ABSTRACT
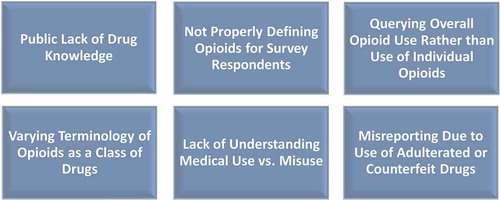
Surveys are the leading method of gathering data on prevalence and correlates of prescription opioid misuse. As the opioid crisis continues in the United States, reliable data on misuse have become increasingly important as under- and overreporting is common. This perspective discusses six potential barriers to researchers accurately assessing opioid misuse on surveys. These barriers include lack of respondent drug knowledge, researchers not properly defining opioids for respondents, querying overall opioid misuse rather than misuse of specific opioids, varying terminology (e.g., of opioids and misuse), and lack of understanding of medical versus nonmedical use or misuse. Finally, a recent barrier is use of counterfeit or adulterated drugs that contain fentanyl, its analogs, or other new synthetic opioids, which can lead to underreporting of exposure. Survey researchers should consider such barriers when querying opioid misuse.
Introduction
The United States (US) is experiencing an opioid crisis with rates of prescription opioid use disorder and opioid-involved overdose deaths continuing to rise (Citation1,Citation2). While data on adverse outcomes related to opioid use such as hospitalizations and deaths are highly informative, surveys are the leading method to gather data on prevalence and correlates of misuse of prescription opioids. As survey data on opioid misuse have become increasingly important to help inform prevention during this crisis, it is essential for researchers to collect reliable data about misuse. Underreporting in particular is problematic as underestimates of misuse may lead to less adequate public health response.
Self-report of drug use on surveys in general is subject to many limitations (Citation3,Citation4), but opioid misuse in particular can be difficult for survey researchers to query, and difficult for survey respondents to comprehend. This perspective discusses six potential barriers to researchers (listed in ) accurately assessing what is commonly referred to as prescription opioid misuse. While some of these barriers discussed also apply to various other classes of drugs, some barriers are more unique to the querying of opioid misuse—on surveys and also on patient screenings.
Lack of drug knowledge
In light of the current opioid crisis, much of the public is now familiar with the term “opioids,” but it is unknown to what extent individuals are able to classify various drugs into this category. For example, an individual may not be aware that Vicodin® is an opioid medication and thus denies his or her misuse on a survey. A recent study focusing on a nationally representative sample of high school seniors found that over a third (37%) of those reporting Vicodin® misuse and over a quarter (28%) of those reporting OxyContin® misuse denied any opioid misuse earlier during the survey (Citation5). This may suggest, in part, that many individuals are unaware that Vicodin® and OxyContin® are opioid drugs.
Lack of drug knowledge can also lead to confusion between drugs. For example, an individual may have misused oxycodone but report use of OxyContin® (a time-released version of oxycodone, often in larger doses) on a survey instead due to confusion as both terms begin with “oxy” (Citation6). Likewise, confusion between Tylenol #3®, which contains codeine, and over-the-counter (OTC) Tylenol can occur, so in order to prevent overreporting of codeine misuse, some surveys note that regular drugstore Tylenol does not contain opioids (Citation7). Misreporting can also occur when street names apply to more than one class of drugs; for example, despite dissimilar effects, methadone may be confused with methamphetamine because both drugs are commonly referred to as “meth.” Thus, in some surveys, it may be important to insert a note next to the drug of concern; for example, “methadone (not to be confused with methamphetamine).” Such notes appear to be useful on surveys that query drugs with similar names. A recent survey, for example, added a short note after 2-MeO-ketamine saying “not regular ketamine which we asked about earlier” (Citation8).
To limit confusion resulting from potential lack of knowledge about opioids, researchers administering surveys can provide respondents with additional information in order to assist them in answering opioid-related questions. For example, individuals surveyed in the National Survey on Drug Use and Health (NSDUH) are shown labeled color images of dozens of opioid pills to help inform their responses (Citation9) and this may increase sensitivity of measurement (Citation10). While showing images of drugs is not feasible in many surveys, providing any information to further educate the respondent about opioids may decrease under- or overreporting.
Not properly defining opioids for survey respondents
Unlike many other drugs or drug classes, opioids are a class of drugs which may require a definition along with examples when use is being queried on a survey. An individual may know that hash is a form of cannabis or that crack is a form of cocaine, but opioids is a drug class containing a wide variety of prescription drugs with various generic and trade names and with numerous illicitly manufactured compounds that may be less familiar to individuals. The opioids class contains prescription opioids, heroin, and synthetic opioids, although heroin and prescription opioids are commonly discussed or queried as separate drugs (Citation11,Citation12). In recent years, however, with proliferation of novel illicitly manufactured synthetic opioids, we now often refer to all compounds in this class as opioids as a whole rather than distinguishing between types of opioids.
Shifting terminology has made it more difficult to query opioid misuse on surveys and more difficult for respondents to understand if not adequately defined. Some surveys simply query opioid misuse without defining opioids or providing examples of opioids. This appears to be more common on health surveys when illegal drug use is only a part of the survey and opioids is a single check-off category included in a list of other prevalent drugs. For example, the Population Assessment of Tobacco and Health (PATH) Study, a longitudinal cohort study focusing primarily on tobacco use, does not define or provide examples for prescription “painkillers” (Citation13). Further, the PATH study queries “painkillers,” sedatives, and tranquilizers in the same question which even further muddies estimates of misuse. Similarly, through 2015, the Youth Risk Behavior Surveillance System queried prescription drug misuse via a single item querying misuse of drugs such as OxyContin®, Percocet®, Vicodin®, codeine, Adderall®, Ritalin®, and Xanax® (Citation14). This potentially confused some respondents and/or led to underreporting and this also prevents analysts from computing estimates of opioid misuse. Collapsing opioids with other drugs should be avoided and definitions and/or examples of opioids should be provided, even when queried along with a list of other drugs. If formatting does not allow for a definition or examples to fit when including opioids in a list of drugs on a survey, researchers can consider including prescription drugs on a separate list or page and define the drug class (and define misuse) above the opioid-specific questions.
While some survey formats may allow for a list of opioids to accompany the definition, most major surveys include only a handful of some of the most common or recognizable opioid products. For example, the Monitoring the Future (MTF) national survey includes morphine, codeine, methadone, opium, Demerol®, Vicodin®, Percocet®, and OxyContin® as examples along with its current definition of opioids for survey respondents (Citation15). The Alcohol, Smoking and Substance Involvement Screening Test, a screening tool developed by the World Health Organization, lists heroin, morphine, methadone, buprenorphine, and codeine as examples of opioids for patients (Citation16). While listing examples of opioid drugs may remind the respondent about previous misuse, a possible risk is that the respondent may not consider drugs not listed and thus underreport use.
Depending on the population being surveyed, “street” names or slang names can also be helpful for respondents when defining opioids and/or listing specific opioids as examples. Vicodin® pills, for example, are known as “vikes” to many users (Citation17) and “roxy” is a street name for Roxicodone®, and these pills are also commonly referred to as “blues” (Citation18) which describes the color of the pill. A respondent may deny his or her use of specific opioid drugs if he or she is unfamiliar with the generic or trade name on the survey. The “street” name “oxy” can refer to oxycodone or OxyContin®, which can lead to inaccurate responses when asked about specific opioids, and a respondent may be unaware that Roxicodone® is a brand of oxycodone. A respondent may also not think of their use of opioid-containing concoctions when answering about opioid use. For example, “Sizzurp,” also known as “Lean” or “Purple drank,” is typically a mixture of codeine cough syrup and candy in a soft drink such as Sprite (Citation19). Some users of this concoction may underreport codeine misuse—assuming they are aware that the cough syrup in this drink often contains codeine. Most surveys that query opioid misuse do not include “Sizzurp” as an example (Citation6), so it is likely that codeine syrup misuse is being underreported.
Querying overall opioid use rather than use of individual opioids
Related to the barrier of not properly defining opioids as discussed above, querying overall nonmedical opioid use via a single question can lead to both under- and overreporting of use. Asking about opioid misuse as a general category can lead some respondents to deny misuse because they were unaware that a specific opioid they misused is classified as an opioid (especially if that opioid is not provided on a list of example drugs). Or, the respondent may simply not recall opioid misuse if the drug used was not specifically asked about or listed as an example. For example, if the list of example opioids only contains Percocet®, Vicodin®, and OxyContin®, the respondent may not be reminded about his or her misuse of codeine and therefore deny opioid misuse. Although, it should be noted that if a respondent reports misuse of one or more opioids and underreports use of one opioid, overall estimates of opioid misuse would likely not be affected. When possible, a more extensive list should be provided, particularly when using a single-item opioid assessment. Research indicates that querying many individual opioid drugs appears to increase sensitivity (Citation10) and is thus likely superior to querying use via a single item. If a checklist of specific opioid drugs is provided, affirmative responses can later be coded into an overall opioid misuse variable with more accurate data.
Relatedly, electronic survey methods such as skip-logic and gate questions are commonly used as they save survey respondents time and also lead to relatively clean data, but this can lead to unintentional underreporting. For example, a survey may provide a gate question asking if any opioid was ever misused, and if a respondent checks “no,” then he or she is not provided with a follow-up checklist of specific opioids. Such skip-logic and gate questions can lead to underreporting because a respondent may (unintentionally) deny misuse on the gate question and then lose the opportunity to report misuse on the follow-up page containing the full list of drugs (Citation8,Citation20,Citation21). While such programming typically does not allow conflicting responses, discordant responses (e.g., reporting Vicodin® misuse after denying opioid misuse) on paper-administered surveys have been found to be prevalent (Citation5). More research is needed to determine whether such conflicting responses are indeed instances of overreporting, but it appears that providing a list of specific drugs that is not dependent on a gate question may be more accurate in detecting prevalence of use (Citation8,Citation20,Citation21).
It should be noted that when lists of opioids are provided, it may be helpful to include options such as “opioid not listed” or “other prescription pain reliever,” especially as novel opioids continue to emerge (Citation22,Citation23). However, it is important for such an option to include a text box which allows the respondent to type in name of the drug not listed, as is done for some drug classes in the NSDUH (Citation24,Citation25). This not only allows researchers to become aware of newer opioids used by respondents but it also provides respondents an opportunity to type in drug names that were unnoticed on the list. Likewise, it provides respondents with an opportunity to type in “street” names when the generic or trade name is not known. In these cases, the researchers can consider whether a response typed in is in fact an opioid and should be coded as one.
Varying terminology of opioids as a class of drugs
Opioids are commonly referred to as painkillers, pain-relievers, narcotics, opiates, and analgesics. While “opioid” now appears to be the most common term used by the media in the US, an individual familiar with the term may become confused when asked about different terms such as prescription painkillers or narcotics. Painkillers, if not properly defined, can imply inclusion of OTC pain-relievers, or prescription nonsteroidal anti-inflammatory drugs, muscle relaxants, anticonvulsants, antidepressants, or other pain medications. The term “narcotics” is now less prevalent on surveys, but MTF, for example, still asks about “narcotics other than heroin” when asking about opioid misuse (Citation15). The term “narcotics” can lead to confusion among survey respondents as while opioids are in fact narcotics, the Controlled Substances Act in the US also includes cocaine and other potentially psychoactive derivatives as narcotics (Citation26).
Terminology also varies between surveys regarding opioid misuse. Opioid misuse may refer to opioids in general or it may refer only to prescription opioids—also commonly referred to as nonmedical use of prescription opioids in the literature (Citation27,Citation28), as it excludes drugs such as heroin which are not prescribed. It is important to be specific regarding whether a definition of opioids includes non-prescribed opioids such as heroin. Other terminology used when describing misuse includes nonmedical use, extramedical use, illicit or illegal use, or even abuse (Citation29–Citation31). All of these terms refer to use outside of prescribed purposes in one way or another, but definitions are typically inconsistent between studies. Consistency in terminology across surveys would be ideal (Citation31), but it is not always possible. Regardless, these terms can be confusing for researchers and survey respondents alike, so when possible, terms need to be clearly defined for respondents and also for readers in publications presenting findings.
Understanding medical use versus misuse
When querying prescription opioid misuse, the researcher must clearly define misuse for the respondent. Opioid misuse (or nonmedical use) is operationalized in different ways on different surveys. Some national surveys define misuse or nonmedical use simply as use without one’s doctor telling them to take it (Citation15) or using a prescription drug without a prescription (Citation14). Through 2014, the NSDUH queried nonmedical use which it defined as when a prescription opioid was used when not prescribed to the user or used for the experience or feeling caused by the drug (Citation32). However, as of 2015, the NSDUH now instead asks assesses “misuse,” which is a more accurate term as it is defined as use not directed by a doctor, including use without a prescription, use of greater amounts, more often, or longer than directed, or use in any other way that was not directed by a doctor (Citation32).
Misuse or nonmedical use can indeed be a confusing concept as it is possible for individuals to use as prescribed and still enjoy the feeling resulting from use. Overuse and use past the prescribed window period can also lead to possible confusion—especially when use for medical reasons (related or not related to the original prescribed purpose) overlaps with the definition of misuse. A survey of middle and high school students found that “medical misuse” is common with many individuals using opioids as other (or later) forms of self-medication (Citation33). Nearly a fifth (18%) of those using their prescribed opioids reported using for nonmedical reasons. However, of these, 88% reportedly used nonmedically to treat pain, 8% reportedly used to help sleep, and 8% to decrease anxiety. Less than a fifth (14%) reported using opioids to get high. A more recent study of 2015 NSDUH data estimated that two-thirds (66%) of adults who had misused prescription opioids in the past year used mainly to relieve physical pain, and nearly half (49%) of adults with opioid use disorder also used mainly to alleviate pain (Citation34). Only about 1 in 10 (11%) misusers is estimated to use to get high as their main motivation for use. Nonmedical use, thus, often includes use for self-medication rather than to get high. So, interpretation should be cautious as misuse or nonmedical use often simply suggests use that is not specifically medically sanctioned, yet not necessarily used to get high.
To limit misinterpretation, it has been argued that motives for nonmedical use should be queried in order to prevent researchers from collapsing those reporting use to treat pain relief outside of prescribed purposes with those who use to get high (Citation29). In addition, opioid misuse is likely overreported in general among respondents who simply do not read the researcher’s definition for misuse. Thus, researchers must try their hardest to not only include these important definitions in their surveys but also to utilize methods that increase the likelihood of respondents paying attention to the definition. Underlining, italicizing, or bolding keywords in definitions are recommended to gauge respondents’ attention (Citation35), but research is needed to determine whether this is effective. Further, on electronic surveys that use skip-logic, it may be helpful to provide a full page or section, stressing the definition before the questions appear.
Adulterated and counterfeit opioid drugs
Adding to the severity of the increasing opioid crisis in the US, in 2016, synthetic opioids such as illicitly manufactured fentanyl were detected in nearly half (46%) of opioid-related deaths (Citation36). However, a major limitation to hospitalization, poisoning, and mortality data is that the extent of unknown or unintentional fentanyl exposure is unknown due to self-report without toxicological confirmation and toxicological testing not accompanied with self-report. Illicitly manufactured fentanyl, its analogs, and other novel synthetic opioids are now being detected as adulterants in a variety of drugs in the US. Fentanyl is now a common adulterant in heroin (Citation37,Citation38), and fentanyl, its analogs, and new synthetic opioids (e.g., U-47700) are also now being detected in non-opioid drugs such as cocaine, and they are now being pressed into counterfeit Xanax®, Percocet®, and hydrocodone pills (Citation39–Citation45). Pills purchased outside of pharmacies illegally can contain such adulterants if illicitly manufactured. Using an opioid such as fentanyl unintentionally is particularly dangerous to opioid-naïve drug users (Citation44). However, little data exist on intentional and unintentional use of illicitly manufactured fentanyl, which severely limits our knowledge about the extent of the opioid crisis.
Correctly reporting the opioid(s) used in the case of hospitalization or calls to Poison Control are important to inform prevention, but users are not always aware which drug was actually used. Use of adulterated or counterfeit drugs can thus lead to underreporting of more dangerous drugs. While it is difficult to determine the contents of drugs illegally purchased, test strips are now available that can detect fentanyl and many of its analogs in pills and powders (Citation46). Test strips can also be used to detect fentanyl and/or its analogs in urine if an individual feels he or she has been exposed (Citation47). This information can lead to more accurate reporting on surveys. However, it should be noted that surveys asking about use of fentanyl, its analogs, and/or other new synthetic opioids should assess whether exposure was intentional or unintentional (e.g., used as an adulterant).
Conclusion
There are many barriers to researchers accurately assessing opioid misuse on surveys. As the opioid crisis continues in the US, it has become important to accurately assess prescription opioid misuse in order to estimate prevalence and correlates of use to better inform prevention. While the potential barriers to accurately assessing opioid misuse discussed in this perspective are by no means exhaustive, survey researchers should consider such barriers when querying opioid misuse. However, addressing these barriers will typically lengthen surveys and take up more of the respondent’s time which can increase the likelihood of satisficing or respondent burnout (Citation48). Even in the age of electronic surveys, it may be difficult to add a full section focusing on opioids which includes full definitions of misuse and an extensive list of opioid drugs. This can be especially problematic for researchers focusing on other topics who wish to include one or more opioid misuse questions. Recommended methods for querying opioid misuse can more easily be incorporated into drug surveys.
Ultimately, researchers must consider the trade-offs between simple and concise survey questions and obtaining more accurate data. Obtaining more accurate data might take an extra minute (or more) of the respondent’s time, so this is something that must be given serious consideration. Considering the tradeoff between topic coverage and accurate data is important, and more research is needed to determine how much estimates of opioid misuse differ according to various survey methods. Paper and pencil surveys are particularly limited. However, electronic surveys can be programmed to utilize skip-logic, so follow-up questions are only administered to those who report any opioid misuse via a gate question. Labeled drug images can also easily be inserted into electronic surveys, but again, this is dependent on how much time and space researchers would like to dedicate to opioid misuse. Researchers also commonly collapse all prescription opioids into a single category for simplicity, so oftentimes the detail regarding which specific prescription opioids were misused may not be of specific interest to the researcher or to the public. But under- and overreporting associated with single-item opioid misuse questions should still be considered. Lastly, the public requires better drug education. While it is inconvenient to include definitions and lists of opioid drugs in a survey, it can also be viewed as an opportunity to educate respondents.
Declaration of Interest
The author declares no conflict of interest.
Additional information
Funding
References
- Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–52. doi:10.15585/mmwr.mm655051e1
- Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468–78. doi:10.1001/jama.2015.11859
- Harrison L. The validity of self-reported drug use in survey research: an overview and critique of research methods. NIDA Res Monogr. 1997;167:17–36.
- Johnson T, Fendrich M. Modeling sources of self-report bias in a survey of drug use epidemiology. Ann Epidemiol. 2005;15(5):381–89. doi:10.1016/j.annepidem.2004.09.004
- Palamar JJ, Shearston JA, Cleland CM. Discordant reporting of nonmedical opioid use in a nationally representative sample of US high school seniors. Am J Drug Alcohol Abuse. 2016;42(5):530–38. doi:10.1080/00952990.2016.1178269
- Palamar JJ, Le A, Cleland CM. Nonmedical opioid use among electronic dance music party attendees in New York City. Drug Alcohol Depend. 2018;186:226–32. doi:10.1016/j.drugalcdep.2018.03.001
- Fischer B, Ialomiteanu A, Boak A, Adlaf E, Rehm J, Mann RE. Prevalence and key covariates of non-medical prescription opioid use among the general secondary student and adult populations in Ontario, Canada. Drug Alcohol Rev. 2013;32(3):276–87. doi:10.1111/dar.12025
- Palamar JJ, Acosta P, Calderon FF, Sherman S, Cleland CM. Assessing self-reported use of new psychoactive substances: the impact of gate questions. Am J Drug Alcohol Abuse. 2017;43(5):609–17. doi:10.1080/00952990.2017.1322094
- Center for Behavioral Health Statistics and Quality. national survey on drug use and health: methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [accessed 2018 Jul 28]. https://www.samhsa.gov/data/sites/default/files/NSDUH-MethodSummDefs-2016/NSDUH-MethodSummDefs-2016.htm
- Biondo G, Chilcoat HD. Discrepancies in prevalence estimates in two national surveys for nonmedical use of a specific opioid product versus any prescription pain reliever. Drug Alcohol Depend. 2014;134:396–400. doi:10.1016/j.drugalcdep.2013.10.005
- Ruhm CJ. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am J Prev Med. 2017;53(6):745–53. doi:10.1016/j.amepre.2017.06.009
- Palamar JJ, Shearston JA, Dawson EW, Mateu-Gelabert P, Ompad DC. Nonmedical opioid use and heroin use in a nationally representative sample of us high school seniors. Drug Alcohol Depend. 2016;158:132–38. doi:10.1016/j.drugalcdep.2015.11.005
- Department of Health and Human Services, National Institutes of Health. National Institute on Drug Abuse, United States Department of Health and Human Services, Food and Drug Administration. Center for tobacco products codebook for wave 1: adult questionnaire data with weights. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2018. [accessed 2018 Jul 28]. https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/36231/datadocumentation#
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Hawkins J, Queen B, et al. Youth risk behavior surveillance - United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. doi:10.15585/mmwr.ss6506a1
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the future national survey results on drug use, 1975-2016: volume I, secondary school students. Ann Arbor: Institute for Social Research, The University of Michigan; 2017. [accessed 2018 Jul 28]. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2016.pdf
- Humeniuk RE, Henry-Edwards S, Ali RL, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): manual for use in primary care. Geneva: World Health Organization; 2010. [accessed 2018 Jul 28]. http://www.who.int/substance_abuse/publications/assist/en/
- Chan B, Lopez A, Sarkar U. The canary in the coal mine tweets: social media reveals public perceptions of non-medical use of opioids. PLoS One. 2015;10(8):e0135072. doi:10.1371/journal.pone.0135072
- Harocopos A, Allen B, Paone D. Circumstances and contexts of heroin initiation following non-medical opioid analgesic use in New York City. Int J Drug Policy. 2016;28:106–12. doi:10.1016/j.drugpo.2015.12.021
- Agnich LE, Stogner JM, Miller BL, Marcum CD. Purple drank prevalence and characteristics of misusers of codeine cough syrup mixtures. Addict Behav. 2013;38(9):2445–49. doi:10.1016/j.addbeh.2013.03.020
- Lessler JT, Caspar RA, Penne MA, Barker PR. Developing computer assisted interviewing (CAI) for the national household survey on drug abuse. J Drug Issues. 2000;30(1):9–33. doi:10.1177/002204260003000102
- Gfroerer J, Lessler J, Parsley T. Studies of nonresponse and measurement error in the national households survey on drug abuse. In: Harrison L, Hughes A, (editors.). The validity of self-reported drug use: improving the accuracy of survey estimates: NIDA research monograph. Rockville, MD: U.S. Department of Health and Human Services, National Institute on Drug Abuse, Division of Epidemiology and Prevention Research, 1997: 273–95
- European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2017. Lisbon. [accessed 2018 Jul 28]. http://www.emcdda.europa.eu/edr2017
- U.S. Drug Enforcement Administration. 2017 Emerging Threat Report.[accessed 2018 Jul 28]. https://ndews.umd.edu/sites/ndews.umd.edu/files/dea-emerging-threat-report-2017-annual.pdf
- Palamar JJ, Martins SS, Su MK, Ompad DC. Self-reported use of novel psychoactive substances in a us nationally representative survey: prevalence, correlates, and a call for new survey methods to prevent underreporting. Drug Alcohol Depend. 2015;156:112–19. doi:10.1016/j.drugalcdep.2015.08.028
- Han B, Compton WM, Blanco C, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. Adults Ann Intern Med. 2018;168(5):383–84. doi:10.7326/M17-0865
- Drug Enforcement Administration, Office of Diversion Control. 1970. Title 21 United States Code (USC) controlled substances act [accessed 2018 Jul 28]. https://www.deadiversion.usdoj.gov/21cfr/21usc/802.htm
- Martins SS, Santaella-Tenorio J, Marshall BD, Maldonado A, Cerda M. Racial/ethnic differences in trends in heroin use and heroin-related risk behaviors among nonmedical prescription opioid users. Drug Alcohol Depend. 2015;151:278–83. doi:10.1016/j.drugalcdep.2015.03.020
- McCabe SE, Schulenberg JE, O’Malley PM, Patrick ME, Kloska DD. Non-medical use of prescription opioids during the transition to adulthood: a multi-cohort national longitudinal study. Addiction. 2014;109(1):102–10. doi:10.1111/add.12347
- Zacny JP, Lichtor SA. Nonmedical use of prescription opioids: motive and ubiquity issues. J Pain. 2008;9(6):473–86. doi:10.1016/j.jpain.2007.12.00
- Cochran G, Woo B, Lo-Ciganic WH, Gordon AJ, Donohue JM, Gellad WF. Defining nonmedical use of prescription opioids within health care claims: a systematic review. Subst Abus. 2015;36(2):192–202. doi:10.1080/08897077.2014.993491
- Larance B, Degenhardt L, Lintzeris N, Winstock A, Mattick R. Definitions related to the use of pharmaceutical opioids: extramedical use, diversion, non-adherence and aberrant medication-related behaviours. Drug Alcohol Rev. 2011;30(3):236–45. doi:10.1111/j.1465-3362.2010.00283.x
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2016 national survey on drug use and health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. [accessed 2018 Jul 28]. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.pdf
- McCabe SE, West BT, Boyd CJ. Motives for medical misuse of prescription opioids among adolescents. J Pain. 2013;14(10):1208–16. doi:10.1016/j.jpain.2013.05.004
- Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 national survey on drug use and health. Ann Intern Med. 2017;167(5):293–301. doi:10.7326/P17-9042
- Mertler CA. Introduction to educational research. Thousand Oaks, CA: Sage Publications; 2018.
- Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010-2016. JAMA. 2018;319(17):1819–21. doi:10.1001/jama.2018.2844
- Ciccarone D. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int J Drug Policy. 2017;46:107–11. doi:10.1016/j.drugpo.2017.06.010
- Ciccarone D, Ondocsin J, Mars SG. Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin’. Int J Drug Policy. 2017;46:146–55. doi:10.1016/j.drugpo.2017.06.004
- US Drug Enforcement Administration. Counterfeit prescription pills containing fentanyls: a global threat [DEA Intelligence Brief; DEA-DCT-DIB-021-16]; 2016. [accessed 2018 Jul 28]. http://www.dea.gov/docs/Counterfeit%20Prescription%20Pills.pdf
- American Association of Poison Control Centers. June 2017 deadly novel synthetic opioid exposure outbreak in Georgia –a case study in the crucial surveillance role of regional poison control centers; 2017. [accessed 2018 Jul 28]. https://aapcc.s3.amazonaws.com/pdfs/releases/June_2017_Deadly_Novel_Synthetic_Opioid_Exposure_Outbreak_in_Georgia_FINAL.pdf
- Arens AM, van Wijk XM, Vo KT, Lynch KL, Wu AH, Smollin CG. Adverse effects from counterfeit alprazolam tablets. JAMA Intern Med. 2016;176(10):1554–55. doi:10.1001/jamainternmed.2016.4306
- Jones CM, Baldwin GT, Compton WM. Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health. 2017;107(3):430–32. doi:10.2105/AJPH.2016.303627
- Pichini S, Solimini R, Berretta P, Pacifici R, Busardo FP. Acute intoxications and fatalities from illicit fentanyl and analogues: an update. Ther Drug Monit. 2017;40(1):38–51. doi:10.1097/FTD.0000000000000465
- Sutter ME, Gerona RR, Davis MT, Roche BM, Colby DK, Chenoweth JA, Adams AJ, et al. Fatal fentanyl: one pill can kill. Acad Emerg Med. 2017;24(1):106–13. doi:10.1111/acem.13034
- Armenian P, Olson A, Anaya A, Kurtz A, Ruegner R, Gerona RR. Fentanyl and a novel synthetic opioid U-47700 masquerading as street “norco” in Central California: a case report. Ann Emerg Med. 2017;69(1):87–90. doi:10.1016/j.annemergmed.2016.06.014
- Bloomberg American Health Initiative. Fentanyl overdose reduction checking analysis study. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; 2018. [accessed 2018 Jul 28]. https://idpc.net/publications/2018/02/fentanyl-overdose-reduction-checking-analysis-study
- Jones AA, Jang K, Panenka WJ, Barr AM, MacEwan GW, Thornton AE, Honer WG. Rapid change in fentanyl prevalence in a community-based, high-risk sample. JAMA Psychiatry. 2018;75(3):298–300. doi:10.1001/jamapsychiatry.2017.4432
- Tourangeau R, Rips LJ, Rasinski K. The psychology of survey response. 6th ed. New York, NY: Cambridge University Press; 2006.