To the Editor,
Creation of stoma is often an initial treatment for patients with low-lying symptomatic rectal cancer and never resectable synchronous distant metastases. However, a stoma impairs some quality of life aspects. We have therefore conducted a phase II trial to evaluate whether the palliative effect of radiotherapy and chemotherapy is sufficient to spare patients from palliative surgery. With short follow-up we previously reported favorable results [Citation1]. It is, however, unclear whether such outcomes are long-lasting. The presented analysis aims to address this issue.
Material and methods have been previously detailed elsewhere [Citation1]. The primary end-point was the rate of surgery performed for palliation of local symptoms that were uncontrolled by upfront short-course radiotherapy and chemotherapy. The secondary end-point was to evaluate the palliative effect of radio- and chemotherapy. The eligibility criteria included a previously untreated symptomatic primary rectal adenocarcinoma proven by pathological examination, synchronous distant metastases deemed never resectable and a lower border of the tumor located up to 10 cm from the anal verge. Five fractions of 5 Gy were given to the primary tumor and adjacent enlarged lymph nodes over five consecutive days. This schedule was chosen because of its similar local efficacy to long-course chemoradiation found in a preoperative setting [Citation2] and because full dose palliative chemotherapy can only be given with a short delay. Chemotherapy was postponed until nine days post-radiation to avoid overlapping toxicity. The protocol stipulated CAPOX administration. The evaluation of the palliative effect was based on self-administered questionnaires completed by patients every three months.
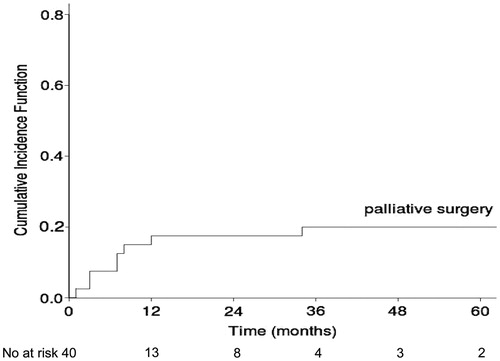
All 40 consecutive patients who met our entry criteria agreed to participate in the study. Patients’ characteristics, treatment details and early results have been detailed previously [Citation1]. None of the patients was lost to follow-up. Thirty-seven patients (93%) died. Three patients were living 54, 65 and 66 months post-radiotherapy. Of these, two had a favorable palliative effect without the need for palliative surgery. The median overall survival was 11.5 months. Eight patients (20%) had palliative surgery (seven stoma creation and one full-thickness local excision) because of local symptoms progression. In the subgroup of 15 patients with a near-obstructing lesion, three (23%) required stoma creation. None of these operations were emergent. The probability of palliative surgery at three years was 20% (95% CI 16–25%) (). Seven surgical procedures were performed within one-year post-radiotherapy. Palliative surgery was needed in only one of 13 patients who had survived for over one year without surgical intervention. The probability of a sustained favorable palliative effect at three years was 63% (95% CI 59–67%). An initially favorable local palliative effect worsened in three of the 13 patients who had survived for over one year with good palliation. Eleven patients (28%) reported complete symptom resolution and 14 (35%) reported significant resolution during the whole course of the follow-up. Fifteen patients (38%) had a poor palliative effect, eight of whom had palliative surgery. The lack of upfront surgery possibly led to death because of a massive hemorrhage in one patient and to suffering that preceded death in two others.
This study demonstrates that for most patients, even in those with a near-obstructing tumor, initial surgery may be avoided by using palliative radiotherapy and chemotherapy. The palliative effect, once sustained for one year, was most often long lasting (). Similar findings to those observed in the current investigation have been reported in the literature [Citation3–6]. The high effectiveness of 5 × 5 Gy and consolidation chemotherapy have also been observed in preoperative settings [Citation7–9]; indeed, a similar local efficacy and lower acute toxicity compared to conventionally fractionated chemoradiation have been observed in a randomized study [Citation9]. Symptoms’ response to 5 × 5 Gy and chemotherapy enables personalized treatment, i.e. avoiding surgery for radio(chemo)sensitive cancer. In this regard, the initial radiotherapy can be regarded as not only a treatment but also a selection test. The integral part of the method was to inform the patients that in cases where symptoms are not improved or if symptoms worsen, then surgical consultation is immediately required. Consequently, none of the rescue operations were emergent. The strength of our study is the absence of selection bias within our institution because all consecutive patients who were referred to our center and who met the entry criteria agreed to participate in the study. This supports the generalizability of our results and also indicates patients’ positive preferences for the proposed method. A weakness of our trial is however the lack of a control group.
In conclusion, our findings suggest that short-course radiotherapy is a valid option and can replace upfront palliative surgery even in patients with near-obstructing lesions. The local palliative effect was long lasting for most of the survivals over one year.
Funding information
The study was supported by grant No N N403 139939 from the Polish Ministry of Science and Higher Education.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Tyc-Szczepaniak D, Wyrwicz L, Kepka L, et al. Palliative radiotherapy and chemotherapy instead of surgery in symptomatic rectal cancer with synchronous unresectable metastases: a phase II study. Ann Oncol 2013;24:2829–34.
- Bujko K, Nowacki MP, Nasierowska-Guttmejer A, et al. Long-term results of randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br J Surg 2006;93:1215–23.
- Crane CH, Janjan NA, Abbruzzese JL, et al. Effective pelvic symptom control using initial chemoradiation without colostomy in metastatic rectal cancer. Int J Radiat Oncol Biol Phys 2001;49:107–16.
- Urdaneta-Lafee N, Kligerman MM, Knowlton AH. Evaluation of palliative irradiation in rectal carcinoma. Radiology 1972;104:673–7.
- Sargeant IR, Tobias JS, Blackman G, et al. Radiation enhancement of laser palliation for advanced rectal and rectosigmoid cancer: a pilot study. Gut 1993;34:958–62.
- Cameron MG, Kersten C, Vistad I, et al. Palliative pelvic radiotherapy of symptomatic incurable rectal cancer – a systematic review. Acta Oncol 2014;53:164–73.
- Radu C, Berglund A, Pahlman L, et al. Short course preoperative radiotherapy with delayed surgery in rectal cancer – a retrospective study. Radiother Oncol 2008;87:343–9.
- van Dijk TH, Tamas K, Beukema JC, et al. Evaluation of short-course radiotherapy followed by neoadjuvant bevacizumab, capecitabine, and oxaliplatin and subsequent radical surgical treatment in primary stage IV rectal cancer. Ann Oncol 2013;24:1762–9.
- Bujko K,L, Wyrwicz L, Rutkowski A, et al. Long-course oxaliplatin based preoperative chemoradiation vs. 5 x 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: results of a randomised phase III study. Ann Oncol 2016; pii: mdw062. [Epub ahead of print]. doi: 10.1093/annonc/mdw062.