Abstract
Background
The exhaustive information about non-communicable diseases associated with COVID-19 and severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) are getting easier to find in the literature. However, there is a lack of knowledge regarding tuberculosis (TB) and chronic obstructed pulmonary disease (COPD), with numerous infections in COVID-19 patients.
Objectives
Priority is placed on determining the patient’s prognosis based on the presence or absence of TB and COPD. Additionally, a comparison is made between the risk of death and the likelihood of recovery in terms of time in COVID-19 patients who have either COPD or TB.
Methodology
At the DHQ Hospital in Muzaffargarh, Punjab, Pakistan, 498 COVID-19 patients with TB and COPD were studied retrospectively. The duration of study started in February 2022 and concluded in August 2022. The Kaplan–Meier curves described time-to-death and time-to-recovery stratified by TB and COPD status. The Wilcoxon test compared the survival rates of people with TB and COPD in two matched paired groups and their status differences with their standard of living.
Results
The risk of death in COVID-19 patients with TB was 1.476 times higher than in those without (95% CI: 0.949–2.295). The recovery risk in COVID-19 patients with TB was 0.677 times lower than in those without (95% CI: 0.436–1.054). Similarly, patients with TB had a significantly shorter time to death (p=.001) and longer time to recovery (p=.001).
Conclusions
According to the findings, the most significant contributor to an increased risk of morbidity and mortality in TB and COPD patients was the COVID-19.
SARS-Cov-19 is a new challenge for the universe in terms of prevention and treatment for people with tuberculosis and chronic obstructive pulmonary disease, among other diseases.
Propensity score matching to control for potential biases.
Compared to hospitalized patients with and without (TB and COPD) had an equivalently higher mortality rate.
KEY MESSAGES
Introduction
The worldwide COVID-19 pandemic burden had reached approximately 63 billion cases as of November 2022, with massive breakouts in different countries [Citation1]. Chronic obstructed pulmonary disease (COPD) affected over 251 million people worldwide, and 3.17 million deaths were reported each year [Citation2,Citation3]. According to the World Health Organization (WHO) report 2022, based on electronic data collected from 215 countries, approximately 40 million people were treated for multidrug and rifampicin-resistant tuberculosis (MDR/RR-TB) worldwide, with 649,000 adults and 17,700 children receiving treatment [Citation4].
Global TB prevention and treatment were challenged by the current severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) pandemic [Citation5]. According to their study, patients with COVID-19 and TB had a higher risk of dying and a lower chance of recovering. Potential treatments must target TB patients to reduce the overall impact of COVID-19. Both the treatment and prevention programs for TB had been disrupted as a consequence of the epidemic [Citation6]. Estimates from conservative models indicated that the pandemic would likely increase TB-related deaths by 20% over the next five years [Citation6,Citation7] as well as the underlying causes of simultaneous COVID-19 and TB disease mortality, which not yet well understood clinically and immune pathologically [Citation8–11]. In 2020, the first pilot study of the Global TB Network (GTN) published 49 co-infected TB/COVID-19 patients from eight countries [Citation12], which indicated that TB diagnosed concomitantly with or after COVID-19 may enhance case-fatality.
Pakistan, a country with a lower-middle income and a population of approximately 200 million, had a high prevalence of chronic respiratory diseases, such as COPD. In Pakistan, it was estimated that the mortality rate among males due to chronic respiratory diseases was 138.2 per 100,000, while the mortality rate among females due to these diseases was 41.3 per 100,000. A global survey (BREATHE) found that 2.1% of Pakistani adults over 40 years were diagnosed with COPD [Citation13,Citation14]. According to the WHO report for 2022, Pakistan developed 2.8% TB of the total population, an increase of 7.9% over the previous year reported [Citation4]. So far, there has been no study of a large multivariate link between TB and COPD in COVID-19 patients.
Materials and methods
Sample size and study population
A retrospective study was done at the DHQ Hospital Muzaffargarh (covering rural and urban areas of four tehsils: Muzaffargarh, Jatoi, Ali Pur and Kot Addu) to test 498 male and female patients for COPD and TB, while the total population of District Muzaffargarh was 43,48,549 [Citation15]. According to the statistical officer at the DHQ Hospital Muzaffargarh, patient history remained in 2020–2021; the total number of TB and COPD (OPD patients), TB and COPD (indoor and follow-up cases), TB and COPD (suspected patients) and TB/COPD (conformed patients with COVID-19) were 22,240, 7514, 17,896 and 1080, respectively. Using a simple random technique, we included COVID-19 cases reported from January 2020 to December 2021. The laboratories accredited by the Punjab Health Council (PHC) and the Research Institute of Nishtar Medical College and University Multan performed real-time reverse transcription polymerase chain reaction (RT-PCR) to confirm the COVID-19 cases. COPD was diagnosed using a simple breathing test called spirometry, and in the context of pulmonary TB, sputum culture revealed Mycobacterium tuberculosis in the majority of reported TB patients [Citation16]. Following a routine medical examination, the data and information were collected by a nursing staff or a consultant pulmonologist. The interview form was manually completed and collected from the resource file of the patients. This study started in February 2022 and concluded in August 2022; data collection concluded in March 2022.
Ethics statement
The department issued a letter of ethical approval on 10 May 2022, with reference no. 1178-81/DHQ, by Aqeel Ahmad, Statistical Officer-in-charge of the ethical committee in DHQ Hospital Muzaffargarh, Punjab, Pakistan.
Variables
This study examined various chest infection-related complaints from patients with COPD and TB. In lung diseases, COPD is a group of diseases that make it hard to breathe and block airflow, including emphysema and chronic bronchitis. The bacterium Mycobacterium tuberculosis is accountable for causing TB. The lungs are the most common target, but the kidney, spine and brain are all possible locations for TB bacterial infection. However, not all people who contract the tuberculosis (TB) bacteria ever develop symptoms. The SARS-CoV-2, which was discovered in 2019, is the cause of COVID-19, a respiratory disease. Coughing, sneezing and talking all contribute to the spread of the virus from person to person [Citation17]. Diagnoses based on TB and COPD included cough, fever, sputum, right-sided chest pain, acid-fast bacillus (AFB), lower respiratory tract infection (LRTI), TB/pulmonary tuberculosis (PTB), shortening of breath (SOB), normal condition, headache, wheezing and body aches [Citation18–29] were present.
Outcomes
The two significant outcomes of interest elaborate on time-to-event variables.
Death/expire
Recovery
Both outcomes were primary, and they occurred over time. If the admitted COVID-19 indoor patients, presence or absence of TB, had severe symptoms, the case would be declared dead. If there were some clinical improvement, the patient would survive and have a better chance of recovering.
Statistical analysis
Descriptive statistics and a Student t-test were used to compare the ages of patients with and without TB and COPD [Citation30]. First, analysis was performed to estimate the relative risk (risk ratio) of mortality and recovery, and the Pearson chi-squared test was used to assess health status, gender, co-morbidities and admission status [Citation31]. The Wilcoxon rank-sum test manipulates the survival rates of patients with TB and COPD into two groups [Citation32]. Kaplan–Meier’s curves were used to plot time-to-event variables based on whether or not a person had TB or COPD. Patients who passed away on their last day of inpatient care were not included in the time-to-recovery analysis [Citation33]. All statistical analyseis were done in SPSS-22 (SPSS Inc., Chicago, IL) and R (R Foundation for Statistical Computing, Vienna, Austria).
Hypothesis
We hypothesized that COVID-19 patients with a prior history of TB or active TB would have worse clinical outcomes than those without TB. Patients with and without TB co-infection at DHQ Hospital Muzaffargarh, Punjab, Pakistan, were analysed to determine differences in mortality and recovery rates associated with the COVID-19.
Ha1: the median difference between TB and those who do not equal zero.
Ha2: the median difference between people with and without COPD is zero.
Results
Propensity score matching
The initially un-matched sample included 17,896 COVID-19 patients, of whom 218 (1.2%) had confirmed TB and 280 (1.56%) did not. Age significantly affected TB patients’ recovery (p=.001) and death (p=.001). The total sample’s average age was 23.81 years, with a variance of 686.50. The admitted sample created a population with similar baseline characteristics (all p > .05; ).
Table 1. Demographics and health status of the matched with/without samples and matched admitted TB/COPD samples by COVID-19 status.
Patients with TB had a 1.476 times higher mortality rate than those without it (95% CI: 0.949–2.295). When hospitalized patients were assessed, those with TB and those without COPD had a similarly higher mortality rate. Patients had a lower chance of recovery at 0.677 (95% CI: 0.436–1.054). The estimates of RR with TB/without COPD were at 0.812 (95% CI: 0.650–1.016), and the estimates of RR without TB/with COPD observed at 1.199 (95% CI: 0.650–1.016), which denoted greater than the estimates of RR in without TB/with COPD patients ().
Table 2. Relative risk estimates of death and recovery with/without TB and COPD matched admitted patient samples of COVID-19.
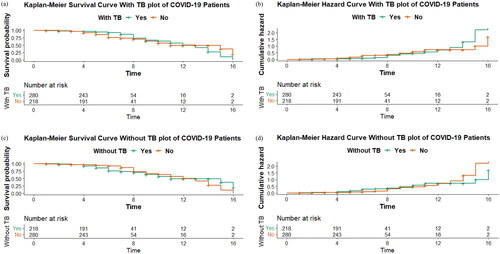
In , Kaplan–Meier’s curves portrayed the results pattern of the graph proposed with and without TB. In sections (a), (b), (c) and (d), the survival and hazards graphs classify the average number of patients who survive or die over time. It validates the findings that average COVID-19 patients, with or without TB, recovered in 12–16 days, and death occurred on average in 0–6 days.
Figure 1. Survival analysis (a) in fully matched samples with TB, time-to-death and survival evaluated the survival function. (b) Time-to-death and survival evaluated the hazard function in fully matched samples with TB. (c) Time-to-death and survival evaluated the survival function in fully matched samples without TB. (d) Time-to-death and survival evaluated the hazard function in fully matched samples without TB.
Discussion
The world has seen different diseases with time, but SARS-Cov-2 has become a new challenge for the universe in terms of the prevention and treatment of TB and COPD patients. Comprehensive measures were adopted to reduce the effect of infectious diseases accordingly. The results indicated that COVID-19 patients with TB and COPD were twice as likely to die and less likely to improve over time. On the other hand, patients with TB had shorter survival times and longer recovery times compared to patients without COPD. According to the WHO report of 3 October 2022 [Citation34], there had been 616,951,418 confirmed cases of COVID-19 and 6,530,281 deaths were reported. Some of these fatalities can be related to TB patients with COVID-19 having higher mortality and a slower recovery rate.
Additionally, our research showed that areas with higher TB prevalence had higher COVID-19 case fatality rates. Health planning and the allocation of resources were compulsory to overcome the disease pattern. Similarly, COVID-19 cases are instantly increasing in many underdeveloped countries, which show a higher trend of TB rates and a significant difference among diseases. Fundamental strategies for individuals with TB and COPD can reduce the burden of COVID-19. Our results correspond with the findings of a study conducted in South Africa’s Western Cape Province, which revealed that COVID-19 patients with an existing TB diagnosis had a 1.47-times greater risk of death, and those with a history of TB had a 50% higher chance of death [Citation35]. Several studies have examined the connection between COVID-19 positivity and COPD and TB. With SARS-CoV-2, TB patients are more likely to deteriorate [Citation36].
We performed propensity score matching to account for confounding variables. However, due to residual confounding, HIV-positive COPD patients will also face difficulties. Further, there were discrepancies in the propensity scores due to the presence of non-matched co-morbid variables.
We did not have any information on HIV-AIDS in our study, which could have influenced our estimates because patients with TB and COPD and no other conditions would have made it easier to rule out other factors. In the survival analyses, we did not include people whose dates were missing. Statistical analyses were used to look at how the confounding factors spread out in the sample used for each time-to-event analysis. It ensured that there were no significant differences between patients with TB and COPD and those who did not have those diseases. Also, there might be some missing data for the primary outcomes of death and recovery. The survival analysis made up for this by censoring patients who were not the outcome on the last day of follow-up (left against medical advice (LAMA) cases).
Our findings show a direct link between COVID-19 and TB/COPD, but SARS-CoV-2 also indirectly contributes to TB and COPD morbidity and mortality. COVID-19 impacted health systems worldwide, and mortality rates for people with TB and COPD are expected to rise due to drug shortages and delays in diagnosis and treatment [Citation37–39]. Furthermore, the inaccessibility of the health care system reduces the ability to pay for medical costs, which disproportionately affects socially disadvantaged populations. Even though the COVID-19 pandemic has caused changes to health and social systems [Citation40], our findings show how important it is to keep TB and COPD routines and testing services a top priority. Longer follow-up studies with a large enough sample size to make inferential comparisons. Based on what we found, this study has enough participants to look into the link between COPD and TB in a high-burden COVID-19.
Conclusions
This study found that cough, fever, sputum, right-sided chest pain, AFB, LRTI, TB/PTB, SOB, normal condition, headache, wheezing and body aches are the most common causes in COVID-19 patients with or without TB. Controlling these factors eliminates or reduces the risk of acquiring COVID-19 and SARS-CoV-2. Patients with TB had a 1.47-times greater risk of death and a 0.67 times lower chance of recovery. The study concluded that the most infective treatment combinations should be considered when designing infection prevention strategies. Our findings can help improve how COVID-19 patients’ health care is organized and help direct health interventions and protection plans to the most vulnerable chronic patients.
Author contributions
Muhammad Muneeb Hassan: conceived idea, developed the theory, coding, graph making and performed the computations, final approval of the version to be published. Muhammad Ameeq: contributes to conceptualization, data analysis, coding, graph making and final approval of the version to be published. Farrukh Jamal: editing, proofreading, data interpretation, writing and final approval for publication. Muhammad H. Tahir: editing, proofreading, data interpretation, writing and final approval for publication. John T Mendy: editing, proofreading, data interpretation, writing and final approval for publication. All authors contributed to interpreting data, drafting the manuscript, and critically revising the manuscript for intellectual content; all authors approved of the published version.
Ethics statement
The Ethical Review Committee of District Hospital Muzaffargarh, Punjab, Pakistan approved that they have no objection and do not raise any ethical issue regarding this research.
Consent form
Not applicable, because secondary data of discharged patient were collected from the hospital record with the approval of ethical committee.
Patient consent
Not required.
Disclosure statement
The authors have declared no conflicts of interest.
Data availability statement
Data, models and code supporting this study’s findings are available from the corresponding author.
Additional information
Funding
References
- Center for Systems Science and Engineering at Johns Hopkins University. COVID-19 dashboard; 2022. Available from: https://coronavirus.jhu.edu/map.html
- Liu Y, Han X, Cui X, et al. Association between air pollutants and acute exacerbation of chronic obstructive pulmonary disease: a time stratified case-crossover design with a distributed lag nonlinear model. GeoHealth. 2022;6(2):e2021GH000529.
- Burić DJ, Erceg M, Antoljak N. Gender differences in specific trends of COPD mortality in Croatia. Public Health. 2022;202:26–31.
- World Health Organization (WHO). Global tuberculosis report 2022. License: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization; 2022. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022
- Gong W, Parkkila S, Wu X, et al. SARS-CoV-2 variants and COVID-19 vaccines: current challenges and future strategies. Int Rev Immunol. 2022:1–22.
- Hogan AB, Jewell BL, Sherrard-Smith E, et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Global Health. 2020;8(9):e1132–e1141.
- Cilloni L, Fu H, Vesga JF, et al. The potential impact of the COVID-19 pandemic on the tuberculosis epidemic a modelling analysis. EClinicalMedicine. 2020;28:100603.
- Visca D, Ong CW, Tiberi S, et al. Tuberculosis and COVID-19 interaction: a review of biological, clinical and public health effects. Pulmonology. 2021;27(2):151–165.
- Stochino C, Villa S, Zucchi P, et al. Clinical characteristics of COVID-19 and active tuberculosis co-infection in an Italian Reference Hospital. Eur Respir J. 2020;56(1):2001708.
- Petrone L, Petruccioli E, Vanini V, et al. Coinfection of tuberculosis and COVID-19 limits the ability to in vitro respond to SARS-CoV-2. Int J Infect Dis. 2021;113:S82–S87.
- Riou C, Du Bruyn E, Stek C, et al. Relationship of SARS-CoV-2-specific CD4 response to COVID-19 severity and impact of HIV-1 and tuberculosis coinfection. J Clin Invest. 2021;131(12):e149125.
- Tadolini M, Codecasa LR, García-García JM, et al. Active tuberculosis, sequelae and COVID-19 co-infection: first cohort of 49 cases. Eur Respir J. 2020;56(1):2001398.
- Khan MA, Khan MA, Walley JD, et al. Feasibility of delivering integrated COPD-asthma care at primary and secondary level public healthcare facilities in Pakistan: a process evaluation. BJGP Open. 2019;3(1):bjgpopen18X101634.
- Baba MA, Khan SE, Hasnain F, et al. Exploring the treatment types and challenges in patients with chronic obstructive pulmonary disease: a qualitative study. Middle East J Fam Med. 2022;7(10):23.
- Census-2017, District table, Punjab, Pakistan Bureau of Statistics; 2022. Available from: www.pbs.gov.pk/sites/default/files/population/2017/punjab_tehsil.pdf
- Mishra A, George AA, Sahu KK, et al. Tuberculosis and COVID-19 co-infection: an updated review. Acta Biomed. 2020;92(1):e2021025.
- CDC&P (Center for Disease Control and Prevention); 2022. Available from: https://www.cdc.gov/copd/index.html#:∼:text=What%20is%20COPD%3F,Americans%20who%20have%20this%20disease
- Taz TA, Ahmed K, Paul BK, et al. Identification of biomarkers and pathways for the SARS-CoV-2 infections that make complexities in pulmonary arterial hypertension patients. Brief Bioinform. 2021;22(2):1451–1465.
- Taz TA, Ahmed K, Paul BK, et al. Network-based identification genetic effect of SARS-CoV-2 infections to idiopathic pulmonary fibrosis (IPF) patients. Brief Bioinform. 2021;22(2):1254–1266.
- Mahmud SH, Chen W, Liu Y, et al. PreDTIs: prediction of drug–target interactions based on multiple feature information using gradient boosting framework with data balancing and feature selection techniques. Briefings Bioinf. 2021;22(5):bbab046.
- Mahmud SH, Al-Mustanjid M, Akter F, et al. Bioinformatics and system biology approach to identify the influences of SARS-CoV-2 infections to idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease patients. Briefings Bioinf. 2021;22(5):bbab115.
- Tanzir Mehedi S, Ahmed K, Bui FM, et al. MLBioIGE: integration and interplay of machine learning and bioinformatics approach to identify the genetic effect of SARS-COV-2 on idiopathic pulmonary fibrosis patients. Biol Methods Protoc. 2022;7(1):bpac013.
- Islam M, Alam MK, Paul BK, et al. Identification of molecular biomarkers and key pathways for esophageal carcinoma (EsC): a bioinformatics approach. Biomed Res Int. 2022;2022:5908402.
- Islam M, Abdulrazak LF, Alam MK, et al. Identification of potential key genes and molecular mechanisms of medulloblastoma based on integrated bioinformatics approach. Biomed Res Int. 2022;2022:1776082.
- Al Zamane S, Nobel FA, Jebin RA, et al. Development of an in silico multi-epitope vaccine against SARS-COV-2 by précised immune-informatics approaches. Inform Med Unlocked. 2021;27:100781.
- Islam R, Ahmed L, Paul BK, et al. Identification of molecular biomarkers and pathways of NSCLC: insights from a systems biomedicine perspective. J Genet Eng Biotechnol. 2021;19(1):1–9.
- Islam MR, Ahmed ML, Paul BK, et al. Identification of the core ontologies and signature genes of polycystic ovary syndrome (PCOS): a bioinformatics analysis. Inf Med Unlocked. 2020;18:100304.
- Bouwens JDM, Bischoff EWMA, In 't Veen JCCM, et al. Diagnostic differentiation between asthma and COPD in primary care using lung function testing. NPJ Prim Care Respir Med. 2022;32(1):32–39.
- Raza A, Syed JG, Ali FM, et al. Incidence of vitamin D deficiency in different seasons in the adult Karachi population presenting in the medical outpatient department with generalized body ache. Cureus. 2019;11:18.
- Curtis A. Hypoxic responses in resting hyperthermic humans [doctoral dissertation]. School of Kinesiology-Simon Fraser University; 2005.
- Sy KT, Haw NJ, Uy J. Previous and active tuberculosis increases risk of death and prolongs recovery in patients with COVID-19. Infect Dis. 2020;52(12):902–907.
- Cheng SL, Chan MC, Wang CC, et al. COPD in Taiwan: a national epidemiology survey. Int J Chron Obstruct Pulmon Dis. 2015;10:2459–2467.
- In J, Lee DK. Survival analysis: part I—analysis of time-to-event. Korean J Anesthesiol. 2018;71(3):182–191.
- WHO; 2022. Available from: https://covid19.who.int/
- Chen Y, Wang Y, Fleming J, et al. Active or latent tuberculosis increases susceptibility to COVID-19 and disease severity. MedRxiv; 2020.
- Motta I, Centis R, D'Ambrosio L, et al. Tuberculosis, COVID-19 and migrants: preliminary analysis of deaths occurring in 69 patients from two cohorts. Pulmonology. 2020;26(4):233–240.
- McQuaid CF, McCreesh N, Read JM, et al. The potential impact of COVID-19-related disruption on tuberculosis burden. Eur Respir J. 2020;56(2):2001718.
- Maciel ELN, Gonçalves E, Dalcolmo MMP. Tuberculosis and coronavirus: what do we know? Epidemiol Serv Saúde. 2020;29(2):e2020128.
- Klinton JS, Oga-Omenka C, Heitkamp P. TB and COVID – public and private health sectors adapt to a new reality. J Clin Tuberc Other Mycobact Dis. 2020;21:100199.
- Amimo F, Lambert B, Magit A. What does the COVID-19 pandemic mean for HIV, tuberculosis, and malaria control? Trop Med Health. 2020;48(1):1–4.
