Abstract
Introduction. The purpose of this study was to investigate long term outcome for women who had undergone mastectomy and immediate breast reconstruction. Material and methods. Patient files of 167 immediately reconstructed breast cancer patients were reviewed for late surgical complications. Furthermore, information of local recurrence rate, radiotherapy and death was obtained from the Danish Breast Cancer Cooperative Group register. Histopatological high and low risk patients were compared with respect to locoregional recurrence rate, recurrence free survival and death. Unpaired t-test and Fisher's exact test were used to test for significance. Results. The overall rate of revision surgery was 27%. Reconstruction with implants was associated with a significantly higher rate of revision surgery compared to reconstructions with transverse rectus abdominis myocutaneous flap or latissimus dorsi flap without implant (36 vs. 14%; p=0.004). The locoregional recurrence rate was 6%. Patients with histopathologically high risk disease had increased death rate (22 vs. 6%; p=0.03) and shorter disease free survival (89±43 months vs. 104±35 months; p=0.048) compared with low risk disease. We found no increase in the occurrence of capsular contracture in our study group in patients who received radiotherapy. Conclusion. Immediate breast reconstruction seems to be oncologically safe. Breast reconstruction performed with implants was associated with a higher risk of late complications, as was histopathologically high risk disease with increased death rate and shorter disease free survival.
Today breast reconstruction is considered an integrated part of the rehabilitation after mastectomy. Skin sparing mastectomy and immediate breast reconstruction have advantages compared to secondary breast reconstruction. It is to a greater extent possible to preserve the inframammary fold and to adjust the placement of the scar, in order to achieve the most aesthetic result Citation[1], Citation[2]. Immediate breast reconstruction reduces the overall cost compared to delayed reconstruction Citation[3]. Furthermore it has been shown to have psychological advantages for the patients Citation[4].
We have in accordance with the literature Citation[5] previously shown that immediate breast reconstruction could be done with an acceptable rate of postoperative complications and morbidity and that the adjuvant oncologic treatment could be given without significant delay Citation[6].
The local recurrence rate for patients who have undergone immediate breast reconstruction with locally advanced breast cancer has been found acceptable in several investigations Citation[3], Citation[7–15].
The aim of this study was to evaluate the long-term outcome for patients, who had undergone immediate breast reconstruction after mastectomy, using three different reconstructive procedures.
Material and methods
Patient files were reviewed for 167 patients who had an immediate breast reconstruction performed at Rigshospitalet, Copenhagen in the period between 1994 and 2001. Twenty-six patients (16%) had bilateral surgery performed, so that a total of 193 cases of mastectomy and immediate reconstruction were carried out. In 115 of the cases (60%), the indication was invasive cancer, in 57 of the cases (30%), the indication was a premalignant condition, and in the remaining 21 cases (11%), the mastectomy was performed as a prophylactic measure. Twenty-two patients (13%) were lost for follow-up, the remaining 145 patients were included in the study, and of these, 23 (16%) had bilateral surgery performed, leaving a total of 168 included mastectomies. Of these, 115 (68%) were invasive cancers and their characteristics are presented in . Mean follow-up was 34±30 months (range 3–130 months).
Table I. Characteristics of invasive cancers.
Patient files were examined for incidences of late complications, defined as indication for revision surgery because of capsular contracture, implant displacement, scar revision, implant rupture, fat necrosis, or other complications. Capsular contracture was determined by clinical judgement according to the Baker scale and only revision demanding class 3–4 contractures were registered. Fat necrosis was diagnosed by palpation in combination with ultrasonography. Additionally, information about local recurrence, death and radiotherapy was obtained from the Danish Breast Cancer Cooperative Group (DBCG) register. The DBCG was initiated in 1977 and designed primarily to provide guidelines for treatment of breast cancer patients, to conduct nationwide trials of adjuvant therapy, and to evaluate treatment programmes Citation[16]. Results regarding recurrence and death apply to all patients from the study group who were registered in the DBCG register, regardless of they were lost for follow-up in the patient file study.
Operative procedures
All patients underwent a skin sparing mastectomy. Before surgery, the inframammary fold and planned incision lines were marked on the patient. In cases of reconstruction with expander, the size of the expander was decided on basis of the width of the breasts. Method of reconstruction was chosen based on technical considerations and patient preferences. A reconstruction with a latissimus dorsi flap was performed when tumour size or location hindered expansion and the amount of lower abdominal tissue was inadequate for a TRAM-flap. Whether the latissimus dorsi flap reconstruction was performed with or without an implant depended on the planned size of the reconstructed breast. Operations were performed in cooperation between breast surgeons and plastic surgeons.
Breast reconstruction with expander and implant
After completed mastectomy, an anatomical expander (McGhan Ltd., Arklow, Ireland or Mentor Medical Systems, Leiden, The Netherlands) was placed under the pectoralis major and the serratus anterior muscle. The expansion was started two weeks after surgery and continued weekly until the expansion was approximately 25% larger than the planned permanent implant. The change of the expander to the silicone implant (McGhan Ltd. or Mentor Medical Systems) was performed 2 months after finished expansion.
Breast reconstruction with latissimus dorsi flap with or without implant
The latissimus dorsi flap was raised based on its neurovascular pedicle. The flap was transposed anteriorly into the mastectomy wound and the new breast was created. In some cases, an implant (McGhan Ltd. or Mentor Medical Systems) was placed under the flap.
Breast reconstruction with transverse rectus abdominis myocutaneous flap (TRAM-flap)
The plastic surgeon prepared the TRAM-flap at the same time as the breast surgeon performed the mastectomy. The flap was based on the inferior epigastric vessels and transplanted to the mastectomy wound as a free flap a and b. The thoracodorsal artery and vein in the axilla were used as recipient vessels.
Data analysis
Data were analyzed using the SPSS statistical analysis program version 13.0 (SPSS Inc., Chicago, Illinois). When comparing high and low risk patients with respect to recurrence free survival, unpaired t-test was used. When comparing high and low risk patients with respect to recurrence and death rate, radiotherapy and incidence of capsular contracture, and implant versus no implant with respect to rate of revision surgery, Fisher's exact test was used. Data are presented as mean±SD for descriptive data.
Results
Mean age was 48.1±8.6 years. An immediate reconstruction with expander and implant was performed in 82 of the patients (57%), latissimus dorsi flap without implant was performed in 26 patients (18%), latissimus dorsi flap with implant was performed in 4 cases (3%) andTRAM-flap was performed in 33 cases (23%).
The incidences of late complications in the different reconstructive methods are shown in .
Table II. Incidences of late complications in the different reconstructive methods.
In implant reconstructions after expansion, 19 patients (23%) had revision surgery performed once because of late complications, and in 9 patients (11%) more than one revision was performed. The most frequent indication for revision surgery was capsular contracture, which occurred in 14 patients (17%). In nine patients (11%), the indications for revision were unsuccessful result, late infection or lack of acceptance of the implant by the patient. Four patients (5%) had scar revision performed and implant displacement occurred in one patient.
Revision surgery after breast reconstruction with a latissimus dorsi flap or a TRAM flap was performed for scar revision in 7 patients (12%). One patient with a latissimus dorsi flap with implant had a capsular contracture, one patient had displacement of the implant, and one patient had displacement of the filling valve in a Becker implant.
Overall, 39 patients (27%) had one or more revisions due to late complications. Patients who had an implant (including latissimus dorsi flap with implant) underwent revision surgery significantly more often than patients with breast reconstructions with flaps alone (36 vs. 14%; p = 0.004).
Radiotherapy
Information about radiotherapy was present in the DBCG register for 91 (79%) of the patients with invasive cancer. Of these, 24 patients (26%) were treated with radiotherapy and 67 patients (74%) did not receive radiotherapy. Of patients who received radiotherapy, 3 (13%; CI 3–32%) developed capsular contracture and of patients who did not receive radiotherapy, 8 (12%; CI 5–22%) developed capsular contracture (NS).
Recurrence
Information about locoregional recurrence was present in the DBCG register for 100 (87%) of the patients with invasive cancer. Four patients (13%; CI 4–29%) with high risk invasive breast cancer, defined as positive axillary lymph nodes or primary tumour size > 50 mm, had local recurrence as opposed to two patients (3%; CI 0–10%) with low risk invasive cancer (; NS). Overall, a local recurrence rate of 6% (CI 2–13%) was found with a mean follow-up period of 108±26 months (range 66–164 months).
Figure 1. Fifty years old female with invasive cancer in the right breast before (a) mastectomy and after (b) mastectomy and immediate breast reconstruction with a TRAM flap. The left breast has been corrected.
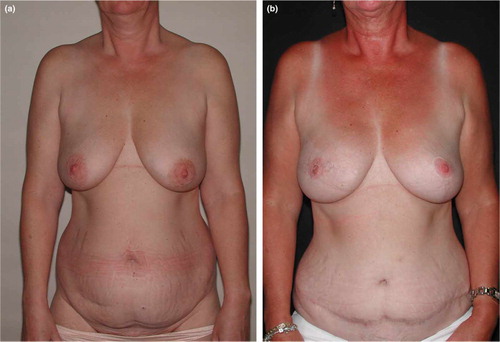
Table III. Locoregional recurrence rate, death rate and disease free survival for patients with invasive cancer.
Death
Information about survival was present in the DBCG register for 104 (90%) of the patients with invasive cancer. Seven patients (22%; CI 9–40%) with high risk invasive breast cancer were registered as dead in the DBCG register as apposed to four patients (6%; CI 2–14%) with low risk invasive cancer (; p=0.032).
Disease free survival
Mean disease free survival was 89±43 months and 104±35 months for high and low risk patients, respectively (; p = 0.048).
Discussion
Immediate breast reconstruction is now a widely accepted method for breast reconstruction after mastectomy. It has an acceptable rate of postoperative complications and is considered oncologically safe Citation[6] with local recurrence rates from 2–10% Citation[7], Citation[8], Citation[10–13], Citation[15]. Hence, the total locoregional recurrence rate for patients with invasive cancer of 6% found by us mirrors the literature well.
Only patients with clinically low risk disease were offered immediate reconstruction. Yet, almost one third of the patients were subsequently categorized as having high-risk disease at histopathologic investigation. This relatively large amount of patients with histopathologically high risk disease compared to what was expected from the clinical evaluation was considered to be a problem at the time, and our findings of a more than four fold higher recurrence rate in high risk compared to low risk disease support this concern. The difference, however, was not significant (p = 0.08) but this could very likely be a statistical type II error due to the small number of incidences of recurrence. With the implementation of the sentinel node technique, it is now much more achievable to avoid patients with high-risk disease as candidates for immediate reconstruction.
We found the rate of revision surgery to be 27%. Reconstructions with implants were associated with a significantly higher rate of late complications, requiring re-operation, compared with reconstructions without implant. Other studies also found a higher risk of late complications after reconstructions with implants versus reconstructions with flaps Citation[7], Citation[13], Citation[17].
Radiotherapy after mastectomy is increasingly being used in patients with early breast cancer Citation[18]. However, a concern could be raised regarding possible negative effects of the radiotherapy on the long term outcome after breast reconstruction. Indeed, higher incidences of capsular contracture have been found after immediate breast reconstruction in patients who also received radiotherapy Citation[13], Citation[19]. We found no increase in the occurrence of capsular contracture in our study group in patients who received radiotherapy. However, this may very well be due to the relatively small number of capsular contractures.
In conclusion, our results are in accordance with the international literature saying that immediate breast reconstruction seems oncologically safe. The risk of late complications is found to be higher in patients who have breast reconstructions performed with implants compared with autologous tissue.
References
- Elberg JJ, Blichert-Toft M, Drzewiecki KT. Primary breast reconstruction after mastectomy for breast cancer]. Ugeskr Laeger 1995; 157: 1013–6
- Kroll SS, Marchi M. Immediate reconstruction: Current status in cancer management. Tex Med 1991; 87: 67–72
- Huang CJ, Hou MF, Lin SD, Chuang HY, Huang MY, Fu OY, et al. Comparison of local recurrence and distant metastases between breast cancer patients after postmastectomy radiotherapy with and without immediate TRAM flap reconstruction. Plast Reconstr Surg 2006; 118: 1079–86
- Eberlein TJ, Crespo LD, Smith BL, Hergrueter CA, Douville L, Eriksson E. Prospective evaluation of immediate reconstruction after mastectomy. Ann Surg 1993; 218: 29–36
- Malata CM, McIntosh SA, Purushotham AD. Immediate breast reconstruction after mastectomy for cancer. Br J Surg 2000; 87: 1455–72
- Elberg JJ, Mollerup CL, Dahlstrom KK, Ravnsbaek JD, Drzewiecki KT, Rank FE, et al. Primary breast reconstruction in connection with mastectomy for breast cancer. Indication, procedure and immediate surgical results]. Ugeskr Laeger 2000; 162: 2550–3
- Carlson GW, Losken A, Moore B, Thornton J, Elliott M, Bolitho G, et al. Results of immediate breast reconstruction after skin-sparing mastectomy. Ann Plast Surg 2001; 46: 222–8
- Foster RD, Esserman LJ, Anthony JP, Hwang ES, Do H. Skin-sparing mastectomy and immediate breast reconstruction: A prospective cohort study for the treatment of advanced stages of breast carcinoma. Ann Surg Oncol 2002; 9: 462–6
- Gherardini G, Thomas R, Basoccu G, Zaccheddu R, Fortunato L, Cortino P, et al. Immediate breast reconstruction with the transverse rectus abdominis musculocutaneous flap after skin-sparing mastectomy. Int Surg 2001; 86: 246–51
- Howard MA, Polo K, Pusic AL, Cordeiro PG, Hidalgo DA, Mehrara B, et al. Breast cancer local recurrence after mastectomy and TRAM flap reconstruction: Incidence and treatment options. Plast Reconstr Surg 2006; 117: 1381–6
- Langstein HN, Cheng MH, Singletary SE, Robb GL, Hoy E, Smith TL, et al. Breast cancer recurrence after immediate reconstruction: Patterns and significance. Plast Reconstr Surg 2003; 111: 712–20
- Medina-Franco H, Vasconez LO, Fix RJ, Heslin MJ, Beenken SW, Bland KI, et al. Factors associated with local recurrence after skin-sparing mastectomy and immediate breast reconstruction for invasive breast cancer. Ann Surg 2002; 235: 814–9
- Newman LA, Kuerer HM, Hunt KK, Ames FC, Ross MI, Theriault R, et al. Feasibility of immediate breast reconstruction for locally advanced breast cancer. Ann Surg Oncol 1999; 6: 671–5
- Salhab M, Al SW, Joseph A, Sheards S, Travers J, Mokbel K. Skin-sparing mastectomy and immediate breast reconstruction: Patient satisfaction and clinical outcome. Int J Clin Oncol 2006; 11: 51–4
- Slavin SA, Schnitt SJ, Duda RB, Houlihan MJ, Koufman CN, Morris DJ, et al. Skin-sparing mastectomy and immediate reconstruction: Oncologic risks and aesthetic results in patients with early-stage breast cancer. Plast Reconstr Surg 1998; 102: 49–62
- Andersen KW, Mouridsen HT. Danish Breast Cancer Cooperative Group (DBCG]. A description of the register of the nation-wide programme for primary breast cancer. Acta Oncol 1988; 27: 627–47
- Kroll SS, Baldwin B. A comparison of outcomes using three different methods of breast reconstruction. Plast Reconstr Surg 1992; 90: 455–62
- Pierce LJ. Postmastectomy radiotherapy: Future directions. Semin Radiat Oncol 1999; 9: 300–4
- Ringberg A, Tengrup I, Aspegren K, Palmer B. Immediate breast reconstruction after mastectomy for cancer. Eur J Surg Oncol 1999; 25: 470–6