Abstract
Objective: Worry is an important perpetuating factor of Medically Unexplained Symptoms (MUS). Former research has shown that a worry postponement instruction is effective in reducing Subjective Health Complaints (SHC) in non-clinical samples. This study aimed to (1) replicate these findings in a MUS-analogue student-sample and (2) assess alexithymia as a moderator.
Design: The current study had an experimental design with two waves of data collection: pre- and post-intervention.
Main outcome measures: A MUS-analogue student-sample consisting of 114 undergraduate students with high self-reported health worry and a minimum of two doctor visits in the previous year with no current diagnosis for a (chronic or acute) disease were instructed to register their worry frequency and duration eight times per day via an experience sampling-application on their smartphones. The intervention group additionally postponed their worries to a 30-minute period in the evening. SHC were assessed pre- and post-intervention.
Results: The intervention did not have an effect on worry or SHC. Alexithymia did not moderate this effect (p’s > .05).
Conclusion: Our study did not find evidence for the effectiveness of the worry reduction intervention on SHC in a MUS-analogue student-sample. This finding contributes to several previous studies that have found mixed evidence for the effectiveness of the worry reduction intervention on SHC and suggests that the worry intervention may not be effective in all cases.
Subjective Health Complaints (SHC), such as fatigue, gastrointestinal problems and musculoskeletal pain, are extremely common. In the Netherlands, SHC score second place on the top 10 list of the most important reasons to consult a General Practitioner (GP; Hammond, Citation1964; Picavet & Schouten, Citation2003; van de Lisdonk, van den Bosch, Huygen, & Lagro-Janssen, Citation1999). One in five people presenting with such SHC in primary care has Medically Unexplained Symptoms (MUS; Barsky & Borus, Citation1995; de Waal, Arnold, Eekhof, & van Hemert, Citation2004). MUS are symptoms without a clear medical cause (Olde Hartman et al., Citation2013; van der Weijden, van Velsen, Dinant, van Hasselt, & Grol, Citation2003). Consequently, GPs cannot adequately help people suffering from these symptoms. This often results in unnecessary referrals to other medical professionals and to unproductive medical procedures. Consequently, MUS are responsible for a poor health-related quality of life and high health care costs (Tveito, Passchier, Duivenvoorden, & Eriksen, Citation2004). Because of the lack of a medical cause for these symptoms, cognitive-behavioural models are used to understand and to treat MUS. These models describe predisposing and perpetuating psychosocial factors of MUS. One important perpetuating factor for physical symptoms in MUS-patients is repetitive negative thinking (Deary, Chalder, & Sharpe, Citation2007). Repetitive negative thinking (i.e. worry and rumination) is defined as a thinking style focussing on problems (current, past, or future) and negative experiences (past or anticipated). This thinking style is characterised by being repetitive, intrusive, and difficult to disengage from. Also, people experience this thinking style as unproductive and capturing their cognitive capacity (Ehring et al., Citation2011).
Thinking in a repetitive negative way about a stressor has been identified as a mechanism prolonging the effect of a stressor on somatic health (Brosschot & Thayer, Citation2004). Based on these findings, Brosschot, Gerin, and Thayer (Citation2006) formulated the ‘perseverative cognition hypothesis’ which indicates that repetitive negative thinking prolongs the physiological stress response and this in turn will lead to negative health consequences, including SHC. In line with this hypothesis, repetitive negative thinking is found to be associated directly with SHC such as fatigue, lower back pain and other pains (Freeston et al., Citation1996; Verkuil, Brosschot, Meerman, & Thayer, Citation2012). In addition, and importantly, such negative health consequences have been reported not only in clinical samples but also in persons who worry and ruminate at a non-clinical level (Brosschot & van der Doef, Citation2006).
The association between repetitive negative thinking and SHC inspired a study in which the prospective relation between worry and SHC was assessed by testing the efficacy of a simple worry postponement instruction in adolescents aged 15–19 years (Brosschot & van der Doef, Citation2006). In this worry reduction intervention, participants were instructed to only register their worries (control group) or to additionally postpone their worries to a 30-minute ‘worry-window’ in the evening (intervention group). Results showed that participants in the intervention group reported significantly less SHC and significantly shorter worry episodes. Similar results were obtained when the worry reduction intervention was later tested among teachers and in a child community sample, aged 9–13 years (Jellesma, Verkuil, & Brosschot, Citation2009; Verkuil et al., Citation2012). However, a more recent study by Versluis, Verkuil, and Brosschot (2016) did not manage to replicate an effect of the worry reduction intervention on SHC. Versluis et al. (2016) tested the efficacy of an online version of the worry reduction intervention in a group of self-selected participants with a mean age of 36.23 (SD = 12.96) from the general population. The authors found that the participants who had received the instruction to postpone their worries, did not report less SHC, nor a reduction in worry frequency or worry duration, as compared to the control group.
In short, several studies have reported positive effects of the worry reduction intervention on SHC in diverse populations. However, the results of Versluis et al. (2016) suggest that the intervention may not work with every sample or with every method of sampling (e.g., on paper or online). Hence, it is important to identify when, for whom and under what conditions the intervention works best. Such knowledge would help to further optimise the worry reduction intervention and its application. So far, studies have only focused on SHC. However, given that worry has also been identified as a perpetuating factor for MUS, the worry reduction intervention might also prove to be effective in people with MUS. Testing alternative interventions for MUS-patients is important as the current treatment standard, Cognitive Behavioral Therapy (CBT; Borkovec & Sharpless, Citation2004; Borkovec, Wilkinson, Folensbee, & Lerman, Citation1983), only modestly improves symptoms and can only be delivered by a trained psychotherapist. As MUS patients typically seek treatment for their physical complaints, a worry reduction intervention by the patient’s GP may be more acceptable for MUS-patients than going to a psychotherapist for CBT.
In the current study, we included a MUS-analogue student sample with self-reported symptoms that are indicative of at least a mild MUS subtype. The mild MUS subtype includes patients that do not meet the formal DSM criteria for MUS diagnosis but who fall on the clinical spectrum for MUS. These patients infrequently seek help and reassurance for health-related worries concerning physical complaints for which no apparent physical illness is identified and make up approximately 80% of all MUS patients (Smith & Dwamena, Citation2007). The goal of our study was to assess the efficacy of the worry reduction intervention on SHC in a MUS-analogue student sample covering the lower end of the MUS spectrum.
To possibly further specify for whom the intervention may be effective, we included alexithymia as a possible moderator of the efficacy of the worry reduction intervention on SHC. Alexithymia is a personality trait, normally distributed across the general population, which entails a difficulty in identifying and labelling emotions and accompanying bodily sensations and has been found to be related to both repetitive negative thinking and to SHC and MUS, which makes it a relevant trait for this particular sample (Cohen et al., Citation1994; De Gucht, Fischler, & Heiser, Citation2004; Lumley et al., Citation1997; Panayiotou et al., Citation2015; Taylor et al., Citation1992). More specifically, it could be that the difficulty to identify and label bodily sensations in people with alexithymia may cause them to worry about the possible origin of these undefined bodily sensations resulting in further SHC. Furthermore, an inability to identify negative emotions and bodily sensations that accompany repetitive negative thinking may make it more difficult for individuals with alexithymia to identify and thus postpone their worrying. Hence, we expect that people high in alexithymic traits will benefit less from the intervention as compared to people low on alexithymic traits.
The present study used a similar experimental procedure as Brosschot and van der Doef (Citation2006) with one notable difference. In contrast to the paper and pencil method that was used by Brosschot and van der Doef (Citation2006) which asked participants to recall how often and how much they were worrying during the day, the current study used an Experience Sampling Method (ESM) to register worry. ESM is especially suitable for assessing behaviour in student populations because of the availability and popularity of smartphones (Free et al., Citation2013). ESM allows automated registration of the frequency and duration of worries in a reliable and ecologically valid manner, without the downside of a recall bias (Shiffman, Stone, & Hufford, Citation2008).
Method
Participants
Participants were undergraduate students who were selected via the online university participation system if they (1) indicated a minimum of two doctor visits during the previous year and (2) indicated a minimum score of 60 on a health worry-item: ‘I worry about my health’ (ranging from 1 [never] to 100 [always]). We selected participants on these two criteria as an average of two doctor visits and health-related worry are indicative of at least mild MUS subtype (Olde Hartman et al., Citation2013; Smith & Dwawema, 2007). Participants were excluded from participation if they were currently in treatment for a (chronic) disease that might account for elevated health complaints (e.g., heart disease and asthma). Participants were only included if they could understand and write in Dutch and if they had an iOS or Android smartphone to their disposal for the research period. The sample initially consisted of a total of 120 participants.1
Over the course of the study, six participants dropped out: because of college obligations (n = 2), because the study became too much of an effort (n = 3) and for unknown reasons (n = 1). In the end, a total of 114 participants (100 females) were included for analyses. The mean age in the remaining group was 20.26 years (SD = 1.99). Drop-outs did not differ from the remaining participant group on the baseline measures and drop-out was not related to condition (p’s > .05). All participants gave written consent before participating. Participants received course credit or 30 euros in vouchers for their participation.
Instruments
Experience-sampling application
Daily assessments were collected via an application for ESM (Real Life Exp Mobile app, Lifedatacorp). Participants downloaded the application on their smartphones. The app was programmed to randomly send participants eight notifications per day between the hours of 08.00 and 22.00 during the six-day research period. Participants were able to open the questionnaire by clicking on the notification. After arrival of the notification, participants had a 15-minute window to fill in the questionnaire. Time periods between the notifications were programmed to a minimum of half an hour.
Worry frequency
At each notification, participants indicated whether they were worrying at that moment (yes/no).
Worry duration
At each notification, participants estimated the number of minutes they had been worrying during the half hour before filling in the questionnaire by positioning a slider on a scale between 0 and 30 minutes.
Paper questionnaires
Several paper questionnaires were administered pre-intervention (T1) and post-intervention (T2).
Trait-repetitive negative thinking
A general tendency to engage in repetitive negative thinking was measured with the Dutch version of the Perseverative Thinking Questionnaire-15 (PTQ-15-NL; Ehring et al., Citation2011; ω = .93, CI [.92, .95]) and was administered pre-intervention. Omega-total is reported here, along with the CI, as research has shown that reporting omega-total as an estimate for internal consistency will lead to a more accurate and higher estimate of the internal consistency than Cronbach’s alpha (see for a discussion; McNeish, Citation2017; Peters, Citation2014). Omega-total was estimated using the userfriendlyscience package (version 0.7.1; Peters, Citation2018). The PTQ-15-NL consists of 15 statements scored on a 5-point Likert-scale ranging from 0 (‘never’) to 4 (‘always’). A total sum score was obtained by adding up the scores on all items. Higher scores indicate a higher tendency to engage in repetitive negative thinking.
Subjective health complaints
The Dutch version of the Subjective Health Complaints Inventory (SHCI; Eriksen, Ihlebaek, & Ursin, Citation1999) was administered pre- (ω = .75, CI [.68, .82]) and post-intervention (ω = .8, CI [.75, .86]). The SHCI reliably scores the number of somatic and psychological health complaints, as well as the duration of these complaints. The SHCI consists of the 29 most common health complaints (domains: musculoskeletal, pseudo-neurological, gastrointestinal complaints, allergy and the flu) which are scored on a 4-point Likert-scale ranging from 0 (‘not at all’) to 3 (‘severely’). Following Brosschot and van der Doef (Citation2006), the total number of SHC in the past week was used as the primary outcome variable in this study. Higher scores indicate a higher number of SHC.
Alexithymia
To assess alexithymia, the Dutch version of the Bermond-Vorst Alexithymia Questionnaire (BVAQ; Vorst & Bermond, Citation2001; ω = .87, CI [.73, .84]) was used pre-intervention. The BVAQ consists of 40 statements to assess alexithymia in a valid, reliable way. The statements are scored on a 5-point Likert-scale ranging from 1 (I totally agree) to 5 (I do not agree at all). A total sum score was obtained by adding up the scores on all items. Higher scores indicate higher levels of alexithymia.
Subjective worry change
To assess how participants subjectively scored their worry after the six-day period, participants rated how their worry had changed over the week (i.e. ‘Over the last week, my worrying …’) on a Visual Analogue Scale ranging from (became a lot less) to (became a lot more). A score was obtained by measuring the length of the line a participant drew in centimetres starting at zero (has not changed).
Worry window compliance
To assess to what extent participants in the intervention group complied with the worry window every evening, participants answered the following question: ‘How many times have you succeeded to do a worry-window over the last week?’, by choosing an option in the following range: 0–6 times.
Explorative questions
Several open questions were asked post-intervention to explore how participants handled the intervention. Also, body awareness was measured at pre- and post-intervention with the BAQ (Shields, Mallory, & Simon, Citation1989) to explore the possibility that the intervention would increase body awareness in participants. None of these measures are discussed in the present paper.2
Procedure
Before coming to the lab, participants were randomly assigned to either the intervention group (worry registration + postponement instruction) or to the control group (worry registration), with a random number table generated by the block.random function from the psych package (version 1.1.11; Revelle, Citation2017). When participants arrived at the lab for the baseline-measures (T1), the researcher explained the procedure and gave participants instructions, not mentioning the study aim. Participants were under the impression that the study goal was to register their worries. Participants filled out the questionnaires (SHCI, PTQ-15-NL, BVAQ) and received instructions on how to register their worries via the ESM-application. The intervention group received additional instructions on how to postpone their worries during the day (see the explanation on the intervention below). All participants received a verbal explanation of negative repetitive thinking based on the definition of Ehring et al. (Citation2011): Repetitive negative thinking (i.e. worry and rumination) is defined as a thinking style focussing on problems (current, past or future) and negative experiences (past or anticipated). This thinking style is characterised by being repetitive, intrusive and difficult to disengage from. Also, people experience this thinking style as unproductive and capturing their cognitive capacity. Participants started with the six-day research period after the day on which they came to the lab for the pre-measure. On the day after the last registration day (T2), participants came to the lab for the post-measure, where they filled out a set of questionnaires (SHCI, explorative questionnaire) and received a debriefing letter.
Intervention
The worry reduction intervention was implemented as described by Brosschot and van der Doef (Citation2006). The participants in the intervention group were instructed to postpone their worrying every time they realised they were worrying during the day, to a self-chosen 30-minute period late in the evening that they would reserve for worrying (i.e. ‘worry-window’). These participants received the following instructions:
Every time you find yourself worrying or ruminating or thinking in a negative, repetitive manner, please try your best to terminate these worries right away, and to ‘postpone’ them to a special, self-chosen 30-minute-time period in the evening that you will use to worry. If you do not succeed right away, please try again.
The instruction to postpone worries is a key component of CBT for Generalised Anxiety Disorder, which is called stimulus control (Borkovec & Sharpless, Citation2004; Borkovec et al., Citation1983). Brosschot and van der Doef (Citation2006) modified this instruction for the purpose of their study, with the difference being that participants in their study did not receive an instruction on the exact time of their worry-window. The current study followed the procedure by Brosschot and van der Doef (Citation2006) by letting participants choose the time of their worry window individually. In the case, participants received an ESM notification in the worry-window or immediately after, they were instructed to fill in the questions with regard to the half hour before the worry-window. Participants in the control group did not receive the instruction to postpone their worries to a later worry window. They simply registered their worry frequency and worry duration in response to the ESM notifications.
Data analysis
First, descriptive statistics of the dependent variables and baseline measures were examined. Second, bivariate Pearson correlations of the dependent variables and baseline measures were examined to explore the associations between these variables. Third, assumptions regarding the distributions of the variables included in the final model were checked. There were no violations regarding the assumptions of normality and homoscedasticity, and there were no univariate outliers (Field, Miles, & Field, Citation2012). Fourth, independent samples t-test were conducted to see whether there were differences between males and females on baseline measures. Fifth, a manipulation check for the effect of the intervention on worry frequency and worry duration was performed (in line with former research [e.g. Brosschot & van der Doef, Citation2006]) using t-tests for independent samples. These preparatory steps were conducted using SPSS, version 21.0 (IBM Corp, 2012).
To test the effect of the intervention on the number of SHC, to test alexithymia as a moderator of this effect, and worry duration and worry frequency as mediators of the effect, a final mediation/moderation-model was constructed. To prepare worry duration and worry frequency for inclusion in the final model, mixed-effects model analyses were used to extract per-participant random slope coefficients of worry frequency and worry duration. We chose to include per-participant random slope coefficients for worry frequency and worry duration as mediators in the final model, because these coefficients take the change over time into account. Mixed-effects models are the preferred choice in this case because of the nested structure of the daily worry assessments and the differing number of unanswered notifications between participants. In comparison to, for example, Repeated-Measures ANOVAs, mixed-effects models are better suitable for handling unbalanced designs and they account for dependencies in the data, which is especially important with ESM-data (Barr, Levy, Scheepers, & Tily, Citation2013). Mixed-effects models were estimated with the lmer and glmer functions from the package lme4 (version 1.1.12; Bates, Maechler, Bolker, & Walker, Citation2015) in RStudio (Rstudio, Citation2012), an integrated development environment for R (version 3.3.30; R Core Team, Citation2017).
Before running the models, model diagnostics for the dependent variables included in the mixed-effects models were examined following the recommendations of Bates, Maechler, Bolker, and Walker (Citation2014). There were no peculiarities regarding the model diagnostics. Two mixed-effects models were tested to be able to extract random-slope coefficients: one to assess the change in worry duration over time and one to assess the change in worry frequency over time. The former included worry duration as the dependent variable and the day of the week as the independent variable. The latter included worry frequency as the dependent variable and the day of the week as the independent variable.
Finally, the mediation/moderation-model was tested. To assess the effect of the intervention on the number of SHC, condition was added as the independent variable and the change in number of SHC over time (SHC T2-T1) was included as the dependent variable. Further, alexithymia was added as a moderator of this effect. The random slope-coefficients for worry frequency and worry duration were added as mediators of the effect. All predictors were centred within PROCESS. This analysis was performed using the PROCESS macro for SPSS with bias-corrected 95% Confidence Intervals using bootstrapping with 5000 resamples (model 5; Hayes, Citation2013). To control for the large number of tests, the significance was set at p < .01.
Results
Descriptive statistics
The final sample consisted of 100 females and 14 males. The intervention group (49 females, 8 males) and the control group (51 females, 6 males) both consisted of 57 participants. Descriptive statistics of the baseline measures, pre-intervention and post-intervention measures are presented per group in . The average score on trait-repetitive negative thinking was 27.26 (SD = 10.42), which is comparable to the mean scores of both a population without a disorder and a population with another disorder than anxiety or depression (Ehring et al., Citation2011). Male participants scored significantly higher on alexithymia (M = 102.54, SD = 28.50) compared to female participants (M = 87.80, SD = 17.00), t(111)= –2.69, p = .008. Men and women did not differ significantly on the other variables (all p’s > .05).
Table 1. Descriptive statistics of age, trait-perseverative negative thinking, alexithymia, and the pre- and post-measure of subjective health complaints
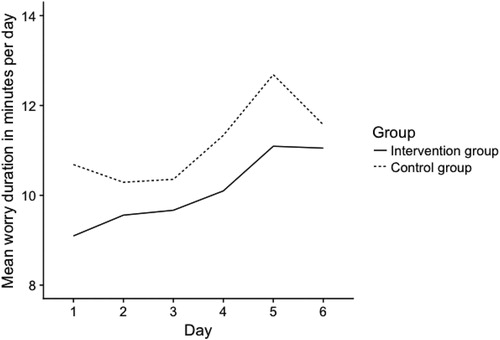
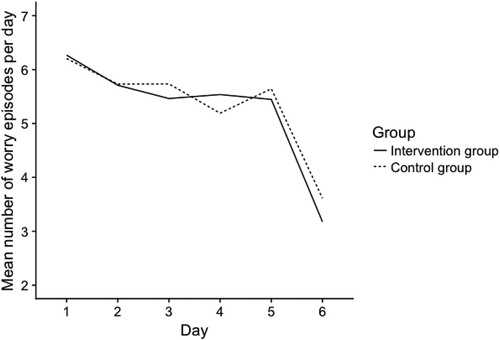
Descriptive statistics of worry frequency and worry duration are presented in . No differences were found regarding the mean number of minutes worried on day 1 between the control group (M = 10.10, SD = 6.79) and the intervention group (M = 9.03, SD = 6.56), p = .236. Both groups showed an increase in worry duration over the course of the week with a peak on day 6. No differences were found regarding the mean worry frequency on day 1 between the intervention group (M = 6.27, SD = 1.76) and the control group (M = 6.20, SD = 2.11), p = .451. Both groups showed a decrease in worry frequency over the course of the week, with a steeper drop on day 6. The worry variables are visualised in and .
Table 2. Descriptive statistics of worry frequency and worry duration throughout the week.
Correlations
Bivariate correlations between all constructs are presented in . As can be seen in , trait-repetitive negative thinking was positively associated with worry duration (r = .35, p < .001) and worry frequency (r = .25, p < .001), and with SHC, as measured at T1 (r = .36, p < .001) and at T2 (r = .37, p < .001). In addition, worry frequency related positively to SHC at T2 (r = .21, p = .028). Gender was positively related to alexithymia (r = .25, p = .008), indicating that the male gender is related to higher scores on alexithymia. The random slopes of worry duration and worry frequency were not significantly related to the difference score of SHC (p = .468 and p = .084, respectively), indicating disconfirmation of our hypothesis that a change in worry is related to a change in SHC.
Table 3. Bivariate correlations between all constructs.
Manipulation check
A t-test revealed that this version of the intervention did not have an effect on the slopes of worry duration (t(107) = 1.27; p = .206; d = .25) and worry frequency (t(107) = .26; p = .798, d = .05). Thus, contrary to expectations, the intervention to postpone worries to the evening did not reduce the frequency of worrying nor its duration in the current sample.
Effect of time on the worry variables
Two mixed-effects models were tested to assess whether there was an effect of time on worry duration and worry frequency using the lmer function and the glmer function of the lme4 package (version 1.1.12; Bates et al., Citation2015). The glmer function was used with a Poisson distribution to estimate a mixed-effects model for worry frequency, as worry frequency is a count variable and is estimated better when accounting for its non-normal distribution (Jaeger, Citation2008). The mixed-effects models included worry duration and worry frequency as dependent variables, fixed effects for day of the week and fixed intercepts. Also, a maximal random-effects structure was used, as advised by Barr et al. (2013) to model the repeated-measures nature of the data, by including random intercepts and random slopes of day of the week. Furthermore, all possible random correlation terms among random effects were included. For the worry duration model, p-values were determined using conditional F tests with Kenward-Roger correction for degrees of freedom, with the ANOVA function (using Type III F tests; car package, version 2.1.2; Fox & Weisberg, Citation2011) which in turn calls the KRmodcomp function (pbkrtest package, version 0.4.6; Halekoh & Højsgaard, Citation2014). For the worry frequency model, the anova function (base package, R Core Team, Citation2017) was used which uses Likelihood Ratio Tests to determine p-values.
The results of the mixed-effects model for worry duration showed a significant change of worry duration over time (B = 0.343, SE = 0.11, F(5, 93.42) = 3.32, p = .008). This indicates that over the days of the week, contrary to our expectation, worry duration increased, as can be seen in (see for descriptive statistics per day and per group). shows a decreasing trend of worry frequency over the days of the week for both groups. However, the results of the mixed-effects model for worry frequency showed a non-significant change of worry frequency over time (B = –.024, SE = 0.01; χ2 (1) = 3.02, p = .090).5 This indicates that over the days of the week, worry frequency did not change. Per-participant coefficients were subtracted for both models (coef. function, base package, R Core Team, Citation2017), to add them as predictors in the mediation model.
Effect of the worry reduction intervention on SHC
First, a repeated-measures analysis revealed a non-significant Time × Group interaction effect on SHC (F(1, 105) = 1.51; p = .223; η2 = .01). Next, the final moderation-model was created and tested within PROCESS (Hayes, Citation2013), despite the absence of a direct effect of the intervention on SHC, following the advice of many authors (e.g., Hayes, Citation2009; MacKinnon et al., Citation2000; Shrout & Bolger, Citation2002). The model included group (intervention group/control group) as the independent variable, the difference score of SHC (T2–T1) as the outcome variable, alexithymia as a moderator, the random slope coefficients of worry duration and worry frequency as mediators, and gender, trait-repetitive negative thinking and worry-window compliance as control variables. However, none of the tested predictors or paths were significant (p’s > .05, R2 = .04; see for coefficients for each of the predictors and paths). Thus, no evidence was found that the intervention has an effect on the number of SHC. Furthermore, alexithymia was not a moderator of the relationship, and worry frequency and worry duration were not mediators of the relationship; the model did not fit the data.
Table 4. Moderation model results for all predictors, the moderator and for the two mediators in the model for the effect on the difference score of SHCa (T2.17).
Discussion
In the current study, we aimed to test the effectiveness of the worry reduction intervention in reducing worry and SHC in a MUS-analogue student-sample. No evidence was found that the manipulation works: the intervention did not reduce worry duration nor worry frequency in this study. The intervention also did not have an effect on SHC. Moreover, worry frequency did not change over time, whereas worry duration did. The change in worry duration over time was not related to the change in SHC score from pre- to post-measure. We replicated the finding that participants who scored high on trait-repetitive negative thinking also reported more SHC, as predicted by the perseverative cognition hypothesis. Also, alexithymia did not moderate the relation between the intervention and SHC. Lastly, worry frequency and worry duration did not mediate the relation between the intervention and SHC. In short, this study did not find evidence to support the effectiveness of the six-day version of the worry reduction intervention in reducing neither worry, nor SHC in the current sample.
These findings are in line with a recent study by Versluis et al. (2016) that also could not replicate the effect of the intervention on both worry and SHC. The present study thus adds to the evidence that the intervention may not always be effective in every population. The present study and the study by Versluis et al (2016) appear to conflict with several earlier studies in which the intervention was found to be effective in reducing worry (Brosschot & van der Doef, Citation2006; Jellesma et al., Citation2009). In this regard, it is relevant to note that Brosschot and van der Doef (Citation2006) only found a marginally significant effect of the worry reduction intervention on worry frequency (Brosschot & van der Doef, Citation2006). This indicates that the effect of the intervention is not consistent across studies.
An explanation for the lack of evidence for an effect of the worry reduction intervention might involve the characteristics of the sample. The students in our analogue MUS-sample were selected on the basis of their high levels of health-related worry and on their relatively high number of doctor visits. In contrast, former studies have mostly included samples from the general population with relatively low worry scores (Brosschot & van der Doef, Citation2006; Jellesma et al., Citation2009; Verkuil et al., Citation2012). Hence, a possible explanation is that the worry intervention may only be effective in individuals with a low tendency to worry. The results of Versluis et al. (2016) are consistent with this interpretation as this study also did not find an effect of the intervention on worry duration, worry frequency and SHC in a population with relatively high scores on trait-worry. A possible explanation might be that for samples with relatively high tendency to worry, the intervention is perhaps not elaborate enough, or is too short to reduce the relatively high levels of worry and SHC. This explanation is supported by the data in : there is a stabilisation/decrease in worry duration after day 5, which could indicate a decreasing trend after day 5. Also, shows that the intervention group did show a slight decrease in SHC from pre- to post-intervention. These trends might be revealed by a longer assessment period and strengthened by a longer intervention period.
A second explanation might involve the worry content. The current sample was selected on high health-related worry, in contrast to samples in earlier research which were not selected on worrying (e.g., Brosschot & van der Doef, Citation2006; Verkuil et al., Citation2012). It could be that worrying about issues related to work, study obligations or relationships are easier to postpone than health-related worries, because health worries might be triggered by one’s current physical condition. For example, if a person suffers from lower back pain, he or she might find it hard to postpone his or her worries about the pain when currently experiencing pain. In line with this idea, Eccleston and Crombez (Citation2007) indicate that (chronic) pain is hard-wired to capture attention, may increasingly trigger worry and distress, and even result in hypervigilance for pain. Future research should include additional measures that assess experience of pain, as well as the success of participants to effectively postpone their worries, to investigate this hypothesis.
A third explanation might lie in the choice of the criterion for success. We have chosen, in line with former research, to assess the number of SHC from pre- to post-intervention. One characteristic of MUS-patients on the low end of the spectrum is that they do not necessarily have a lot of complaints, but rather that they have some SHC that are very persistent and bothersome. As our sample included MUS-analogue students, it might be that the intensity of their SHC has changed, rather than the number of their SHC. For example, if a MUS-patient is experiencing lower back pain, the intervention might cause the pain to become less intense, instead of causing it to disappear entirely. This explanation remains speculative, because the current study did not include any measures that can support this claim. Future research should take into account the intensity/severity of SHC to assess this explanation.
We found an increase in worry duration over time for both groups, which is in the opposite direction of what is usually found in this line of research. There are several explanations that may be considered for this unexpected finding. First, participants were instructed to fill out a minimum of 38 notifications (from a total of 48 notifications) throughout the week to get full course credit or vouchers. This instruction was intended to motivate participants to register their worries. However, this instruction might have caused participants to worry about whether they registered their worries often enough. This explanation is supported by the fact that multiple participants gave verbal feedback to the researcher that this occupied their minds during the week.
A second explanation might pertain to the methods that were used in this study. In this study, an ESM-application was used to send participants eight notifications per day to register their worries. ESM is known to be more intrusive than paper-pencil methods (Scollon, Kim-Prieto, & Diener, Citation2003). The notifications might have served as reminders for the participants that they were worrying. As a consequence, participants might have become more sensitised to the fact that they were worrying and may have worried about how much they were worrying, as can be explained by the literature on measurement reactivity: Responding to repeated measurements regarding cognitions or worries has the effect of creating new thoughts, including worries (Darker & French, Citation2009; French, Cooke, McLean, Williams, & Sutton, Citation2007; French & Sutton, Citation2010). This explanation is supported by the fact that the increase in worry duration was observed in both groups. However, an increase in negative emotions or worrying has been found to usually resolve within two or three days (see for a discussion, French & Sutton, Citation2010).
The current study had several strengths and limitations that are worth mentioning. First, this study included ESM to assess worry frequency and worry duration. Former research mostly used paper-pencil tasks, which have the drawback of introducing recall bias. ESM assesses the variables of interest in a more reliable way (Shiffman et al., Citation2008). However, as noted above, sampling of worry via ESM may have the downside of enhancing worry, as may have been the case in the present study. Second, in contrast to earlier studies, this study included a worry-window compliance measure, which was added as a control variable in the analyses. However, as our compliance measure was a one-time measure at the end of the intervention period, we recommend that future research includes a daily compliance measure. This would give a more precise indication of worry-window compliance. A limitation of our study is that our study sample was characterised by an underrepresentation of males: only 12% of the participants were male. The underrepresentation of males is quite common in research into repetitive negative thinking (e.g., Wittchen, Zhao, Kessler, & Eaton, Citation1994). In the present study, no effects of gender were found in the distributions of the dependent variables, which suggest that gender effects did not play a prominent role in the outcome of the study. We did find that male participants scored higher on alexithymia which is a normal finding in the alexithymia literature (e.g., Taylor et al., Citation1992).
In conclusion, this study suggests that students with SHC and health worries analogue to MUS-patients do not necessarily benefit from a six-day version of a worry-postponement intervention. Thereby this paper casts further doubt on the applicability of the worry reduction intervention as a general tool that is effective in all cases where repetitive negative thinking may influence health. However, one must view these conclusions in the light of the study’s limitations. Therefore, taking these limitations in mind, we still consider the worry reduction intervention as a potentially fruitful and effective technique to reduce repetitive negative thinking, SHC, and stress-related disease. It is important that future research invests in determining the factors that enable or prevent the worry reduction intervention to be effective such as individual differences in worry tendencies, effects of measurement or sampling method, the influence of pain or worry about health-related problems, duration of the intervention and instructions for compliance. It is our hope that these and related initiatives will contribute to a better understanding and treatment of SHC.
Notes
1 The sample size of 120 participants was determined a priori using G*Power (Faul, Erdfelder, Lang, & Buchner, 2007) with a 95% chance to detect a small effect size (d = 0.2; based on Brosschot & van der Doef, Citation2006) at an alpha level of .05.
2 These measures were included as part of a separate research question and will be discussed elsewhere. The data on these measures is available upon request from the authors.
3 Calculating and reporting effect sizes for mixed-models is currently still problematic and under debate (see for a discussion, Kramer, Citation2005). However, the coefficient can be interpreted as an unstandardized effect index. B = 0.34 in this case means that for every one unit increase, so each day of the week, worry duration increased by 0.34 minutes (20.4 seconds) for the entire sample.
4 B = –.02 in this case means that for every one unit increase, so each day of the week, worry frequency decreased by -.02 episodes for the entire sample (not-significant).
5 Exploratory correlation analysis indicated that there was no correlation between worry frequency and worry duration (r = .04) suggesting that there was no trade-off between the two worry measures. Future research may in fact combine worry duration and worry frequency in a single estimate of time spend worrying in order to rule out trade-off effects and obtain a single measure reflecting the amount of repeated negative thinking.
References
- Bagby, R. M., & Taylor, G. J. (1997). Affect dysregulation and alexithymia. In: G. J. Taylor, R. M. Bagby, & J. D. A. Parker (Eds.), Disorders of affect regulation: Alexithymia in medical and psychiatric illness (pp. 26–45). Cambridge: Cambridge University Press.
- Barr, D. J., Levy, R., Scheepers, C., & Tilly, H. J. (2013). Random effects structure for confirmatory hypothesis testing: Keep it maximal. Journal of Memory and Language, 68, 255–278. doi: 10.1016/j.jml.2012.11.001
- Barsky, A. J., & Borus, J. F. (1995). Somatization and medicalization in the era of managed care. JAMA, 274, 1931–1934.
- Bates, D., Maechler, M., Bolker, B., & Walker, S. (2014). lme4: Linear mixed-effects models using eigen and S4. R package version 1.1–7. Retrieved from http://CRAN.Rproject.org/package=lme4
- Bates, D., Maechler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67, 1–48. doi: 10.18637/jss.v067.i01.
- Borkovec, T. D. (1994). The nature, functions, and origins of worry. In G. C. L. Davey & F. Tallis (Eds.), Worrying. Perspectives on theory, assessment and treatment (pp. 5–33). New York, NY: Wiley.
- Borkovec, T. D., Robinson, E., Pruzinsky, T., & DePree, J. A. (1983). Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy, 21, 9–16. doi: 10.1016/0005-7967(83)90121-3
- Borkovec, T.D., & Sharpless, B. (2004). Generalized anxiety disorder: Bringing cognitive behavioral therapy into the valued present. In S. Hayes, V. Follette, & M. Linehan (Eds.), Mindfulness and acceptance expanding the cognitive behavioral tradition. New York, NY: Guilford Press.
- Borkovec, T. D., Wilkinson, L., Folensbee, R., & Lerman, C. (1983). Stimulus control applications to the treatment of worry. Behaviour, Research and Therapy, 21, 247–251. doi: 10.1016/0005-7967(83)90206-1
- Brosschot, J.F., Gerin, W., & Thayer, J.F. (2006). The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research, 60, 113–124. doi: 10.1016/j.jpsychores.2005.06.074
- Brosschot, J. F., & Thayer, J. F. (2004). Worry, perseverative thinking and health. In L. R. Temoshok (Ed.), Biobehavioral perspectives on health and disease (Vol. 6). New York, NY: Harwood Academic.
- Brosschot, J. F., & van der Doef, M. (2006). Daily worrying and somatic health complaints: Testing the effectiveness of a simple worry reduction intervention. Psychology and Health February, 21, 19–31. doi: 10.1080/14768320500105346
- Cohen, K., Auld, F., & Brooker, H. (1994). Is alexithymia related to psychosomatic disorder and somatizing? Journal of Psychosomatic Research, 38, 119–127. doi: 10.1016/0022-3999(94)90085-X
- Darker, C. D., & French, D. P. (2009). What sense do people make of a theory of planned behaviour questionnaire? A think-aloud study. Journal of Health Psychology, 14, 861–871. doi: 10.1177/1359105309340983
- De Gucht, V., Fischler, B., & Heiser, W. (2004). Neuroticism, alexithymia, negative affect, and positive affect as determinants of medically unexplained symptoms. Personality and Individual Differences, 36, 1655–1667. doi: 10.1016/j.paid.2003.06.012
- De Waal, M. W., Arnold, I. A., Eekhof, J. A., & van Hemert, A. M. (2004). Somatoform disorders in general practice: Prevalence, functional impairment and comorbidity with anxiety and depressive disorders. British Journal of Psychiatry, 184, 470–476. doi: 10.1192/bjp.184.6.470
- Deary, V., Chalder, T., & Sharpe, M. (2007). The cognitive behavioural model of medically unexplained symptoms: A theoretical and empirical review. Clinical Psychology Review, 27, 781–797. doi: 10.1016/j.cpr.2007.07.002
- Eccleston, C., & Crombez, G. (2007). Worry and chronic pain: A misdirected problem-solving model. Pain, 132, 233–236. doi: 10.1016/j.pain.2007.09.014
- Ehring, T., Zetscher, U., Weidacker, K., Wahl, K., Schönfeld, S., & Ehlers, A. (2011). The Perseverative Thinking Questionnaire (PTQ): Validation of a content-independent measure of repetitive negative thinking. Journal of Behavioral Therapy and Experimental Psychiatry, 42, 225–232. doi: 10.1016/j.jbtep.2010.12.003
- Eriksen, H. R., Ihlebæk, C., & Ursin, H. (1999). A scoring system for subjective health complaints (SHC). Scandinavian journal of public health, 27, 63–72. doi: 10.1177/14034948990270010401
- Faul, F., Erdfelder, E., Lang, A., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioural, and biomedical sciences. Behavioral Research Methods, 39, 175–191. doi: 10.3758/BF03193146
- Field, A., Miles, J., & Field, Z. (2012). Discovering statistics using R. Los Angeles, CA: Sage.
- Fox, J., & Weisberg, S. (2011). An {R} companion to applied regression (2nd ed.). Thousand Oaks, CA: Sage. Retrieved from http://socserv.socsci.mcmaster.ca/jfox/Books/Companion
- Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., … Haines, A. (2013). The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Med, 10, e1001362.
- Freeston, M. H., Dugas, M. J., Letarte, H., & Rheaume, J. (1996). Physical symptoms associated with worry in a nonclinical population. Journal of Anxiety Disorders, 10, 365–377. doi: 10.1016/0887-6185(96)00017-5
- French, D. P., Cooke, R., McLean, N., Williams, M., & Sutton, S. (2007). What do people think about when they answer theory of planned behaviour questionnaires? A think aloud study. Journal of Health Psychology, 12, 672–687. doi: 10.1177/1359105307078174
- French, D. P., & Sutton, S. (2010). Reactivity of measurement in health psychology: How much of a problem is it? What can be done about it? British Journal of Health Psychology, 15, 453–468. doi: 10.1348/135910710X492341
- Halekoh, U., & Højsgaard, S. (2014). A Kenward-Roger approximation and parametric bootstrap methods for tests in linear mixed models – the R package pbkrtest. Journal of Statistical Software, 59(9), 1–30. Retrieved from http://www.jstatsoft.org/v59/i09/.
- Hammond, E. C. (1964). Some preliminary findings on physical complaints from a prospective-study of 1,064,004 men and women. American Journal of Public Health and the Nation’s Health, 54, 11–23. doi: 10.2105/AJPH.54.1.11
- Hayes, A. F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76, 408–420. doi: 10.1080/03637750903310360
- Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: Methodology in the Social Sciences. Kindle Edition, 193.
- IBM Corp. Released. (2012). IBM SPSS statistics for windows, version 21.0. Armonk, NY: IBM Corp.
- Jaeger, T. F. (2008). Categorical data analysis: Away from ANOVAs (transformation or not) and towards logit mixed models. Journal of Memory and Language, 59, 434–446. doi: 10.1016/j.jml.2007.11.007
- Jellesma, F., Verkuil, B., & Brosschot, J. F. (2009). Postponing worrisome thoughts in children: The effects of a postponement intervention on perseverative thoughts, emotions and somatic complaints. Social Science & Medicine, 69, 278–284. doi: 10.1016/j.socscimed.2009.04.031
- Kramer, M. (2005). R2 statistics for mixed models. Conference on Applied Statistics in Agriculture. doi: 10.4148/2475-7772.1142
- Lumley, M. A., Tomakowsky, J., & Torosian, T. (1997). The relationship of alexithymia to subjective and biomedical measures of disease. Psychosomatics, 38, 497–502. doi: 10.1016/S0033-3182(97)71427-0
- MacKinnon, D. P., Krull, J. L., & Lockwood, C. M. (2000). Equivalence of the mediation, confounding, and suppression effect. Prevention Science, 1, 173–181. doi: 10.1023/A:1026595011371
- McNeish, D. (2017). Thanks coefficient alpha, we’ll take it from here. Psychological Methods. Advance online publication. doi:10.1037/met0000144
- Olde Hartman, T., Blankenstein, N., Molenaar, B., van den Berg, D. B., van der Horst, H., Arnold, I., Burgers, J., Wiersma, T., & Woutersen-Koch, H. (2013). NHG-Standaard Somatisch Onvoldoende verklaarde Lichamelijke Klachten (SOLK). Huisarts Wet, 56, 222–230.
- Panayiotou, G., Leonidou, C., Constantinou, E., Hart, J., Rinehart, K. L., Sy, J. T., & Björgvinsson, T. (2015). Do alexithymic individuals avoid their feelings? Experiential avoidance mediates the association between alexithymia, psychosomatic, and depressive symptoms in a community and a clinical sample. Comprehensive Psychiatry, 56, 206–216. doi: 10.1016/j.comppsych.2014.09.006
- Peters, G.-J. Y. (2014). The alpha and the omega of scale reliability and validity: Why and how to abandon Cronbach’s alpha and the route towards more comprehensive assessment of scale quality. The European Health Psychologist, 16, 56–69.
- Peters, G.-J. Y. (2018). userfriendlyscience: Quantitative analysis made accessible_. R package version0.7.1. Retrieved from https://userfriendlyscience.com>.
- Picavet, H. S. J., & Schouten, J. S. A. G. (2003). Musculoskeletal pain in the Netherlands: Prevalences, consequences and risk groups, the DMC3-study. Pain, 102, 167–178. doi: 10.1016/s0304-3959(02)00372-x
- R Core Team. (2017). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. Retrieved from http://www.R-project.org/
- RStudio Team (2012). RStudio: Integrated Development for R. RStudio, Inc., Boston, MA Retrieved from http://www.rstudio.com/.
- Revelle, W. (2017). psych: Procedures for personality and psychological research. Evanston, IL: Northwestern University. Retrieved from https://CRAN.R-project.org/package=psych Version = 1.7.5.
- Scollon, C. N., Kim-Prieto, C., & Diener, E. (2003). Experience sampling: Promises and pitfalls, strengths and weaknesses. Journal of Happiness Studies, 4, 5–34. doi: 10.1023/A:1023605205115
- Shields, S. A., Mallory, M. A., & Simon, A. (1989). The Body Awareness Questionnaire: Reliability and validity. Journal of Personality Assessment, 53, 802–815. doi: 10.1207/s15327752jpa5304_16
- Shiffman, S., Stone, A. A., & Hufford, M. R. (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415
- Shrout, P. E., & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7, 422–445. doi: 10.1037/1082-989X.7.4.422
- Smith, R. C., & Dwamena, F. C. (2007). Classification and diagnosis of patients with medically unexplained symptoms. Journal of General Internal Medicine, 22, 685–691. doi: 10.1007/s11606-006-0067-2
- Taylor, G. J., Parker, J. D. A., Bagby, R. M., & Acklin, M. W. (1992). Alexithymia and somatic complaints in psychiatric out-patients. Journal of Psychosomatic Research, 36, 417–424. doi: 10.1016/0022-3999(92)90002-J
- Tveito, T. H., Passchier, J., Duivenvoorden, H. J., & Eriksen, H. R. (2004). Subjective health complaints and health related quality of life in a population of health care workers. Psychology and Health, 19, 247–259. doi: 10.1080/08870440310001613491
- van de Lisdonk, E. H., van den Bosch, W. J., Huygen, F. J. A., & Lagro-Janssen, A. L. M. (1999). Psychische en Psychiatrische stoornissen. Ziekten in de huisartspraktijk [Psychological and psychiatric disorders. Morbidity in general practice]. Nijmegen: Elsevier/Bunge.
- van der Weijden, T., van Velsen, M., Dinant, G. J., van Hasselt, C. M., & Grol, R. (2003). Unexplained complaints in general practice: Prevalence, patients’ expectations, and professionals’ test-ordering behavior. Medical Decision Making, 23, 226–231. doi: 10.1177/0272989X03023003004
- Verkuil, B., Brosschot, J. F., Meerman, E. E., & Thayer, J. F. (2012). Effects of momentary assessed stressful events and worry episodes on somatic health complaints. Psychology and Health, 27, 141–158. doi: 10.1080/08870441003653470
- Versluis, A., Verkuil, B., & Brosschot, J. F. (2016). Reducing worry and subjective health complaints: A randomized trial of an internet‐delivered worry postponement intervention. British Journal of Health Psychology, 21, 318–335. doi: 10.1111/bjhp.12170
- Vorst, H. C. M., & Bermond, B. (2001). Validity and reliability of the Bermond-Vorst Alexithymia Questionnaire. Personality and Individual Differences, 30, 413–434. doi: 10.1016/S0191-8869(00)00033-7
- Wittchen, H. U., Zhao, S., Kessler, R. C., & Eaton, W. W. (1994). DSM-III-R generalized anxiety disorder in the national comorbidity survey. Archives of General Psychiatry, 51, 355–364. doi: 10.1001/archpsyc.1994.03950050015002