Abstract
Background
Satisfaction of pregnancy and childbirth is an important quality measure of maternity care. Satisfaction questionnaires generally result in high scores. However, it has been argued that dissatisfaction relies on a different construct. In response to a worldwide call for obstetric care that is more woman-centered, we identified and described the contributors to suboptimal satisfaction with pregnancy and childbirth.
Methods
A prospective subcohort of 739 women from a larger cohort (Expect Study I, n = 2614) received a pregnancy and childbirth satisfaction questionnaire. Scores were transformed to a binary outcome whereby a score <100 points corresponded with less satisfied women. We performed a multiple logistic regression analysis to define independent perinatal factors related to suboptimal satisfaction.
Results
Decreased perceived personal well-being, antenatal anxiety, and obstetrician-led care during labor were all independently associated with suboptimal pregnancy and childbirth satisfaction. No difference in satisfaction was found between antenatal care led by a midwife or an obstetrician, but midwife-led antenatal care reduced the odds of suboptimal satisfaction compared to women who were transferred to an obstetrician in the antenatal period. Antenatal anxiety was experienced by 25% of all women and is associated with decreased satisfaction scores.
Discussion
Screening and treatment of women suffering from anxiety might improve pregnancy and childbirth satisfaction, but further research is necessary. Women’s birthing experience may improve by reducing unnecessary secondary obstetric care.
Introduction
Satisfaction with care delivered during pregnancy and birth is a topic of increasing interest and is an essential component of quality of obstetric care [Citation1]. In the Netherlands, one in six women has a negative recall of their birth experience [Citation2]. The prevalence of post-traumatic stress disorders resulting from childbirth is estimated at 2.9% [Citation3]. Patient satisfaction and birth experience are important factors influencing short- and long-term outcomes of both mother and child (e.g. postpartum depression, the ability to breast-feed, and child abuse) [Citation1].
Studies of satisfaction with childbirth care are beset by several problems. The role of the healthcare professional is an influential factor shaping a woman’s birthing experience [Citation4]. Findings regarding the contribution of several other factors to satisfaction with obstetric care, such as age and pain, are inconsistent [Citation1,Citation5]. Satisfaction questionnaires administered shortly after birth generally result in high satisfaction scores. It has been argued that women may be unable to assess the perceived maternity care properly because they are unaware of other options [Citation6]. Additionally, satisfaction and dissatisfaction are considered to be different constructs rather than a continuum of each other [Citation7]. It may be better to focus on determinants associated with women who are not perfectly satisfied with the obstetric care services received during pregnancy and birth [Citation8]. Focusing on the less satisfied women may result into renewed insights that could improve obstetric care. At present, few studies have focused on determinants of suboptimal care as perceived as such by pregnant women [Citation5].
Antenatal anxiety is related to several adverse pregnancy outcomes (e.g. spontaneous preterm birth, low birth weight [Citation9]) and is associated with a negative subsequent birthing experience [Citation10]. The negative influence of maternal anxiety upon satisfaction levels with received obstetric care services has been reported as well, but mostly for specific subgroups (i.e. women with fear of birth) [Citation11,Citation12].
Women’s satisfaction regarding pregnancy and labor is also associated with parity. In general, multiparous women report higher levels of satisfaction as compared to nulliparous women [Citation13,Citation14]. Furthermore, it is likely that multiparous women’s expectations concerning their current pregnancy is influenced by their previous experiences with pregnancy, giving birth, and the obstetric care system [Citation11]. These expectations are likely to be more realistic than those of nulliparous women (e.g. prior birth mode is an important prognostic factor for the subsequent mode of birth [Citation15,Citation16]) which expectedly contributes to better satisfaction levels [Citation13].
In this study, we examined the Pregnancy and Childbirth Satisfaction (PCS) of women who recently gave birth in a prospective multicenter cohort. Our objective was to identify factors independently associated with suboptimal PCS and to evaluate the association of maternal anxiety with subsequent PCS in a general population.
Methods
We conducted a cross-sectional analysis among a subgroup of a prospective multicenter cohort study, the Expect Study I. The recruitment of this cohort has been described in detail elsewhere [Citation17]. Briefly, women aged 18 years or older were recruited at their first prenatal visit (<16 weeks of pregnancy), in the south region of the Netherlands between 2013 and 2015. Pregnancies ending in a miscarriage (<16 weeks of gestation) or termination before 24 weeks of gestation and women lost-to-follow-up were excluded from the main cohort. Additionally, for this study, we excluded twin pregnancies.
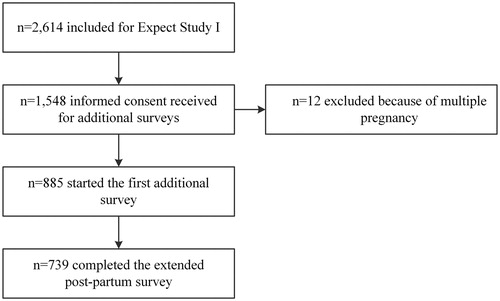
Women were approached for participation in a sub cohort of the Expect Study I after completion of the first survey (). Participants in this subcohort received additional surveys at 24 and 32 weeks of gestation. Moreover, the postpartum survey of the Expect Study, sent 6 weeks after the due date, was extended. The additional questions these women received addressed topics of patient satisfaction, anxiety state, and obstetric care services used. Women who reported preterm birth during the surveys at 24 or 32 weeks were automatically redirected to the postpartum survey.
The medical ethics committee of Maastricht University Medical Center (MUMC+) evaluated the study protocol and declared that no ethical approval was necessary for this study under Dutch law (METC-17-4-057). All participants gave informed consent.
Pregnancy and childbirth satisfaction was measured using the pregnancy and childbirth questionnaire (PCQ). The PCQ is a validated questionnaire measuring perceived quality of care among post-partum women [Citation18]. With 25 questions using a five-point Likert scale, it addresses topics specifically related to pregnancy and giving birth. Because the PCQ contains questions addressing childbirth, the PCQ was incorporated in the postpartum questionnaire. PCQ-scores were converted so that higher scores correlate with higher levels of satisfaction. Total scores can range from 25 to 125 points (Cronbach’s alpha 0.92). We classified women with a total PCQ score of less than 100 points, mean score <4 out of 5, less satisfied regarding their childbirth experience. In this study, we classified these women as “dissatisfied”. Therefore, we will refer to this group from now on as Pregnancy and Childbirth Dissatisfaction (PCD) instead of PCS.
To estimate the strength of the association of independent variables with PCD, we used multiple logistic regression analysis. The independent variables of interest were selected from the literature and consist of maternal factors, neonatal health outcomes, and factors related to the obstetric care received. Additionally, we performed sub-analyses for nulliparous and multiparous women.
Maternal factors included demographic variables such as age, educational degree, and socio-economic status. Other factors were; antenatal anxiety, parity (nulliparous or multiparous), decrease in perceived personal wellbeing, a neonatal health composite outcome, and a maternal health composite outcome.
Antenatal anxiety levels were measured using the state anxiety items of the State-Trait Anxiety Inventory (STAI), completed at 24 weeks of gestation. The STAI is a validated and commonly used inventory for the measurement of the general anxiety state. Consisting of 20 items using a four-point Likert scale, STAI scores can range from 20–80. Higher STAI scores represent a higher state of anxiety [Citation19]. We used a threshold of 39 points to identify antenatal anxiety as this cutoff has been suggested to detect clinical significant anxiety symptoms [Citation20].
Socio-economic status was estimated using postal codes and corresponding socio-economic status scores provided by the Dutch government [Citation21].
A decrease in perceived personal well-being was defined as a postpartum self-report score (scale 0-100) that was at least 10 points lower than the health status reported at enrollment (<16 weeks of gestation). Personal wellbeing was measured with the Euroqol Visual Analog Scale [Citation22].
We defined the maternal health composite outcome, a binary outcome, as an occurrence of either pre-eclampsia, gestational diabetes, postpartum hemorrhage (reported blood loss >1000 ml), or admission to an intensive or high care unit.
The neonatal composite outcome, a binary outcome defined in Expect Study I [Citation17], was defined as an occurrence of one of the following situations; perinatal death within seven days after birth, asphyxia (Apgar score <7 after 5 min), admission to a neonatal intensive care unit (NICU) within 28 days after birth, birthweight <2.3 weight percentile, birth before 32 completed weeks of pregnancy. The birthweight percentile was assessed using Dutch customized birth weight curves which correct for gestational age, ethnicity, gender and parity [Citation23].
Parity and all items of both the neonatal and maternal composite health outcomes, were retrieved from discharge letters, medical records, and the questionnaires. In case of discrepancies, we contacted the corresponding healthcare professional for the final decision.
Independent variables related to the obstetric care services received were: healthcare professional in lead during antenatal care until at least 34 weeks of gestation (categorical variable: autonomous midwife in a primary care setting, obstetrician in a secondary care setting, or both as a result of transfer of care); healthcare professional during labor (categorical variable: midwife, obstetrician, or both as a result of transfer during labor), birth mode (categorical variable: spontaneous vaginal birth, instrumental vaginal birth, or cesarean section), and usage of analgesics (epidural analgesia, intravenous remifentanil) during labor (yes/no). The variable “transfer of care” refers to transfer in only one direction, namely from midwife (primary care) to obstetrician (secondary care). In case of antenatal or intrapartum transfer of care after 34 weeks of gestation, we considered the healthcare professional who was in lead until 34 weeks of gestation to be the one in lead during antenatal care.
Missing data for explanatory variables were imputed using stochastic regression imputation with predictive mean matching as the imputation model [Citation24]. Characteristics of the observed cohort were described as mean ± standard deviation (SD) for continuous variables. Categorical variables were expressed as an absolute value with a percentage. We compared the distribution of characteristics in order to evaluate the relatedness of the imputed cohort and the observed cohort.
In the Dutch obstetric system, obstetric care is divided in primary, secondary and tertiary care. Autonomous midwives provide care for low-risk pregnant women in primary care independently. Women with high-risk pregnancies receive care by obstetricians in a secondary care (hospital) setting. If women remain low-risk throughout pregnancy, they remain under the supervision of their midwife, including the postpartum period. These women have the option of giving birth at home or in a birthing center supervised by their midwife, or in a hospital supervised by an obstetrician. Women with a high-risk pregnancy are always supervised by an obstetrician and thus give birth in a hospital. Antenatal, intrapartum or postpartum transfer of care, from midwife to obstetrician, is a result of either an unexpected finding or a complication during pregnancy or labor.
Results
In total 2614 women were included in the Expect cohort of whom 1548 (59%) gave informed consent for receiving the additional questionnaires. Twelve participants were excluded because of multiple gestation, which complicates the interpretation of the neonatal composite outcome. After providing informed consent, 885 women eventually participated in the sub cohort by completing the first additional survey. The PCQ was completed by the majority of these women (n = 739, 84%), implying a loss to follow-up of 16%.
displays the characteristics of participants, illustrating the differences between participants lost to follow-up and those who completed the postpartum survey. The differences between these groups were minimal. Women lost to follow-up had a slightly lower socio-economic status, they tended to have a lower level of education and were more likely to receive analgesics during labor. The postpartum questionnaire is the only instrument with questions regarding a decreased perceived personal well-being and admission to a high care or intensive care unit. As a result, differences with respect to these variables between completers and women lost to follow-up cannot be measured.
Table 1. Characteristics of the non-responders, the observed cohort, imputed cohort, and women lost to follow-up.
Overall, total PCQ-scores were high with a mean score of 109.7 out of 125 points for all respondents (SD 12.5). One quarter of all respondents (n = 176) had PCD, with a mean PCQ score of 92.6 points (SD 6.8). As shown in , these women scored lower on all subscales.
Table 2. Pregnancy and Childbirth Questionnaire scores.
In the multivariable logistic regression, several factors were significantly associated with PCD. Results were adjusted for all other factors, as shown in . Statistically significant maternal factors associated with PCD were decreased perceived personal wellbeing (odds ratio: 1.62; 95% CI: 1.09–2.40), and antenatal anxiety (odds ratio: 2.23; 95% CI: 1.50–3.30). Age was borderline significant with younger women tending to be more likely to experience PCD (odds ratio: 0.95; 95% CI: 0.90–1.00).
Table 3. Multiple logistic regression of maternal and healthcare factors related to pregnancy and childbirth discontent.
Regarding factors related to obstetric care services, there was a statistically significant association between PCD and the healthcare professional in charge of antenatal care and during labor. Transfer from primary to secondary care during the antenatal period was associated with increased PCD. Antenatal transfer of care before 34 weeks of gestation, was significantly associated with PCD when compared to uninterrupted midwife led care (odds ratio: 1.82; 95% CI: 1.10–3.00). Antenatal transfer also increased the odds of PCD (albeit not significantly) when compared to uninterrupted obstetrician led care (odds ratio: 1.62; 95% CI: 0.93–2.83).
If all labor stages were led by an obstetrician (n = 368), the odds ratio for experiencing PCD was 2.33 (95% CI: 1.34–4.08), compared to all labor stages led by a midwife (n = 232). For women who were referred by their midwife to an obstetrician during labor (n = 100), the odds ratio of PCD was 0.80 (95% CI: 0.37–1.65) compared to those who were assisted by their midwife from onset of labor.
We performed sub-analyses for nulliparous and multiparous women. This did not result in material differences except for cesarean section. A cesarean section was significantly correlated with PCD in nulliparous women (odds ratio 2.68; 95% CI: 1.30–5.57), but not in multiparous women (odds ratio 0.61; 95% CI: 0.25–1.47).
Discussion
In general, women were highly satisfied with the obstetric care received during their pregnancy and childbirth period. Women who experienced PCD scored lower on all subscales, indicating that PCD cannot be attributed to one of the PCQ subscales.
Factors statistically significantly and independently related with PCD were antenatal anxiety, decreased perceived personal wellbeing, and labor led by an obstetrician. Antenatal transfer of care significantly increased the odds upon PCD compared to antenatal care led by a midwife and tends to increase the odds upon PCD compared to antenatal care led by an obstetrician.
The main strengths of our study are the multicenter prospective cohort design, the large sample size, and the completeness of data. Using a multicenter prospective design improves the probability of collecting a representative sample. Furthermore, it enables optimal measurement of outcomes by minimizing recall bias and recording of all independent variables before completion of the PCQ. Additionally, the PCQ, used to assess satisfaction, has been validated among Dutch women and takes the unique features of the Dutch obstetric care system into account [Citation18,Citation25].
A limitation of this study is that our sub cohort may suffer from some selection bias due to non-response rates, particularly since participants were included from a larger cohort [Citation26]. However, differences between the sub cohort and main cohort were minimal. Moreover, the differences between women who agreed to receive additional surveys but never responded them and those who did were minimal as well, as shown in . For women who started with the first additional survey eventually only 16% did not complete the postpartum questionnaire. For women who did complete the postpartum questionnaire, we had 98% completeness of data. By imputing independent variables containing missing data, we limited the possibility of biased results and a loss of statistical precision [Citation27].
To obtain sufficient numbers of women with PCD in our analysis, we focused on women who experienced less than perfect obstetric care, using a total PCQ score of less than 100 points as a cutoff. Our study does not have qualitative data regarding the level of satisfaction or dissatisfaction related to the obstetric care services. However, the amount of studies using the PCQ questionnaire is limited and none of these use dissatisfaction as outcome [Citation18,Citation25].
In line with previous reports, our results indicate that most postpartum women are highly satisfied with obstetric care [Citation6,Citation25,Citation28–30]. We found no association between PCD and maternal demographic factors including, socio-economic status, educational level, and parity. These results correspond with the findings by previous reports [Citation14]. We found a borderline association between PCD and maternal age, whereby younger women tend to be more likely to experience PCD. Results of previous studies are inconsistent regarding the influence of maternal age. Some studies report younger women tend to reflect on their childbirth experience more negatively, whereas a recent study, focusing on discontent as well, does not report any effect of age [Citation5,Citation30,Citation31]. Additionally, since age is a nonmodifiable factor, its relevance in the reduction of PCD is limited; still it could serve as a risk indicator increasing awareness among healthcare professionals.
Interestingly, the neonatal and maternal composite outcomes, measures of the occurrence of complications, were not correlated with PCD, but there was a significant association between decreased perceived personal wellbeing and PCD. This suggests that it is not the presence or absence of complications, but rather perceived wellbeing that affects the experience of pregnancy and birth care. It has been reported that the interaction between a woman and her healthcare professional has a greater influence upon women’s perceptions of birth than the physical experience of the birth itself [Citation32].
Our analysis discovered antenatal anxiety is highly correlated to PCD. Nearly a quarter of the women met the criteria of clinically relevant anxiety. Taken together, this makes antenatal anxiety an important factor of interest in order to reduce the number of women who experience PCD.
Referral during antenatal care, which results in transfer from primary care to secondary care, was associated with increased odds of PCD. Although several studies discuss the effects of transfer during labor, studies reporting antenatal transfer are limited. This could be due to the unique Dutch setting, which divides obstetric care between primary and secondary care. Women generally go to a midwife for their first antenatal visit, and in case of a healthy woman with an uncomplicated pregnancy, they receive midwife-led care throughout pregnancy, labor and the postpartum period. Due to the nature of this system, transfer of care is a result of either an unexpected finding or a complication during pregnancy or childbirth. This may increase anxiety. In our analysis we adjusted for clinically relevant anxiety, however the increase of anxiety may be more subtle. Another possibility explaining the increased odds of PCD, may be the result of feelings of loss of control [Citation2,Citation32].
We found no association of PCD with either mode of birth or primary (midwife-led) or secondary (obstetrician-led) antenatal care. However, we did find a correlation between the healthcare professional in charge during labor and PCD. Women assisted by a midwife throughout all stages of labor were significantly less likely to experience PCD when compared to women assisted by an obstetrician. This accords with previous literature showing that women receiving continuity of midwifery care are more likely to be satisfied [Citation33]. In contrast with the findings of previous reports [Citation2,Citation29,Citation32,Citation34], transfer during labor was not associated with PCD. The odds of PCD did not differ significantly between women who were transferred during labor and women who continued to receive midwife-led care (adjusted odds ratio 0.80; 95% CI: 0.37–1.65). Furthermore, the odds of PCD was significantly lower for women who were transferred during labor compared to women who received obstetrician-led care during the entire birthing process (adjusted odds ratio 0.34; 95%CI: 0.17–0.66).
Unfortunately, our data do not permit a reliable analysis regarding the reasons for transfer during labor. A woman may be referred for an emergency with varying degrees of urgency (and experienced associated stress) or a woman may be referred as a result of her request of analgesics. In case of a medical emergency, it is reasonable to believe that a woman will feel a loss of control, which has been strongly associated with a traumatic childbirth experience [Citation32]. Because we do not have information on the reasons for transfer of care, we are not able to analyze this with our data, but it is interesting that women who are transferred have lower levels of PCD. This may suggest that, overall, the Dutch system of primary and secondary care works well with respect to women’s birthing experience in relation to transfer during labor.
Our sub-analyses in nulliparous and multiparous women did not yield any material differences except for cesarean section and level of antenatal care. These two factors increase the odds of PCD only in nulliparous women. A possible explanation for this discrepancy could be a difference in expectations between nulliparous and multiparous women. Unmet expectations have been linked to influence women’s satisfaction with pregnancy and childbirth [Citation13]. A substantial proportion of multiparous women may have received obstetrician-led antenatal care, or a cesarean in any of their previous pregnancies. As a result, their expectations regarding the course of their current pregnancy may have altered.
Implications
At the moment, the Dutch obstetric system is changing, with a movement toward more integrated care [Citation35,Citation36]. The Ministry of Health published a report promoting patient-centred care combined with integrated care and shared decision making as key concepts of the future obstetric care system [Citation37]. As a result, there is increased interest in the use of individual risk-management systems and decision support aids [Citation17,Citation38]. Depending on how it is organized, integrated care has the potential to increase positive collaboration between midwives in a primary care setting and obstetricians in a secondary care setting. Those who design models of integrated care should take note of the positive birthing experiences associated with midwives and find ways to insure that features of midwife-led care are not lost in the transition [Citation39,Citation40].
Antenatal anxiety was the most important factor related to a negative childbirth experience. It is already known that maternal anxiety is related to adverse outcomes, but this study shows that it is an independent factor for the way women experience their childbirth [Citation9].
Current guidelines on anxiety in pregnancy are mostly focused on anxiety or mood disorders and the effects of medication [Citation41,Citation42]. However, they offer little help for women or healthcare professionals who are dealing with the less severe cases. Our study found that almost 25% of women had an anxiety score that was clinically relevant. Postpartum interventions in women with poor mental health have shown to be cost effective [Citation43]. Our work underscores the need for further research on the effects of screening and treatment for anxiety in pregnancy. Similar to somatic diseases like diabetes and hypertension, pregnancy might be a stress test for women’s mental health and early identification and treatment is likely to result in an improved birthing experience [Citation44,Citation45]. Decision support aids are reported to reduce anxiety scores and may be effective tools to imply in order to reduce PCD [Citation46].
Conclusions
Decreased perceived personal well-being, increased anxiety, transfer of care antenatal, and obstetrician-led birth were all independently associated with PCD. One in four women experienced general antenatal anxiety. Women’s birthing experience may improve by increased awareness regarding women’s antenatal anxiety state and reducing the proportion of women unnecessarily receiving obstetric care in a secondary care setting.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J Adv Nurs. 2004;46(2):212–219.
- Rijnders M, Baston H, Schönbeck Y, et al. Perinatal factors related to negative or positive recall of birth experience in women 3 years postpartum in the Netherlands. Birth. 2008;35(2):107–116.
- Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 2014;34(5):389–401.
- Larkin P, Begley CM, Devane D. Women's experiences of labour and birth: an evolutionary concept analysis. Midwifery. 2009;25(2):e49–e59.
- Baas CI, Wiegers TA, de Cock TP, et al. Client-related factors associated with a “less than good” experience of midwifery care during childbirth in the Netherlands. Birth. 2017;44(1):58–67.
- Teijlingen ER, Hundley V, Rennie AM, et al. Maternity satisfaction studies and their limitations: “What is, must still be best”. Birth. 2003;30(2):75–82.
- Lee AV, Moriarty JP, Borgstrom C, et al. What can we learn from patient dissatisfaction? An analysis of dissatisfying events at an academic medical center. J Hosp Med. 2010;5(9):514–520.
- Redshaw M. Women as consumers of maternity care: measuring “satisfaction” or “dissatisfaction”? Birth. 2008;35(1):73–76.
- Grigoriadis S, Graves L, Peer M, et al. Maternal anxiety during pregnancy and the association with adverse perinatal outcomes: systematic review and meta-analysis. J Clin Psychiatry. 2018;79(5):e1–e22.
- Munstedt K, von Georgi R, Eichel V, et al. Wishes and expectations of pregnant women and their partners concerning delivery. J Perinatal Med. 2000;28(6):482–490.
- Tschudin S, Alder J, Hendriksen S, et al. Previous birth experience and birth anxiety: predictors of caesarean section on demand? J Psychosom Obstet Gynaecol. 2009;30(3):175–180.
- Spice K, Jones SL, Hadjistavropoulos HD, et al. Prenatal fear of childbirth and anxiety sensitivity. J Psychosom Obstet Gynaecol. 2009;30(3):168–174.
- Christiaens W, Bracke P. Assessment of social psychological determinants of satisfaction with childbirth in a cross-national perspective. BMC Pregnancy Childbirth. 2007;7(1):26.
- Britton JR. The assessment of satisfaction with care in the perinatal period. J Psychosom Obstet Gynaecol. 2012;33(2):37–44.
- Verhoeven CJ, Nuij C, Janssen-Rolf CR, Schuit E, et al. Predictors for failure of vacuum-assisted vaginal delivery: a case-control study. Eur J Obstet Gynecol Reprod Biol. 2016;200:29–34.
- Schoen C, Navathe R. Failed induction of labor. Semin Perinatol. 2015;39(6):483–487.
- Meertens LJE, Scheepers HC, De Vries RG, et al. External validation study of first trimester obstetric prediction models (Expect Study I): research protocol and population characteristics. JMIR Res Protoc. 2017;6(10):e203.
- Truijens SE, Pommer AM, van Runnard Heimel PJ, et al. Development of the Pregnancy and Childbirth Questionnaire (PCQ): evaluating quality of care as perceived by women who recently gave birth. Eur J Obstet Gynecol Reprod Biol. 2014;174:35–40.
- Ploeg HM, Defares PB, Spielberger CD. Handleiding bij de Zelf-Beoordelings Vragenlijst ZBV: een nederlandstalige bewerking van de Spielberger State-Trait Anxiety Inventory STAI-DY: Swets & Zeitlinger [Manual for ‘De Zelf-Beoordelings Vragenlijst (ZBV)’, a Dutch version of the Spielberger State-Trait Anxiety Inventory STAI-DY: Swets & Zeitlinger]; 1980.
- Julian LJ. Measures of anxiety. Arthritis Care Res. 2011;63:S467–S472.
- SCP. SCP Statusscores: Sociaal en Cultureel Planbureau; 2017. [cited 2017 Aug 08]. Available from: http://www.scp.nl/Formulieren/Statusscores_opvragen.
- EuroQol-Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
- Visser GH, Eilers PH, Elferink-Stinkens PM, et al. New Dutch reference curves for birthweight by gestational age. Early Human Develop. 2009;85(12):737–744.
- Van Buuren S. Flexible imputation of missing data. 2nd. Boca Raton, FL: Chapman & Hall/CRC; 2018.
- Truijens SE, Banga FR, Fransen AF, et al. The effect of multiprofessional simulation-based obstetric team training on patient-reported quality of care: a pilot study. Simul Healthc. 2015;10(4):210–216.
- Berman DM, Tan LL, Cheng TL. Surveys and response rates. Pediatrics Rev. 2015;36(8):364–366.
- Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338(jun29 1):b2393–b2393.
- Karlström A, Nystedt A, Hildingsson I. The meaning of a very positive birth experience: focus groups discussions with women. BMC Preg Childbirth. 2015;15(1):251.
- Hitzert M, Hermus MA, Scheerhagen M, et al. Experiences of women who planned birth in a birth centre compared to alternative planned places of birth. Results of the Dutch Birth Centre Study. Midwifery. 2016;40:70–78.
- Jenkinson C, Coulter A, Bruster S, et al. Patients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. QSHC. 2002;11(4):335–339.
- Borjesson B, Paperin C, Lindell M. Maternal support during the first year of infancy. J Adv Nurs. 2004;45(6):588–594.
- Hollander MH, van Hastenberg E, van Dillen J, et al. Preventing traumatic childbirth experiences: 2192 women’s perceptions and views. Arch Womens Ment Health. 2017;20(4):515–523.
- Sandall J, Soltani H, Gates S, et al. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database System Rev. 2015;(9):Cd004667.
- Geerts CC, van Dillen J, Klomp T, et al. Satisfaction with caregivers during labour among low risk women in the Netherlands: the association with planned place of birth and transfer of care during labour. BMC Preg Childbirth. 2017;17(1):229.
- Visser G. Obstetric care in the Netherlands: relic or example?. JOGC. 2012;34(10):971–975.
- Boesveld IC, Valentijn PP, Hitzert M, et al. An approach to measuring integrated care within a maternity care system: experiences from the maternity care network study and the Dutch Birth Centre Study. Int J Integr Care. 2017;17(2):6.
- Geboortezorg EZI. Zorgstandaard Integrale Geboortezorg. Utrecht: College Perinatale Zorg; 2016.
- Schoorel EN, Vankan E, Scheepers HC, et al. Involving women in personalised decision-making on mode of delivery after caesarean section: the development and pilot testing of a patient decision aid. BJOG: Int J Obstet Gy. 2014;121(2):202–209.
- Perdok H, Jans S, Verhoeven C, et al. Opinions of maternity care professionals and other stakeholders about integration of maternity care: a qualitative study in the Netherlands. BMC Preg Childbirth. 2016;16(1):188.
- Hodnett ED. Continuity of caregivers for care during pregnancy and childbirth. Birth. 2000;27(3):218–218.
- Yonkers KA, Wisner KL, Stewart DE, et al. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;114(3):703–713.
- National Collaborating Centre for Mental Health. National Institute for Health and Clinical Excellence: Guidance. Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance: Updated edition. Leicester (UK): British Psychological Society; 2014.
- Chojenta C, William J, Martin MA, et al. The impact of a history of poor mental health on health care costs in the perinatal period. Arch Womens Ment Health. 2019;22:467–473.
- Hermes W, Tamsma JT, Grootendorst DC, et al. Cardiovascular risk estimation in women with a history of hypertensive pregnancy disorders at term: a longitudinal follow-up study. BMC Preg Childbirth. 2013;13(1):126.
- Kramer CK, Swaminathan B, Hanley AJ, et al. Each degree of glucose intolerance in pregnancy predicts distinct trajectories of beta-cell function, insulin sensitivity, and glycemia in the first 3 years postpartum. Dia Care. 2014;37(12):3262–3269.
- Tucker Edmonds B. Shared decision-making and decision support: their role in obstetrics and Curr Opin Obstet Gynecol. 2014;26(6):523–530.