ABSTRACT
Clinical relevance
Constant technological improvements require practitioners to be open to adopting technologies such as telehealth for enhanced patient care. Understanding the barriers and facilitators of telehealth adoption will guide stakeholders in making decisions for safe and effective implementation of telehealth.
Background
Effective use of telehealth improves patient outcomes. It is unclear if optometry students feel supported in using and/or are accepting of telehealth. This study evaluated telehealth acceptance of optometry students, its association with their technology self-efficacy, and whether telehealth training alters this relationship.
Methods
Final-year optometry students at the University of Melbourne were invited to participate in a telehealth course. A 22-item online survey adapted from the Technology Proficiency Self-Assessment for twenty-first Century Learning was used to evaluate technology self-efficacy pre- and post-learning. Telehealth acceptance was evaluated using a 34-item survey according to the Unified Theory of Acceptance and Use of Technology-2. A 5-point Likert scale was used for each item, yielding two total scores. Respondent demographics, frequency of usage and number of devices were recorded. Descriptive statistics, ANOVA and Pearson correlation were used to analyse demographic variables and relationship between technology self-efficacy and telehealth acceptance.
Results
58 (68%) and 49 (58%) students participated in the pre- and post-learning surveys. Majority were 20–29-year-old females. Students used between two and four devices for online activities, with 62% being online at least hourly. Technology self-efficacy scores (average ± SD) pre- and post-learning were 83.8% ± 8.2 and 87.8% ± 7.1. Telehealth acceptance scores pre- and post-learning were 66.1% ± 9.6 and 73.98% ± 9.9. There was no association with gender, number of devices and frequency of online use for all scores. Correlation between technology self-efficacy and telehealth acceptance was insignificant pre-learning (p = 0.3) but was significant post-learning (p = 0.04).
Conclusion
Optometry students demonstrated high technology self-efficacy compared to telehealth acceptance. Telehealth training resulted in marked improvement in telehealth acceptance.
Introduction
Telehealth involves practitioner-to-patient or practitioner-to-practitioner interactions using technology instead of in-person encounters.Citation1 These can be synchronous, such as real-time interactive sessions, or asynchronous involving remote monitoring or store-and-forward, where information is collected and reviewed at another time.Citation2 Telehealth can be used as an adjunct for initial and subsequent consultations, for disease prevention, patient education, or treatment.Citation2 Using telehealth, health practitioners can extend services to rural and remote patients,Citation3,Citation4 provide privacy for patients with stigmatised health conditions,Citation1 and reduce time and travel costs for both patients and practitioners resulting in cost-effectiveness.Citation1,Citation2
Whilst telehealth has existed for some time now, the COVID-19 pandemic has increased its uptake and utilisation across health professions, and optometrists had to adapt to virtual patient care.Citation5 There is currently limited published literature on telehealth use in optometryCitation5 with the scope of optometry-facilitated telehealth varying between countries, including independent optometry practice and co-management with ophthalmology.Citation5 In Australia, published literature has described synchronous and asynchronous collaborative patient care with ophthalmology, primarily in rural and remote Australia.Citation3,Citation4
With improvements in technology software and equipment supported by high-speed internet, and evolving expectations of patients and practitioners, it is likely that telehealth will become a larger part of optometric practice. It is unclear if optometrists or optometry students feel supported and equipped for telehealth usage, and if they are accepting of utilising telehealth practice in providing safe and effective patient care in this new and changing environment.
A major factor that has been shown to affect attitudes towards technology acceptance and their actual use in healthcare is self-efficacy. Technology self-efficacy was found to influence the intention of healthcare workers to use electronic medical recordsCitation6 and clinical information systems.Citation7 In pharmacy students, greater information technology self-efficacy was associated with readiness of students to utilise health information technology.Citation8 Self-efficacy can be described as ‘assessments of effectiveness or competency to perform a specific behaviour successfully of an individual’.Citation9
In assessing self-efficacy, the focus is not on the skills that one has but with judgements of what one can do with whatever skills one possesses.Citation10 Individuals with high self-efficacy perceptions exhibit positive attitudes about their ability to navigate obstacles and complete a task, whilst individuals with low perceptions of self-efficacy tend to underestimate their true capability to handle the same critical situation. Currently, there are no published studies on technology self-efficacy in optometry, and it is not known if optometry students who will become practitioners have high technology self-efficacy, indicating a positive attitude towards accepting telehealth practice.
Another key factor that influences telehealth adoption in healthcare is the lack of clinician training.Citation11 While growing, there remains limited literature on telehealth education and training in healthcare.Citation12,Citation13 Training for telehealth delivery in Australian optometry institutions might focus mainly on communication, as it is the only explicit competency associated with telehealth in the Optometry Australia Entry-Level Competency Standards for Optometry (2022).Citation14
Previous work demonstrated that telehealth training can result in increased awareness of the benefits of telehealth,Citation15,Citation16 increased telehealth acceptance,Citation15–17 and a desire to incorporate telehealth into their future practice.Citation17 Training also resulted in actual incorporation of telehealth by healthcare graduates in their workplace.Citation18 These results suggest that telehealth should be taught in a comprehensive and systematic manner.
This study aims to evaluate if optometry students are accepting towards using telehealth and if this is associated with their technology self-efficacy. This study further investigates if online training alters this relationship. It is hypothesised that online training on telehealth will improve telehealth acceptance scores, resulting in a stronger association between technology self-efficacy and telehealth acceptance scores post-learning.
Methods
A single cohort pre-test and post-test design was used. This study was approved by The University of Melbourne Institutional Human Research Ethics Committee (approval ID 20,529).
Participants
Final-year Doctor of Optometry students enrolled at the University of Melbourne were invited to participate in the study via a total of three announcements on the learning management system (Canvas) during the period of July–September 2022. Participation was non-incentivised and voluntary and included undertaking an online telehealth curriculum, a pre- and post-learning survey. Participants remained anonymous for the pre- and post- learning surveys.
Demographic, technology usage and prior telehealth experience data
Demographic data collected in pre- and post-learning surveys included gender and age range of participants. In the pre-learning survey, questions regarding the type of devices that participants used to go online, and frequency of going online were also included. In the post-learning survey, participants were asked if they had prior telehealth experience either as a patient, carer, or student.
Telehealth curriculum
The telehealth curriculum is designed for entry-to-practice health profession students at the University of Melbourne. The course learning outcomes and content are outlined in . The emphasis of the course was to introduce concepts of digital health, what Telehealth is, as well as its key components and delivery. Students also learnt about Telehealth architectures, funding and reimbursement, ethics, and legalities of virtual models of care. Participants completed five modules, and a minimum score of 80% in a series of 10 multiple choice or short-answer questions was required before they had access to the next module.
Table 1. Learning objectives of telehealth curriculum.
Table 2. Telehealth curriculum – telehealth foundations for entry to practice health professional students: a suite of core elements.
Evaluation of technology self-efficacy
A 22-item online survey () adapted from the Technology Proficiency Self-Assessment for twenty-first Century Learning (TPSA C21),Citation19 was used to evaluate technology self-efficacy pre- and post-learning. The TPSA C21 was originally designed to evaluate technology self-efficacy of teachers in the classroom. Questions were modified to evaluate technology self-efficacy in optometry students in this study. Five domains ordered from the least difficult to the most difficult included three questions on the ‘internet’, five questions on ‘integrated applications’, three questions on ‘working with technology’, seven questions on ‘emerging technology’, and four questions on ‘emerging technology skills’.
Table 3. Technology self-efficacy survey; questions, score, and response distribution. Instructions for participants: The following questions relate to your PERCEPTIONS ABOUT USING TELEHEALTH as part of health professional practice. Please select the most appropriate rating on the scale from Strongly disagree (SD), Somewhat disagree (SWD), Neither agree or disagree (NAD), Somewhat agree (SWA) to Strongly Agree (SA). Note: some questions may be difficult to answer if you haven’t used telehealth or, based on future expectations – that’s ok – do your best to answer them based on how you feel at this time.
It is recognised that the questions included in the ‘emerging technology’ and ‘emerging technology skills’ domains involve technology that are now commonly used as compared to when the survey was first designed. These domain names remain unchanged in this study. A 5-point Likert scale was used (strongly disagree to strongly agree), yielding a final score for all questions and for each domain.
Evaluation of telehealth acceptance
Telehealth acceptance was evaluated using a 34-item survey () adapted version of the widely used Unified Theory of Acceptance and Use of Technology 2 (UTAUT-2).Citation20 There are ten domains, including three questions on ‘performance expectancy’, four questions on ‘effort expectancy’, three questions on ‘social influence’, four questions in ‘facilitating conditions’, three questions in ‘hedonic motivation’, three questions on ‘price value’, three questions on ‘habit’, four questions on ‘self-perception’, three questions on ‘behavioural intention’ and four questions on ‘use behaviour’.
Table 4. Telehealth acceptance survey questions, score, and response distribution. Instructions for participants: The following questions relate to your PERCEPTIONS ABOUT USING TELEHEALTH as part of health professional practice. Please select the most appropriate rating on the scale from Strongly disagree (SD), Somewhat disagree (SWD), Neither agree or disagree (NAD), Somewhat agree (SWA) to Strongly Agree (SA). some questions may be difficult to answer if you haven’t used telehealth or, based on future expectations – that’s ok – do your best to answer them based on how you feel at this time.
The definition for each domain is outlined in . A 5-point Likert scale (‘strongly disagree to strongly agree’ for all domains except ‘Use behaviour’ where it was ‘never to always’) was used for each item. A total score for the survey and each domain was calculated.
Data analysis
SPSS version 29 (SPSS Inc., Chicago, Illinois, USA) was used for data analysis. Student demographics, device use behaviour including the type and frequency, and pre- and post-learning responses to telehealth self-efficacy and telehealth acceptance surveys were analysed using descriptive statistics.
Linear regression was used to identify any significant factors associated with pre-learning technology self-efficacy and pre- and post-learning telehealth acceptance scores.
Pearson correlation was used to analyse the relationship between technology self-efficacy and telehealth acceptance scores.
Cronbach’s alpha was used to evaluate the internal consistency for each survey including domains.
Analyses were two-tailed and p-values less than 0.05 were considered statistically significant.
Results
Participant demographics
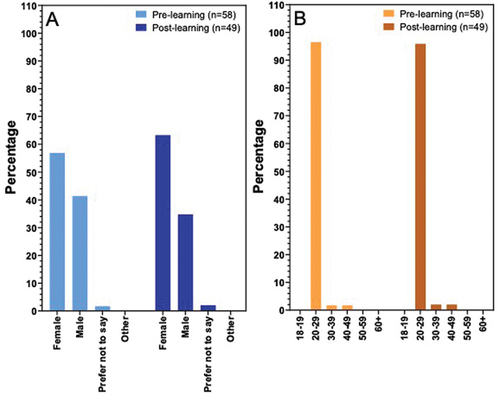
A total of 85 students were invited to participate, with 58 (68%) students completing the pre-learning survey. 49 (58%) students completed the telehealth curriculum and post-learning survey. shows the gender of the participants, with the majority being females (pre-learning: 56.9%; post-learning: 63.3%). shows the age of the participants with the majority aged between 20 and 29 (pre-learning: 96.6%; post-learning: 95.9%).
Participant technology usage
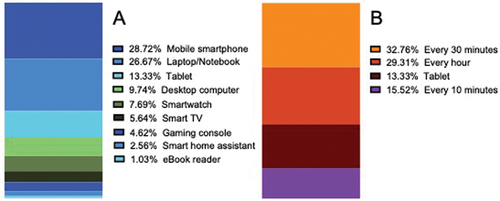
Participants who completed the pre-learning survey (n = 58) used between 1 and 7 devices (average ± standard deviation: 3 ± 1). shows the number and percentage of users for each type of device. Mobile smartphone was the most frequently used device (56, 96.6%), and eBook reader (e.g. kindle, kobo, etc.) (2, 3.4%) was the least frequently used. shows the frequency of going online or accessing the internet on average, with 19 (32.8%) participants accessing the Internet every 30 min.
Telehealth curriculum performance
An average of approximately 7 h was recorded as the time that participants (n = 49) were online when completing the telehealth curriculum. The average score was 91.7% (standard deviation: 12.2).
Technology self-efficacy
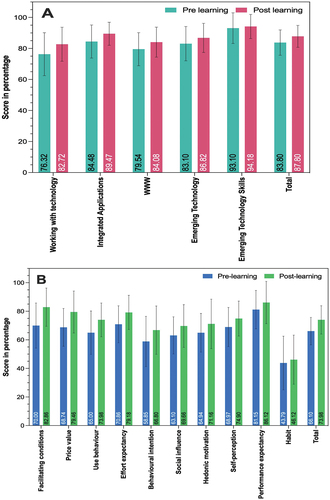
shows the pre- and post-learning technology self-efficacy scores in total and for each domain. These values and Cronbach’s alpha are also shown in . In , the domains are ranked according to the change in scores post-learning. The domain with the greatest improvement in score post-learning was ‘working with technology’ (+6.4%), with ‘emerging technology skills’ (+1.08%) having the least improvement in score. Total technology self-efficacy scores (average ± standard deviation) pre- and post-learning were 83.8% ± 8.2 and 87.8% ± 7.1.
Figure 3. Pre- and post-learning total and domain scores for A: Technology self-efficacy scores, and B: Telehealth acceptance scores.
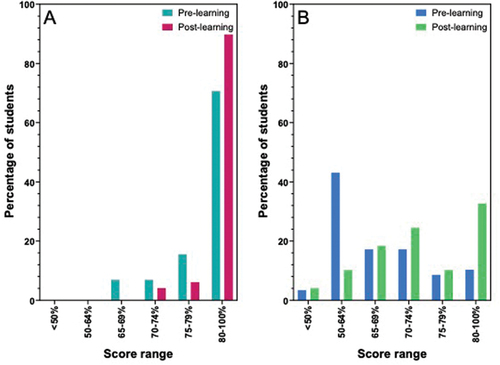
and show the percentage of students in each score range pre- and post-learning for technology self-efficacy.
Figure 4. Percentage of participants in each score range pre- and post- learning for A: Technology self-efficacy B: Telehealth acceptance.
The distribution of change in responses (strongly disagree to strongly agree) for the technology self-efficacy survey is shown in and .
Figure 5. Distribution of change in responses in A: Technology self-efficacy and B: Telehealth acceptance. Percentage change (post-learning score – pre-learning score) for each response category (strongly disagree- strongly agree) for each domain. Values below 0 indicate fewer respondents post-learning and values above 0 indicate more respondents post-learning.
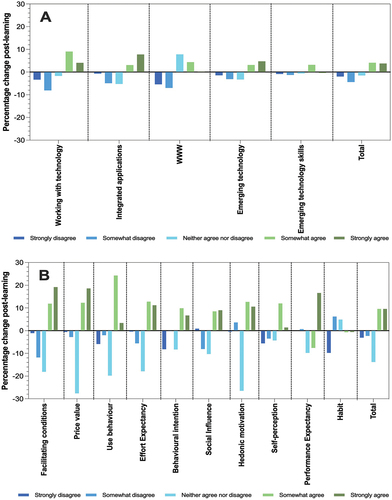
The ranking of the technology self-efficacy domain scores pre-learning in descending order is ‘emerging technology skills’ (93.1%), ‘integrated applications’ (84.48%), ‘emerging technology’ (83.1%), ‘internet’ (79.54%) and ‘working with technology’ (76.32%). This order did not change post-learning, and scores were 94.18%, 89.47%, 86.82%, 84.08% and 82.72%, respectively.
There were no associations with gender, number of devices, frequency of online use and pre-learning technology self-efficacy total scores (p = 0.72).
Telehealth acceptance
shows the pre- and post-learning telehealth acceptance scores in total and for each domain. The values and Cronbach’s alpha are also shown in . In , the domains are ranked according to the change in scores post-learning. The domains that had the greatest improvement in score post-learning were ‘facilitating conditions’ (+12.86%), with ‘habit’ (+2.33%) having the least improvement in score. The total telehealth acceptance scores (average ± standard deviation) pre- and post-learning were 66.1% ± 9.6 and 73.98% ± 9.9.
and show the percentage of students in each score range pre- and post-learning for telehealth acceptance.
The distribution of change in responses (strongly disagree to strongly agree) for the telehealth acceptance survey is shown in and .
The ranking of the telehealth acceptance scores pre-learning in descending order is ‘performance expectancy’ (81.15%), ‘effort expectancy’ (70.86%), ‘facilitating conditions’ (70%), self-perception’ (68.97%), ‘price value’ (68.74%), ‘use behaviour’ (65%), hedonic motivation’ (64.94%), social influence’ (63.1%), ‘behavioural intention’ (58.85%), and ‘habit’ (43.79%). This order changed post-learning for the second to fifth positions to be ‘performance expectancy’ (86.12%), ‘facilitating conditions’ (82.86%), ‘price value’ (79.46%), ‘effort expectancy’ (79.18%), ‘self-perception’ (74.9%), ‘use behaviour’ (73.98%), hedonic motivation’ (71.16%), social influence’ (69.66%), ‘behavioural intention’ (66.8%), and ‘habit’ (46.12%).
There were no associations with gender, number of devices, frequency of online use and pre-learning telehealth acceptance scores (p = 0.37). Twenty-three (46.94%) participants indicated that they had prior telehealth experience. Prior telehealth experience, gender and age had no associations with post-learning acceptance scores (0.34).
Relationship between technology self-efficacy and telehealth acceptance
Correlation between technology self-efficacy and telehealth acceptance was insignificant pre-learning (p = 0.3) but was significant post-learning (p = 0.04).
Discussion
Despite the obvious benefits of telehealth and the introduction of reimbursement for telehealth in Australia,Citation21 telehealth adoption by health practitioners has been reported to be less than expected between 2011 and 2014. In optometry, telehealth adoption appears to be positive after the introduction of new MBS telehealth item numbers in 2015.Citation22 However, this mainly involved collaborative patient care with ophthalmologists in rural and remote Australia.Citation22 It is unclear how telehealth is being utilised in the day-to-day practice of Australian optometrists practising in non-rural areas, and more can be done in understanding the challenges of telehealth implementation and supporting telehealth practice in optometric care. In exploring the barriers to telehealth adoption, the focus of this study included technology self-efficacy, behavioural factors of telehealth acceptance and how telehealth training alters these factors in optometry students.
The high number of device usage and frequency of device use found in this study were consistent with previous studies on graduate students.Citation23,Citation24 This frequent use of technology on multiple devices was not associated with pre-learning technology self-efficacy and telehealth acceptance scores. There is limited literature on this topic, with one study reporting an association between increased home computer use and increased self-efficacy among undergraduate college students.Citation25 Other studies have reported that high technological usage does not translate to technology competenciesCitation23,Citation26,Citation27 and technology competencies of university students can be inadequate.Citation23,Citation28 Altogether, these findings suggest that daily use of technological devices does not reflect capabilities and acceptance in utilising technology in the patient care of healthcare students.
Previous studies have reported an average of ~77% computer-related self-efficacy score in pharmacy studentsCitation8 and that Internet self-efficacy was higher in nursing students (~69%) compared to nurses (~63%).Citation29 In this study, TPSA C-21, which has been shown to have good reliability,Citation19 was adapted to assess perceptions about the ability of students to use a wide range of technology. The high technology self-efficacy scores indicate that optometry students have a high ability to overcome barriers in using technology as a health professional. Martin et al. (2002) utilised a telehealth self-efficacy survey to examine perceived knowledge, skills and self-efficacy pre- and post-telehealth learning among physiotherapy students, reporting a significantly higher score post-learning.Citation30 In the current study, improvements in scores post-learning improvements in technology self-efficacy scores are small and less when compared to telehealth scores. This might be due to students demonstrating high self-efficacy scores pre-learning, leaving a smaller room to demonstrate improvement post-learning. In line with this, the lowest ranking domain, ‘working with technology’ had the greatest improvement, where students perceived that they are more capable of using technology to collaborate, budget, and describe software used in their provision of healthcare post-learning.
The domain that students demonstrated the highest efficacy ‘emerging technology skills’, including skills such using cloud-based environments, downloading, and streaming videos, and sending and transferring photos on smartphones, had the least improvement.
Several theoretical models have been developed from theories in psychology and sociology and employed to explain technology acceptance and use.Citation31 In this study, UTAUT-2 with 10 domains,Citation20 which has been shown to be a suitable model for eHealth technologies,Citation20,Citation32 was adapted. In contrast to previous studies using statistical modelling to identify factors/domains determining acceptance of telehealth technology among physicians,Citation33 a descriptive data analysis approach was used to examine the telehealth acceptance levels of optometry students pre- and post-learning in this study.
There are no previous studies examining telehealth acceptance levels of healthcare students using descriptive methods. In this study, the pre-learning score indicates that optometry students are moderately accepting of telehealth and training improved telehealth acceptance overall. This improvement is consistent with previous studies reporting benefits of telehealth education.Citation13 Descriptive analysis allowed inquiry into the extent of impact on each factor/domain post-learning. Not surprisingly, optometry students perceived an increase in telehealth resources and support, with ‘facilitating conditions’ having the greatest improvement in score post-learning. The improvement in the degree that telehealth will be used automatically, ‘habit’, was the least. Students scored less than 50% in ‘habit’, and this domain was ranked the last against other domains pre- and post-learning. This indicates that using telehealth spontaneously might require more than an entry to practice telehealth curriculum in preparing and aiding optometry students to practice telehealth when they graduate.
Training also resulted in positive improvements in all other domains, where students perceived greater benefits of using telehealth to be greater than the monetary cost (price value); greater frequency of telehealth use (use behaviour); greater ease of telehealth use (effort expectancy); greater intent to telehealth use (behavioural intent); greater perception of how important others believe they should use telehealth (social influence); greater internal motivation (hedonic motivation) and greater perception of telehealth as part of their health belief model (self-perception). Students also perceived telehealth as a great benefit to their practice, with performance expectancy ranking first pre- and post-learning. More studies are required to investigate the long-term effects of training and if training resulted in telehealth adoption in practice.
High self-efficacy has consistently been shown as a significant predictor of positive technology acceptance and adoption for healthcare workers,Citation6,Citation7,Citation34 healthcare studentsCitation8 and consumers.Citation35,Citation36 This current study did not demonstrate a significant association between technology self-efficacy and telehealth acceptance pre-learning, but an association (p = 0.04) post-learning. This suggests the value of telehealth training in the acceptance and adoption of telehealth practice.
An online curriculum designed for entry to practice University of Melbourne healthcare students including students from physiotherapy, audiology, speech therapy, social work, nursing, and optometry was delivered in this study. In providing online training to optometry students, five modules were introduced with the last two modules including critical reflection, and simulation were not delivered due to logistical challenges.
Literature on telehealth curriculum, although scarce has described methods of delivery including theoretical teachings, didactic learning, online learning, experiential learning and learning through simulation and interprofessional education.Citation12,Citation13 PhysiotherapyCitation30 and nursingCitation30 students who had simulation incorporated into their learning expressed intention to use telehealth in their future careers post-learning, supporting the effectiveness of incorporating simulation in telehealth education. Research has also demonstrated that critical reflectionCitation37 and simulationCitation38 aid in developing clinical skills, and it is likely that optometry students will demonstrate a greater telehealth acceptance if the last two modules were delivered.
The use of telehealth might imply a change in clinical practice for both students and practitioners, and this requires support through education. Optometry Australia has developed a clinical practice guide to telehealth to aid optometrists in telehealth adoption.Citation2 Integrating telehealth education into an already crowded university curriculum can be a challenge. Recommended competency-based outcomes by accrediting bodies can guide the implementation of appropriate curriculum content.Citation39 At this stage, ‘communication’ is the only competency made explicit for telehealth in the Optometry Australia Entry-Level Competency Standards for Optometry (2022).Citation14 To prepare graduates for telehealth use at work, accrediting bodies and educators can state explicitly how other competencies such as professionalism and privacy relate to the provision of telehealth care. More research is required to establish evidence-based best practice guidelines and in understanding the long-term effects of telehealth training and telehealth use in practice.
This study is the first to comprehensively examine technology self-efficacy, telehealth acceptance before and after an online telehealth course for optometry students. A limitation of this study is that only one optometric institution was involved with a moderate response rate. There is a possibility that self-selecting participants, coupled with the time invested in telehealth training resulted in a bias that leans towards positive telehealth acceptance scores post-learning. Additionally, having anonymous survey participation did not allow statistical methods to be applied in studying pre- and post-learning effects, and association with telehealth training scores. Nonetheless, this study demonstrates that high-technology self-efficacy did not translate to similar scores for telehealth acceptance and online training resulted in higher telehealth scores, improving this relationship.
The barriers to telehealth adoption are wide-ranging,Citation40 and more work is required in understanding current telehealth practices and attitudes in optometry, challenges in telehealth adoption, and telehealth curriculum effectiveness. Understanding these will help educational institutions, professional bodies, and policymakers in making decisions to support the implementation of telehealth successfully, in providing safe and effective care to the community.
Acknowledgements
The authors would like to thank all the students that participated in this study. Further, the Universitas 21 Health Sciences Group and University of Melbourne Learning and Teaching Initiative for funding to support to develop the telehealth training program.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Sood S, Mbarika V, Jugoo S et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health 2007; 13: 573–590. doi: 10.1089/tmj.2006.0073.
- Optometry Australia. Telehealth clinical practice guide. May 2021. https://www.optometry.org.au/wp-content/uploads/Professional_support/Guidelines/OPT003_Telehealth-Clinical-Practice-Guide_210520.pdf
- O’Day R, Smith C, Muir J et al. Optometric use of a teleophthalmology service in rural Western Australia: comparison of two prospective audits. Clin Exp Optom 2016; 99: 163–167. doi: 10.1111/cxo.12334.
- Bartnik SE, Copeland SP, Aicken AJ et al. Optometry-facilitated teleophthalmology: an audit of the first year in Western Australia. Clin Exp Optom 2018; 101: 700–703. doi: 10.1111/cxo.12658.
- Massie J, Block SS, Morjaria P. The role of optometry in the delivery of eye care via telehealth: a systematic literature review. Telemed J E Health 2022; 28: 1753–1763. doi: 10.1089/tmj.2021.0537.
- Vitari C, Ologeanu-Taddei R. The intention to use an electronic health record and its antecedents among three different categories of clinical staff. BMC Health Serv Res 2018; 18: 194. doi: 10.1186/s12913-018-3022-0.
- Dillon TW, Lending D. Will they adopt? Effects of privacy and accuracy. J Comput Inf Syst 2010; 50: 20–29.
- Jacobs RJ, Caballero J, Parmar J et al. The role of self-efficacy, flexibility, and gender in pharmacy students’ health information technology readiness. Curr Pharm Teach Learn 2019; 11: 1103–1110. doi: 10.1016/j.cptl.2019.07.016.
- Bandara A. Social foundations of thought and action. Englewood Cliffs NJ 1986; 1986: 2.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977; 84: 191–215. doi: 10.1037/0033-295X.84.2.191.
- Moore MA, Coffman M, Jetty A et al. Family physicians report considerable interest in, but limited use of, telehealth services. J Am Board Fam Med 2017; 30: 320–330. doi: 10.3122/jabfm.2017.03.160201.
- Edirippulige S, Armfield NR. Education and training to support the use of clinical telehealth: a review of the literature. J Telemed Telecare 2017; 23: 273–282. doi: 10.1177/1357633X16632968.
- Chike-Harris KE, Durham C, Logan A et al. Integration of telehealth education into the health care provider curriculum: a review. Telemed J E Health 2021; 27: 137–149. doi: 10.1089/tmj.2019.0261.
- Entry-level competency standards for optometry 2022. Optometry Australia; 2022. https://www.optometry.org.au/wp-content/uploads/Professional_support/Guidelines/Final_Entry-level-Competency-Standard-for-Optometry-2022.pdf.
- Bulik RJ, Shokar GS. Integrating telemedicine instruction into the curriculum: expanding student perspectives of the scope of clinical practice. J Telemed Telecare 2010; 16: 355–358. doi: 10.1258/jtt.2010.090910.
- Brockes C, Grischott T, Dutkiewicz M et al. Evaluation of the education “clinical telemedicine/e-health” in the curriculum of medical students at the university of zurich. Telemed E-Health 2017; 23: 899–904. doi: 10.1089/tmj.2017.0011.
- Erickson CE, Fauchald S, Ideker M. Integrating telehealth into the graduate nursing curriculum. J Nurse Practitioners 2015; 11: e1–e5. doi: 10.1016/j.nurpra.2014.06.019.
- Rutledge CM, Haney T, Bordelon M et al. Telehealth: preparing advanced practice nurses to address healthcare needs in rural and underserved populations. Int J Nurs Educ Scholarsh 2014; 11: 1–9. doi: 10.1515/ijnes-2013-0061.
- C R, K G. Validating the technology proficiency self-assessment questionnaire for 21st Century learning (TPSA C-21). J Digit Learn Teach Educ 2017; 33: 20–31. doi: 10.1080/21532974.2016.1242391.
- Tavares J, Oliveira T. Electronic health record patient portal adoption by health care consumers: an acceptance model and survey. J Med Internet Res 2016; 18: e49. doi: 10.2196/jmir.5069.
- Wade V, Soar J, Gray L. Uptake of telehealth services funded by medicare in Australia. Aust Health Rev 2014; 38: 528–532. doi: 10.1071/AH14090.
- Turner A, Copeland S, Aicken A Optometry-facilitated videoconference uptake in Western Australia following introduction of new MBS item numbers. CLINICAL AND EXPERIMENTAL OPHTHALMOLOGY; 2016: WILEY-BLACKWELL 111 RIVER ST, HOBOKEN 07030-5774, NJ USA.
- Cham K, Edwards ML, Kruesi L et al. Digital preferences and perceptions of students in health professional courses at a leading Australian university: a baseline for improving digital skills and competencies in health graduates. Australas J Educ Technol 2022; 38: 69–86. doi: 10.14742/ajet.6622.
- Perifanou M, Tzafilkou K, Economides AA. The role of Instagram, Facebook, and YouTube frequency of use in university students’ digital skills components. Educ Sci 2021; 11: 766. doi: 10.3390/educsci11120766.
- McCoy C. Perceived self-efficacy and technology proficiency in undergraduate college students. Comput Educ 2010; 55: 1614–1617. doi: 10.1016/j.compedu.2010.07.003.
- Burton LJ, Summers J, Lawrence J et al. Digital literacy in higher education: the rhetoric and the reality. In: Harmes M, Huijser H Danaher P, editors. Myths in education, learning and teaching: policies, practices and principles. London: Palgrave Macmillan UK; 2015. p. 151–172.
- McLachlan CA, Craig A, Coldwell-Neilson J. Students’ computing use and study: when more is less. Australas J Inf Syst 2016; 20. doi: 10.3127/ajis.v20i0.990.
- Gibadullin A. Assessing digital skills in tertiary students. In 2021 International Scientific and Practical Conference “‘Information Technologies and Intelligent Decision Making Systems’”, Russian Federation, Moscow: ITIDMS 2021; 2021.
- Warshawski S, Itzhaki M, Barnoy S. Nurse and nurse student attitudes and perceived self-efficacy in use of information and communication technologies: professional and cultural differences. Comput Inf Nurs 2019; 37: 20–28. doi: 10.1097/CIN.0000000000000470.
- Martin R, Mandrusiak A, Lang R et al. A telehealth curriculum: a pre-post study of physiotherapy students’ perceived knowledge, self-efficacy and intentions for future use. Focus Health Prof Educ 2022; 23: 56–72. doi: 10.11157/fohpe.v23i3.595.
- Venkatesh V, Morris MG, Davis GB et al. User acceptance of information technology: toward a unified view. Mis Q 2003; 27: 425–478. doi: 10.2307/30036540.
- Venkatesh V, Thong JY, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. Mis Q 2012; 36: 157–178. doi: 10.2307/41410412.
- Garavand A, Aslani N, Nadri H et al. Acceptance of telemedicine technology among physicians: a systematic review. Inf Med Unlocked 2022; 30: 100943. doi: 10.1016/j.imu.2022.100943.
- Ma Q, Liu L. The role of internet self-efficacy in the acceptance of web-based electronic medical records. J Organ End User Comput 2005; 17: 38–57. doi: 10.4018/joeuc.2005010103.
- Rahman MS, Ko M, Warren J et al. Healthcare technology self-efficacy (HTSE) and its influence on individual attitude: an empirical study. Comput Hum Behav 2016; 58: 12–24. doi: 10.1016/j.chb.2015.12.016.
- Simon SR, Evans JS, Benjamin A et al. Patients’ attitudes toward electronic health information exchange: qualitative study. J Med Internet Res 2009; 11: e30. doi: 10.2196/jmir.1164.
- Mann K, Gordon J, MacLeod A. Reflection and reflective practice in health professions education: a systematic review. Adv Health Sci Educ 2009; 14: 595–621. doi: 10.1007/s10459-007-9090-2.
- Motola I, Devine LA, Chung HS et al. Simulation in healthcare education: a best evidence practical guide. AMEE guide No. 82. Med Teach 2013; 35: e1511–e1530. doi: 10.3109/0142159X.2013.818632.
- Stovel RG, Gabarin N, Cavalcanti RB et al. Curricular needs for training telemedicine physicians: a scoping review. Med Teach 2020; 42: 1234–1242. doi: 10.1080/0142159X.2020.1799959.
- Scott Kruse C, Karem P, Shifflett K et al. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018; 24: 4–12. doi: 10.1177/1357633X16674087.