Abstract
Introduction
Health professionals are expected to consistently perform to a high standard during a variety of challenging clinical situations, which can provoke stress and impair their performance. There is increasing interest in applying sport psychology training using performance mental skills (PMS) immediately before and during performance.
Methods
A systematic review of the main relevant databases was conducted with the aim to identify how PMS training (PMST) has been applied in health professions education and its outcomes.
Results
The 20 selected studies noted the potential for PMST to improve performance, especially for simulated situations. The key implementation components were a multimodal approach that targeted several PMS in combination and delivered face-to-face delivery in a group by a trainer with expertise in PMS. The average number of sessions was 5 and of 57 min duration, with structured learner guidance, an opportunity for practice of the PMS and a focus on application for transfer to another context.
Conclusion
Future PMST can be informed by the key implementation components identified in the review but further design and development research is essential to close the gap in current understanding of the effectiveness of PMST and its key implementation components, especially in real-life situations.
Introduction
Health professionals are expected to maintain a high standard of performance during a wide variety of clinical situations. Some situations are experienced by the individual as being challenging and stressful, such as when managing cases with an acutely ill patient or performing surgery on a rapidly deteriorating patient. These clinical situations have high complexity and risk that is often combined with the additional pressures of time and multiple distractions (Krage et al. Citation2014; Anton and Stefanidis Citation2016). During these types of situations, individuals have high mental and physical arousal which can enhance their performance. However, often stress is provoked with a variety of inter-related cognitive and physiological effects, especially a feeling of loss of control and increased heartbeat and muscle tension. The impact of stress on clinical performance can be potentially significant, with impaired cognitive and motor function, which often leads to worse outcomes for both procedural clinical skills, such as suturing, and higher-level functions, such as decision-making, emotional control, and effective interpersonal communication (Arora et al. Citation2010). Individuals may develop their own approach to manage their stress in challenging clinical situations, but often their chosen techniques are inconsistently implemented or ineffective (Anton and Stefanidis Citation2016).
Practice points
Training to support health professionals to ensure optimal performance in challenging and stressful situations has recently applied insights from sports psychology.
Implementing training in performance mental skills (PMS) immediately before and during performance has the potential to improve performance and several key components have been identified.
Future training in PMS can be informed by several key implementation components: a multimodal approach that targets several PMS in combination and delivered face-to-face delivery in a group by a trainer with expertise in PMS, with structured learner guidance, an opportunity for practice of the PMS and a focus on application for transfer to another context
Further research is essential to close the gap in the current understanding of the effectiveness of PMT and its key implementation components, especially in real-life situations, and also in nursing and allied health professions.
There has been increasing interest in applying sport psychology techniques for training health professionals in how to effectively manage their stress in challenging clinical situations (Anton, Bean, et al. Citation2017; Church et al. Citation2017). Athletes across multiple sports are trained to apply one or more cognitive and behavioural skills ‘in the moment’ immediately before and during performance in a challenging situation to maintain control over their stress so that they are within their individual optimal zone of mental arousal, physical arousal, and attention for maintaining optimal performance (Cotterill Citation2010; Gallucci Citation2013). For example, a gymnast who is just about to perform their routine can rapidly optimise their arousal and attention by control of negative thoughts through positive self-talk, the use of motivational-related imagery (which has a focus on visualisation of successful performance during similar situations), and physical relaxation. The effectiveness of training on the use of specific cognitive and behavioural skills for optimal performance has been demonstrated across a range of different sports (Mccann et al. Citation2001; Czech et al. Citation2004; Cotterill Citation2011; Clowes and Knowles Citation2013; Hazell et al. Citation2014; McGowan et al. Citation2015).
The term Performance Mental Skills (PMS) has been recommended in sport psychology for describing the specific cognitive and behavioural skills for maintaining optimal mental arousal, physical arousal, and attention immediately before and during a challenging situation (Vealey Citation1988). This recommendation avoids any potential confusion due to the variety of terms that appear in the literature, such as psychological skills, mental skills, and pre-performance routines. These terms are often used for describing both specific ‘in the moment’ skills and more general skills with a focus on enhancing wellbeing, such as mindfulness training, which are provided between performances. Further confusion can also occur with the use of the term ‘warm up,’ which is also a cognitive and behavioural skill that physically and mentally prepares an individual for a performance but this does not occur ‘in the moment’ (McGowan et al. Citation2015).
Health professions educators interested in the application of sport psychology for PMS training (PMST) require a detailed understanding of how to implement the training, especially the key components which are effective. Whilst a recent review of interventions for junior surgeons noted that applied sport psychology training appeared to be effective (Anton, Bean, et al. Citation2017), a subsequent review highlighted the limited description of both how the training had been implemented and its impact on clinical performance in real-life situations (Lin et al. Citation2020). Both reviews have highlighted significant gaps in the current understanding of how to implement effective PMST for health professions education (HPE). First, the focus has been limited to surgical performance rather than other equally challenging and stressful clinical situations; second, there has been little attempt to identify the key implementation components of the training that are associated with meaningful clinical outcomes.
The aim of the study was to conduct a systematic review of how PMST has been applied in HPE and its outcomes.
Methods
The review followed ‘best practice’ in performing systematic reviews (Sharma et al. Citation2015) and met the PRISMA (Preferred reporting items for systematic reviews and meta-analyses) statement criteria (Moher et al. Citation2009). The review was registered with the Faculty of Health, Social Care & Medicine at Edge Hill University. Further ethical scrutiny was not applicable for this systematic review as it did not involve primary data collection.
Identifying relevant articles
A research team of reviewers with expertise in undergraduate and postgraduate medical education (JB, HC, MP, RP, JS), sport psychology research (LJ, JR), allied health profession education (KH), and systematic reviews (MM) was established.
The review search strategy was developed by the research team, which included an experienced health information and evidence synthesis specialist (MM). The search terms were based upon a conceptual framework relating to three concepts: population (medical, nursing, midwifery, emergency medical personnel) AND intervention (PMST), AND outcomes. Search terms based on these concepts were proposed by the research team and supplemented with additional relevant terms from a set of key studies in HPE and sport psychology. The search strategy was initially developed in MEDLINE using a combination of controlled vocabulary and free-text keywords (see Supplement Appendix A: MEDLINE Search terms). A small set of key relevant articles was identified, and the initial MEDLINE search strategy was piloted to ensure it captured these studies. The final list of search terms used for each database was tailored to each database.
The search strategy included nine major databases: MEDLINE, PubMed, Web of Science (which includes CINAHL and EMBASE), PsycINFO, SPORTDiscus, ERIC (Education Resources Information Centre), and the BEI (British Education Index). Four PhD literature databases were also included: Proquest Dissertations and Theses: UK and Ireland, the British Library’s Electronic Theses Online Service (EThOS), Networked Digital Library of Theses and Dissertations (NDLTD) – Global ETD Search and Open Access Theses and Dissertations (OATD).
Included studies were limited to primary research published in English within the last 20 years (1 January 2000–11 May 2020). To be included in the review, studies had to (a) be primary research studies of PMST for one or more PMS (imagery, relaxation, self-talk, attentional control, and goal setting) used before and/or during performance; (b) target undergraduate or postgraduate medical, nursing, midwifery or emergency medical personnel education; and (c) evaluate PMST on PMS and/or clinical performance outcomes. Interventions conducted in both simulated and/or real-life clinical settings were included. Studies reporting training to achieve general psychological wellbeing and ‘warm up’ were excluded. To simplify the classification of clinical performance outcomes, the term clinical skill (CS) was used and further classified based as ‘open’ or ‘closed’ CS (Singer Citation2000; Wang et al. Citation2013). Closed skills are self-paced specific performances under stable and predictable environmental conditions, such as a golf swing or a tennis serve. Open skills are more complex, multi-task performances contextualised within more rapidly changing conditions, such as a cycling sprint in the closing stages of a race or shooting at the goal during a game of soccer. In a clinical context, examples of closed CS include suturing or venous cannulation and open CS include management of a surgical emergency during an operation or coordinating a team response to a cardio-pulmonary crisis.
The reference lists of all included articles and identified systematic reviews were hand-searched for additional eligible studies. Citations from the databases and journals were imported into Covidence (a Cochrane systematic review technology platform: Melbourne, VIC: Australia) and this platform was also used for screening and selection of studies, including removal of duplicates.
Selecting studies for review
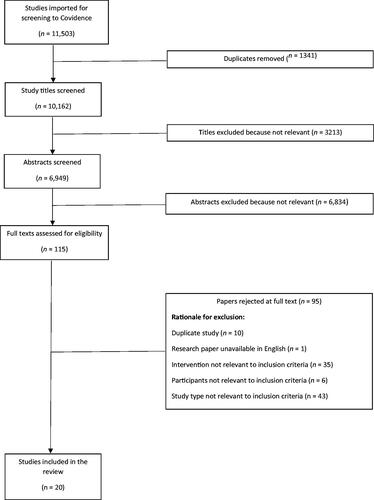
Two reviewers (LJ, JS) initially independently screened the titles and abstracts of each study according to the inclusion criteria and only definitely irrelevant studies were excluded at this stage. The full text of the remaining studies was screened by two reviewers (LJ, JS) and any disagreements were discussed with a third reviewer (JB) until a consensus agreement was reached. The PRISMA flow chart is presented in .
Data extraction
A data extraction template was jointly developed by all the research team to capture information on study design, demographics, design and delivery implementation components, PMS and CS outcomes, and the future implications and recommendations made by the authors of these studies. The design and delivery implementation components for each study were evaluated by using a combination of the Template for Intervention Description and Replication (TiDieR) tool (Hoffmann et al. Citation2014) and Gagne’s Nine Events of Instruction (Gagne et al. Citation2005). The effectiveness of each study was evaluated to identify the reported outcomes, including the significance of the effect size, on the target PMS and CS. Methodological quality of each study was assessed using the Medical Education Research Study Quality Instrument (MERSQI) tool (Reed et al. Citation2007). The ten items are aligned to six categories of study quality: study design, sampling, data type (subjective or objective), validity of assessments, data analysis, and outcomes. The possible total MERSQI scores can range from 5 to 18, allowing comparison of scores across different studies. The quality of the reporting of the training intervention for each study was assessed as high, unclear or low across five elements (U = Underpinning theory described, R = Resources described, S = Settings described, E = Educational methods described, C = Content described) (Gordon et al. Citation2020). A visual ranking system (green: high; yellow: unclear; red: low) was used to present the data as previously used by Gordon et al. (Citation2020).
One reviewer (LJ) initially charted five studies to pilot the extraction sheet, which was then was amended through discussion between the research team. The research team was separated into two groups for data extraction (Group 1: JS, HC, RP, JR; Group 2: LJ, MP, KH, JB), with a lead reviewer (JS and LJ) for each extraction group. The extraction groups were organised to ensure that each one contained a member of the research team with a sports/performance psychology background, a research background, and a clinical background. Initially the lead reviewers completed an extraction template document for each of their group’s allocated papers (group 1 was allocated 10 studies, and 10 studies for group 2). Then, the remaining extraction group members collaboratively performed the second reviewer role for their group’s allocated studies. Any disagreements or divergences in the extractions for each paper were resolved by a third reviewer or by consensus within each extraction group. At the final stage of this process, the extraction documents from both groups were crosschecked by LJ for consistency, resulting in a single master extraction document for each study.
Data synthesis and interpretation
The data from all studies was summarised and interpreted, including further synthesis of [1] key PMST implementation components and measured outcomes for studies with (a) significant combined PMS and CS outcomes (b) significant only PMS or CS outcomes (c) non-significant associated PMS and CS outcomes and [2] key PMST implementation components and measured outcomes for the studies of open and closed clinical skills (CS). This was initially conducted by the lead reviewers (JS and LJ) with subsequent discussion and consensus with all the research team in relation to the aim of the review.
Results
The review identified 20 relevant studies; six targeted open clinical skills (Wetzel et al. Citation2011; Ignacio et al. Citation2016; Lorello et al. Citation2016; Ignacio et al. Citation2017; Goldberg et al. Citation2018; Church Citation2019) and 14 targeted closed clinical skills (Immenroth et al. Citation2007; Wright et al. Citation2008; Arora et al. Citation2011; Hunziker et al. Citation2013; Maher et al. Citation2013; Anton et al. Citation2016; Anton, Howley, et al. Citation2017; Anton, Mulji, et al. 2017; Stefanidis, Anton, Howley, et al. Citation2017; Stefanidis, Anton, McRary, et al. Citation2017; Anton et al. Citation2018, Citation2019, Citation2020; Raison et al. Citation2018
The extent of PMST in HPE
As Supplement Table 1 shows, the majority of the studies were from the United States of America (n = 10) and the United Kingdom (n = 5), with 14 studies on closed CS and six studies on open CS.
Most studies were for surgical skills, especially suturing, and had medical students as participants (n = 9) or surgical doctors in training (n = 7). For open CS, there were three simulation studies conducted with junior doctors in training, with one for a surgical procedure and two for the management of an acutely ill patient. Nursing students were the only other health professions participants, with three studies; one targeting closed CS and two targeting open CS (both management of the acutely ill patient).
The key implementation components of PMST in HPE
The majority of studies used imagery (n = 19), with relaxation (n = 12), self-talk (n = 12) and goal setting (n = 8), especially in combination (n = 13). Supplement Table 2 describes the key implementation components for the selected studies.
For delivery, all PMST were face-to-face and the majority were group-based (n = 13). The mean number of sessions was 5 (range: 1–12) with a mean session duration of 57 min (range: 10–180). Most trainers had a sport psychology background (n = 7) or were an experienced clinician who had previously used PMS (n = 4). One study described a sport psychologist training a clinician to become a trainer.
For design, activation of prior knowledge through discussion of previous experiences was used in five studies and combined with an initial assessment of the use of PMS in two studies. Additional written guidance for the practice of a specific PMS was used in nine studies and this was used in combination with instructional videos in seven studies. An opportunity for practice the application of PMS to a simulated scenario was described in five studies and to a real-life situation in two studies. Only two studies stated that feedback was provided, and both were after the participants’ use of PMS in a simulated scenario. There was a general discussion about transfer of PMS to clinical situations in four studies, transfer to simulated scenarios (n = 3) and real-life situations (n = 2). One study used an individual self-reflective diary to refine PMS to real-life situations and another developed a personalised mental imagery script.
The outcomes of PMST in HPE
Consideration of study design and outcomes
Most studies were randomised controlled trials (12 studies) and the mean MERSQI scores of the studies was 13.8 (range: 11.5–16.5), suggesting overall high quality conduct of the research study. However, the reporting of the studies was often unclear or poor, especially for the content of PMST (see Supplement Table 1).
All studies measured PMS and CS as pre and immediate post-test but only three studies measured transfer outcomes at a later date: two studies on simulated outcomes (one study measured after 21 days and unclear in the other study) and one study in a real-life context but only participant perceptions were obtained. A variety of PMS outcome measures were used, including validated self-report questionnaires and physiological measures, especially heart rate (n = 12). A variety of objective CS outcome measures were used for both closed and open CS. Participant feedback on the positive perceptions of the usefulness of PMST was obtained in nine studies but there was no data collected on the barriers to PMST.
Identifying the overall outcomes of PMST in HPE
For identifying the overall outcomes of PMST, studies which demonstrate outcomes which have a logical association, such as the studies with both PMS and CS (associated PMS and CS) are of greater interest compared than studies which only measured PMS or CS. Significant positive outcomes for associated PMS and CS were identified in seven studies (Wetzel et al. Citation2011; Lorello et al. Citation2016; Stefanidis, Anton, Howley, et al. Citation2017; Stefanidis, Anton, McRary, et al. Citation2017; Anton, Mulji, et al. 2017; Anton et al. Citation2018; Raison et al. Citation2018) (see Supplement Table 3).
No data analysis to identify a direct statistical correlation or causation between significant positive associated PMS and CS outcomes had been conducted. Comparison across the studies and greater details the significance was precluded due to the heterogeneity of the use of different PMS or CS outcome measures, methods of analysis (within and/or between groups) and presentation of effect size.
The key implementation components of PMST and outcomes
To identify the key implementation components, the studies with reported significant positive outcomes for associated PMS and CS (n = 7), PMS only (n = 5) and CS only (n = 7) were considered for analysis (see Supplement Table 4).
The small number of key implementation components in each category precluded statistical analysis to identify the key implementation components that were statistically significant. However, some apparent trends were identified for the key implementation components in studies with positive outcomes (associated PMS and CS and only PMS or CS). A multimodal approach that targeted several PMS in combination (especially imagery, relaxation and self-talk) and delivered face to face in a group by a trainer with expertise in PMS appeared to be important. Structured learner guidance, an opportunity for practice of the PMS and a focus on application for transfer to another context were also important.
A comparison to identify if there were similarities or differences between the key implementation components for open and closed CS was conducted, with inclusion of open and closed studies with associated PMS and CS, PMS only and CS only outcomes (see Supplement Table 5).
The small number of key implementation components in each category, especially for open CS, precluded statistical analysis to identify the key implementation components that were statistically significant. However, some apparent trends for the key implementation components that were most associated with positive outcomes were identified. Comparison of the key implementation components and reported statistically significant positive outcomes (PMS and/or CS) for the studies of open and closed CS noted that PMST targeting closed CS were more often delivered using a multimodal approach (71% vs. 50%) and with a higher mean number of sessions (6.3 vs. 1.4). Closed CS studies were more commonly designed to activate prior knowledge (50% vs. 17%), provide opportunities for practice (71% vs. 67%), and focussed on transfer with application to another context (57% vs. 50%). No studies targeting open CS stated goal setting as a component of PMST.
Discussion
The review identified 20 studies that suggest PMST can be potentially effective for HPE with significant positive outcomes for PMS and/or CS reported in the included studies. Although PMST was a complex intervention, with multiple components implemented in several ways, some key implementation components were identified that appeared to be associated with significant positive outcomes: a multimodal approach that targeted several PMS in combination (especially imagery, relaxation and self-talk) and delivered face to face in a group by a trainer with expertise in PMS. The average number of sessions was 5 and of 57 min duration, with structured learner guidance, an opportunity for practice of the PMS and a focus on application for transfer to another context. There may also be differences for positive outcomes of PMST between open and closed CS. Delivery using a multimodal approach with a higher number of sessions that included activation of prior knowledge, provided opportunities for practice and focussed on transfer with application to another context appeared to be especially important for closed CS.
The findings of the review provide an important addition to the current understanding of PMST for HPE educators. Whilst several key implementation components have been identified, especially for closed CS, that can inform future practice, several major gaps have also been highlighted that limit future applicability of PMST interventions to other contexts (Cambon et al. Citation2012). These major gaps in understanding PMST are:
Few studies had been conducted across different clinical contexts, especially for open CS in real-life clinical situations, and also in nursing and allied health professions.
There was often a lack of detailed description of several of the key implementation components in the studies, although this may be related to journal requirements.
The contribution of specific key implementation components to positive PMS and CS outcomes was difficult to interpret due to the heterogeneity in the research design (between-groups only, within-groups only and both) and the analysis of outcomes, including no analysis of a causal relationship between PMS and CS.
Strengths and limitations of the review
A strength of the review is that it is the first review, to our knowledge, that has critically evaluated the use of sport psychology informed PMST across a range of HPE contexts. The review also extends previous research of PMST in surgical education. Another strength of the review is that it was conducted throughout (from the development of a comprehensive search strategy, data extraction and analysis, to writing up of the final paper) by a multi-disciplinary team of HPE educators from different disciplines, sport psychology researchers and a health information and an evidence synthesis specialist.
A potential limitation of the review, similar to all systematic reviews, is that the data was based on the selected studies and their analysis, which required individual judgments by the reviewers, including the classification of PMS. However, this potential limitation was reduced by adopting a systematic process and attempts were made to reduce variation in reviewers’ judgments by the use of paired-reviewers and additional reviewers who discussed any differences until consensus was reached.
Recommendations
We recommend that future implementation of PMST in HPE should be informed by our review to maximise its potential to be effective on CS. Several of the key implementation components identified in the review are closely aligned to important evidence-based implementation components for effective PMST in sport psychology and clinical skills training:
For design, it is essential to ensure that CS, both open and closed, are developed and transferred to real-life clinical practice but also that skill decay over time can be minimised. The review and the wider evidence base, that also includes sport psychology and clinical skills training, highlights the importance of guided deliberate practice, goal setting, spaced learning (short and repeated sessions), repeated assessment of skill with feedback and opportunities for practice across a wide variety of situations, both simulated and real-life (Cecilio-Fernandes et al. Citation2018; McGinn et al. Citation2018; Higgins et al. Citation2021).
For delivery, the review and sports psychology evidence-base also highlight the importance of group-based (Greenspan and Feltz Citation1989) and multimodal approaches that target several PMS in combination (Sharp et al. Citation2013), with PMST guided by a trainer with sport psychology expertise, including a focus on coaching to enable personalised adaptation of PMS to different challenging situations (Mageau and Vallerand Citation2003; Hanin and Hanina Citation2009). An essential aspect of this personalisation and adaptation of PMS for open CS, as in real-life clinical situations, is development in the use of metacognitive skills, including goal setting with self-monitoring and adaptive regulation to ensure that the effect of the chosen PMS is optimised during the evolving demands of the situation (Brick et al. Citation2015).
Further research is essential to close the gap in the current understanding of the effectiveness of PMT and the contribution of its key implementation components, especially in real-life situations and open CS, and also for nursing and allied health professions. An important aspect will be the need for greater detail in reporting future studies to ensure both increased understanding within the field but also to share best practice and applicability to other contexts (Hoffmann et al. Citation2014; Ogrinc et al. Citation2019). This is likely to require increased use of supplementary online material for journals and greater information on the factors that enable and constrain PMST.
We recommend a change in the current trend of mainly conducting randomised controlled trials to the use of design and development research that both iteratively develops and evaluates PMST. This approach to research enables understanding and optimisation of key implementation components for effective outcomes on both PMS and CS to be adapted across different clinical situations and health professions (Sandars et al. Citation2020). An essential aspect of this future research will be making explicit choices about the focus (open and/or closed CS), the key implementation components to be included in the PMST and the outcome measures of PMST, especially to identify the impact on real-life clinical performance. Most studies in the review used validated self-report questionnaires and objective outcome measures of CS but an important consideration for future research is the reliance on a variety of physiological measures, especially heart rate, as used in the selected studies. These studies often had a hypothesis that PMS would decrease physiological responses to stress, with a lowered heart rate, but the expected positive result was not obtained since the rate increased. There are concerns about the validity of these types of measures (Charles and Nixon Citation2019), especially since individuals often perform within a personalised zone of optimal arousal and this may not be reflected in their physiological response (Németh and Balogh Citation2021).
Conclusions
Training interventions for health professionals to optimise their performance during a variety of challenging and stressful clinical situations has recently applied insights from sport psychology by using a variety of PMS skills ‘in the moment’ immediately before and during performance. The review confirmed that PMST can be potentially effective on CS and also highlighted several key components which may enhance effectiveness. Importantly for HPE educators, the review noted that future PMST can be informed by several key implementation components which are aligned to evidence-based sport psychology and clinical skills training. Further research is essential to close the gap in the current understanding of the effectiveness of PMT and the contribution of its key implementation components, especially in real-life situations and open CS, and for nursing and allied health professions. Researchers are also encouraged to pay specific attention to the selection of appropriate outcome measures.
Supplemental Material
Download MS Word (17.2 KB)Supplemental Material
Download MS Word (32.6 KB)Supplemental Material
Download MS Word (24.1 KB)Supplemental Material
Download MS Word (22.4 KB)Supplemental Material
Download MS Word (25.9 KB)Supplemental Material
Download MS Word (35 KB)Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Glossary
Performance Mental Skills: Specific cognitive and behavioural skills used immediately before and during performance with the intention of enabling an individual to have the optimal mental arousal, physical arousal, and attention required to perform optimally during a challenging situation. These specific cognitive and behaviours skills have been classified into four main groups (goal setting, imagery, physical relaxation, and thought control (also known as self-talk)) and are collectively referred to as Performance Mental Skills (PMS).
Additional information
Funding
Notes on contributors
John Sandars
John Sandars, MBChB (Hons), MSc, MD, is a Professor of Medical Education in the Health Research Institute, Faculty of Health, Social Care & Medicine, Edge Hill University, Ormskirk, UK.
Liam Jenkins
Liam Jenkins, BSc, MSc, is a Research Assistant in the Health Research Institute, Faculty of Health, Social Care & Medicine, Edge Hill University, Ormskirk, UK.
Helen Church
Helen Church, MBChB, PhD, is a Clinical Assistant Professor in Medical Education at the University of Nottingham and Academic General Practice Trainee in the East Midlands Deanery.
Rakesh Patel
Rakesh Patel, MBChB, MMedEd, MD, is a Clinical Associate Professor of Medical Education, University of Nottingham, UK and honorary consultant nephrologist, Nottingham University Hospitals NHS Trust, UK.
James Rumbold
James Rumbold, BSc, MSc, PhD, C Psychol, is a Senior Lecturer in Sport and Exercise Psychology, College of Health, Wellbeing and Life Sciences, Sheffield Hallam University, UK.
Michelle Maden
Michelle Maden, MA, PhD, is an Information Specialist, Faculty of Health, Social Care & Medicine, Edge Hill University, Ormskirk, UK.
Mumtaz Patel
Mumtaz Patel, MBChB, MMedEd, MD, is an Associate Postgraduate Dean, Health Education England North West, Manchester, UK and consultant nephrologist, Manchester University Hospitals NHS Trust, UK.
Kevin Henshaw
Kevin Henshaw, BSc, is an Associate Head of Allied Health Programmes, Department of Allied Healthcare, Faculty of Health, Social Care & Medicine, Edge Hill University, Ormskirk, UK.
Jeremy Brown
Jeremy Brown, BA, PhD, is a Professor of Clinical Education in the Health Research Institute, Faculty of Health, Social Care & Medicine, Edge Hill University, Ormskirk, UK.
References
- Anton N, Bean EA, Hammonds SC, Stefanidis D. 2017. Application of mental skills training in surgery: a review of its effectiveness and proposed next steps. J Laparoendosc Adv Surg Tech A. 27(5):459–469.
- Anton N, Bean EA, Myers E, Stefanidis D. 2020. Optimizing learner engagement during mental skills training: a pilot study of small group vs. individualized training. Am J Surg. 219(2):335–339.
- Anton N, Beane J, Yurco A, Howley L, Bean E, Myers E, Stefanidis D. 2018. Mental skills training effectively minimizes operative performance deterioration under stressful conditions: results of a randomized controlled study. Am J Surg. 215(2):214–221.
- Anton N, Howley LD, Davis CK, Brown C, Stefanidis D. 2017. Minimizing deterioration of simulator-acquired skills during transfer to the operating room: a novel approach. Curr Surg Rep. 5(8):1–8.
- Anton N, Howley LD, Pimentel M, Davis CK, Brown C, Stefanidis D. 2016. Effectiveness of a mental skills curriculum to reduce novices’ stress. J Surg Res. 206(1):199–205.
- Anton N, Mizota T, Whiteside JA, Myers EM, Bean EA, Stefanidis D. 2019. Mental skills training limits the decay in operative technical skill under stressful conditions: results of a multisite, randomized controlled study. Surgery. 165(6):1059–1064.
- Anton N, Mulji N, Howley LD, Yurco AM, Tobben D, Bean E, Stefanidis D. 2017. Effects of a novel mental skills curriculum on surgical novices’ attention. J Surg Res. 219:86–91.
- Anton N, Stefanidis D. 2016. Should surgeons have mental skills training? Eur J Cardiothorac Surg. 50(1):1–3.
- Arora S, Aggarwal R, Sirimanna P, Moran A, Grantcharov T, Kneebone R, Sevdalis N, Darzi A. 2011. Mental practice enhances surgical technical skills: a randomized controlled study. Ann Surg. 253(2):265–270.
- Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. 2010. The impact of stress on surgical performance: a systematic review of the literature. Surgery. 147(3):318–330.e1–6.
- Brick N, MacIntyre T, Campbell M. 2015. Metacognitive processes in the self-regulation of performance in elite endurance runners. Psychol Sport Exerc. 19:1–9.
- Cambon L, Minary L, Ridde V, Alla F. 2012. Transferability of interventions in health education: a review. BMC Public Health. 12:497.
- Cecilio-Fernandes D, Cnossen F, Jaarsma D, Tio RA. 2018. Avoiding surgical skill decay: a systematic review on the spacing of training sessions. J Surg Educ. 75(2):471–480.
- Charles RL, Nixon J. 2019. Measuring mental workload using physiological measures: a systematic review. Appl Ergon. 74:221–232.
- Church H. 2019. PERFORM: performance enhancing routines for optimising readiness using metacognition for the management of acutely unwell patients [PhD Thesis]. Sheffield (UK): University of Sheffield.
- Church H, Murdoch-Eaton D, Patel R, Sandars J. 2017. What can medical educators learn from the Rio 2016 Olympic Games? Med Teach. 39(6):665–666.
- Clowes H, Knowles Z. 2013. Exploring the effectiveness of pre-performance routines in elite artistic gymnasts: a mixed method investigation. Sci Gymnast J. 5(2):27–40.
- Cotterill S. 2010. Pre- performance routines in sport: current understanding and future directions. Int Rev Sport Exerc Psychol. 3(2):132–153.
- Cotterill S. 2011. Experiences of developing pre-performance routines with elite cricket players. J Sport Psychol Action. 2(2):81–91.
- Czech DR, Ploszay A, Burke KL. 2004. An examination of the maintenance of preshot routines in basketball free throw shooting. J Sport Behav. 27(4):323.
- Gagne RM, Wager WW, Golas KC, Keller JM, Russell JD. 2005. Principles of instructional design. Amsterdam (The Netherlands): Wiley.
- Gallucci NT. 2013. Sport psychology: performance enhancement, performance inhibition, individuals, and teams. Hove (UK): Psychology Press.
- Goldberg MB, Mazzei M, Maher Z, Fish JH, Milner R, Yu D, Goldberg AJ. 2018. Optimizing performance through stress training – an educational strategy for surgical residents. Am J Surg. 216(3):618–623.
- Gordon M, Patricio M, Horne L, Muston A, Alston SR, Pammi M, Thammasitboon S, Park S, Pawlikowska T, Rees EL, et al. 2020. Developments in medical education in response to the COVID-19 pandemic: a rapid BEME systematic review: BEME Guide No. 63. Med Teach. 42(11):1202–1215.
- Greenspan MJ, Feltz DL. 1989. Psychological interventions with athletes in competitive situations: a review. Sport Psychol. 3(3):219–236.
- Hanin Y, Hanina M. 2009. Optimization of performance in top-level athletes: an action-focused coping approach. Int J Sports Sci Coach. 4(1):47–91.
- Hazell J, Cotterill ST, Hill DM. 2014. An exploration of pre-performance routines, self-efficacy, anxiety and performance in semi-professional soccer. Eur J Sport Sci. 14(6):603–610.
- Higgins M, Madan C, Patel R. 2021. Development and decay of procedural skills in surgery: a systematic review of the effectiveness of simulated-based medical education interventions. The Surgeon. 19(4):e67–e77.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, Altman DG, Barbour V, Macdonald H, Johnston M, et al. 2014. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 348:g1687.
- Hunziker S, Pagani S, Fasler K, Tschan F, Semmer NK, Marsch S. 2013. Impact of a stress coping strategy on perceived stress levels and performance during a simulated cardiopulmonary resuscitation: a randomized controlled trial. BMC Emerg Med. 13(1):8–9.
- Ignacio J, Dolmans D, Scherpbier A, Rethans J-J, Lopez V, Liaw SY. 2016. Development, implementation, and evaluation of a mental rehearsal strategy to improve clinical performance and reduce stress: a mixed methods study. Nurse Educ Today. 37:27–32.
- Ignacio J, Scherpbier A, Dolmans D, Rethans J-J, Liaw SY. 2017. Mental rehearsal strategy for stress management and performance in simulations. Clin Simul Nurs. 13(7):295–302.
- Immenroth M, Bürger T, Brenner J, Nagelschmidt M, Eberspächer H, Troidl H. 2007. Mental training in surgical education: a randomized controlled trial. Ann Surg. 245(3):385–391.
- Krage R, Tjon Soei Len L, Schober P, Kolenbrander M, van Groeningen D, Loer S, Wagner C, Zwaan L. 2014. Does individual experience affect performance during cardiopulmonary resuscitation with additional external distractors? Anaesthesia. 69(9):983–989.
- Lin JC, Paul AA, Greenberg PB. 2020. Mental skills training and resident surgical outcomes: a systematic review. J Surg Educ. 77(6):1377–1391.
- Lorello GR, Hicks CM, Ahmed S-A, Unger Z, Chandra D, Hayter MA. 2016. Mental practice: a simple tool to enhance team-based trauma resuscitation. Can J Emerg Med. 18(2):136–142.
- Mageau GA, Vallerand RJ. 2003. The coach-athlete relationship: a motivational model. J Sports Sci. 21(11):883–904.
- Maher Z, Milner R, Cripe J, Gaughan J, Fish J, Goldberg AJ. 2013. Stress training for the surgical resident. Am J Surg. 205(2):169–174.
- Mccann P, Lavallee D, Lavallee R. 2001. The effect of pre-shot routines on golf wedge shot performance. Eur J Sport Sci. 1(5):1–10.
- McGinn S, Alcock D, Cameron L. 2018. Straight from the horse’s mouth: understanding professional event riders’ mental preparation for maximising self-confidence prior to competition using thematic analysis. Comp Exerc Physiol. 14(4):261–270.
- McGowan CJ, Pyne DB, Thompson KG, Rattray B. 2015. Warm-up strategies for sport and exercise: mechanisms and applications. Sports Med. 45(11):1523–1546.
- Moher D, Liberati A, Tetzlaff J, Altman DG. 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 151(4):264–269.
- Németh K, Balogh L. 2021. The relationship between arousal zone, anxiety, stress and sports performance. Stadium. 3(2):1–14.
- Ogrinc G, Armstrong GE, Dolansky MA, Singh MK, Davies L. 2019. SQUIRE-EDU (Standards for QUality Improvement Reporting Excellence in Education): publication guidelines for educational improvement. Acad Med. 94(10):1461–1470.
- Raison N, Ahmed K, Abe T, Brunckhorst O, Novara G, Buffi N, McIlhenny C, van der Poel H, van Hemelrijck M, Gavazzi A, et al. 2018. Cognitive training for technical and non-technical skills in robotic surgery: a randomised controlled trial. BJU Int. 122(6):1075–1081.
- Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. 2007. Association between funding and quality of published medical education research. JAMA. 298(9):1002–1009.
- Sandars J, Cecilio-Fernandes D, Patel R, Gandomkar R. 2020. Avoid ‘running before we can walk’ in medical education research: the importance of design and development research. Med Teach. DOI:https://doi.org/10.1080/0142159X.2020.1854452.
- Sharma R, Gordon M, Dharamsi S, Gibbs T. 2015. Systematic reviews in medical education: a practical approach: AMEE guide 94. Med Teach. 37(2):108–124.
- Sharp L-A, Woodcock C, Holland MJ, Cumming J, Duda JL. 2013. A qualitative evaluation of the effectiveness of a mental skills training program for youth athletes. Sport Psychol. 27(3):219–232.
- Singer RN. 2000. Performance and human factors: considerations about cognition and attention for self-paced and externally-paced events. Ergonomics. 43(10):1661–1680.
- Stefanidis D, Anton NE, Howley LD, Bean E, Yurco A, Pimentel ME, Davis CK. 2017. Effectiveness of a comprehensive mental skills curriculum in enhancing surgical performance: results of a randomized controlled trial. Am J Surg. 213(2):318–324.
- Stefanidis D, Anton NE, McRary G, Howley LD, Pimentel M, Davis C, Yurco AM, Sevdalis N, Brown C. 2017. Implementation results of a novel comprehensive mental skills curriculum during simulator training. Am J Surg. 213(2):353–361.
- Vealey RS. 1988. Future directions in psychological skills training. Sport Psychol. 2(4):318–336.
- Wang CH, Chang CC, Liang YM, Shih CM, Chiu WS, Tseng P, Hung DL, Tzeng OJL, Muggleton NG, Juan CH. 2013. Open vs. closed skill sports and the modulation of inhibitory control. PLoS One. 8(2):e55773.
- Wetzel CM, George A, Hanna GB, Athanasiou T, Black SA, Kneebone RL, Nestel D, Woloshynowych M. 2011. Stress management training for surgeons – a randomized, controlled, intervention study. Ann Surg. 253(3):488–494.
- Wright C, Hogard E, Ellis R, Smith D, Kelly C. 2008. Effect of PETTLEP imagery training on performance of nursing skills: pilot study. J Adv Nurs. 63(3):259–265.