. Addict Res Theory 2012;20:435–446.
- Boman JH, Stogner JM, Miller BL, Griffin OH, Krohn MD. On the operational validity of perceptual peer delinquency: exploring projection and elements contained in perceptions. J Res Crime Delinquency 2012;49:601–621.
- Cao L, Zhao R. The impact of culture on acceptance of soft drugs across Europe. J Crim Justice 2012;40:296–305.
- Csemy L, Zabransky T, Grohmannova K, Dvořáková Z, Brenza J, Janikova B. Adolescent heroin and methamphetamine users reassessed after 14 years: analysis of psychosocial characteristics. Ces Psychol 2012;56:505–544.
- Figlio D, Ludwig J. Sex, drugs, and catholic schools: private schooling and non-market adolescent behaviors. Ger Econ Rev 2012;13:385–415.
- Frank VA, Anker J, Tammi T. Drug user organizations in the Nordic countries – local, national, and international dimensions. Subst Use Misuse 2012;47:462–473.
- Friedmann PD, Green TC, Taxman FS, Harrington M, Rhodes AG, Katz E, et al. Collaborative behavioral management among parolees: drug use, crime and re-arrest in the Step’n Out randomized trial. Addiction (Abingdon) 2012;107:1099–1108.
- Hooshmand S, Willoughby T, Good M. Does the direction of effects in the association between depressive symptoms and health-risk behaviors differ by behavior? A longitudinal study across the high school years. J Adolesc Health 2012;50:140–147.
- Koski-Jännes A, Hirschovits-Gerz T, Pennonen M. Population, professional, and client support for different models of managing addictive behaviors. Subst Use Misuse 2012;47:296–308.
- Laroche F, Rostaing S, Aubrun F, Perrot S. Pain management in a patient addicted to hard drugs (heroin and cocaine) [Prise en charge de la douleur chez le toxicomane aux drogues dures (héroïne et cocaïne)]. Rev Rhum Ed Fr 2012;79:306–311.
- Lee C, White HR. Effects of childhood maltreatment on violent injuries and premature death during young adulthood among urban high-risk men. Arch Pediatr Adolesc Med 2012;166:814–820.
- Leech TGJ. Subsidized housing, public housing, and adolescent violence and substance use. Youth Soc 2012;44:217–235.
- Milburn NG, Iribarren FJ, Rice E, Lightfoot M, Solorio R, Rotheram-Borus MJ, et al. A family intervention to reduce sexual risk behavior, substance use, and delinquency among newly homeless youth. J Adolesc Health 2012;50:358–364.
- Oteo Pérez A, Benschop A, Korf DJ. Differential profiles of crack users in respondent-driven and institutional samples: a three-site comparison. Eur Addict Res 2012;18:184–192.
- Palamar JJ, Kiang MV, Halkitis PN. Predictors of stigmatization towards use of various illicit drugs among emerging adults. J Psychoactive Drugs 2012;44:243–251.
- Pereira RR, Kanhai H, Rosendaal F, Van D, Swaab D, Pereira ER, et al. Parenteral Pethidine for labour pain relief and substance use disorder: 20-Year follow-up cohort study in offspring. BMJ Open 2012;2:e000719.
- Quintero G. Problematizing “drugs”: a cultural assessment of recreational pharmaceutical use among young adults in the US. Contemp Drug Probl 2012;39:491.
- Rotheram-Borus MJ, Rice E, Comulada WS, Best K, Li L. Comparisons of HIV-affected and non-HIV-affected families over time. Vulnerable Child Youth Stud 2012;7:299–314.
- Ruttan L, Laboucane-Benson P, Munro B. Does a baby help young women transition out of homelessness? Motivation, coping, and parenting. J Fam Soc Work 2012;15:34–49.
- Seal DW, Parisot M, DiFranceisco W. Substance use and sexual behavior among men prior to parole revocation: prevalence and correlates. J Correct Health Care 2012;18:96–104.
- Shamblen SR, Miller T. Inhalant initiation and the relationship of inhalant use to the use of other substances. J Drug Educ 2012;42:327–346.
- Sussman S, Sun P, Rohrbach LA, Spruijt-Metz D. One-year outcomes of a drug abuse prevention program for older teens and emerging adults: evaluating a motivational interviewing booster component. Health Psychol 2012;31:476–485.
- Urgelles J, Donohue B, Wilks C, Van Hasselt VB, Azrin NH. A standardized method of preventing and managing emergencies within the context of evidence-based therapy implementation. Behav Modif 2012;36:558–579.
- van Amsterdam JGC, van Laar M, Brunt TM, van den Brink W. Risk assessment of gamma-hydroxybutyric acid (GHB) in the Netherlands. Regul Toxicol Pharmacol 2012;63:55–63.
- Vilalta CJ, Martinez JM. The making of Narco bosses: hard drug dealing crimes among Mexican students. Trends Organ Crime 2012;15:47–63.
- Vogel I, van de Looij-Jansen PM, Mieloo CL, Burdorf A, de Waart F. Risky music-listening behaviors and associated health-risk behaviors. Pediatrics 2012;129:1097–1103.
- Wenzel SL, Rhoades H, Hsu H-T, Golinelli D, Tucker JS, Kennedy DP, et al. Behavioral health and social normative influence: correlates of concurrent sexual partnering among heterosexually-active homeless men. AIDS Behav 2012;16:2042–2050.
- Wouters M, Benschop A, van Laar M, Korf DJ. Cannabis use and proximity to coffee shops in the Netherlands. Eur J Criminol 2012;9:337–353.
- Yeater EA, Lenberg KL, Bryan AD. Predictors of sexual aggression among male juvenile offenders. J Interpers Violence 2012;27:1242–1258.
- Akins S, Lanfear C, Cline S, Mosher C. Patterns and correlates of adult American Indian substance use. J Drug Issues 2013;43:497–516.
- Baggio S, Studer J, Mohler-Kuo M, Daeppen J-B, Gmel G. Profiles of drug users in Switzerland and effects of early-onset intensive use of alcohol, tobacco and cannabis on other illicit drug use. Swiss Med Wkly 2013;143:w13805.
- Ballester-Arnal R, Salmerón-Sánchez P, Gil-Llario MD, Giménez-Garcia C. The influence of drug consumption on condom use and other aspects related to HIV infection among male sex workers in Spain. AIDS Behav 2013;17:536–542.
- Bracken BK, Rodolico J, Hill KP. Sex, age, and progression of drug use in adolescents admitted for substance use disorder treatment in the northeastern United States: comparison with a national survey. Subst Abuse 2013;34:263–272.
- Farmer GW, Bucholz KK, Flick LH, Burroughs TE, Bowen DJ. CVD risk among men participating in the National Health and Nutrition Examination Survey (NHANES) from 2001–10: differences by sexual minority status. J Epidemiol Community Health 2013;67:772–778.
- Friedman SR, West BS, Pouget ER, Hall HI, Cantrell J, Tempalski B, et al. Metropolitan social environments and pre-HAART/HAART era changes in mortality rates (per 10,000 adult residents) among injection drug users living with AIDS. PloS One 2013;8:e57201.
- Gordon DM, Hawes SW, Reid AE, Callands TA, Magriples U, Divney A, et al. The many faces of manhood: examining masculine norms and health behaviors of young fathers across race. Am J Mens Health 2013;7:394–401.
- Hahm HC, Jang J, Vu C, Alexander LM, Driscoll KE, Lundgren L. Drug use and suicidality among Asian American women who are children of immigrants. Subst Use Misuse 2013;48:1563–1576.
- Hermanns-Lé T, Delvenne P, Piérard GE, Rousseau AF, Piérard-franchimont C. Risquer sa peau pour quelques “joints”. Rev Médicale Liège 2013;68:311–314.
- Illangasekare S, Burke J, Chander G, Gielen A. The syndemic effects of intimate partner violence, HIV/AIDS, and substance abuse on depression among low-income urban women. J Urban Health 2013;90:934–947.
- Kibusi SM, Ohnishi M, Outwater A, Seino K, Kizuki M, Takano T. Sociocultural factors that reduce risks of homicide in Dar es Salaam: a case control study. Inj Prev 2013;19:320–325.
- Lai MH, Graham JW, Caldwell LL, Smith EA, Bradley SA, Vergnani T, et al. Linking life skills and norms with adolescent substance use and delinquency in South Africa. J Res Adolesc 2013;23:128–137.
- Lanfear C, Akins S, Mosher C. Examining the relationship of substance use and sexual orientation. Deviant Behav 2013;34:586–597.
- Olthuis JV, Darredeau C, Barrett SP. Substance use initiation: the role of simultaneous polysubstance use. Drug Alcohol Rev 2013;32:67–71.
- Otiniano Verissimo AD, Gee GC, Iguchi MY, Ford CL, Friedman SR. Discrimination, drugs, and alcohol among Latina/os in Brooklyn, New York: differences by gender. Int J Drug Policy 2013;24:367–373.
- Phinney R. Exploring residential mobility among low-income families. Soc Serv Rev 2013;87:780–815.
- Ramanathan S, Balasubramanian N, Krishnadas R. Macroeconomic environment during infancy as a possible risk factor for adolescent behavioral problems. JAMA Psychiatry 2013;70:218–225.
- Samuelsson E, Blomqvist J, Christophs I. Addiction and recovery: perceptions among professionals in the Swedish treatment system. Nord Stud Alcohol Drugs. 2013;30:51–66.
- Siconolfi DE, Halkitis PN, Barton SC, Kingdon MJ, Perez-Figueroa RE, Arias-Martinez V, et al. Psychosocial and demographic correlates of drug use in a sample of HIV-positive adults ages 50 and older. Prev Sci 2013;14:618–627.
- Temple JR, Shorey RC, Fite P, Stuart GL, Le VD. Substance use as a longitudinal predictor of the perpetration of teen dating violence. J Youth Adolesc 2013;42:596–606.
- van Gastel WA, Tempelaar W, Bun C, Schubart CD, Kahn RS, Plevier C, et al. Cannabis use as an indicator of risk for mental health problems in adolescents: a population-based study at secondary schools. Psychol Med 2013;43:1849–1856.
- Vinkers DJ, Selten JP, Hoek HW, Rinne T. Psychotic disorders are more common in ethnic minority than in Dutch native defendants. Soc Psychiatry Psychiatr Epidemiol 2013;48:1399–1404.
- Vos HMM, Schellevis FG, van den Berkmortel H, van den Heuvel LGAM, Bor HHJ, Lagro-Janssen ALM. Does prevention of risk behaviour in primary care require a gender-specific approach? A cross-sectional study. Fam Pract 2013;30:179–184.
- Amato L, Davoli M. Drug addiction: between classification and social and health policies [Tossicodipendenze: Tra classificazione e politiche socio-sanitarie]. Recenti Prog Med 2014;105:91–92.
- Baumann M, Chau K, Kabuth B, Chau N. Association between health-related quality of life and being an immigrant among adolescents, and the role of socioeconomic and health-related difficulties. Int J Environ Res Publ Health 2014;11:1694–1714.
- Blomqvist J, Koski-Jännes A, Cunningham J. How should substance use problems be handled? Popular views in Sweden, Finland, and Canada. Drugs Alcohol Today 2014;14:19–30.
- Camus J, Sastre MTM, Sorum PC, Mullet E. French people’s positions regarding national policies about illicit drugs: a preliminary study. Soc Indic Res 2014;118:1191–1204.
- Caudy MS, Tang L, Wooditch A, Taxman FS. Short-term trajectories of substance use in a sample of drug-involved probationers. J Subst Abuse Treat 2014;46:202–213.
- Coullaut-Valera R, Arbaiza I, Bajo R, Arrúe R, López ME, Coullaut-Valera J, et al. Drug polyconsumption is associated with increased synchronization of brain electrical-activity at rest and in a counting task. Int J Neural Syst 2014;24:1450005.
- Donohue B, Azrin NH, Bradshaw K, Van Hasselt VB, Cross CL, Urgelles J, et al. A controlled evaluation of family behavior therapy in concurrent child neglect and drug abuse. J Consult Clin Psychol 2014;82:706–720.
- Faggiano F, Minozzi S, Versino E, Buscemi D. Universal school-based prevention for illicit drug use. Cochrane Database Syst Rev 2014;CD003020.
- Feingold A, Capaldi DM. Associations of women’s substance dependency symptoms with intimate partner violence. Partn Abuse 2014;5:152–167.
- Gallupe O, Baron SW. Morality, self-control, deterrence, and drug use: street youths and situational action theory. Crime Delinquency 2014;60:284–305.
- Gorman DM. Is Project Towards No Drug Abuse (Project TND) an evidence-based drug and violence prevention program? A review and reappraisal of the evaluation studies. J Prim Prev 2014;35:217–232.
- Hanson KL, Thayer RE, Tapert SF. Adolescent marijuana users have elevated risk-taking on the balloon analog risk task. J Psychopharmacol (Oxford) 2014;28:1080–1087.
- Havinga P, van der Velden C, de Gee A, van der Poel A. Differences in sociodemographic, drug use and health characteristics between never, former and current injecting, problematic hard-drug users in the Netherlands. Harm Reduct J 2014;11:6.
- Kelly E, Rasul I. Policing cannabis and drug related hospital admissions: evidence from administrative records. J Public Econ 2014;112:89–114.
- Kepper A, van den Eijnden R, Monshouwer K, Vollebergh W. Understanding the elevated risk of substance use by adolescents in special education and residential youth care: the role of individual, family and peer factors. Eur Child Adolesc Psychiatry 2014;23:461–472.
- Klimstra TA, Luyckx K, Hale Iii WW, Goossens L. Personality and externalizing behavior in the transition to young adulthood: the additive value of personality facets. Soc Psychiatry Psychiatr Epidemiol 2014;49:1319–1333.
- McNaughton Reyes HL, Foshee VA, Bauer DJ, Ennett ST. Proximal and time-varying effects of cigarette, alcohol, marijuana and other hard drug use on adolescent dating aggression. J Adolesc 2014;37:281–289.
- Mönckeberg BF. Pros and cons of legalizing marijuana. Rev Chil Pediatría 2014;85:229–237.
- Nau JY. Cannabis should no longer be considered as a soft drug (1). Rev Med Suisse 2014;10:770–771.
- Omura JD, Wood E, Nguyen P, Kerr T, DeBeck K. Incarceration among street-involved youth in a Canadian study: implications for health and policy interventions. Int J Drug Policy 2014;25:291–296.
- Palamar JJ. Predictors of disapproval toward “hard drug” use among high school seniors in the US. Prev Sci 2014;15:725–735.
- Rhoades H, Winetrobe H, Rice E. Prescription drug misuse among homeless youth. Drug Alcohol Depend 2014;138:229–233.
- Robins P. Narcotic drugs in Dubai: lurking in the shadows. Br J Middle East Stud 2014;41:151–166.
- Safren SA, Biello KB, Smeaton L, Mimiaga MJ, Walawander A, Lama JR, et al. Psychosocial predictors of non-adherence and treatment failure in a large scale multi-national trial of antiretroviral therapy for HIV: data from the ACTG A5175/PEARLS trial. PloS One 2014;9:e104178.
- Sekoni AO, Ayoola OO, Somefun EO. Experiences of social oppression among men who have sex with men in a cosmopolitan city in Nigeria. HIVAIDS (Auckland) 2014;7:21–27.
- Xian H, Giddens JL, Scherrer JF, Eisen SA, Potenza MN. Environmental factors selectively impact co-occurrence of problem/pathological gambling with specific drug-use disorders in male twins. Addiction (Abingdon) 2014;109:635–644.
- Allem J-P, Soto D, Baezconde-Garbanati L, Unger J. The relationship between the accumulated number of role transitions and hard drug use among Hispanic emerging adults. J Psychoactive Drugs 2015;47:60–64.
- Amesty S, Crawford ND, Nandi V, Perez-Figueroa R, Rivera A, Sutton M, et al. Evaluation of pharmacy-based HIV testing in a high-risk New York city community. AIDS Patient Care STDs 2015;29:437–444.
- Arnold EM, Desmond KA, Rotheram-Borus MJ, Scheffler A, Comulada WS, Johnson MO, et al. Drug use and emotional distress differentiate unstably-versus stably-housed adults living with HIV who engage in unprotected sex. J Health Psychol 2015; doi:10.1177/1359105315603465.
- Arpawong TE, Sussman S, Milam JE, Unger JB, Land H, Sun P, et al. Post-traumatic growth, stressful life events, and relationships with substance use behaviors among alternative high school students: a prospective study. Psychol Health 2015;30:475–494.
- Baggio S, Henchoz Y, Studer J, Deline S, N’goran A, Mohler-Kuo M, et al. Cannabis use and other illicit drug use: Do subjective experiences during first cannabis use increase the probability of using illicit drug? J Subst Use 2015;20:234–238.
- Bauermeister JA, Eaton L, Meanley S, Pingel ES. Transactional sex with regular and casual partners among young men who have sex with men in the Detroit metro area. Am J Mens Health 2015; doi:10.1177/1557988315609110.
- Carmona J, Slesnick N, Guo X, Murnan A, Brakenhoff B. Predictors of outreach meetings among substance using homeless youth. Community Ment Health J 2015; doi: 10.1007/s10597-015-9919-8
- Dean DO, Cole V, Bauer DJ. Delineating prototypical patterns of substance use initiations over time. Addiction (Abingdon) 2015;110:585–594.
- Deza M. Is there a stepping stone effect in drug use? Separating state dependence from unobserved heterogeneity within and between illicit drugs. J Econom 2015;184:193–207.
- Deza M. The effects of alcohol on the consumption of hard drugs: regression discontinuity evidence from the National Longitudinal Study of Youth, 1997. Health Econ 2015;24:419–438.
- Grundetjern H. Women’s gender performances and cultural heterogeneity in the illegal drug economy. Criminology 2015;53:253–279.
- Hanssens L, Felgueroso F. Management of tobacco smoking in general practice. Rev Médicale Brux 2015;36:95–100.
- Hjorthøj C, Østergaard MLD, Benros ME, Toftdahl NG, Erlangsen A, Andersen JT, et al. Association between alcohol and substance use disorders and all-cause and cause-specific mortality in schizophrenia, bipolar disorder, and unipolar depression: a nationwide, prospective, register-based study. Lancet Psychiatry 2015;2:801–808.
- Chu Y-WL. Do medical marijuana laws increase hard-drug use? J Law Econ 2015;58:481–517.
- Iranpour A, Jamshidi E, Nakhaee N, Haghdoost AA, Shojaeizadeh D, Eftekhar-Ardabili M, et al. Development and psychometric properties of risk and protective factors of substance use scale in Iran: an application of social development model. Addict Health 2015;7:117–129.
- Kosty DB, Farmer RF, Seeley JR, Gau JM, Duncan SC, Lewinsohn PM. Parental transmission of risk for cannabis use disorders to offspring. Addiction (Abingdon) 2015;110:1110–1117.
- Matejovičová B, Trandžík J, Schlarmannová J, Boledovičová M, Velemínský M. Illegal drug use among female university students in Slovakia. Med Sci Monit 2015;21:254–261.
- Mimiaga MJ, Biello KB, Robertson AM, Oldenburg CE, Rosenberger JG, O’Cleirigh C, et al. High prevalence of multiple syndemic conditions associated with sexual risk behavior and HIV infection among a large sample of Spanish- and Portuguese-speaking men who have sex with men in Latin America. Arch Sex Behav 2015;44:1869–1878.
- Razali MM, Kliewer W. Risk and protective factors for recreational and hard drug use among Malaysian adolescents and young adults. Addict Behav 2015;50:149–156.
- Schaefer BP, Vito AG, Marcum CD, Higgins GE, Ricketts ML. Examining adolescent cocaine use with social learning and self-control theories. Deviant Behav 2015;36:823–833.
- Schijven EP, Engels RCME, Kleinjan M, Poelen EAP. Evaluating a selective prevention program for substance use and comorbid behavioral problems in adolescents with mild to borderline intellectual disabilities: study protocol of a randomized controlled trial. BMC Psychiatry 2015;15:167.
- Spapens T, Müller T, van de B. The Dutch Drug Policy from a regulatory perspective. Eur J Crim Policy Res 2015;21:191–205.
- Tanidir C, Ciftci AD, Doksat NG, Gunes H, Toz HI, Erdogan A. Trends and gender differences in substance use among children and youths admitted to an addiction treatment center in Turkey: years 2011-2013. Klin Psikofarmakol Bul 2015;25:109–117.
- White HR, Buckman J, Pardini D, Loeber R. The Association of Alcohol and Drug Use with persistence of violent offending in young adulthood. J Dev Life Course Criminol 2015;1:289–303.
- Mallard TT, Doorley J, Esposito-Smythers CL, McGeary JE. Dopamine D4 receptor VNTR polymorphism associated with greater risk for substance abuse among adolescents with disruptive behavior disorders: preliminary results. Am J Addict 2016;25:56–61.
- Meier MH, Hall W, Caspi A, Belsky DW, Cerda M, Harrington HL, et al. Which adolescents develop persistent substance dependence in adulthood? Using population-representative longitudinal data to inform universal risk assessment. Psychol Med 2016;46:877–889.
- Unger JB, Soto DW, Baezconde-Garbanati L. Trajectories of perceived discrimination from adolescence to emerging adulthood and substance use among Hispanic youth in Los Angeles. Addict Behav 2016;53:108–112.
- Fulgoni VL, Keast DR, Lieberman HR. Trends in intake and sources of caffeine in the diets of US adults: 2001-2010. Am J Clin Nutr 2015;101:1081–1087.
- Nutt DJ, King LA, Phillips LD, Independent Scientific Committee on Drugs. Drug harms in the UK: a multicriteria decision analysis. Lancet 2010;376:1558–1565.
- Taberner PV. The GABA system in functional tolerance and dependence following barbiturates, benzodiazepines or ethanol – correlation or causality? Comp Biochem Physiol A 1989;93:241–245.
- Calixto E. GABA withdrawal syndrome: GABAA receptor, synapse, neurobiological implications and analogies with other abstinences. Neuroscience 2016;313:57–72.
- Segeda V, Turček M, Hamráková L, Pečeňák J. Anxiolytics and hypnotics addiction. Part 2 – comparative clinical study. Alkoholizmus a Drogové Závislosti 2015;50:149–158.
- Gill TM, Feinstein AR. A critical appraisal of the quality of quality-of-life measurements. JAMA 1994;272:619–626.