?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective: Based on the Health Action Process Approach, we tested the efficacy of a theory-based program using an online social media platform (Telegram) to promote good oral hygiene behaviour among Iranian adolescents.
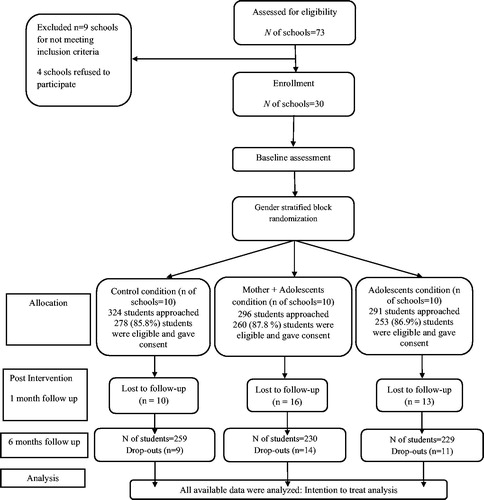
Design: A three-arm randomized-controlled trial design was used, consisting of an adolescent only intervention group (A group; n = 253), an adolescent and mother intervention group (A + M group; n = 260), and a control group (n = 278).
Main outcome measures: Psychosocial variables, toothbrushing behaviour, Visual Plaque Index, and Community Periodontal Index.
Results: Increases in adolescent toothbrushing at the one- and six-month follow-ups in both intervention groups compared to the control group were observed. Adolescents in the A + M group showed significant greater improvements in their toothbrushing behaviour, Visual Plaque Index, and Community Periodontal Index scores than adolescents in the A group. Improvements to toothbrushing social cognitions were also observed.
Conclusions: Current results support the use of the theory-based program delivered by Telegram in improving good oral hygiene behaviour and oral health outcomes among Iranian adolescents. Involving mothers in an intervention can confer additional benefits for adolescent oral health.
Clinicaltrials.Gov Number:
Approximately 60–90% of school-aged children suffer from dental caries in high-income countries (Petersen, Citation2003). Globally, the mean number of decayed, missing, and filling teeth (DMFT) in 15-year olds is the highest in the Eastern Mediterranean region, including Iran (Petersen, Citation2003). In 2008, the mean DMFT value for 15-year-old people in Tehran was reported to be approximately 2.1 (Yazdani, Vehkalahti, Nouri, & Murtomaa, Citation2008), and this value is even higher in the region of Qazvin where it has been reported at 2.61 for 14–18-year olds ( Pakpour, Hidarnia, Hajizadeh, Kumar, & Harrison, Citation2011) . Although oral diseases are largely preventable, and some may be reversed by regular performance of good oral hygiene behaviour, for example, regular toothbrushing with fluoride toothpaste (Davies, Davies, Ellwood, & Kay, Citation2003), studies have shown that adolescents do not perform these necessary oral self-care behaviours regularly (Pakpour, Yekaninejad, Sniehotta, Updegraff, & Dombrowski, Citation2014; Scheerman et al., Citation2017). Eleven percent of Iranian adolescents reported never using a toothbrush, and only 22% reported brushing their teeth at least once daily (Kazemnejad, Zayeri, Rokn, & Kharazifard, Citation2008). This emphasizes the urgent need for effective oral health promotion programs in this region.
Online social media platforms are readily available and versatile. Current data indicates that the majority of individuals access social media on a daily basis (Buis, Citation2011; Herold, Citation2018; Madden, Lenhart, Duggan, Cortesi, & Gasser, Citation2014). Social media can therefore be utilised to deliver behaviour change interventions and has the potential to aid with the enhancement of oral health (Godino et al., Citation2016; Patel, Chang, Greysen, & Chopra, Citation2015). To date, few randomized controlled trials have evaluated the use of online social media platforms as portals for intervention delivery (Badawy & Kuhns, Citation2017) and, at present, there is modest evidence that oral health interventions delivered by this approach are effective (Li et al., Citation2016; Zotti et al., Citation2016). Telegram is a popular social media platform that is open access and available for smartphones. It allows users to send messages and receive photographs, videos, audio, and data files, and has been reported as the most favoured and widespread software among Iranian students (Ebrahimpour et al., Citation2016).
Webb et al. (Citation2010) conducted a systematic review and meta-analysis to assess the characteristics of Internet-based interventions and their effectiveness in promoting health behaviour change. Interventions designed on behavioural theory and those with a greater number of behaviour change techniques were found to be most effective (Webb et al., Citation2010). Despite these findings, historically intervention development has rarely been informed by theories of behaviour change (Dombrowski, Sniehotta, Avenell, & Coyne, Citation2007). Given interventions based on theory provide most promise in effectively changing behaviour, intervention design, content, implementation, and evaluation should therefore be informed by appropriate theory. The Health Action Process Approach (HAPA) is a theoretical framework designed to better understand health behaviour change (Schwarzer, Citation2008).
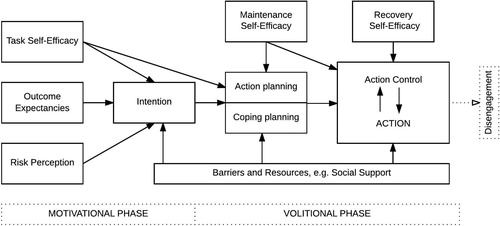
The HAPA describes the social-cognitive and self-regulatory processes that are involved in the adoption and maintenance of health behaviours (Schwarzer, Citation2008). It is based on the assumption that there is a distinction between a motivational and a volitional phase of behaviour, and that different psychological constructs are seen as being influential in each of the phases. In the motivational phase, factors such as perceptions of risk, outcome expectancies, and action self-efficacy are proposed to play an important role in motivating individuals into action. In the volition phase, coping self-efficacy, planning, and action control (such as self-monitoring) are proposed as key self-regulatory factors that are important in ensuring an intended behaviour is initiated, and then maintained once initiated (See , Schwarzer, Citation2008). Several studies have showed the usefulness of the HAPA in explaining oral health behaviour in general (Gholami, Knoll, & Schwarzer, Citation2015; Hamilton, Bonham, Bishara, Kroon, & Schwarzer, Citation2017; Hamilton, Cornish, Kirkpatrick, Kroon, & Schwarzer, Citation2018; Hamilton, Orbell, Bonham, Kroon, & Schwarzer, Citation2018; Lhakhang et al., Citation2016; Zhou, Sun, Knoll, Hamilton, & Schwarzer, Citation2015), and specifically in adolescents (Pakpour et al., Citation2016; Scheerman et al., Citation2016; Citation2017). There is also growing support for the effectiveness of HAPA-based interventions in the context of promoting oral hygiene behaviours (e.g. Lhakhang et al., Citation2016; Schüz, Sniehotta, Wiedermann, & Seemann, Citation2006; Schwarzer, Antoniuk, & Gholami, Citation2015; Hamilton, Bonham, Bishara, Kroon, & Schwarzer, Citation2017; Zhou et al., Citation2015), including mobile health (mHealth) interventions (Scheerman, et al., Citation2019).
Figure 1. The Health Action Process Approach model (Schwarzer, Citation2008).
The current study
The aim of the current study was to test the efficacy of a theory-based program delivered by the online social media platform (Telegram) to promote good oral hygiene behaviour and oral health outcomes among Iranian adolescents. Using the HAPA as a theoretical guide to intervention development, the social media program consisted of two components: an oral health education component and a behavioural coaching program comprising motivational and volitional components to promote regular toothbrushing. The intervention was directed solely at the adolescent (A group) with another arm directed at the adolescent and their mother (A + M group). This latter arm was decided important given parents have a central role in educating their children and encouraging and supporting healthy lifestyle choices (Christensen, Citation2004), with the main responsibility for oral health behaviour falling on mothers (Åstrøm, Citation1998). Also, an experimental study has shown the effectiveness of involving mothers in changing dietary behaviour in adolescents (Lin, Scheerman, Yaseri, Pakpour, & Webb Citation2017). In the A + M intervention group, in addition to the social media education and behavioural coaching material given as part of the A group, mothers were instructed to coach and monitor their child’s behaviour, to assist their child in making action and coping plans, and to encourage their child to accomplish their daily oral health behaviour tasks. To evaluate the effectiveness of the adolescent only and the adolescent + mother interventions in terms of changes in oral hygiene behaviour (i.e., toothbrushing) and oral health outcome, a passive control group was selected.
It was expected that adolescents randomized to the A group would exhibit greater improvements in oral hygiene behaviour and oral health outcomes at the follow-up assessments one and six months later than adolescents in the control group (Hypothesis 1). In addition, it was expected that adolescents randomized to the A + M group would exhibit greater improvements in oral hygiene behaviour and oral health outcomes at follow-up than adolescents in the A group (Hypothesis 2) and control group (Hypothesis 3). Finally, the HAPA-based self-regulatory factors were expected to be higher at follow-up in both the A and A + M intervention groups compared to the control group (Hypothesis 4), and that these would serve as mediators between intervention conditions and toothbrushing behaviour at follow-up (Hypothesis 5).
Methods
Participants and procedure
This study adopted a three-arm cluster randomized-controlled trial design: adolescent only Telegram group (A group), adolescent and mother (A + M group) Telegram group, and control group. Data was collected at baseline, and at 1 month and 6 months following baseline. Recruitment commenced January 2017 and was completed February 2018. All procedures were carried out in compliance with the Helsinki Declaration. The research protocol was approved by the Ethics Committee of Qazvin University of Medical Sciences (IR.QUMS.REC.1398.083) and was registered at clinicalgov.com (registration number: NCT03641885).
Adolescents (N = 791) aged 12–17 years were recruited from 30 out of 73 high schools in Qazvin city, Iran. Schools were eligible for the study if they were situated in Qazvin province and not currently engaged in an oral health education or promotion program. Sample size was calculated to detect significant differences in self-reported toothbrushing behaviour of 2 units per month (Pakpour et al., Citation2016) with an alpha level of 0.05, a power (1-β error probability) of 0.80, a coefficient of between-cluster variation of 0.05, the mean cluster size of 28 students (according to the formal report of the Organization for Education at Qazvin in 2018), and 20% drop-out. This corresponded to a total sample size of 233 adolescents needed in each group.
Adolescents and their mothers were eligible for the study if they met the following criteria: residents in the urban area of Qazvin city; access to Telegram via a smartphone; not engaged in other oral health education or research program; willing to participate and provided written informed consent before entry to the study; no physical and/or cognitive disabilities impeding the ability to perform oral hygiene activities. After determining eligibility for inclusion, adolescents and their mothers were informed about the study in a single face-to-face information session, after which they were requested to provide their contact information by completing and submitting a questionnaire via Google Forms and Telegram. Adolescents completed a baseline assessment that included clinical indicators of oral health status, self-reported measures of oral hygiene behaviour and the HAPA-based self-regulatory factors. These same measures were re-tested at 1 month and 6 months after baseline. After baseline assessment, the intervention was randomly allocated.
Random allocation and masking
A 1:1:1 cluster randomized controlled trial was designed with the schools (clusters) as units of randomization. Randomization was stratified for gender specific schools and was performed by an independent statistician (masked) using a computerized, random-number generator. The allocation sequence was sequentially numbered and stored in opaque sealed envelopes until intervention assignment. It was not possible to blind participants; however, the statistician and all outcome assessors were blind to treatment allocation throughout the study. Participants were randomised to one of the three study groups (A group, A + M group, or control group).
The study conditions
A group
For the A group, a dental professional and health scientist (JS) and a health psychologist (AP) created the content of the intervention that was delivered by the Telegram platform. The principal researcher (AP) created the Telegram channel named “بهداشت دهان و دندان” (translation: Dental Health) and invited participants to join by telephone. A number of behaviour change techniques (BCT) (Michie et al., Citation2013) were incorporated in the intervention for adolescents (see Supplementary Materials, ). Prior meta-analytic studies on theory-based interventions have found that, compared to interventions that used only a few BCTs, those that used multiple techniques were more effective in changing behaviour (Webb et al., Citation2010).
Table 1. Baseline characteristics by group.
Specifically, the A group intervention included general information on oral health behaviours as well as health risk information about poor oral hygiene practices. Information was also given about the positive consequences of daily toothbrushing and adolescents were encouraged to formulate their own potential pros and cons of regular toothbrushing. Further, instructions on and role modelling of effective behaviours, such as a three-minute video clip demonstrating effective toothbrushing, was provided. In addition, adolescents were asked to make concrete plans on when, where, and after what activity they would brush their teeth in future using the if-then formulation (Pakpour et al., Citation2016). Individual schools printed and disseminated forms on which these action plans could be created and enter into a weekly calendar and on which adolescents could monitor their behaviour at home. Adolescents were also asked to identify barriers and possible solutions by making coping plans, in order to increase adherence to their action plans (see Scheerman, van Empelen, van Loveren, & van Meijel, Citation2018). These volitional sheets were created by the principal researcher and were based on previous used volitional sheets on oral health behaviour (Scheerman, et al., Citation2018). During the intervention period, the Telegram account provided reinforcement by sending text-messages about the potential positive outcomes of dental cleaning.
After two weeks of intervention exposure, adolescents were asked to monitor their oral hygiene behaviour and oral health status by using disclosing tablets, taking selfies of their teeth, and sending photos to an additional channel that was created and owned by the principal researcher (AP). Prior instructions were given to the participants to use the disclosing tablets. This was done once a week, and three research associates compared the weekly photos and provided feedback on progress that had been made in a private Telegram conversation with individual adolescents. The progress reports were based information provided by the adolescents, i.e. the photos on which the amount of dental plaque was visualized by the disclosing tablets. Feedback included, for example, providing advice on effective oral hygiene behaviour techniques, such as appropriate cleaning advice, and/or praise on improvements noted.
A + M group
In addition to the A group intervention, in the A + M group a Telegram channel was created for mothers that instructed them to coach and monitor their child’s behaviour by checking their children’s plans and daily brushing activities. Where there were several children within the same family, only one child (the oldest) was included in the study. Mothers were also asked to encourage their adolescent to complete all intervention activities, and specifically assist them in creating their individual action and coping plans, and to help them accomplish their daily task and if needed to provide social support. Encouragement by mothers was conducted by using role modelling, i.e. mothers performing their own oral health behaviour.
Control group
Adolescents in the control group did not receive any intervention during the experimental phase of the intervention.
Measures
A range of clinical and self-reported outcome measures were assessed at baseline and follow-up. The primary outcome was change in self-reported frequency of toothbrushing (behaviour). Secondary outcomes included changes in Visual Plaque Index (VPI) and Community Periodontal Index (CPI), intention, outcome expectancy, risk perception, self-efficacy, self-monitoring, action planning, coping planning, perceived social support, and Oral Health Related Quality of Life (OHRQoL).
Clinical measures
Periodontal condition and plaque status of adolescents were examined by two trained dental professionals and assessed using the VPI and CPI. All clinical examinations were conducted during school hours in the health office of the schools under artificial light illumination. Serval instruments were used for these examinations including a mouth mirror attached to an intraoral LED light and a World Health Organization periodontal probe. The Turesky modification of the Quigley- Hein plaque index (VPI) was used to evaluate plaque scores on the buccal and lingual tooth surfaces using disclosing agent. The amount of plaque on each enamel block for each lingual and buccal surface was rated on a 6-point scale ranging from 0 = no plaque to 5 = plaque covering two thirds or more of the crown of the tooth (Turesky, Gilmore, & Glickman, Citation1970).CPI was used to assess periodontal condition. The mouth was divided into sextants and six sites of tooth index (i.e., teeth 16, 11, 26, 36, 31, and 46) were evaluated using a CPI probe. The CPI was recorded based on the following criteria: 0 = healthy, 1 = gingival bleeding after probing, 2 = presence of supra- or subgingival calculus, 3 = 4-5 mm periodontal pocket, and 4 = periodontal pocket of at least 6 mm (Ainamo et al., Citation1982). Inter- and intra-rater reliability were assessed in a separate sample of adolescents (n = 31; 16 boys and 15 girls) in prior to the trial. Intraclass Correlation Coefficients (ICC) were 0.96 and 0.95 for VPI and CPI, respectively, indicating acceptable interrater reliability.
Self-reported measures
To assess the frequency of toothbrushing behaviour, adolescents were asked to indicate “How many times in the past month have you brushed your teeth?”. The validity of the single item measure has been documented in previous studies (Pakpour, Hidarnia, Hajizadeh, & Plotnikoff, Citation2012; Pakpour et al., Citation2014; Pakpour & Sniehotta, Citation2012). Moreover, a correlation was detected between the self-reported toothbrushing behaviour and VPI (rho = 0.66, p < 0.001) as well as CPI (rho = 0.54, p < 0.001) in the baseline assessment of the current study. Behavioural intention towards toothbrushing was measured using a four-item scale (e.g. “I intend to brush my teeth twice a day in the future”), scored on a 5-point Likert scale ranging from 1 strongly disagree to 5 strongly agree. Outcome expectancies was assessed by six items (e.g. ‘‘If I brush my teeth regularly, my breath will be fresh’’), scored on a 5-point Likert scale ranging from 1= strongly disagree to 5 = strongly agree. Risk perceptions was measured using two items (e.g. “If I do not brush my teeth frequently, the risk of caries will be”), scored on a 5-point Likert scale ranging from 1 = very low to 5 = very high. Self-efficacy was measured by three items (e.g. ‘I am confident that I can brush my teeth twice a day in the future’), scored on a 5-point Likert scale ranging from 1= not at all true to 5 = exactly true. Perceived social support was measured by three items (e.g. ‘My parents encourage me to brush my teeth regularly), scored on a 5-point Likert scale ranging from ranging from 1 = strongly disagree to 5 = strongly agree. Self-monitoring was assessed by three items using the stem “I have consistently monitored…” followed by (a) “when to brush my teeth”, (b) “how often to brush my teeth”, and (c) “how to brush my teeth”; responses were rated on a scale ranging from 1 = not at all true to 5 = exactly true. Action planning was assessed with the stem item “I have made a detailed plan regarding…” followed by (a) “when to brush my teeth”, (b) “where to brush my teeth”, (c) “how to brush my teeth”, (d) “how often to brush my teeth”, and (e) “how much time to spend on brushing my teeth”; responses were rated on a scale ranging from 1 = strongly disagree to 5 = strongly agree. Coping planning was assessed with the stem item “I have made a detailed plan regarding…” followed by (a) “what to do if something interferes with my plans”, (b) “how to cope with possible setbacks”, (c) “what to do if I forget”, (d) “which good opportunities for action to take”, (e) “what to do in difficult situations to act according to my intentions”“, (f) “how to motivate myself”, (g) “how to cope with bleeding”, and (h) “how to cope with pain”; responses were rated on a scale ranging from 1 strongly disagree to 5 strongly agree. OHRQoL was measured using the Pediatric Quality of Life Inventory TM (PedsQLTM) Oral Health Scale. The scale comprises five items. All responses are reverse scored and transformed into a 0–100-point scale with higher scores representing better OHRQoL. The psychometric properties of the Iranian scale have been confirmed in previous studies (Lin, Kumar, & Pakpour, Citation2016; Pakpour, Yekaninejad, et al., Citation2011). All measures had satisfactory internal consistency (Cronbach’s α ranging from 0.79 to 0.94, see ).
Table 2. Descriptive statistics for outcome measures by time and group.
Statistical analysis
All analyses were performed using the intention-to-treat principle with MLwin 2.27. All reported p-values were set to 0.05. Before performing main analyses the distributions of residuals were examined; results showed that they were compatible with a normal distribution. A series of multilevel linear mixed models using a restricted iterative generalized least square (RIGLS) estimation procedure was used to examine change in outcome measures from baseline to six months after intervention. The effect size B presents the mean differences in outcome. To take into account that possible clustering of data, and correlations between the observations within the participants and between participants within the same schools, we used mixed models analysis. A three-level model was specified for the analyses of all outcome measures where repeated assessment (time) was entered at the first level, adolescent was entered at the second level, and school was entered at the third level. Potential confounding variables (i.e. age, gender, and mother’s education) were identified by univariate multilevel analyses and included in all models. To estimate indirect effects of the intervention on change in toothbrushing at six months through changes in social–cognitive variables at one month, a multilevel mediation analysis was performed according to methods suggested by Krull and MacKinnon (Krull & MacKinnon, Citation2001). According to Baron and Kenny (Citation1986) and Krull and MacKinnon (Citation2001), three criteria should be met to support mediation effects: (1) the independent variable (i.e. intervention) should be significantly associated with outcome (i.e. toothbrushing behaviour) (path “C” in Table 5); (2) the dependent variable (i.e. toothbrushing behaviour) should be significantly associated with potential mediator (i.e. outcome expectancy, risk perception, intention, self-efficacy, action planning and coping planning, and perceived social support) (path “A” in Table 5); and (3) the change score of the mediators significantly effect on the outcome.
Results
demonstrates the flow of participants throughout the trial. In total 791 adolescents (female = 332, male = 459; with a mean age of 15.3 years (SD = 1.3) participated in the study (A group, n = 253; A + M group, n = 260; and control group, n = 278) (). Drop out analyses showed no significant differences between nonparticipants and participants regarding sex, age, parents’ education or family income. The reasons for dropout included families changing place of residence and adolescent being absent from school on the day of the assessment. summarizes the descriptive statistics for the outcomes for the three conditions at each time point. show the point estimates and standard errors for the effects of the interventions and other covariates on outcome variables using multilevel mixed model analysis.
Table 3. Three-level linear mixed models predicting the effects of the intervention on tooth brushing (TB), dental plaque (DP), Parent Social Support (PSS), Outcome Expectancies (OE), Risk Perceptions (RP) and Self-monitoring (SM).
Table 4. Three-level Linear Mixed Models Predicting the Effects of the Intervention on Self-Efficacy (SE), Intention (INT), Action Planning (AP), Coping Planning (CP), community periodontal index (CPI), and oral health related quality of life (OHRQOL).
At the 1-month follow-up, three-level linear mixed effects models revealed that the frequency of toothbrushing among adolescents in both intervention groups was significantly higher than among those in the control group (B = 3.74, SE = 0.28 [p < 0.001] for M + A; B = 2.64, SE = 0.29 [p < 0.001] for A). As and indicate, adolescents in both intervention groups reported higher outcome expectancy (B = 1.01, SE = 0.08 [p < 0.001] for A; B = 0.44, SE = 0.09 [p < 0.001] for M + A), higher risk perceptions (B = 0.35, SE = 0.05 [p < 0.001] for A; B = 0.31, SE = 0.05 [p < 0.001] for M + A), higher self-efficacy (B = 0.34, SE = 0.06 [p < 0.001] for A; B = 0.48, SE = 0.05 [p < 0.001] for M + A), stronger intention (B = 0.39, SE = 0.06 [p < 0.001] for A; B = 0.60, SE = 0.07 [p < 0.001] for M + A), higher self-monitoring (B = 0.74, SE = 0.05 [p < 0.001] for A; B = 0.88, SE = 0.09 [p < 0.001] for M + A), higher action planning (B = 0.67, SE = 0.07 [p < 0.001] for A; B = 0.80, SE = 0.06 [p < 0.001] for M + A), higher coping planning (B = 0.58, SE = 0.08 [p < 0.001] for A; B = 0.76, SE = 0.07 [p < 0.001] for M + A), and better OHRQoL B = 2.82, SE = 1.33 [p < 0.05] for A; B = 2.87, SE = 1.30 [p < 0.05] for M + A) compared to those in control group at one month follow-up. The adolescents in M + A group perceived significantly more social support from their mothers compared to those in A group (B = 0.62, SE = 0.07 [p < 0.001]) and control group (B = 0.74, SE = 0.06 [p < 0.001].
Similar differences were found between the study groups for the frequency of toothbrushing at the six months follow-up (B = 3.90, SE = 0.27 [p < 0.001] for M + A; B = 2.78, SE = 0.29 [p < 0.001] for A). Regarding secondary outcomes, the adolescents in intervention groups showed improvements in outcome expectancy (B = 1.09, SE = 0.09 [p < 0.001] for A; B = 1.13, SE = 0.07 [p < 0.001] for M + A), risk perceptions (B = 0.39, SE = 0.04 [p < 0.001] for A; B = 0.38, SE = 0.05 [p < 0.001] for M + A), self-efficacy (B = 0.36, SE = 0.06 [p < 0.001] for A; B = 0.43, SE = 0.06 [p < 0.001] for M + A), intention (B = 0.44, SE = 0.06 [p < 0.001] for A; B = 0.66, SE = 0.08 [p < 0.001] for M + A), self-monitoring (B = 0.92, SE = 0.08 [p < 0.001] for A; B = 1.21 SE = 0.07 [p < 0.001] for M + A), action planning (B = 0.70, SE = 0.06 [p < 0.001] for A; B = 0.87, SE = 0.07 [p < 0.001] for M + A), coping planning (B = 0.59, SE = 0.07 [p < 0.001] for A; B = 0.80, SE = 0.06 [p < 0.001] for M + A), and OHRQoL (B = 9.82, SE = 1.53 [p < 0.05] for A; B = 11.98, SE = 1.20 [p < 0.05] for M + A) compared to those in control group at six month of follow-up. Adolescents in A group did not report an increased level of perceived social support compared to those in control group (p > 0.05). The adolescents in M + A group, however, reported significantly more perceived social support from their mothers compared to those in A and control groups at six months of follow-up.
The intervention effects on clinical oral measures were also examined using the linear mixed models. The results indicated that adolescents in both intervention groups showed a significant greater improvement in their VIP and CPI scores than adolescents in the control group at 1-month and 6-month follow-up (p < 0.01).
Multiple mediation models for psychosocial variables revealed that the intervention in M + A group could affect toothbrushing by increasing self-efficacy, self-monitoring, intention, perceived social support and coping planning (p < 0.01) (see Supplementary Materials, ).
Discussion
In general, adolescents allocate large amounts of time for mobile technology use yet often do not prioritize sufficient time to devote to oral hygiene behaviours (Kazmnejad et al., Citation2008; Madden et al., Citation2014). Mobile technology was therefore considered a useful tool to use to develop a theory-based oral health intervention delivered by the Telegram platform. The program targeted multiple BCTs that mapped on to the motivational and volitional phases proposed in the HAPA. This study demonstrated that the oral health intervention resulted in significant improvements in toothbrushing behaviour and clinical oral health indicators (CPI and VPI) as well as more positive social cognitions (intention, outcome-expectancies, risk-perception, self-efficacy, perceived social support, action planning, coping planning, self-monitoring), and OHRQoL among Iranian adolescent students in the short- and long-term. The study also highlighted that involving mothers in the process resulted in better outcomes in terms of oral hygiene practices and oral health. The literature has consistently revealed that a youth’s social networks, particularly mothers that are primary agents of parenting in almost all Iranian families, influence the decisions that are made and the actions that are taken during the transition to adulthood (Domene, Socholotiuk, & Young, Citation2011).
Given little is known about the psychological determinants of oral health behaviour and oral health outcomes (Da Silva, Alvares de Lima, & Vettore, Citation2018; Scheerman et al., Citation2016), this study also provided novel understandings of the key determinants in this context. Specially, the mediation effect of the HAPA factors on toothbrushing was assessed where it was found that intention, self-efficacy, perceived social support, self-monitoring, and coping planning were significant mediators of the intervention effect on toothbrushing. These finding are in accordance with the results of a recent systematic review with meta-analysis showing that intention, self-efficacy, social influence, and coping planning are important psychosocial factors of toothbrushing (Scheerman, et al., Citation2018).
The current study, to the authors’ knowledge, is the first in utilising Telegram as a medium to deliver a theory-based program to promote good oral hygiene behaviours and oral health in Iranian adolescents. Consistent with current findings, previous research has also shown that the use of mobile applications as a medium for oral health promotion is effective in improving oral health and oral hygiene behaviours (Marchetti, Fraiz, Nascimento, Soares, & Assunção, Citation2018; Scheerman, et al., Citation2019; Zotti et al., Citation2016). For example, Scheerman et al. evaluated the WhiteTeeth app designed to promote oral health behaviour in Dutch adolescents (Scheerman, et al., Citation2019) and Zotti et al. evaluated a Whatsapp-based program to promote oral health in Italian adolescents. Both studies asked the participants to share selfies with the research team and provided feedback and education via the app, with significant results observed for oral hygiene outcomes. A study conducted by Li et al. (Citation2016), however, showed that the use of a social media-based app called ‘WeChat’ failed to change oral health behaviour (Li et al., Citation2016). A potential reason for the differences in findings might be that Li et al. only used text-messaging as a behaviour change technique rather than multiple behaviour change techniques. Previous research has shown that mobile applications which incorporate multiple behaviour change techniques (BCT’s) are more effective in changing behaviour as they target a range of behavioural determinants (Webb et al., Citation2010).
Study strengths, limitations, and conclusions
In addition to the key strengths of developing an oral health intervention based in theory and using social media to deliver the program, the homogenous characteristics observed among study groups reflects a good randomization process. Other strengths include the masking of researchers, recruiting a large sample of adolescents across multiple schools, and short- and long-term assessment follow-ups. Further, the study was able to determine additional effects of including mothers in the intervention. To give more insight in how mothers influence the effectiveness of the intervention, future studies should measure the extent to which mothers are involved in the experiment, such as how often mothers supported and monitored their child’s behaviour. Another limitation that should be noted is that toothbrushing behaviour was based on self-report, which is prone to memory or social desirability bias. However, it should be noted that clinical objective measures of oral health were also taken and significantly and positively correlated with toothbrushing behaviour. Further, the results require validation and extension to other primary carers who have been found to play a significant role in a child’s healthy development (e.g. fathers, grandparents) and to a broader population of mothers including those in rural areas, single mothers, and those with less education; all factors known to be linked with poorer quality diets (Saied-Moallemi, Vehkalahti, Virtanen, Tehranchi, & Murtomaa, Citation2008).
Conclusion
This oral health promotion intervention utilising Telegram resulted in an improvement in toothbrushing behaviour and oral hygiene status of participants in the intervention groups, this was evident both in the short- and long-term. The current findings highlight that, within an Iranian adolescent sample, a theory-based program delivered by an online social-media platform involving mothers, in addition to adolescents, further improves effectiveness of toothbrushing. Mobile phone use is rapidly expanding around the world; thus, the impact of effective oral health interventions delivered via mobile phones could have significant positive implications.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ainamo, J., Barmes, D., Beagrie, G., Cutress, T., Martin, J., & Sardo-Infirri, J. (1982). Development of the World Health Organization (WHO) community periodontal index of treatment needs (CPITN). International Dental Journal, 32(3), 281–291.
- Åstrøm, A. N. (1998). Parental influences on adolescents’ oral health behavior: Two-year follow-up of the Norwegian Longitudinal Health Behavior Study participants. European Journal of Oral Sciences, 106, 922–930. doi:10.1046/j.0909-8836.1998.eos106504.x
- Badawy, S. M., & Kuhns, L. M. (2017). Texting and mobile phone app interventions for improving adherence to preventive behaviour in adolescents: A systematic review. JMIR mHealth and Uhealth, 5(4), e50. doi:10.2196/mhealth.6837
- Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173.
- Buis, L. R. (2011). The potential for web-based social network sites and self-regulation for health promotion. American Journal of Health Promotion, 26(2), 73–76. doi:10.4278/ajhp.110223-CIT-83
- Christensen, P. (2004). The health-promoting family: A conceptual framework for future research. Social Science & Medicine, 59, 377–387. doi:10.1016/j.socscimed.2003.10.021
- Da Silva, A. N., Alvares de Lima, S. T., & Vettore, M. V. (2018). Protective psychosocial factors and dental caries in children and adolescents: A systematic review and meta‐analysis. International Journal of Paediatric Dentistry, 28(5), 443–458. doi:10.1111/ipd.12375
- Davies, R. M., Davies, G. M., Ellwood, R. P., & Kay, E. J. (2003). Prevention. Part 4: Toothbrushing: What advice should be given to patients? British Dental Journal, 195(3), 135. doi:10.1038/sj.bdj.4810396
- Dombrowski, S. U., Sniehotta, F. F., Avenell, A., & Coyne, J. C. (2007). Current issues and future directions in psychology and health: Towards a cumulative science of behaviour change: Do current conduct and reporting of behavioural interventions fall short of best practice? Psychology & Health, 22, 869–874.
- Domene, J. F., Socholotiuk, K. D., & Young, R. A. (2011). The early stages of the transition to adulthood: Similarities and differences between mother-daughter and mother-son dyads. Qualitative Research in Psychology, 8(3), 273–291.
- Ebrahimpour, A., Rajabali, F., Yazdanfar, F., Azarbad, I. R., Node, M. R., Siamian, H., & Vahedi, M. (2016). Social network sites as educational factors. Acta Informatica Medica, 24(2), 134. 134-138doi:10.5455/aim.2016.24
- Gholami, M., Knoll, N., & Schwarzer, R. (2015). A brief self-regulatory intervention increases dental flossing in adolescent girls. International Journal of Behavioral Medicine, 22(5), 645–651.
- Godino, J. G., Merchant, G., Norman, G. J., Donohue, M. C., Marshall, S. J., Fowler, J. H., … Gupta, A. (2016). Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): A 2 year, parallel-group, randomised, controlled trial. The Lancet Diabetes & Endocrinology, 4, 747–755. doi:10.1016/S2213-8587(16)30105-X
- Herold, K. (2018). How people use social media in 2018. The manifest (2018, December 3). Retrieved from: https://themanifest.com/social-media/how-people-use-social-media-2018
- Hamilton, K., Bonham, M., Bishara, J., Kroon, J., & Schwarzer, R. (2017). Translating dental flossing intentions into behavior: A longitudinal investigation of the mediating effect of planning and self-efficacy on young adults. International Journal of Behavioral Medicine, 24(3), 420–427. doi:10.1007/s12529-016-9605-4
- Hamilton, K., Cornish, S., Kirkpatrick, A., Kroon, J., & Schwarzer, R. (2018). Parental supervision for their children’s toothbrushing: Mediating effects of planning, self-efficacy, and action control. British Journal of Health Psychology, 23(2), 387–406. doi:10.1111/bjhp.12294
- Hamilton, K., Orbell, S., Bonham, M., Kroon, J., & Schwarzer, R. (2018). Dental flossing and habit: A longitudinal moderated mediation analysis. Psychology, Health, & Medicine, 23, 619–627. doi:10.1080/13548506.2017.1381339
- Kazemnejad, A., Zayeri, F., Rokn, A. R., & Kharazifard, M. J. (2008). Prevalence and risk indicators of periodontal disease among high-school students in Tehran. Eastern Mediterranean Health Journal, 14(1), 119–125.
- Krull, J. L., & MacKinnon, D. P. (2001). Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research, 36(2), 249–277. doi:10.1207/S15327906MBR3602_06
- Lhakhang, P., Hamilton, K., Sud, N., Sud, S., Kroon, J., Knoll, N., & Schwarzer, R. (2016). Combining self-management cues with incentives to promote interdental cleaning among Indian periodontal disease outpatients. BMC Oral Health, 16(1), 6. doi:10.1186/s12903-016-0164-5
- Li, X., Xu, Z. R., Tang, N., Ye, C., Zhu, X. L., Zhou, T., & Zhao, Z. H. (2016). Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clinical Oral Investigations, 20(8), 1849–1859. doi:10.1007/s00784-015-1662-6
- Lin, C. Y., Kumar, S., & Pakpour, A. H. (2016). Rasch analysis of the Persian version of PedsQLTM Oral Health Scale: Further psychometric evaluation on item validity including differential item functioning. Health Promotion Perspectives, 6(3), 145. doi:10.15171/hpp.2016.23
- Lin, C. Y., Scheerman, J. F. M., Yaseri, M., Pakpour, A. H., & Webb, T. L. (2017). A cluster randomised controlled trial of an intervention based on the Health Action Process Approach for increasing fruit and vegetable consumption in Iranian adolescents. Psychology & Health, 32(12), 1449–1468.
- Madden, M., Lenhart, A., Duggan, M., Cortesi, S., & Gasser, U. (2014). Teens and Technology 2013. Washington, DC: Pew Research Center.
- Marchetti, G., Fraiz, F. C., Nascimento, W. M. D., Soares, G. M. S., & Assunção, L. R. D. S. (2018). Improving adolescents’ periodontal health: Evaluation of a mobile oral health App associated with conventional educational methods: A cluster randomized trial. International Journal of Paediatric Dentistry, 28(4), 410–419. doi:10.1111/ipd.12371
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., … Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. doi:10.1007/s12160-013-9486-6
- Pakpour, A. H., Hidarnia, A., Hajizadeh, E., Kumar, S., & Harrison, A. P. (2011). The status of dental caries and related factors in a sample of Iranian adolescents. Medicina Oral Patología Oral y Cirugia Bucal, 16, e822–7. doi:10.4317/medoral.17074
- Pakpour, A. H., Yekaninejad, M. S., Zarei, F., Hashemi, F., Steele, M. M., & Varni, J. W. (2011). The Pedsql™ Oral Health Scale in Iranian children: Reliability and validity. International Journal of Paediatric Dentistry, 21(5), 342–352. doi:10.4317/medoral.17074
- Pakpour, A. H., & Sniehotta, F. F. (2012). Perceived behavioural control and coping planning predict dental brushing behaviour among Iranian adolescents. Journal of Clinical Periodontology, 39(2), 132–137. doi:10.1111/j.1600-051X.2011.01826.x
- Pakpour, A. H., Hidarnia, A., Hajizadeh, E., & Plotnikoff, R. C. (2012). Action and coping planning with regard to dental brushing among Iranian adolescents. Psychology, Health & Medicine, 17, 176–187. doi:10.1080/13548506.2011.596551
- Pakpour, A. H., Yekaninejad, M. S., Sniehotta, F. F., Updegraff, J. A., & Dombrowski, S. U. (2014). The effectiveness of gain-versus loss-framed health messages in improving oral health in Iranian secondary schools: A cluster-randomized controlled trial. Annals of Behavioral Medicine, 47(3), 376–387. doi:10.1007/s12160-013-9543-1
- Pakpour, A. H., Gholami, M., Gellert, P., Yekaninejad, M. S., Dombrowski, S. U., & Webb, T. L. (2016). The effects of two planning interventions on the oral health behavior of Iranian adolescents: A cluster randomized controlled trial. Annals of Behavioral Medicine, 50(3), 409–418. doi:10.1007/s12160-015-9767-3
- Patel, R., Chang, T., Greysen, S. R., & Chopra, V. (2015). Social media use in chronic disease: A systematic review and novel taxonomy. The American Journal of Medicine, 128(12), 1335–1350. doi:10.1016/j.amjmed.2015.06.015
- Petersen, P. E. (2003). The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology, 31(s1), 3–24. doi:10.1046/j.2003.com122.x
- Saied-Moallemi, Z., Vehkalahti, M. M., Virtanen, J. I., Tehranchi, A., & Murtomaa, H. (2008). Mothers as facilitators of preadolescents' oral self-care and oral health. Oral Health & Preventive Dentistry, 6(4), 271–277.
- Scheerman, J. F. M., van Loveren, C., van Meijel, B., Dusseldorp, E., Wartewig, E., Verrips, G. H. W., … van Empelen, P. (2016). Psychosocial correlates of oral hygiene behaviour in people aged 9 to 19–A systematic review with meta‐analysis. Community Dentistry and Oral Epidemiology, 44(4), 331–341. doi:10.1111/cdoe.12224
- Scheerman, J. F. M., van Empelen, P., van Loveren, C., Pakpour, A. H., van Meijel, B., Gholami, M., … Verrips, G. H. W. (2017). An application of the health action process approach model to oral hygiene behaviour and dental plaque in adolescents with fixed orthodontic appliances. International Journal of Paediatric Dentistry, 27(6), 486–495. doi:10.1111/ipd.12287
- Scheerman, J. F. M., van Empelen, P., van Loveren, C., & van Meijel, B. (2018). A Mobile App (WhiteTeeth) to promote good oral health behavior among Dutch adolescents with fixed orthodontic appliances: Intervention mapping approach. JMIR mHealth and Uhealth, 6(8), e163. doi:10.2196/mhealth.9626
- Scheerman, J. F. M., van Meijel, B., van Empelen, P., Verrips, G. H. W., van Loveren, C., Twisk, J. W. R., … Kramer, G. J. C. (2019). The effect of using a mobile application (‘WhiteTeeth’) on improving oral hygiene: A randomized controlled trail. International Journal of Dental Hygiene. 1–11. doi:10.1111/idh.12415
- Schüz, B., Sniehotta, F. F., Wiedermann, A., & Seemann, R. (2006). Adherence to a daily flossing regimen in university students: effects of planning when, where, how and what to do in the face of barriers. Journal of Clinical Periodontoly, 33(9), 612–619.
- Schwarzer, R. (2008). Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology, 57, 1–29. doi:10.1111/j.1464-0597.2007.00325.x
- Schwarzer, R., Antoniuk, A., & Gholami, M. (2015). A brief intervention changing oral self-care, and self-monitoring. British Journal of Health Psychology, 20(1), 56–67.
- Turesky, S., Gilmore, N. D., & Glickman, I. (1970). Reduced plaque formation by the chloromethyl analogue of victamine C. Journal of Periodontology, 41(41), 41–43. doi:10.1902/jop.1970.41.41.41
- Webb, T. L., Joseph, J., Yardley, L., & Michie, S. (2010). Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research, 12(1), e4. doi:10.2196/jmir.1376
- Yazdani, R., Vehkalahti, M. M., Nouri, M., & Murtomaa, H. (2008). Oral health and treatment needs among 15-year-olds in Tehran, Iran. Community Dental Health, 25(4), 221.
- Zotti, F., Dalessandri, D., Salgarello, S., Piancino, M., Bonetti, S., Visconti, L., & Paganelli, C. (2016). Usefulness of an app in improving oral hygiene compliance in adolescent orthodontic patients. The Angle Orthodontist, 86(1), 101–107. doi:10.2319/010915-19.1
- Zhou, G., Sun, C., Knoll, N., Hamilton, K., & Schwarzer, R. (2015). Self-efficacy, planning, and action control in an oral self-care intervention. Health Education Research, 30(4), 671–681. doi:10.1093/her/cyv032