ABSTRACT
Background
Clinical practice guidelines and best practice statements aim to optimise patient outcomes through recommended processes of care. The Aphasia United Best Practice Recommendations were developed to provide multi-national best-practice guidance for post-stroke aphasia services. The recommendations were developed through a multi-stage process which synthesised research evidence and the expert opinions of clinicians and researchers. To date, however, people with lived experience of aphasia have not contributed their expertise to these recommendations.
Aims
To explore the relevance, comprehensibility, and comprehensiveness of the Aphasia United Best Practice Recommendations, from the perspective of people with aphasia and their significant others. Conducted during the COVID-19 pandemic, a secondary aim was to evaluate participants’ satisfaction with videoconferencing for research.
Methods & Procedures
People with aphasia and their significant others participated in separate focus groups via videoconferencing. Participants were recruited at five Australian sites (representing major cities and regional locations). Participants rated the relevance and comprehensibility (clarity) of the recommendations and suggested improvements. Using the nominal group technique, participants assessed the comprehensiveness of the existing recommendations, and generated and prioritised new items for inclusion. These recommendations were synthesised across groups using qualitative content analysis. Participants rated their satisfaction with videoconferencing for research through a bespoke questionnaire.
Outcomes & Results
People with aphasia (n=13) and their significant others (n=10) participated in one of eight focus groups in Australia. Most participants rated the existing recommendations as highly relevant, however improvements to comprehensibility and comprehensiveness were suggested. Fifty-one new recommendations were prioritised and synthesised into seven themes for people with aphasia and six themes for significant others. The most highly ranked theme for people with aphasia was, Increased awareness about: what aphasia is, the impacts of aphasia, and how to communicate with a person with aphasia. The theme ranked most highly by significant others was, Aphasia services should be person and family centred. All participants reported being satisfied or highly satisfied with the use of Zoom videoconferencing for research.
Conclusions
People with aphasia and their significant others in Australia identified new important best practice recommendations for aphasia services. The results of this study suggest that revisions to existing recommendations may improve their relevance, comprehensibility, and comprehensiveness. Participants were satisfied with the use of videoconferencing for research. The results of this research will inform a future consensus process to finalise the revised recommendations and to pair them with measurable quality indicators for post-stroke aphasia services.
Introduction
Best practice recommendations and clinical practice guidelines are designed to guide the decision-making of clinicians and patients about healthcare (Lohr & Field, Citation1992). Such recommendations and guidelines are used to enhance service quality, while optimising the efficient use of available resources (Grimshaw & Russell, Citation1993; Institute of Medicine, Citation2011). When implemented effectively, best practice recommendations for stroke rehabilitation have been shown to improve patient outcomes (Hubbard et al., Citation2012). However, inconsistent implementation in clinical practice is common. For example, nearly 50% of stroke care services audited across England, Northern Ireland, and Wales, and 22% of those audited in Australia, complied with less than half of their respective stroke management guidelines (Donnellan et al., Citation2013; Schindel et al., Citation2022; Sentinel Stroke National Audit Programme, Citation2019; Stroke Foundation, Citation2020). The inconsistent adherence to best practice recommendations in clinical practice is a long-standing issue (Cabana et al., Citation1999). Known barriers to adherence in stroke rehabilitation include health professionals’ lack of awareness of interventions, lack of skills in applying interventions, and low motivation to implement evidence-based therapy (Munce et al., Citation2017). Speech-language pathologists have also identified that stroke guidelines are challenging to implement, citing their impractical nature, unclear presentation, and lack of client-centredness (Hadely et al., Citation2014). Historically, these barriers were further compounded in post-stroke aphasia management due to an absence of rigorously designed and comprehensive recommendations specific to aphasia management (Rohde et al., Citation2013; Shrubsole et al., Citation2016).
Aphasia United, an international body that seeks to support the provision of high-quality aphasia services, sought to address the gap in high-quality aphasia-specific guidelines through the development of a set of universal best practice recommendations for aphasia management (Simmons-Mackie et al., Citation2016). A set of 10 best practice recommendations were produced using a multi-stage process. First, recommendations for aphasia management were extracted from published research, national clinical guidelines for stroke and/or aphasia, and evidence websites. Recommendations were themed and iteratively reviewed and revised by an expert panel. This was followed by a multi-national consensus process with professional aphasia experts. The result was a set of brief, practical, and user-friendly recommendations, that have subsequently been translated into 29 languages and aphasia-friendly formats (https://www.aphasiatrials.org/multilingual-information-sheets/). However, like many existing guidelines, the input of people with lived experience is yet to be applied to the content or format of the recommendations.
Attaining outcomes that matter to consumers is vital to achieving high-value healthcare (Porter & Lee, Citation2013). In line with this, seeking the opinions and experiences of health service users and their significant others is widely considered an essential construct of high-quality healthcare (Australian Commission on Safety and Quality in Health Care, Citation2011; United States Department of Health and Human Services, Citation2008; WHO, Citation2000). Most creators of clinical guidelines recommended the inclusion of patients or their representatives in the development process, however guidance on how to best do this is less readily available (Selva et al., Citation2017). Inclusion of consumers is essential to the development of ecologically valid guidelines, given that developers are required to make judgements about whether an aspect of care would lead to a desirable outcome (Andrews et al., Citation2013) and consumers have their own values and preferences (Wallace et al., Citation2017). Moreover, consumer input has resulted in the identification of ideas that are novel and more easily implemented (Armstrong et al., Citation2018). Once developed, guidelines should then be accessible to consumers, empowering them to make informed decisions about their healthcare. It is well recognised that people with aphasia face unique barriers in accessing written information due to language impairment. The use of modifications to improve accessibility of written information is often preferred by people with aphasia (Rose et al., Citation2011) and can help their understanding of information (Rose et al., Citation2003). Despite this, clinical practice guidelines are not typically presented in a format that promotes accessibility. The Aphasia United Best Practice Recommendations are available in an “aphasia friendly” format, however people with aphasia have not assessed their comprehensibility. Therefore, the current research aimed to determine if people with aphasia and their significant others consider the Aphasia United Best Practice Recommendations to be: (1) relevant; (2) comprehensible (i.e., clear/ able to be understood); and (3) comprehensive (i.e., not missing essential recommendations). A further aim was to evaluate participants’ satisfaction with the use of videoconferencing as a platform for data collection.
Methods
Study design
Focus groups took place between June 2020 and July 2021 and used a modified nominal group technique (Delbecq et al., Citation1975). The nominal group technique is a structured group decision-making process, which supports small groups of participants to generate, and then prioritise, ideas in response to a question (Delbecq et al., Citation1975). This approach is recognised as an effective technique for gaining group consensus (Harvey & Holmes, Citation2012) and has been successfully used with people with communication disabilities including aphasia (Wallace et al., Citation2017). In the current study, the nominal group technique was modified to include assessment of the existing Aphasia United Best Practice Recommendations, in addition to generation and ranking of new best practice recommendations.
Due to the COVID-19 pandemic and social distancing restrictions, online data collection was undertaken using the videoconferencing platform Zoom (Zoom Video Communications, Citation2020). Ethical approval for this study was obtained from the Royal Brisbane and Women’s Hospital (HREC/2020/QRBW/62310) and The University of Queensland, Australia (2018002154).
Participants
Sampling and recruitment
Purposive sampling was used to recruit participants with aphasia with variation in age (<65 years; ≥ 65 years), sex (male; female), geographical remoteness (major city; regional), aphasia severity (mild-moderate; severe), and time since onset of aphasia (<12 months; ≥ 12 months). Aphasia severity was independently assessed by two members of the research team who are experienced speech-language pathologists (SW and CB). The Aphasia Severity Rating Scale (Goodglass et al., Citation2001) was used to rate and classify a conversation sample from the technology preparation session. People with aphasia were recruited through email networks, newsletters, aphasia-related community groups, social media, and word-of-mouth. Significant others were recruited using convenience sampling, whereby each person with aphasia was asked to nominate one person who they considered to be their significant other, to participate.
Eligibility criteria
The inclusion criteria for people with aphasia were: (a) over 18 years of age; (b) diagnosed with post-stroke aphasia; (c) able to participate in a focus group (with support for communication and technology use), as determined by the local speech-language pathologist or lead investigator; and (d) living in the community. Significant others of people with aphasia (family members or friends) aged 18 years or above who were English-speaking were eligible for inclusion in this study. Significant others were nominated by the person with aphasia and there were no other eligibility criteria for inclusion.
Informed consent
Consent was gained in alignment with Kagan and Kimelman’s (Citation1995) guidelines for acquiring informed consent from research participants with aphasia. Information about the study was provided verbally, in writing (with pictorial supports), and through a 4-minute video. The video presented images with a voice-over to convey a summary of information about the study (see https://youtu.be/oeFKNpaA-jk). More detailed information was available in the written participant information sheet and participants provided written consent. A representative from the Poche Centre for Indigenous Health and the Royal Brisbane and Women’s Hospital Cultural Capability Officer provided advice on how best to support the ethical, safe, and respectful inclusion of First Nations Australians in this research. This included: review of information sheets and consent forms to ensure they were clear, understandable, and appropriately formatted; advice on methods (e.g., to offer the option of participating in a group specific to Aboriginal/Torres Strait Islander people); and avenues for accessing support for culturally safe and respectful participation (e.g., engaging with Indigenous Liaison Officers and Community leaders where appropriate).
Pilot
The study was piloted in-person with four people with aphasia and three significant others in November 2018. The 10 existing Aphasia United Best Practice Recommendations were presented, and participants were asked the following questions: (a) “Do you agree with the statement? If not, why?” (b) “Do you recall receiving this aspect of care?”. After discussing the existing best practice statements, the following nominal question was presented: “Are there any other recommendations that you believe are essential for best practice aphasia services?” Following piloting, question (b) was removed to reduce discussion of previously received services and to increase focus on the relevance, comprehensibility, and comprehensiveness of the recommendations.
Procedures
All groups were facilitated by a qualified speech-language pathologist with experience using the nominal group technique (SW), supported by a minimum of two co-facilitators who provided communication and technology support and collected field notes. To promote consistency between groups, a procedural manual was developed, and all facilitators attended a training session and reviewed the video recording of the pilot group focus group session.
Technology preparation session and assessment of communication support needs
A week before each group, a technology preparation session was held with participants via Zoom. This included an explanation of technological requirements (e.g., bandwidth, webcam, speakers); practice with basic Zoom functions; and troubleshooting. Individual communication strategies (e.g., writing key words on the digital whiteboard) for participants with aphasia were also discussed and preferences were noted to accommodate specific needs.
Communication support
All written materials were designed according to aphasia-friendly principles to maximise comprehension (Rose et al., Citation2012). Strategies to maximise participation of people with aphasia in groups included: (a) use of short and simple questions supplemented by an aphasia-friendly slide presentation; (b) use of the Zoom shared whiteboard function to document key phrases spoken by facilitators or participants; (c) provision of extra response time; and (d) verification of participant responses in real-time by group facilitators (Dalemans et al., Citation2009).
Modified nominal group technique procedure
Two hours was allocated to each group. Separate groups were held for people with aphasia and for their significant others. Participants were allocated to groups according to their geographical location (i.e., major city or regional area). The following procedure was used:
Each of the 10 existing recommendations was presented individually. People with aphasia viewed the “aphasia friendly” version of the recommendations and family members the standard version. Participants took turns answering the following questions: “Do you agree with the recommendation?” (relevance); “Is the wording clear?” (comprehensibility).
The nominal question was then presented to the group: “Are there any other recommendations that you believe are essential for best practice aphasia services?” (comprehensiveness). Participants offered one response at a time until no new responses were generated. The responses were recorded by the group facilitator, using the Zoom shared whiteboard function, before a compiled list of new recommendations was generated.
Finally, each participant was assigned to a Zoom breakout room with a group facilitator to individually rank their top three new recommendations from the generated list. A Zoom satisfaction survey was also completed with facilitator support.
Data analysis
The relevance and comprehensibility of the existing recommendations were determined quantitatively by percentage agreement. Qualitative information about comprehensibility and comprehensiveness was recorded using the facilitator’s field notes. Verbatim quotes were recorded and transcribed to inform suggested amendments to best practice recommendations. To determine the relative importance of prioritised new recommendations quantitatively, participants’ rankings #1, #2 and #3 were assigned a point value: three, two and one points, respectively. These points were summed in real time within groups to produce a prioritised list. Subsequently, the prioritised ideas from each group were analysed using qualitative content analysis (Graneheim & Lundman, Citation2004) to allow comparison across groups. Content analysis was performed by authors SW and KS with input from all co-authors. Familiarisation with the dataset was achieved through repeated readings and review of audio recordings and notes. Similar ideas were then grouped into categories and further organised into larger themes. Based on McMillan et al. (Citation2014), a secondary analysis was conducted, involving calculation of the sum of scores and ranked priority.
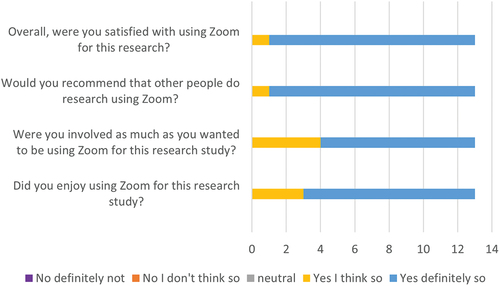
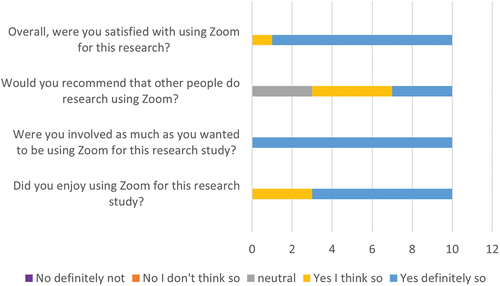
Participant satisfaction with research conducted using videoconferencing
Participants rated their satisfaction with use of the Zoom platform for research, answering four questions using a five-point Likert scale. These questions assessed level of satisfaction, enjoyment and involvement in using Zoom for the research and likelihood of recommending this mode of research participation to other people with aphasia. Participant ratings were analysed using descriptive statistics (i.e., frequencies and percentages of each rating per question).
Results
A total of 23 people (13 people with aphasia and 10 significant others) participated in the eight focus groups (Group 1: 3 people with aphasia from major city; Group 2: 3 people with aphasia from regional location; Group 3: 5 people with aphasia from major city; Group 4: 2 people with aphasia from regional location; Group 5: 3 significant others from major city; Group 6: 3 significant others from regional location Group 7: 2 significant others from major city; Group 8: 2 significant others from regional location). Variation in age (<65 years, 53%), sex (male, 69%), geographical remoteness (major city, 62%), aphasia severity (mild-moderate, 77%), and time since onset of aphasia (<12 months; 31%) was achieved for participants with aphasia. Most significant others were family members (90%). Participant characteristics are provided in . This study pre-dated the development of the DESCRIBE standards for reporting of participants in aphasia studies (Wallace et al., Citation2023) and therefore not all DESCRIBE characteristics are reported.
Table 1. Participant Characteristics (n=23)
Relevance and comprehensibility of the Best Practice Recommendations
There was 100% agreement from both stakeholder groups that eight of the 10 best practice recommendations were relevant. A small number of participants responded that recommendation 5: People with aphasia should be offered intensive and individualised aphasia therapy designed to have a meaningful impact on communication and life. This intervention should be designed and delivered under the supervision of a qualified professional and recommendation 8: Services for people with aphasia should be culturally appropriate and personally relevant were not relevant to all people with aphasia, however all participants agreed that the recommendations were important to retain. See for relevance ratings.
Table 2. Relevance and Comprehensibility of Existing Best Practice Recommendations and Suggested Changes.
Only one best practice recommendation was comprehensible to all participants: All health and social care providers working with people with aphasia across the continuum of care (i.e., acute care to end-of-life) should be educated about aphasia and trained to support communication in aphasia. Changes to wording were suggested for the remaining nine recommendations. Common suggestions for improvement of the existing recommendations included: explaining technical terms (e.g., explaining the acronym “AAC”, “suspected aphasia”), specifying subjects (e.g., who is a “qualified professional”), adding detail to make the recommendations more operationalisable (e.g., adding information about the optimal timing of the processes of care, such as when screening should occur). See for comprehensibility ratings and suggested changes to wording.
Comprehensiveness of the Best Practice Recommendations
Participants were asked to respond to the question, “Are there any other recommendations that you believe are essential for best practice aphasia services?” People with aphasia prioritised 28 ideas and significant others, 23 ideas. Using qualitative content analysis these ideas were organised into seven themes for people with aphasia (see ) and six themes for significant others (see ).
Table 3. People with aphasia: Themes across groups in response to the nominal question “Are there any other recommendations that are essential for aphasia services?”
Table 4. Significant Others: Themes across groups in response to the nominal question “Are there any other recommendations that are essential for aphasia services?”
People with aphasia
The most highly ranked theme for this group related to increased awareness about aphasia. This not only related to a desire for better understanding of what aphasia is, but also how to communicate with a person with aphasia. Equal second was the recommendation for coordinated, comprehensive, and consistent care and training; support; and access to technology for communication. Third and fourth respectively, were recommendations for increased social support and psychological support for people with aphasia and the same for their families. The fifth-highest ranked recommendation was for support for people with aphasia to build skills that support self-management and community re-integration. Finally, it was recommended that people with aphasia should receive information about their prognosis and factors that influence recovery.
Significant others
Of greatest importance to significant others in the current study was the need for aphasia services that are person- and family-centred. Equal second were the need for psychological support for families and the need for social support for families. Third most important was the recommendation that people with aphasia and their families receive coordinated, comprehensive, and consistent care. Equal fourth were the need for information about prognosis and recovery informed by assessment at regular timepoints; and greater awareness about aphasia in the public, and amongst people living with aphasia.
Participant satisfaction with videoconferencing platform Zoom
Participant ratings for all questions demonstrated that they were positive about using Zoom in this research study during the COVID-19 pandemic, as shown in . Overall, people with aphasia and significant others were satisfied with the use of Zoom for research purposes (12/13 participants with aphasia and 9/10 significant others rated they were “definitely” satisfied). Participants from both groups agreed that they were able to be involved as much as they had wanted to and that they had enjoyed using Zoom (10/13 participants with aphasia and 7/10 significant others rated they “definitely” enjoyed using Zoom. People with aphasia (12/13) indicated they would recommend that other people participate in research using Zoom. Significant others were either neutral (3/10) or positive (7/10) about making such a recommendation.
Discussion
This study explored the relevance, comprehensibility, and comprehensiveness of Aphasia United’s Best Practice Recommendations from the perspective of people with aphasia and their significant others. The existing 10 recommendations were considered relevant by all participants within both stakeholder groups and suggestions were made to improve their comprehensibility. In addition, participants generated new recommendations to enhance the comprehensiveness of the existing guidelines. While there were some differences in how each stakeholder group prioritised and generated recommendations, five common themes were identified. They were the need for (1) greater awareness of aphasia, (2) more coordinated, comprehensive, and consistent approaches to care, (3) greater social support, (4) greater psychological support for both people with aphasia and their families, and (5) more information about prognosis and recovery. Two additional themes (training and support for technology, and person- and family-centred care) were identified by one stakeholder group only.
Both stakeholder groups identified a need for increased awareness about what aphasia is, the impacts of aphasia, and how to communicate with a person with aphasia, as an important new recommendation. This finding aligns with previous research that there are low levels of aphasia awareness in the general population (Code et al., Citation2016) and that increased awareness is a desired outcome for people with aphasia and their families (Wallace et al., Citation2017). This recommendation was ranked highly by participants from regional sites (#1 for people with aphasia and #2 for significant others), indicating that awareness in regional areas where access to services can be limited is particularly important. Participants with aphasia from regional sites also highlighted the need for health professionals “to use the word ‘aphasia’ (not ‘communication difficulties’ or ‘speech problems’)”. Given that the term “aphasia” is widely used in scholarly publications, clinical practice guidelines, and by consumer organisations, consistent use of the term may be crucial to both awareness raising and health information seeking (Worrall et al., Citation2016).
Coordinated, comprehensive, and consistent care was highly valued by both people with aphasia and their significant others, and this may reflect the added burden experienced by stroke survivors in managing their recovery. In their systematic review, Gallacher and associates (Citation2013) highlighted the significant treatment burden experienced by people with stroke, including difficulty understanding stroke management, a lack of continuity of care and poor co-ordination of care transitions and discharge services. This is often further compounded for people with aphasia, whose communication impairments present a further barrier to receiving information and communication with healthcare providers (van Rijssen et al., Citation2022). The reference to comprehensive care reflects the previously reported preference for intensive and comprehensive aphasia services, including interprofessional psychoeducation and wellbeing sessions (Kincheloe et al., Citation2023).
Both participant groups prioritised the need for information about prognosis and recovery and factors that influence recovery, informed by assessment at regular timepoints. This finding is in accordance with recent research by Cheng and associates (2022a, Citation2022b) who found that both people with aphasia and significant others desire prognostic information and have a strong need to know what ‘recovery’ will look like. There is, however, great variation in both what prognostic information is delivered to people with aphasia and their significant others and how, and clinicians lack confidence in the task (Cheng et al., Citation2021). The prioritisation of this recommendation by participants in the current study, further underscores the need for continued attention to this complex area of clinical practice.
The need for greater psychological and social support was seen as essential by both stakeholder groups. This is unsurprising given people with aphasia and their significant others are at increased risk of experiencing a range of psychosocial problems in post-stroke recovery and rehabilitation (Zanella et al., Citation2023; Hilari & Northcott et al., Citation2017). Common impacts can include distress, grief, reduced social networks and participation in activities, and depression and anxiety (Hilari & Northcott, Citation2017; Zanella et al., Citation2023; Morris et al., Citation2017). Findings from the current study emphasised the importance of aphasia rehabilitation addressing loss, grief, and depression. This finding is also consistent with other recent studies, in that people with aphasia and their significant others value psychological care for depression and hold various preferences for the type of support needed (Iwasaki et al., Citation2022; Baker et al., Citation2020). Psychological support and care can include interdisciplinary approaches to identifying and actively monitoring mood problems, and prevention and treatment using therapies matched to the needs of the person (Kneebone et al., Citation2016). There is growing research evidence to address psychological problems and enhance wellbeing for people with aphasia and/or their significant others. including rehabilitation therapies for depression and anxiety (Baker et al., Citation2018; Ryan et al., Citation2022); counselling (Sekhon et al., Citation2022); behavioural activation (Thomas et al., Citation2019); relaxation therapy (El-Helou et al., Citation2023); community aphasia group support (Pettigrove et al., Citation2022); peer-befriending (Hilari et al., Citation2021) and solution-focused brief therapy (Northcott et al., Citation2021). A previous systematic review also found that to improve the acceptability of social support within one’s social network, family and friends need information about aphasia and supported conversation training (Manning et al., Citation2019). Despite this growing evidence base, there are barriers to psychological care and access to services (Baker et al., Citation2021). Potential solutions require effective translation of the evidence and best practice recommendations to stroke rehabilitation (Baker et al., Citation2021). There is an opportunity for clinicians to increase knowledge and upskill in counselling and provision of therapies with appropriate training (Sekhon et al., Citation2022).
Another new recommendation prioritised by participants with aphasia was the need to receive training, support, and access to technology for communication. Digital access has been identified as a challenge for people with aphasia (Kelly et al., Citation2016) and is an area requiring future research. Access to technology has many potential benefits, including enhanced self-management through online therapy programs (Nichol et al., Citation2022a) and the potential to improve quality of life and wellbeing via online social connection through peer support groups (Pitt et al., Citation2019). However, many clinicians lack confidence in training and supporting people with aphasia to access technology (Nichol et al., Citation2022b), and therefore more specialised training and support may be needed. In the current study, people with aphasia were able to participate using videoconferencing technology following a brief preparation session and were satisfied with use of this platform. This suggests that training people with aphasia to engage in technology can enable successful participation in activities including research.
Finally, significant others prioritised the recommendation that aphasia services should be person and family centred, emphasising that people with aphasia and their families should be involved in all stages of rehabilitation and should have access to personalised communication resources. Person-and family-centred care is recommended in speech-language therapy practise (Meyer et al., Citation2019) and healthcare more broadly (World Health Organization, Citation2007), however family members are often insufficiently involved (Sherratt et al., Citation2011; Haley et al., Citation2019). Although it may be perceived that the concept of person-and family-centred care is already included within the existing Aphasia United Best Practice Recommendations (see recommendations 5 and 7), the identification of this additional recommendation shows that person-and family-centred care should stand alone and thus be more visible.
Strengths, limitations, and future research
This study enhances current best practice recommendations for aphasia healthcare by adding the voices of those with lived experience of aphasia. Additionally, this is the first study to use the nominal group technique via Zoom with people with aphasia. People with aphasia and their significant others were satisfied with their involvement using this platform and its application for research. A limitation of the current study was the small sample size, the inclusion of only English-speaking Australian participants, as well as that no First Nations Australians were able to be recruited. While advice was received on how best to involve First Nations people in this research, our recruitment pathways were not effective in reaching this population. Efforts are needed to strengthen relationships and connections with First Nations people living with aphasia. Most participants with aphasia were from major cities and had mild-moderate aphasia, and we acknowledge that this may impact the relevance of findings to people with severe aphasia or those living in regional or remote areas. While best efforts were made to support the inclusion of participants in online focus groups (through technology training) some participants without ready internet access may have been deterred from participating. International data collection for the exploration of Aphasia United’s Best Practice Recommendations from consumers’ perspectives, involving participants with diverse cultural and linguistic backgrounds, is warranted to compare the findings of this study to participants from other cultural and linguistic backgrounds, and is currently underway. Upcoming research conducted by members of this team will combine the perspectives of people with lived experience with an updated systematic review of empirical research (Burton et al., Citation2023) and establish consensus on indicators of best practice aphasia services using a multi-stakeholder consensus process.
Conclusion
People with aphasia and their significant others found the Aphasia United Best Practice Recommendations to be relevant, but not always comprehensible or comprehensive. Participants extended the current 10 recommendations by adding prioritised statements regarding the need for: a coordinated, comprehensive, consistent approach to care; psychological and social support; more information about prognosis and recovery; and greater awareness of aphasia. The perspectives of people with lived experience of aphasia will be combined with evidence from an updated systematic review of clinical practice guidelines for post-stroke aphasia and revised using a future multi-stakeholder consensus process.
Acknowledgements
The authors thank participants with aphasia and their significant others for their invaluable contributions to this research and acknowledge funding and support from the Centre for Research Excellence in Aphasia Rehabilitation and Recovery (Aphasia CRE).
Disclosure statement
Authors LW and NSM led the development of the Aphasia United Best Practice Recommendations. Authors LW, NSM, SJW have served as executive committee members for Aphasia United. The remaining authors report no conflicts of interest.
Additional information
Funding
References
- Andrews, J., Guyatt, G., Oxman, A. D., Alderson, P., Dahm, P., Falck-Ytter, Y., Nasser, M., Meerpohl, J., Post, P. N., Kunz, R., Brozek, J., Vist, G., Rind, D., Akl, E. A., & Schünemann, H. J. (2013). GRADE guidelines: 14. Going from evidence to recommendations: The significance and presentation of recommendations. Journal of Clinical Epidemiology, 66(7), 719–725. https://doi.org/10.1016/j.jclinepi.2012.03.013
- Armstrong, M. J., Mullins, C. D., Gronseth, G. S., & Gagliardi, A. R. (2018). Impact of patient involvement on clinical practice guideline development: A parallel group study. Implementation Science, 13(1), 55.
- Australian Commission on Safety and Quality in Health Care. (2011). Patient centred care: Improving quality and safety through partnership with patients and consumers.
- Baker, C., Rose, M. L., Ryan, B., & Worrall, L. (2021). Barriers and facilitators to implementing stepped psychological care for people with aphasia: Perspectives of stroke health professionals. Topics in Stroke Rehabilitation, 28(8), 581–593. https://doi.org/10.1080/10749357.2020.1849952
- Baker, C., Worrall, L., Rose, M., Hudson, K., Ryan, B., & O’Byrne, L. (2018). A systematic review of rehabilitation interventions to prevent and treat depression in post-stroke aphasia. Disability and Rehabilitation, 40(16), 1870–1892. https://doi.org/10.1080/09638288.2017.1315181
- Baker, C., Worrall, L., Rose, M., & Ryan, B. (2020). ‘It was really dark’: the experiences and preferences of people with aphasia to manage mood changes and depression. Aphasiology, 34(1), 19–46. https://doi.org/10.1080/02687038.2019.1673304
- Burton, B., Isaacs, M., Brogan, E., Shrubsole, K., Kilkenny, M. F., Power, E., Godecke, E., Cadilhac, D. A., Copland, D., & Wallace, S. J. (2023). An updated systematic review of stroke clinical practice guidelines to inform aphasia management. International Journal of Stroke. https://doi.org/10.1177/17474930231161454
- Cabana, M. D., Rand, C. S., Powe, N. R., Wu, A. W., Wilson, M. H., Abboud, P. A. C., & Rubin, H. R. (1999). Why don’t physicians follow clinical practice guidelines?: A framework for improvement. JAMA, 282(15), 1458–1465.
- Cheng, B. B. Y., Ryan, B. J., Copland, D. A & Wallace, S. J. (2021). Prognostication in post-stroke aphasia: Speech pathologists’ clinical insights on formulating and delivering information about recovery. Disability and Rehabilitation, 1–14. https://doi.org/10.1080/09638288.2021.1922514
- Cheng, B. B. Y., Ryan, B. J., Copland, D. A. and Wallace, S.J. (2022a).Prognostication in post-stroke aphasia: Perspectives of people with aphasia on receiving information about recovery. Neuropsychological Rehabilitation, 1–32. https://doi.org/10.1080/09602011.2022.2051565
- Cheng, B. B. Y., Ryan, B. J., Copland, D. A & Wallace, S. J. (2022b). Prognostication in poststroke aphasia: perspectives of significant others of people with aphasia on receiving information about recovery. American Journal of Speech-Language Pathology, 31(2), 1–16. https://doi.org/10.1044/2021_AJSLP-21-00170
- Code, C., Papathanasiou, I., Rubio-Bruno, S., Cabana Mde, L., Villanueva, M. M., Haaland-Johansen, L., Prizl-Jakovac, T., Leko, A., Zemva, N., Patterson, R., Berry, R., Rochon, E., Leonard, C., & Robert, A. (2016). International patterns of the public awareness of aphasia. International Journal of Language Communication Disorder, 51(3), 276–284. https://doi.org/10.1111/1460-6984.12204
- Zoom Video Communications. (2020). Zoom (Version 5.0.5) [Computer software]. https://zoom.us/
- Dalemans, R., Wade, D. T., van den Heuvel, W. J., & de Witte, L. P. (2009). Facilitating the participation of people with aphasia in research: A description of strategies. Clinical Rehabilitation, 23(10), 948–959. https://doi.org/10.1177/0269215509337197
- Delbecq, A. L., Van de Ven, A. H., & Gustafson, D. H. (1975). Group techniques for program planning: A guide to nominal group and Delphi processes. Scott, Foresman and Co.
- Donnellan, C., Sweetman, S., & Shelley, E. (2013). Health professionals’ adherence to stroke clinical guidelines: A review of the literature. Health Policy (Amsterdam), 111(3), 245–263.
- El-Helou, R., Ryan, B., & Kneebone, I. (2023). Development of the “Kalmer” relaxation intervention: co-design with stroke survivors with aphasia. Disability and Hadley
- Stroke Foundation. (2020). National stroke audit: Rehabilitation services report 2020. https//informme.org.au/stroke-data/Rehabilitation-audits
- Gallacher, K., Morrison, D., Jani, B., Macdonald, S., May, C. R., Montori, V. M., Erwin, P. J., Batty, G. D., Eton, D. T., Langhorne, P., & Mair, F. S. (2013). Uncovering treatment burden as a key concept for stroke care: A systematic review of qualitative research. PLoS Med, 10(6), e1001473. https://doi.org/10.1371/journal.pmed.1001473
- Goodglass, H., Kaplan, E., & Barresi, B. (2001). The Assessment of Aphasia and Related Disorders. Lippincott Williams & Wilkins.
- Graneheim, U. H. & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. https://doi.org/10.1097/TLD.0000000000000176
- Grimshaw, J., & Russell, I. (1993). Achieving health gain through clinical guidelines: Developing scientifically valid guidelines. Quality in Health Care, 2(4), 243–248. https://doi.org/10.1136/qshc.2.4.243
- Hadely, K. A., Power, E., & O’Halloran, R. (2014). Speech pathologists’ experiences with stroke clinical practice guidelines and the barriers and facilitators influencing their use: a national descriptive study. BMC Health Services Research, 14(1), 110.
- Haley, K. L., Womack, J. L., Harmon, T. G., McCulloch, K. L., & Faldowski, R. A. (2019). Life activity choices by people with aphasia: repeated interviews and proxy agreement. Aphasiology, 33(6), 710–730.
- Harvey, N., & Holmes, C. A. (2012). Nominal group technique: An effective method for obtaining group consensus. International Journal of Nursing Practice, 18(2), 188–194. https://doi.org/10.1111/j.1440-172X.2012.02017.x
- Hilari, K., Behn, N., James, K., Northcott, S., Marshall, J., Thomas, S., Simpson, A., Moss, B., Flood, C., McVicker, S., & Goldsmith, K. (2021). Supporting wellbeing through peer-befriending (SUPERB) for people with aphasia: A feasibility randomised controlled trial. Clinical Rehabilitation, 35(8), 1151–1163. https://doi.org/10.1177/0269215521995671
- Hilari, K., & Northcott, S. (2017). “Struggling to stay connected”: comparing the social relationships of healthy older people and people with stroke and aphasia. Aphasiology, 31(6), 674–687. https://doi.org/10.1080/02687038.2016.1218436
- hRehabilitation, 45(9), 1517–1529. https://doi.org/10.1080/09638288.2022.2069294
- Hubbard, I. J., Harris, D., Kilkenny, M. F., Faux, S. G., Pollack, M. R., & Cadilhac, D. A. (2012). Adherence to clinical guidelines improves patient outcomes in Australian audit of stroke rehabilitation practice. Archives of Physical Medicine and Rehabilitation, 93(6), 965–971. https://doi.org/10.1016/j.apmr.2012.01.011
- Institute of Medicine. (2011). Clinical practice guidelines we can trust. Washington, DC: National Academies Press.
- Iwasaki, N., Ryan, B., Worrall, L., Rose, M., & Baker, C. (2023). Experiences of mood changes and preferences for management within stepped psychological care from the perspective of spouses of people with aphasia. Aphasiology, 37(2), 330–361. https://doi.org/10.1080/02687038.2021.2015746
- Kagan, A., & Kimelman, M. D. (1995). Informed consent in aphasia research: Myth or reality. Clinical Aphasiology, 23, 65–75.
- Kelly, H., Kennedy, F., Britton, H., McGuire, G., & Law, J. (2016). Narrowing the “digital divide”—facilitating access to computer technology to enhance the lives of those with aphasia: a feasibility study. Aphasiology, 30(2–3), 133–163. https://doi.org/10.1080/02687038.2015.1077926
- Kincheloe, H., Off, C., Murphy, M., Griffin-Musick, J., Murray, K., & Jakober, D. (2023). “We all have coping and communication problems”. Experiences of stroke survivors living with aphasia and graduate student clinicians who participated in a telehealth interprofessional psychoeducation and wellness group Aphasiology 37(3), 408–431. https://doi.org/10.1080/02687038.2021.2020716
- Kneebone, I. I. (2016). Stepped psychological care after stroke. Disability and Rehabilitation, 38(18), 1836–1843. https://doi.org/10.3109/09638288.2015.1107764
- Lohr, K. N., & Field, M. J. (1992). Guidelines for clinical practice: From development to use. National Academies Press.
- Manning, M., MacFarlane, A., Hickey, A., & Franklin, S. (2019). Perspectives of people with aphasia post-stroke towards personal recovery and living successfully: A systematic review and thematic synthesis. PLoS One, 14(3), e0214200. https://doi.org/10.1371/journal.pone.0214200
- McMillan, S. S., Kelly, F., Sav, A., Kendall, E., King, M. A., Whitty, J. A., & Wheeler, A. J. (2014). Using the nominal group technique: how to analyse across multiple groups. Health Services and Outcomes Research Methodology, 14(3), 92–108.
- Meyer, C., Scarinci, N., and Hickson, L. (2019). Patient and Family-Centered Speech-Language Pathology and Audiology. New York, NY, United States:Thieme Verlag. https://doi.org/10.1055/b/006/161149
- Morris, R., Eccles, A., Ryan, B., & Kneebone, I. I. (2017). Prevalence of anxiety in people with aphasia after stroke. Aphasiology, 31(12), 1410–1415. https://doi.org/10.1080/02687038.2017.1304633
- Munce, S. E. P., Graham, I. D., Salbach, N. M., Jaglal, S. B., Richards, C. L., Eng, J. J., Desrosiers, J., MacKay-Lyons, M., Wood-Dauphinee, S., Korner-Bitensky, N., Mayo, N. E., Teasell, R. W., Zwarenstein, M., Mokry, J., Black, S., & Bayley, M. T. (2017). Perspectives of health care professionals on the facilitators and barriers to the implementation of a stroke rehabilitation guidelines cluster randomized controlled trial. BMC Health Services Research, 17(1), 440. https://doi.org/10.1186/s12913-017-2389-7
- Nichol, L., Pitt, R., Wallace, S. J., Rodriguez, A. D., & Hill, A. J. (2022b). “There are endless areas that they can use it for”: speech-language pathologist perspectives of technology support for aphasia self-management. Disability and Rehabilitation: Assistive Technology, 1–16. https://doi.org/10.1080/17483107.2022.2037758
- Nichol, L., Wallace, S. J., Pitt, R., Rodriguez, A. D., Diong, Z. Z., & Hill, A. J. (2022a). People with aphasia share their views on self-management and the role of technology to support self-management of aphasia. Disability and Rehabilitation, 44(24), 7399–7412. https://doi.org/10.1080/09638288.2021.1989501
- Northcott, S., Simpson, A., Moss, B., Ahmed, N., & Hilari, K. (2017). How do speech-and-language therapists address the psychosocial well-being of people with aphasia? Results of a UK online survey. International Journal of Language and Communication Disorders, 52(3), 356–373. https://doi.org/10.1111/1460-6984.12278
- Northcott, S., Thomas, S., James, K., Simpson, A., Hirani, S., Barnard, R., & Hilari, K. (2021). Solution Focused Brief Therapy in Post-Stroke Aphasia (SOFIA): feasibility and acceptability results of a feasibility randomised wait-list controlled trial. BMJ Open, 11(8), e050308–e050308. https://doi.org/10.1136/bmjopen-2021-050308
- World Health Organization. (2007). People-centred health care: A policy framework. Manila: WHO Regional Office for the Western Pacific.
- Pettigrove, K., Lanyon, L. E., Attard, M. C., Vuong, G., & Rose, M. L. (2022). Characteristics and impacts of community aphasia group facilitation: A systematic scoping review. Disability and Rehabilitation, 44(22), 6884–6898. https://doi.org/10.1080/09638288.2021.1971307
- Pitt, R., Theodoros, D., Hill, A., Russell, T. (2019). The impact of the telerehabilitation group aphasia intervention and networking programme on communication, participation, and quality of life in people with aphasia. International Journal of Speech-Language Pathology, 21(5), 513–523.
- Porter, M. E., & Lee, T. H. (2013). The strategy that will fix health care. Harvard Business Review, 91(12), 24–24.
- Rohde, A., Worrall, L., & Le Dorze, G. (2013). Systematic review of the quality of clinical guidelines for aphasia in stroke management. Journal of Evaluation in Clinical Practice, 19(6), 994–1003.
- Rose, T. A., Worrall, L. E., Hickson, L. M., & Hoffmann, T. C. (2011). Aphasia friendly written health information: content and design characteristics. International Journal Speech Language Pathology, 13(4), 335–347. https://doi.org/10.3109/17549507.2011.560396
- Rose, T. A., Worrall, L. E., Hickson, L. M., & Hoffmann, T. C. (2012). Guiding principles for printed education materials: design preferences of people with aphasia. International Journal Speech Language Pathology, 14(1), 11–23. https://doi.org/10.3109/17549507.2011.631583
- Rose, T., Worrall, L., & McKenna, K. (2003). The effectiveness of aphasia‐friendly principles for printed health education materials for people with aphasia following stroke. Aphasiology, 17(10), 947–963. https://doi.org/10.1080/02687030344000319
- Ryan, B. J., Clunne, S. M., Baker, C. J., Shiggins, C., Rose, M. L., & Kneebone, I. I. (2022). A systematic review of non-drug interventions to prevent and treat anxiety in people with aphasia after stroke. Disability and Rehabilitation, 44(18), 4997–5006. https://doi.org/10.1080/09638288.2021.1925752
- Schindel, D., Mandl, L., Schilling, R., Meisel, A., Schenk, L. (2022). Guideline adherence in speech and language therapy in stroke aftercare. A health insurance claims data analysis. PLoS One, 17(2). https://doi.org/10.1371/journal.pone.0263397
- Sekhon, J. K., Oates, J., Kneebone, I., & Rose, M. L. (2022). A phase II randomised controlled trial evaluating the feasibility and preliminary efficacy of an education program on speech-language pathologist’ self-efficacy, and self-rated competency for counselling to support psychological wellbeing in people with post-stroke aphasia . Topics in Stroke Rehabilitation, ahead-of-print (ahead-of-print), 1–23. https://doi.org/10.1080/10749357.2022.2145736
- Selva, A., Sanabria, A. J., Pequeño, S., Zhang, Y., Solà, I., Pardo-Hernandez, H., Selva, C., Schünemann, H., & Alonso-Coello, P. (2017). Incorporating patients’ views in guideline development: a systematic review of guidance documents. Journal of Clinical Epidemiology, 88, 102–112. https://doi.org/10.1016/j.jclinepi.2017.05.018
- Sentinel Stroke National Audit Programme. (2019). Acute organisational audit report December 2019 https://www.strokeaudit.org/Documents/National/AcuteOrg/2019/2019-AOANationalReport.aspx
- Sherratt, S., Worrall, L., Pearson, C., Howe, T., Hersh, D., & Davidson, B. (2011). “Well it has to be language-related”: Speech-language pathologists’ goals for people with aphasia and their families. International Journal of Speech Language Patholology, 13(4), 317–328. https://doi.org/10.3109/17549507.2011.584632
- Shrubsole, K., Worrall, L., Power, E., & O’Connor, D. A. (2016). Recommendations for post-stroke aphasia rehabilitation: An updated systematic review and evaluation of clinical practice guidelines. Aphasiology, 31(1), 1–24. https://doi.org/10.1080/02687038.2016.1143083
- Simmons-Mackie, N., Worrall, L., Murray, L. L., Enderby, P., Rose, M. L., Paek, E. J., & Klippi, A. (2016). The top ten: Best practice recommendations for aphasia. Aphasiology, 31(2), 131–151. https://doi.org/10.1080/02687038.2016.1180662
- Thomas, S. A., Drummond, A. E., Lincoln, N. B., Palmer, R. L., das Nair, R., Latimer, N. R., Hackney, G. L., Mandefield, L., Walters, S. J., Hatton, R. D., Cooper, C. L., Chater, T. F., England, T. J., Callaghan, P., Coates, E., Sutherland, K. E., Eshtan, S. J., & Topcu, G. (2019). Behavioural activation therapy for post-stroke depression: The BEADS feasibility RCT. Health Technology Assessment, 23(47), 1–176. https://doi.org/10.3310/hta23470
- United States Department of Health and Human Services. (2008). Personalized health care: Pioneers, partnerships, progress.
- van Rijssen, M. N., Veldkamp, M., Bryon, E., Remijn, L., Visser-Meily, J. M. A., Gerrits, E., & van Ewijk, L. (2022). How do healthcare professionals experience communication with people with aphasia and what content should communication partner training entail?. Disability and Rehabilitation, 44(14), 3671–3678. https://doi.org/10.1080/09638288.2021.1878561
- Wallace, S. J., Isaacs, M., Ali, M., & Brady, M. C. (2023). Establishing reporting standards for participant characteristics in post-stroke aphasia research: An international e-Delphi exercise and consensus meeting. Clinical Rehabilitation, 37(2), 199–214. https://doi.org/10.1177/02692155221131241
- Wallace, S. J., Worrall, L., Rose, T., Le Dorze, G., Cruice, M., Isaksen, J., Kong, A. P. H., Simmons-Mackie, N., Scarinci, N., & Gauvreau, C. A. (2017). Which outcomes are most important to people with aphasia and their families? An international nominal group technique study framed within the ICF. Disability and Rehabilitation, 39(14), 1364–1379. https://doi.org/10.1080/09638288.2016.1194899
- World Health Organisation. (2000). The world health report 2000- Health systems: improving performance. https://www.who.int/whr/2000/en/
- Worrall, L., Simmons-Mackie, N., Wallace, S. J., Rose, T., Brady, M. C., Kong, A. P., Murray, L., & Hallowell, B. (2016). Let’s call it “aphasia”: Rationales for eliminating the term “dysphasia”. International Journal of Stroke, 11(8), 848–851. https://doi.org/10.1177/1747493016654487
- Zanella, C., Laures-Gore, J., Dotson, V. M., & Belagaje, S. R. (2023). Incidence of post-stroke depression symptoms and potential risk factors in adults with aphasia in a comprehensive stroke center. Topics in Stroke Rehabilitation, 30(5), 448–458. https://doi.org/10.1080/10749357.2022.2070363