Abstract
Background: Cervical cancer survivors treated with radiotherapy report vaginal inelasticity and decreased lubrication that may affect their sexual health, but it is unknown which normal tissue reactions mediate these symptoms. The aim of this study was to investigate the morphology of the connective tissue of the vaginal wall in cervical cancer survivors treated with radiotherapy.
Material and methods: We recruited 34 cervical cancer survivors treated with radiotherapy and 37 age-matched controls. Via clinical examination the degree of vaginal atrophy and pelvic fibrosis were estimated. We collected vaginal biopsies, which underwent morphometric analysis focused on elastin and collagen. Additionally, radiation dose at biopsy site were calculated and correlated to the clinical and morphological findings.
Results: The survivors had marked morphological vaginal changes, most prominent in the survivors that had received the highest radiation dose at the biopsy site. Mucosal atrophy was observed in 91% and pelvic fibrosis in 97%. A shorter vagina was measured; 7.0 cm versus 10.3 cm in controls (p < 0.001). The area fraction of elastin was greater in survivors; 10.0% (range 5.8–12.9), compared with controls; 3.4% (range 1.8–5.8), p < 0.001. The survivors had signs of elastosis with thick aggregated elastin fibers irregularly scattered throughout the connective tissue, while the controls had elastin fibers in a thin sub-epithelial layer. The area fraction of high density collagen in the connective tissue was larger among the survivors (p < 0.001). The collagen with the highest density (fibrosis) was more common in the group of cancer survivors that had received external radiation.
Conclusions: We found drastic differences in the vaginal wall between the irradiated cervical cancer survivors and the controls, indicating that radiotherapy-induced vaginal symptoms are mediated by connective tissue fibrosis and elastosis. Our results also support that patients treated with external radiation have the highest risk of developing vaginal fibrosis with impairment of their sexual health.
Women who have been treated for cervical cancer have persistent changes in their sexual function, which result in considerable distress [Citation1]. Advances in treatment of radiotherapy and additional chemotherapy have resulted in improvement in survival rates [Citation2]. The majority of new cervical cancer cases are diagnosed in young or middle-aged women. Therefore, a rising number of cervical cancer survivors are at risk for chronic side effects of the treatment.
In Sweden the incidence rate of cervical cancer has declined, but still around 450 new cases of cervical cancer are diagnosed every year. The therapy can include surgery, radiation, and chemotherapy depending on the stage at diagnosis. The radiotherapy, often combined with chemotherapy, is important for long-term survival in patients with advanced stages.
The late effect of radiotherapy on the surrounding pelvic structure, with morphological changes on bladder and intestine, are well known [Citation3]. Cervical cancer survivors report that the vaginal changes that decrease sexual health are one of the most distressful symptoms [Citation1]. Even so, the vaginal pathophysiological changes have received little attention and still the effects of radiotherapy on the vaginal epithelium and connective tissue are unknown.
The aim of the study was to investigate the morphology of the connective tissue of the vaginal wall in cervical cancer survivors treated with radiotherapy. Biopsies were investigated with focus on the amount and structure of elastin and collagen fibers. The morphological results and clinical observations were correlated to radiation dose at biopsy site.
Material and methods
Patients
Sixty-six cervical cancer survivors treated with radiotherapy were identified from the medical records at our oncological clinic, between 1 January 2004, and 31 December 2007. Inclusion criteria were a diagnosis of cervical cancer treated with radiotherapy and age ≤51 years (the mean age for menopause for Swedish women). The time from the end of treatment to participation in the study was from two to five years. Exclusion criteria were recurrence of cervical cancer and significant co-morbidity. As controls, 37 premenopausal women, aged ≤51 years undergoing benign gynecological surgery were recruited. Exclusion criteria for the controls were a history of cancer, current pregnancy, systemic disease, and vulvovaginal infections and/or inflammation. The study was approved by the Regional Research Ethics Committee at the Karolinska Institute (EPN Stockholm, Dnr 2003-753) and all the participants signed a written informed consent.
The standard treatment for cervical cancer, according to the regional guidelines at the time of the study, was for stage IA2-IB1 and small IIA tumors radical hysterectomy with lymphadenectomy (Piver type II) with or without preoperative intracavitary pulse dose rate (PDR) brachytherapy (BT) (38 Gy in 2 fractions). Patients with lymph node metastases or close surgical margins were typically treated with postoperative three-dimensional conformal chemoradiation (3D-CRT) [45 Gy external beam radiotherapy (EBRT) to a standard pelvic field and two vaginal (high dose rate) HDR-BT insertions, 10 Gy in two fractions, if not preoperative BT was given, and five concomitant courses of cisplatin]. For stage IB2 and more advanced disease, the standard treatment was definitive 3D-CRT 45 Gy to a pelvic field, an integrated external boost to the tumor to 50 Gy, 24 Gy PDR BT in 3 fractions, and six concomitant courses of cisplatin. In the case of co-morbidity or a low risk of disseminated spread, chemotherapy was excluded.
Clinical assessments
In 2009 and 2010 letters explaining the objectives of the study, were sent to the identified cervical cancer survivors inviting them to participate in the study. After one week a research nurse telephoned the women. Thirty-four survivors agreed to participate and were scheduled for a research visit. One gynecological oncologist (AH) performed the gynecological examinations. During the inspection, vaginal atrophy was graded as absent (normal mucosa), mild (slightly pale mucosa, reduced folding), moderate (moderately pale, reduced folding) or severe (pronounced pallor, absent folding). Pelvic fibrosis and grade of vaginal inelasticity were determined by palpation as absent, mild (restricted to vagina), moderate (vagina and parametria) or severe (vagina and pelvis; ‘frozen pelvis’). Vaginal length was measured by a vaginal measuring cylinder. One gynecologist (NBS) examined all the control women according to protocol.
Biopsies and laboratory studies
After a five-minute application of lidocaine/prilocaine cream (EMLA®, AstraZeneca, Sweden) two vaginal biopsies were taken from all the participants. The biopsies were taken with a 3 mm forceps at the three and nine o’clock positions, 3–4 cm from the vaginal introitus. The biopsies were placed in neutral buffered 4% formaldehyde solution for approximately 12 hours. Dehydration, fixation, and paraffin embedding were performed according to a standard protocol. From each block, 5 μm sections were cut perpendicularly to the surface. All biopsies and sections were handled and analyzed in a blinded manner throughout all the analyses (HJ).
The elastic fibers in the connective tissue were visualized by their autofluorescent properties in unstained sections in three images from each patient and control. The specimens were placed in the microscope (Axioplan 2, Zeiss) under a 40 × objective and three random-sampled images per section were captured, with a three-chip CCD RGB-color camera (Sony DXC-9100P). The images were digitized and stored in eight-bit RGB-mode in the computer under the control of MicroGOP 2000s (Context Vision) image analysis software. The image size was equal in all specimens. Finally, the image analysis program calculated the area fraction of the elastic fibers (in percent) in each slide by dividing the total elastic fiber area by the total tissue area of the three images [Citation4].
To analyze the collagen content in the tissue, sections were stained with Sirius red, which binds covalently to the collagen molecule and is thus highly specific. Thereafter, the density of the collagen fibers were measured by intensitometry, i.e., calculation of the intensity of light passing through the collagen in the sections using the same equipment as above, but programed for intensitometric measurements. The specimens were placed on a light table and the light was calibrated with a filter set of known densities. Optical density was estimated by detecting and measuring the area fraction for pixels in the specimen within certain defined gray level intervals, ranging from black = 0, to white = 255 (eight-bit gray level). Subsequently, the total intensity, obtained from each gray level interval, was compared with the total area of the section [Citation5,Citation6]. The collagen fibers were divided into four different panels (A–D) according to their optical densities, panel A representing the fibers with the highest density and panel D the fibers with the lowest density. For each participant three sections were evaluated and the result is presented as median percentage of total pixel area.
Radiation dose at biopsy site
The patients were treated before the use of 3D-guided BT. The EBRT plans were stored in an old planning system, and the plans could not be retrieved. We therefore collected the prescribed field margins, target definition, set-up images, portal image films, treatment protocol and dose per fraction, and the total prescribes dose for each patient. On portal image films the vaginal introitus was identified. The distance from the lower border of the EBRT field was measured and the EBRT dose at the biopsy site was calculated. For the BT we used orthogonal X-ray images and made an estimation of the delivered dose based on isodose curves from the actual treatment for each patient. We calculated the EQD2 doses for both the EBRT and the BT, and thus obtaining the total dose at the biopsy site.
In order to correlate radiotherapy-induced histological findings, the radiation dose at the biopsy site was calculated in three different treatment groups; (I) preoperative BT, (IIA) preoperative BT + EBRT and (IIB) primary radiochemotherapy.
Statistical analysis
Data was analyzed using IBM SPSS Statistics 22. Fisher’s exact test was used for comparing categorical variables between patients and controls. For analyzing median radiation dose between two or three treatment groups, Mann-Whitney U-test or Kruskal-Wallis test were used. Differences in median elastin and collagen content between patients and controls were analyzed with Mann-Whitney U-test. The significance level was set at p < 0.05.
Results
Of the 66 cervical cancer survivors who met the inclusion criteria, 34 agreed to participate in the study. The majority declined to come for an extra visit at the oncological clinic, due to psychological reasons. Age, stage, and treatment did not differ significantly between participants and non-participants. There was no difference between the survivors and controls in mean age. FIGO tumor stage, histology, and cancer treatment are shown in . The surgery performed was radical hysterectomy and pelvic lymph node extirpation (Piver type II), except for one patient with a history of occult cervical cancer. All patients received BT, either preoperative, during postoperative external beam radiotherapy or during primary radiochemotherapy (). Two-thirds of the patients received concomitant cisplatin. Hormonal treatments and the use of vaginal dilators are shown in .
Table 1. Demographics and clinical characteristics of cervical cancer survivors and controls.
Radiation dose at biopsy site
Five patients received preoperative BT only and received minimal radiation at the biopsy site (Group I). Patients treated with additional postoperative EBRT received median 44.3 Gy at the biopsy site (Group IIA), as compared to Group IIB, treated with primary radiochemotherapy, which received median 53.4 Gy (p < 0.001) (). For further analysis of clinical findings treatment Groups IIA and IIB are analyzed together, including patients that received a high radiation dose at the biopsy site ().
Table 2. Radiotherapy dose at the vaginal biopsy site in the cervical cancer survivors.
Table 3. Vaginal characteristics among all cervical cancer survivors and controls, and cancer survivors divided in two different treatment groups.
Clinical findings
The survivors had a shorter vagina, 7.0 cm (range 5.0–9.0), than the controls, 10.0 cm (range 7.0–13.0), p < 0.001. Ninety-one percent of the survivors had signs of different degrees of atrophy. Ninety-seven percent of the survivors had pelvic fibrosis, with reduced elasticity of the vagina and the pelvis both at speculum examination and palpation, the majority to a mild or moderate degree. The women in treatment Group II with a high radiation dose at biopsy site showed the most prominent changes in vaginal length, atrophy, and pelvic fibrosis (). No women in the control group had visible or palpable vaginal changes at examination. There was almost no bleeding when taking the biopsies in the survivor group but, in the control group there was expected bleeding, and in a few cases a stitch was needed for hemostasis. No other complications were observed.
Histological results
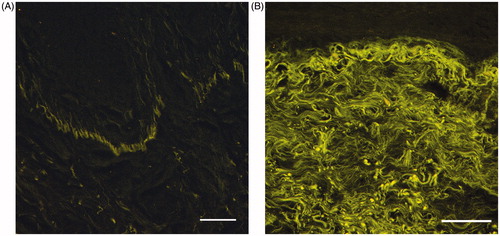
During the initial examination of the biopsies we noticed marked differences in the composition of the tissue between survivors and controls. The survivors had a thinner epithelium and a dense connective tissue (). The area fraction of elastin was greater in the survivors 10.0% (range 0.8–18.1) compared with the controls 3.4% (range 0.9–11.6) (p < 0.001). The distribution and organization of the elastin fibers differed markedly (). In the controls, the elastin fibers were located in a thin sub-epithelial layer under the basal membrane (), while in the survivors, thick aggregated elastin fibers were scattered throughout the connective tissue (); a morphological finding resembling actinic elastosis.
Figure 1. Hematoxylin-eosin stained biopsies from the vaginal wall in healthy women with thick squamous cell epithelia with dermal papillae (A), and cervical cancer survivors with thin epithelia and dense connective tissue with signs of fibrosis and elastosis (B). Scale bar = 200 μm.
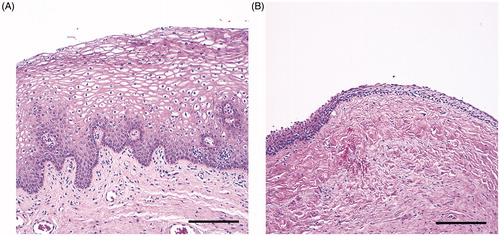
Figure 2. Autofluorescent elastin fibers under the basal membrane in the vaginal wall in healthy women (A), and thick aggregated elastin fibers scattered throughout the connective tissue in the cervical cancer survivors (B). Scale bar = 200 μm.
Collagen fibers from all four panels were found in each specimen, but the distribution of various fibers differed between survivors and controls. The collagen was denser and more tightly packed in the survivors; almost half was found in panel A, i.e. the collagen with the highest density (fibrosis), compared with the controls who had a relatively even distribution between all panels. Women in treatment Group II with external radiation had more collagen with high density compared to those who only received preoperatively BT ().
Discussion
We found fibrosis and elastosis in the connective tissue, with noticeably dense collagen and numerous entangled elastin fibers, in the vaginal wall of cervical cancer survivors treated with radiotherapy. These results were accompanied by our observations during the vaginal examination with marked differences in all clinical parameters between the survivors and the controls. The survivors with high radiation dose at biopsy site showed the most prominent changes in both morphological and clinical findings. Women treated for cervical cancer report physical sexual dysfunction such as reduced vaginal elasticity at intercourse, reduced lubrication, and dyspareunia [Citation1]. The morphological findings can be an important part of the explanation of these symptoms.
Unexpectedly, we found a high prevalence of elastin (elastosis) in the vaginal connective tissue in cervical cancer survivors compared with controls. One would expect that a high prevalence of elastin would imply a more elastic tissue, which is contrary to our clinical findings and the reports from the cancer survivors. When we studied the microscopic slides we could observe that the elastic fibers had a dysfunctional distribution, with thick aggregated elastin fibers scattered throughout the connective tissue in an entangled manner. This contrasted with the distribution of elastin fibers in the controls, which were located in a thin sub-epithelial layer along the basal membrane. We tried to correlate the elastin content to the radiation dose in the different treatment groups, but we were unable to confirm any correlation. This might be due to the small sample sizes, with only five patients in the treatment group receiving preoperatively BT. Studies on elastin content and distribution are rare. The high prevalence of elastin is, however, in accordance with sparse reports from patients with connective tissue diseases. A study by Rustin et al. reports altered elastin fibers with thickening and clumping in patients with scleroderma [Citation7]. This finding has likenesses to actinic elastosis, which is otherwise seen in heavily sun-exposed skin [Citation8]. The dysfunctional elastin can explain the symptoms reported by the cancer survivors such as shortened, inelastic vagina and subsequent dyspareunia [Citation1] and our clinical findings of rigid and unyielding tissues during the gynecological examination.
The vaginal connective tissue collagen showed higher density in survivors compared with controls. In subanalyses the collagen with the highest density, equivalent to fibrosis, were more common in the group of cancer survivors that had received a high radiation dose at the biopsy site. Our calculations of the radiation dose at the biopsy site showed that the patients treated with preoperative BT only had received minimal radiation at the distal part of the vagina, in contrast to those who had received additional external radiation affecting the whole vaginal wall. We therefore conclude that the finding of fibrosis is radiotherapy-induced. In studies from other irradiated tissues, mainly skin, collagen deposition is described as part of the radiation fibrosis and defective tissue healing [Citation9–11]. To our knowledge, there are no previous studies analyzing the connective tissue of the vaginal wall after radiotherapy in survivors. We have only found two previous studies reporting morphological changes in vaginal biopsies after radiotherapy. In 1974, Abitbol and Davenport reported fibrotic changes with hyalinization and collagenization of the connective tissue [Citation12]. The second study is from Shield in 1995 where 11 vaginal biopsies were described morphologically with fibrotic stromal changes without a specific description of collagen content [Citation13].
During the clinical examination we found pale thin mucous membranes and signs of pelvic fibrosis, which is in contrast to the non-existence of these findings in the control group. Similar findings have previously been reported by Kirchheiner et al. [Citation14]. After pelvic radiotherapy women report sore mucous membranes [Citation1], partly because of atrophic epithelium [Citation15] and possibly due to hypo-vascularization and hypoxia [Citation16]. The treatment of cervical cancer with radiotherapy and/or surgery results in low levels of circulating estrogen. In spontaneous menopause, vaginal atrophy can be treated with vaginally administrated estrogen [Citation17]. In our study almost all the cancer survivors were substituted with systemic and/or local hormonal therapy at time of the study, but even so, 91% of the survivors showed signs of vaginal atrophy. These findings support previous suggestions that radiotherapy-induced vaginal changes make the vagina less responsive to systemic and topical estrogen [Citation12]. The effect of radiation on the amount and distribution of estrogen receptors in the vaginal mucosa is unknown. One may speculate if a possible alteration of receptor function is both an early and late effect of the radiation and whether an early start of topical estrogen before symptoms occurs could preserve the receptor function and thus hamper the atrophic process.
The strengths of this study are the standardized sampling, the inclusion criteria of premenopausal women with no age-induced vaginal atrophy, and the blinded samples analyzed by the same pathologist and examiner. The study is limited though, by its small size and heterogeneous material concerning treatment. All the survivors were, however, treated with radiotherapy. Approximately 75% also underwent surgery as a part of their treatment. Radical hysterectomy alone may cause vaginal shortening and inelasticity [Citation11]. More than half of the survivors also had chemotherapy. An important finding in this study is that several assessed parameters were related to the dose of radiation at biopsy site. Previous studies have shown more severe late toxicities following concomitant radiochemotherapy, compared with radiotherapy alone. However, this effect was seen in post- but not in premenopausal women. In premenopausal women there were no additional effects of chemotherapy [Citation18].
In summary, the radio-induced changes in the vaginal wall can give a morphological explanation of the physical symptoms in cervical cancer survivors. Our results also support that patients treated with external radiation have the highest risk of developing vaginal fibrosis. In future improvements of radiotherapy, the vagina should be regarded as an organ at risk to minimize the physical side effects in cervical cancer patients. A better understanding of the interplay between the early uses of dilators, in combination with an early start of topical estrogen treatment, may also be a way to preserve a functional vaginal wall.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Bergmark K, Avall-Lundqvist E, Dickman PW, et al. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med. 1999;340:1383–1389.
- Vale CTJ, Stewart LA. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: a systematic review and meta-analysis of individual patient data from 18 randomized trials. J Clin Oncol. 2008;26:5802–5812.
- Andreyev HJ, Wotherspoon A, Denham JW, et al. Pelvic radiation disease: new understanding and new solutions for a new disease in the era of cancer survivorship. Scand J Gastroenterol. 2011;46:389–397.
- Blomgren B, Falconer C, Roomans G, et al. A novel method for visualisation of elastic fibres – suiteble for image analysis and morphometry. Image Anal Stereol. 2001;20:522–526.
- Danielsson BR, Skold AC, Johansson A, et al. Teratogenicity by the hERG potassium channel blocking drug almokalant: use of hypoxia marker gives evidence for a hypoxia-related mechanism mediated via embryonic arrhythmia. Toxicol Appl Pharmacol. 2003;193:168–176.
- Gundersen B. Context-dependent plasticity in a sensory circuit. Nat Neurosci. 2013; 16:1366.
- Rustin MH, Papadaki L, Rode J, et al. Elastic fibres in patients with systemic sclerosis. A morphological study. Virchows Arch a Pathol Anat Histopathol. 1989;416:115–120.
- Weedon D, Rubin AI, Strutton G. Weedon's Skin Pathology. 3th ed. London: Churchill Livingstone; 2010.
- Denham JW, Hauer-Jensen M. The radiotherapeutic injury-a complex 'wound'. Radiother Oncol. 2002;63:129–145.
- Delanian S, Lefaix JL. Current management for late normal tissue injury: radiation-induced fibrosis and necrosis. Semin Radiat Oncol. 2007;17:99–107.
- Abitbol MM, Davenport JH. Sexual dysfunction after therapy for cervical carcinoma. Am J Obstet Gynecol. 1974;119:181–189.
- Abitbol MM, Davenport JH. The irradiated vagina. Obstet Gynecol. 1974;44:249–256.
- Shield PW. Chronic radiation effects: a correlative study of smears and biopsies from the cervix and vagina. Diagn Cytopathol. 1995;13:107–119.
- Kirchheiner K, Fidarova E, Nout RA, et al. Radiation-induced morphological changes in the vagina. Strahlenther Onkol. 2012;188:1010–1017.
- Pitkin RM, Bradbury JT. The effect of topical estrogen on irradiated vaginal epithelium. Am J Obstet Gynecol. 1965;92:175–182.
- Bentzen SM. Preventing or reducing late side effects of radiation therapy: radiobiology meets molecular pathology. Nat Rev Cancer. 2006;6:702–713.
- Heimer GM, Englund DE. Effects of vaginally-administered oestriol on post-menopausal urogenital disorders: a cytohormonal study. Maturitas. 1992;14:171–179.
- Gondi V, Bentzen SM, Sklenar KL, et al. Severe late toxicities following concomitant chemoradiotherapy compared to radiotherapy alone in cervical cancer: an inter-era analysis. Int J Radiat Oncol Biol Phys. 2012;84:973–982.
