Abstract
Objective
Compassion-based interventions show promise in enhancing well-being and reducing distress, but little is known about their applications for people with long-term physical conditions. This study explores compassion-based interventions for this population: what are their differing elements (content, structure, tailoring, use of technology), feasibility and acceptability, effects and experienced benefits?
Design
A mixed-methods systematic review was conducted. Four bibliographic databases were searched without study design restrictions. Meta-synthesis was used to integrate quantitative results of effects and qualitative results of experienced benefits.
Results
Twenty studies met the inclusion criteria. Most studies targeted people with cancer or persistent pain. Interventions were either comprehensive with 6–12 face-to-face sessions, or brief based on a single compassion exercise. Feasibility and accessibility were highly rated by participants. Amongst a plethora of outcomes, reductions in depression and anxiety were the most common findings. Our qualitative synthesis yielded experienced benefits of (1) acceptance of the condition; (2) improved emotion regulation skills; (3) reduced feelings of isolation. There was minimal overlap between quantitative and qualitative outcomes.
Conclusion
While the field is still in its infancy, this review highlights the potential benefits of compassion-based interventions for people with long-term physical conditions and discusses recommendations for further intervention research and development.
Being diagnosed with a long-term physical condition, such as cancer or a chronic illness like asthma or diabetes, can bring many adaptive challenges; both abrupt, such as finding oneself in the midst of myriad medical procedures, and gradual, such as the ongoing loss of energy and adjusting to emerging limitations (Dekker & de Groot, Citation2018). This new reality is a process that requires people to accept, cope with and self-manage their condition as well as integrate it into their lives and form a new identity (Ambrosio et al., Citation2015). While some people with long-term physical conditions experience positive changes, such as increased closeness with others or posttraumatic growth (Petrie, Buick, Weinman, & Booth, Citation1999; Rzeszutek & Gruszczyńska, Citation2018), generally many are at an increased risk for lower emotional well-being (Heinze, Kruger, Reischl, Cupal, & Zimmerman, Citation2015), depression and anxiety (Clarke & Currie, Citation2009; Patten, Citation2001), and this may further hinder adjustment to the condition and increase symptom burden (Katon & Ciechanowski, Citation2002). In the meantime, daily life goes on and basic housing, financial and employment issues and social problems interact with the demands of the illness and may interfere with the capacity for active coping behaviour (Van Houtum, Rijken, & Groenewegen, Citation2015). In response to the challenges of living with a long-term physical condition, many people report blaming themselves for their perceived role in causing or exacerbating their condition and this self-blame may further increase distress (Callebaut, Molyneux, & Alexander, Citation2017).
One attribute to help people to accept and cope with the challenges of a long-term physical condition may be compassion, defined as ‘a sensitivity to suffering in self and others with a commitment to try to alleviate and prevent it’ (Gilbert, Citation2014, p. 19). Compassion encompasses the acknowledgement that all humans go through difficult experiences and entails tending to those difficult experiences with kindness and wise, caring action (Gilbert, Citation2014; Neff, Citation2011; Strauss et al., Citation2016). Compassion for ourselves, or self-compassion, is associated with lower distress (Costa & Pinto-Gouveia, Citation2013; Friis, Johnson, Cutfield, & Consedine, Citation2015; Pinto‐Gouveia, Duarte, Matos, & Fráguas, 2014) and higher health-related quality of life (Brion, Leary, & Drabkin, Citation2014; Dewsaran-van der Ven et al., Citation2018; Nery-Hurwit, Yun, & Ebbeck, Citation2018; Pinto‐Gouveia et al., 2014), adaptive coping (Sirois, Molnar, & Hirsch, Citation2015), emotion-regulation (Trompetter, de Kleine, & Bohlmeijer, Citation2017), reduced feelings of shame (Sedighimornani, Rimes, & Verplanken, Citation2019) health-promoting behaviours (Dunne, Sheffield, & Chilcot, Citation2018; Homan & Sirois, Citation2017), seeking social support (Brion et al., Citation2014) and treatment adherence (Sirois & Hirsch, Citation2019) in various long-term physical condition and healthy populations. Research on giving and receiving compassion to and from others is relatively scarce in the context of long-term physical conditions, while there is some research on fears that may come up when attempting to cultivate compassion (e.g. fears that are fuelled by a lack of safe early memories around receiving compassion). It is important to acknowledge and validate these fears, as they are integral to the training of compassion (as addressed in compassion-based interventions such as Compassion Focused Therapy (CFT; ‘fears, blocks & resistances’) and Mindful Self-Compassion (MSC; ‘backdraft’)). A recent meta-analysis regarding clinical and non-clinical populations based on data from 4,723 participants found that fears of receiving compassion have significant and moderate effect sizes with shame, self-criticism and depression (Kirby, Day, & Sagar, Citation2019), and two studies concerning long-term physical conditions found relations between fear of receiving compassion and depression (Trindade, Ferreira et al., Citation2018) and lower psychological health (Trindade, Duarte, Ferreira, Coutinho, & Pinto-Gouveia, Citation2018). In summary, (self-)compassion is associated with lower distress and reduced feelings of (bodily) shame, and may foster adaptive responses to the illness such as seeking social support and living healthily. Therefore, compassion is a relevant resource in facing the specific challenges of living with a long-term physical condition.
Particularly, it appears that compassion can be trained, as a recent meta-analysis indicates that compassion-based interventions show promise in enhancing well-being as well as reducing distress (Kirby, Tellegen, & Steindl, Citation2017). While these compassion-based interventions mostly consist of core elements of psycho-education regarding emotions, meditative and reflective compassion exercises, and homework to practice compassionate responding in daily life, they vary in their theoretical underpinnings, definition of compassion, delivery format and intervention length (Kirby, Citation2017). For example, there are comprehensive multi-component interventions that last multiple weeks as well as brief sessions that consist of a single compassion exercise; some interventions are delivered true to the original intervention protocol while others are tailored to the target population; and while the use of (mobile) technology is on the rise in psychosocial interventions (Luxton, McCann, Bush, Mishkind, & Reger, Citation2011; Marzano et al., Citation2015) it is unclear how this is implemented in compassion-based interventions. Moreover, only two of the studies in the aforementioned meta-analysis focused on long-term physical conditions, while most focused on non-clinical (e.g. athletes) and mental health (e.g. depression) populations. Since there has recently been an increase in compassion-based interventions for long-term physical conditions, a review is warranted. To enable an exploration of the appropriateness of interventions beyond questions of efficacy only (e.g. examining intervention characteristics such as structure, use of technology, tailoring, and feasibility and acceptability), a mixed methods approach is called for (Harden, Citation2010). The first aim of this mixed-methods systematic review is therefore to provide an overview of which compassion-based interventions are available for people with long-term physical conditions. Consequently, their content, structure, use of technology, tailoring and helpful elements will be assessed. Second, their feasibility and acceptability will be examined and third, their effects and experienced benefits will be investigated. We expect that this work will generate insights into the potential utility of compassion-based interventions for people with long-term physical conditions as well as inform further intervention development.
Methods
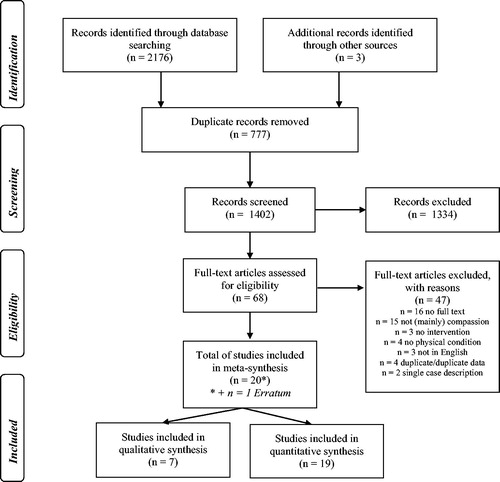
A mixed-methods systematic review was conducted. For conducting and reporting this review the PRISMA guidelines were adhered to.
Search and selection methods
Four bibliographic databases (PsychINFO, PubMed, Scopus and Web of Science) were searched, with the first search taking place on the 15th of November 2018 and the last update on the 4th of September 2019. No publication date or study design restrictions were employed. The following terms were searched for in any field: ‘compassion’, AND ‘intervention’, ‘training’, ‘program’, ‘therapy’, AND ‘chronic illness’, ‘physical illness’, ‘somatic illness’, ‘somatic’, ‘HIV’, ‘cancer’, ‘diabetes’, ‘heart’, ‘stroke’, ‘MS’, ‘epilepsy’, ‘chronic pain’, ‘dementia’, ‘arthritis’, ‘asthma’, ‘COPD’, ‘ALS’, ‘bowel’, ‘obesity’, ‘Parkinson’ and ‘fibromyalgia’. To cover the broad scope of long-term physical conditions, we included general (e.g. ‘physical illness’) and specific (e.g. ‘asthma’) free-text terms as well as controlled vocabulary (DE ‘Physical Disorders’ in PsychINFO and ‘Disease”[Mesh]’ in PubMed). While the terms loving-kindness (metta) and compassion are often conflated in the literature and loving-kindness practices may be part of compassion training, they are distinct concepts. Loving-kindness focuses on increasing well-being or positive affect, while compassion focuses on the alleviation and prevention of suffering (see Gilbert, Basran, MacArthur, & Kirby, Citation2019): hence loving-kindness and metta were not included as search terms. Finally, reference lists of relevant articles were screened and key authors were contacted for further studies to review.
After removal of duplicates, two independent researchers screened all titles and abstracts and subsequently reviewed full-text articles to make decisions regarding eligibility. Studies were included if they met the following criteria: an intervention was provided (1); the main objective of the intervention was the training of (self-)compassion (2); and the population was affected by a long-term physical condition (3). Studies were excluded if they did not meet these criteria or if they were not in English or consisted of a single case description. Disagreements and uncertainties regarding eligibility were resolved in discussion until consensus was reached. See for an overview of the flow of papers at each stage.
Data extraction, quality assessment and synthesis
Data on intervention characteristics, feasibility and acceptability, study characteristics and all study-reported outcome measures (including adverse outcomes) were extracted independently by two researchers. For feasibility and acceptability, any researcher-indicated benchmark for feasibility and acceptability was extracted (qualitative and quantitative). Qualitative data on intervention experiences (citations and researcher-described) were extracted in full for text analysis. In addition, qualitative data on intervention evaluation, helpful elements and barriers were extracted. Methodological quality was assessed by two independent reviewers using the Mixed Methods Appraisal Tool (MMAT) (Hong et al., Citation2018). The MMAT is designed to appraise the quality of studies in a review process based on criteria appropriate to the type of design. Example criteria are appropriate interpretation of results for qualitative studies, complete outcome data for quantitative non-randomized studies and adherence for randomized controlled trials. Mixed method studies are evaluated based on the individual study components and on the integration of different methods. Each criterion is rated as sufficient or insufficient, resulting in scores of out of 5 for single method studies and out of 15 for mixed method studies. Summary scores are discouraged to prevent oversimplification (Crowe & Sheppard, Citation2011; Hong et al., Citation2018).
Thematic synthesis
Thematic synthesis was conducted to analyse which changes and benefits participants of compassion-based intervention experienced. Two independent researchers analysed the results in accordance to the approach described by Thomas and Harden (Citation2008). Findings of primary studies were analysed with line-by-line coding. Next, the resulting codes were categorized into descriptive themes that remained close to the content of primary studies, and finally these themes were categorized into overarching analytical themes. Throughout the process disagreements were resolved by discussion until consensus was reached and codes and themes were checked against the primary results for accuracy and completeness.
Results
A total of n = 20 articles met the inclusion criteria, two of which described the same study sample2,11. Studies were published between 2012 and 2019 and most (n = 13) were published in the last three years. Fourteen articles presented exploratory or pilot studies1–6,9,10, 13,14,17–20 and six presented main studies7,8,11,12,15,16. Study designs varied widely and included ten randomized controlled trials6–9,12,15–18,20, four pre-posttests2,4,10,19, five mixed methods1,3,5,13,14 and one qualitative study11.
Interventions characteristics
Population
Among the studies, the target populations were people with cancer (n = 7)2,6,8,9,11,17,18 (breast cancer and young adult), persistent pain (n = 4)3,13,14,20, dementia (n = 2)4,5, brain injury (n = 2)1,15, diabetes type I and II (n = 1)7, heart failure (n = 1)10, visible skin conditions (n = 1)19, fibromyalgia (n = 1)12 and day hospice patients (n = 1)16. Most study participants had been living with their illness for a while (>6 months to decades; chronic or survivor) (n = 11)2,3,6–8,11,16–20, while for a few studies the time since diagnoses is unclear (n = 7)1,5,10,12,13,14,15 or very recent (n = 2)4,9. Apart from interventions that only targeted women (with breast cancer), approximately 70% of intervention participants across studies were female. See for an overview of intervention characteristics.
Table 1. Intervention characteristics and qualitative evaluation.
Comprehensive vs. brief interventions: content and structure
The interventions can be divided into comprehensive interventions (n = 14) and brief interventions (n = 6). Comprehensive interventions consist of many different exercises that are trained over an extended period of time, while brief interventions consist of a single exercise that may be repeated a couple of times. The majority of comprehensive interventions were based on Compassion Focused Therapy (CFT; n = 6)1,4,5,9,13,14, followed by Mindful Self-Compassion (MSC; n = 4)2,7,10,11, Cognitively-Based Compassion Training (CBCT; n = 2)6,8, Compassion Cultivation Training (CCT, n = 1)3 and Attachment-Based Compassion Therapy (ABCT, n = 1)12. See Kirby (Citation2017) for an overview of the theoretical background and evidence base for these interventions. Comprehensive interventions were provided in a group setting (n = 10)2–4,6–8,11–14, individual setting (n = 3)5,9,10 or a combination of both (n = 1)1 and typically consisted of weekly sessions over a period of 6–12 weeks. Most (n = 11)1–3,5–8,10–13, included homework practices such as audio-supported guided meditations. All comprehensive interventions were guided by one or more psychologists or instructors trained in the intervention. Intervention protocols ranged from a topic list to fully manualized sessions, thus varying in their degree of consistency and flexibility. Brief interventions consisted of an expressive writing exercise (n = 5)16–20 or a compassion-focused imagery exercise (n = 1)15. With the exception of compassion-focused imagery, all brief interventions were unguided. Brief interventions lasted 20–50 minutes in either a single session (n = 4)15,17–19 or repeated over the course of a few weeks (n = 2)16,20.
Tailoring to the target population
Seven out of 14 comprehensive interventions were not tailored to the target population and adhered to the original intervention protocols2,3,6,7,8,9,11. Two articles described that they did not tailor the intervention in favour of preventing contamination with condition-specific content3,7, and one article mentioned the absence of an available protocol for the target population as a rationale9. Seven comprehensive interventions were tailored to the target population to some extent1,4,5,10,12,13,14. Most of the tailored interventions were based on CFT (n = 5)1,4,5,13,14, wherein the neurobiological and evolutionary theories behind CFT are expanded upon to provide psycho-education specific to the physical condition. For example, a main theory in CFT is that we all have ‘tricky brains’ that inevitably come with difficult emotions and contradicting experiences. In CFT with dementia or brain injury it is explained that participants have ‘even trickier brains’ as a way to frame difficult experiences related to the physical condition. Most tailored interventions also include practical adaptations to make the intervention more manageable, such as increased repetition, the presence of a supportive other and visual learning materials to aid memory (dementia and brain injury) and omitting certain exercises to reduce intervention burden (heart failure). The majority of brief interventions were also tailored (n = 5)15,17–20. For example, in the expressive writing interventions participants were instructed to write about a difficult experience specific to their condition (e.g. body image distress in women with breast cancer) from a perspective of self-compassion. No studies described the role of tailoring in participant involvement.
Use of technology
The use of technology (i.e. the use of information, mobile or sensor technology for delivery of (elements of) the intervention or for communication) in the comprehensive interventions is scarce, with only one intervention taking place completely online via video-conference2,11, one intervention using compassionate messages and alerts via smartphone1, and two interventions making use of a study website for class discussions or providing audio exercises3,6. Some interventions were minimally supported by technology e.g. in the form of using e-mail reminders or providing take-home exercises on USB drive. Three of the brief interventions were entirely provided via a website18–20 while one was supported by preparatory video-instruction15.
Helpful elements and barriers
Six studies of comprehensive interventions provided qualitative data on helpful elements and barriers within the intervention in the context of experienced effectiveness1,4,5,11,13,14. The most frequently mentioned helpful element was support by the group or therapist/trainer (n = 5 studies)1,4,5,11,14 followed by specific practices such as mindfulness5,11,13,14 and compassionate imagery11,14. Condition-specific psycho-education13,14 and a therapist/trainer who is knowledgeable about the physical condition5 were also appreciated. Experienced barriers were difficulty in engaging with the material due to memory problems (dementia)5, difficulty with integrating the exercises into daily life11, and the challenge of finding a self-compassionate voice5,11. One study described a body scan practice as a barrier for some participants because it triggered health-related anxiety, and a helpful element for others because it elicited gratitude for working body parts11.
Feasibility and acceptability
A wide variety of feasibility and acceptability benchmarks was used. Of the eight studies that explicitly reported on feasibility, seven concluded that the intervention in question was feasible2,6,8,10,11,13,16. The most common indicator was attendance to sessions, which ranged from 75–100%. One study reported that their intervention manual was not feasible, because the material could not be covered in the allotted time and two extra sessions would be needed5.
Four studies reported that participants rated the intervention as acceptable2,5,6,10, and no study reported that the intervention was not acceptable. Some studies described acceptability in terms of whether participants choose the intervention out of various intervention options or whether they would continue to practice what they learned, while others used quantitative measures. Satisfaction was the most common indicator of acceptability, which ranged from 92 to 95%.
Effects and experienced benefits
Quality appraisal
Out of the 21 articles that were critically appraised with the MMAT, 11 studies rated 4–5 out of 5 points2,4,6–8,11,12,15,17–19 and five studies rated 2–3 points9,10,14,16,20. Mixed methods studies rated 10–13 out of 15 points1,3,5,12,13 (see for a full overview of ratings per study). Thus, overall criteria of appropriate methods and measures and reduction of bias were sufficiently met. Nevertheless, it is important to emphasize that most studies had (very) small sample sizes (and may thus be underpowered), therefore the following results for study outcomes should be interpreted with caution.
Table 2. Study and intervention characteristics and outcomes.
Outcome measures
For ease of interpretation, outcomes of the 21 included studies have been categorized into psychological, physical and functional outcome measures and process measures (e.g. compassion, mindfulness). For a full overview, including other study-specific outcome measures (e.g. fear of cancer recurrence), see . Overall, outcome measures varied widely. Most studies assessed depression and anxiety and results for reductions in these outcomes are the most consistent, while results for physical outcomes are the most inconsistent. In contrast to comprehensive interventions, no significant changes in depression or anxiety were found for brief interventions. Both brief and comprehensive interventions yielded improvements in self-compassion, and results for improved (health-related) quality of life in comprehensive interventions seem promising.
Psychological outcomes
Depression (n = 11 studies) and anxiety (n = 10 studies) were the most frequent outcome measures overall. All comprehensive studies that employed significance testing (both controlled and uncontrolled studies) found a significant intervention effect for reduced anxiety1,2,3,12,13 and depression1,2,4,6–8,9,10,12,13. In contrast, the two brief expressive writing interventions did not yield a significant change in anxiety15,18 or depression18,20. Studies of brief expressive writing interventions found significant changes in positive but not negative affect20 and negative but not positive affect19. Only two studies of comprehensive interventions assessed general and mental well-being, and found no significant improvements.6,8
Physical outcomes
Nine studies administered subjective or objective physical outcome measures3,4,6,7,9,10,14,15,20. Pain was the most common physical outcome measure (n = 6), typically measured in different components such as pain severity and pain intensity. Two studies of comprehensive interventions reported significant changes3,14 in components of pain and two reported no significant changes3,6. Of the brief interventions, one study found a significant change in pain20. Other physical outcome measures vary widely per target population and include respiratory rate, HbA1c, and heart rate, with mixed findings.
Functional outcomes
(Health-related) quality of life was assessed in five studies of comprehensive interventions, of which four found improvements3,4,10,12 and one did not8. Other outcome measures were functional status, activity engagement and general health, with mixed results.
Process measures
Comprehensive interventions yielded significant changes in self-compassion2,7,8, mindfulness1,2,6,8 and self-criticism1, with no nonsignificant findings. Brief interventions also yielded significant results for self-compassion17–19, with one non-significant finding15.
Adverse outcomes
Out of the four studies on comprehensive interventions that examined and reported on adverse outcomes, three studies reported no adverse outcomes1,5,9 and one study12 reported a drop-out (n = 1) due to adverse outcomes (not further specified).
Thematic synthesis of qualitative studies
Studies that included qualitative analysis1,3,5,11,13,14 or a description of participant feedback4 were included in the thematic synthesis (n = 7; all are comprehensive interventions). With regard to changes and benefits that participants experienced post-intervention, three themes were identified: (1) acceptance of the condition, the changed body and the resulting limitations; (2) emotion regulation skills (e.g. in threatening medical situations); and (3) reduced feelings of isolation and increased connectedness. See for an overview of descriptive themes with the study sources.
Table 3. Changes or beneficial experiences post-intervention as reported in qualitative studies.
Theme 1: acceptance of the condition, the changed body and the resulting limitations
Compassion-based interventions helped participants to accept their condition and condition-related limitations, as opposed to feeling guilty or blaming themselves. Participants began to have empathy for their feelings that resulted from a difficult situation and learned to respond to physical limitations with self-kindness and self-care. This included accepting the changes of the post-condition body and feeling gratitude towards working body parts. As accepting the condition allowed for a sense of self that is less tied to the condition, rediscovery of other parts of the self became possible.
Theme 2: emotion regulation skills (e.g. in threatening medical situations)
Participants described that they were able to soothe themselves during difficult situations, e.g. during a medical check-up. They reported a decrease in experienced threat-based emotions (e.g. feeling less anger) and an increased sense of calmness, as well as having learned helpful new strategies to handle threat-based emotions (e.g. to regulate anxiety). In addition, participants discovered that they could be a source of support and comfort to themselves, instead of only comforting others or relying solely on others for emotional support.
Theme 3: reduced feelings of isolation and increased connectedness
Participants reported how the intervention and being part of a group helped them to feel understood and less isolated, both through compassion exercises and through a sense of common humanity based on shared struggles. Participants described an increased understanding of others as well as an increased awareness of the already available positive relationships and support in their environment (i.e. through compassionate imagery practice).
Meta-synthesis of quantitative and qualitative findings
When contrasting the results of the thematic synthesis with quantitative outcome measures, we find some overlap and some disparities. First, while acceptance appears to be a major theme for participants, only a very small number of studies measured acceptance, and in a more limited scope (e.g. only acceptance of pain) than the reported range of acceptance-related experiences. Specifically, two quantitative studies assessed and found improvements in body image and appreciation2,18 and three studies found increases in (pain) acceptance3,12,14. Related to the second theme of emotion-regulation, reductions in depression and anxiety were the main focus and the main finding of quantitative studies1–4,6–8,10,12,13,15,18,20, which is different than the experience of participants related to skills and tools to deal with these emotions. No measures of emotion-regulation skills or coping (e.g. Difficulties in Emotion Regulation Scale, Perasso & Velotti, Citation2017) were employed in quantitative studies, except for self-compassion. Increased self-compassion was reported (as a way of dealing with difficult situations or emotions) in both qualitative and quantitative findings. Finally, in support of the third theme of reduced feelings of isolation, a single quantitative study assessed social isolation and found a significant reduction post-intervention2. Overall, it seems that quantitative and qualitative findings are in line with each other to the extent that there are no contradicting findings and both confirm findings of increased acceptance, reduced threat-based emotions (e.g. anxiety) and reduced isolation. However, there seems to be a considerable gap between the themes highlighted in the thematic synthesis and the highly limited extent to which these are represented in the quantitative outcomes measures, as most quantitative studies focus on reductions in depression and anxiety.
Discussion
To our knowledge, this review is the first to investigate the applications, barriers and benefits of compassion-based interventions for people with long-term physical conditions. Our aims were to investigate which compassion-based interventions exist for people with long-term physical conditions and to explore their differing elements (e.g. content and structure, tailoring, use of technology), feasibility and acceptability, and effects and experienced benefits. Our findings show that this is a rapidly emerging field, since the vast majority of studies were published in the last three years and were pilot or exploratory studies. Most of the interventions were targeted at cancer or persistent pain populations. Interventions varied in their structure, with some consisting of weekly group sessions for a period of 6–12 weeks supplemented by homework exercises, others of a single compassion exercise with a few repetitions. Overall, the compassion-based interventions showed encouraging results for reducing anxiety and depression and were considered feasible and acceptable by the participants.
Our results show promising indications of effectiveness of comprehensive compassion-based interventions regarding improvements in depression, anxiety, self-compassion and health-related quality of life, among others. A note of caution is necessary though, as most studies were small scale pilot studies. While brief interventions showed improvements on various outcomes, mostly notably on process measures such as self-compassion, they did not yield improvements in depression and anxiety. Thus, while it is quite promising that brief interventions as short as twenty minutes can already be beneficial, their effects may not be as widespread as comprehensive interventions (or perhaps as long lasting). Across studies the outcome measures used varied widely (with a plethora of psychological, physical and functional outcomes) and it is evident that there is no consensus yet on appropriate outcome measures. Depression and anxiety are most commonly measured, which is expected given the wider comparability within psychosocial intervention literature. However, this focus on general outcome measures rather than outcomes specific to long-term physical conditions does not represent intervention benefits as described by participants in the qualitative and mixed method studies. Our meta-synthesis showed that important themes raised by the participants, namely acceptance of the condition, increased emotion-regulation skills and reduced feelings of isolation, were only marginally represented in the quantitative outcome measures. Being diagnosed with a long-term physical condition does indeed entail an increased risk for higher depression and anxiety (Clarke & Currie, Citation2009; Patten, Citation2001), but it can also involve acceptance of and coping with the condition (Ambrosio et al., Citation2015), isolation (Ohman, Soderberg, & Lundman, Citation2003), self-blame (Callebaut, Molyneux, & Alexander, Citation2017) and emotion-regulation (Wierenga, Lehto, & Given, Citation2017) and it may be important to measure these outcomes. Furthermore, compassion-based interventions target both mental health difficulties and mental health resources (Bohlmeijer & Westerhof, in press), yet resources such as mental well-being (e.g. as measured by the Mental Health Continuum Short-Form with the components emotional, psychological and social well-being (Lamers, Westerhof, Bohlmeijer, ten Klooster, & Keyes, Citation2011)) were rarely assessed. However, in facilitating personal recovery (e.g. reconstructing an identity, finding meaning) in addition to clinical recovery, mental well-being is an important resource (Bohlmeijer & Westerhof, in press). Given the emergence of the field, and the fact that most compassion-based interventions were originally developed for psychiatric or generic target populations (e.g. Gilbert, Citation2009; Neff & Germer, Citation2013), now is the time to consider which outcome measures should be addressed in the context of long-term physical conditions. Based on the results of this review, we recommend that in addition to depression and anxiety, at least mental well-being, acceptance, emotion-regulation and social isolation should be measured.
Future studies should not only carefully reconsider their outcome measures, but also consider which process measures to include. We were surprised to find that the majority of our studies did not measure compassion (or self-compassion) as a process measure. In addition, other potential mediating and moderating variables were not obtained in most of the studies, which is understandable given the pilot nature (and presumably limited power) of the studies. In order to better understand the mechanisms of these interventions, as well as for which patients they might be most effective, it is important to pay attention to process measures as well as moderating variables. We recommend that in future compassion-based interventions for people with long-term physical conditions, at least one compassion measure (e.g. The Self-Compassion Scale (Neff, Citation2016), The Fears of Compassion Scale (Gilbert, McEwan, Matos, & Rivis, Citation2011)) should be included as a process measure. In addition, the themes of our thematic synthesis (acceptance of the condition, increased emotion-regulation skills and reduced feelings of isolation) could be explored as potential mediating variables.
Interventions varied in the extent to which they were tailored to the target population, ranging from practical adjustments such as increased repetition (e.g. for people with dementia), to major adaptation of the content to the particular disease (e.g. compassion-based psychoeducation about pain mechanisms). Such adaptations are thought to bridge the gap between the context in which the intervention was developed and the target context (Stirman, Miller, Toder, & Calloway, Citation2013; Wensing et al., Citation2011), although it is unclear whether tailored interventions are indeed more effective than interventions that are not tailored to the target population (Baker et al., Citation2010; Stirman et al., Citation2013). While the small scale of included studies precluded a thorough comparison, at face value our data did not indicate any differences in effectiveness of tailored vs. untailored interventions. Drawing from qualitative evaluations however, we do note that condition-specific elements of the interventions were considered especially helpful by intervention participants (e.g. by allowing them to find recognition) possibly indicating that tailored interventions may better meet patients’ specific needs. It should be noted that untailored intervention protocols were generally already more supported by existing research, while tailored interventions were typically novel pilot compositions. To address the so-called dichotomy between fidelity and adaptation, it has been suggested that more continuous evidence generation throughout the implementation and adaptation process is needed (Chambers & Norton, Citation2016). Further research could map the extent and type of adaptations that are beneficial for people with long-term physical conditions and compare the effectiveness and experience of tailored vs. untailored compassion-based interventions.
Most interventions consisted of weekly face-to-face meetings in group sessions while only a few were supported by the use of technology, such as websites, apps or e-mail reminders. Yet, for people with long-term physical conditions, these regular face-to-face meetings can present a burden in addition to the high load of medical appointments. While intervention participants described the face-to-face contact as helpful, we have no data on the people that were not reached with these interventions. Internet-based interventions can lower the threshold to participate in an intervention by increased accessibility and scalability (Van Gemert-Pijnen, Kip, & Kelders, Citation2018; Kelders & Howard, Citation2018). In addition, since most people nowadays have their devices such as smartphones at arm’s length, internet-based, mobile interventions could aid with the integration of learned skills into daily lives (Jones et al., Citation2015; Williams, Lynch, & Glasgow, Citation2007). Only one of the included studies made use of mobile technology for sending compassionate messages, and other uses for mobile technology such as offering compassion exercises via push notifications or offering personalized feedback and practice recommendations are yet to be investigated. Moreover, since physical outcomes are particularly relevant to this population, and compassion-based interventions have been associated with improved physical outcomes like adaptive heart rate variability (Kirby et al., Citation2019), further examining the use of sensor technology in this context is relevant. More research is needed to examine the added value of supporting compassion-based interventions with the aforementioned technologies, either in a blended or stand-alone format.
This review was strengthened by the mixed-methods approach which enabled a comprehensive review and integration of qualitative and quantitative findings. Limitations were the exclusion of non-English language studies and the fact that we only included published data. Therefore it is possible that we missed studies that were conducted in other parts of the world or in other languages, and publication bias may have coloured our results. Since the final step of our thematic synthesis was based on discussion until consensus was reached, we did not calculate a measure of interrater agreement and were thus unable to test the agreement and consistency of our coding (Burla et al., Citation2008). In addition, synthesizing qualitative results may present limitations regarding de-contextualization, since it can be unclear how findings of different primary studies translate into other contexts (Thomas & Harden, Citation2008). In this review, we attempted to provide sufficient context for the reader to interpret the findings by thoroughly describing intervention and study characteristics in conjunction with the source studies of qualitative themes.
In conclusion, compassion-based interventions represent a potentially beneficial way to support people with long-term physical conditions and are well-received by intervention participants. Nonetheless, it is clear that the field and the available evidence are in their infancy. First indications of intervention effectiveness are improvements in anxiety, depression, self-compassion and health-related quality of life, among other outcomes. The variety of employed outcome measures is large, and does not match qualitative findings of increased acceptance of the condition, increased emotion regulation skills and reduced feelings of isolation. Based on the results of this review, we suggest that in addition to depression and anxiety, at least (self-)compassion, mental well-being, acceptance, emotion-regulation and social isolation should be measured more often. Further research is needed to examine the impact of brief and comprehensive interventions in sufficiently powered controlled studies and to investigate the role of tailoring and the support of mobile and sensor technologies.
Acknowledgements
We would like to thank Kathi Imani for her help with the search and selection phase and Britt Bente for her help with the quality appraisal phase of the review process. We also thank the Dutch Cancer Society for providing funding for this research.
Conflicts of interest
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ambrosio, L., Senosiain García, J. M., Riverol Fernández, M., Anaut Bravo, S., Díaz De Cerio Ayesa, S., Ursúa Sesma, M. E., … Portillo, M. C. (2015). Living with chronic illness in adults: A concept analysis. Journal of Clinical Nursing, 24(17-18), 2357–2367. doi:10.1111/jocn.12827
- Ashworth, F., Clarke, A., Jones, L., Jennings, C., & Longworth, C. (2015). An exploration of compassion focused therapy following acquired brain injury. Psychology and Psychotherapy: Theory, Research and Practice, 88(2), 143–162. doi:10.1111/papt.12037
- Baker, R., Camosso-Stefinovic, J., Gillies, C., Shaw, E. J., Cheater, F., Flottorp, S., & Robertson, N. (2010). Tailored interventions to overcome identified barriers to change: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews, , Cd005470.
- Bohlmeijer, E. T., & Westerhof, G. J. (in press). A new model for sustainable mental health: Integrating well-being into psychological treatment. In J. Kirby & P. Gilbert (Ed.), Making an impact on mental health and illness. London: Routeledge.
- Brion, J. M., Leary, M. R., & Drabkin, A. S. (2014). Self-compassion and reactions to serious illness: The case of HIV. Journal of Health Psychology, 19(2), 218–229. doi:10.1177/1359105312467391
- Burla, L., Knierim, B., Barth, J., Liewald, K., Duetz, M., & Abel, T. (2008). From text to codings: Intercoder reliability assessment in qualitative content analysis. Nursing Research, 57(2), 113–117. doi:10.1097/01.NNR.0000313482.33917.7d
- Callebaut, L., Molyneux, P., & Alexander, T. (2017). The relationship between self-blame for the onset of a chronic physical health condition and emotional distress: A systematic literature review. Clinical Psychology & Psychotherapy, 24(4), 965–986. doi:10.1002/cpp.2061
- Campbell, I. N., Gallagher, M., Mcleod, H. J., O’neill, B., & Mcmillan, T. M. (2019). Brief compassion focused imagery for treatment of severe head injury. Neuropsychological Rehabilitation, 29(6), 917–927. doi:10.1080/09602011.2017.1342663.
- Campbell, I. N., Gallagher, M., McLeod, H. J., O’Neill, B., & McMillan, T. M. (2019). Brief compassion focused imagery for treatment of severe head injury. Neuropsychological Rehabilitation, 29(6), 917–927. doi:10.1080/09602011.2017.1342663
- Campo, R. A., Bluth, K., Santacroce, S. J., Knapik, S., Tan, J., Gold, S., … Asher, G. N. (2017). A mindful self-compassion videoconference intervention for nationally recruited posttreatment young adult cancer survivors: Feasibility, acceptability, and psychosocial outcomes. Supportive Care in Cancer, 25(6), 1759–1768. doi:10.1007/s00520-017-3586-y
- Chambers, D. A., & Norton, W. E. (2016). The adaptome: Advancing the science of intervention adaptation. American Journal of Preventive Medicine, 51(4), S124–S131. doi:10.1016/j.amepre.2016.05.011
- Chapin, H. L., Darnall, B. D., Seppala, E. M., Doty, J. R., Hah, J. M., & Mackey, S. C. (2014). Pilot study of a compassion meditation intervention in chronic pain. Journal of Compassionate Health Care, 1(1), 4. doi:10.1186/s40639-014-0004-x
- Clarke, D. M., & Currie, K. C. (2009). Depression, anxiety and their relationship with chronic diseases: A review of the epidemiology, risk and treatment evidence. Medical Journal of Australia, 190(S7), S54–S60. doi:10.5694/j.1326-5377.2009.tb02471.x
- Collins, R. N., Gilligan, L. J., & Poz, R. (2018). The evaluation of a compassion-focused therapy group for couples experiencing a dementia diagnosis. Clinical Gerontologist, 41(5), 474–486. doi:10.1080/07317115.2017.1397830
- Costa, J., & Pinto-Gouveia, J. (2013). Experiential avoidance and self-compassion in chronic pain. Journal of Applied Social Psychology, 43(8), 1578–1591. doi:10.1111/jasp.12107
- Craig, C., Hiskey, S., Royan, L., Poz, R., & Spector, A. (2018). Compassion focused therapy for people with dementia: A feasibility study. International Journal of Geriatric Psychiatry, 33(12), 1727–1735. doi:10.1002/gps.4977
- Crowe, M., & Sheppard, L. (2011). A review of critical appraisal tools show they lack rigor: Alternative tool structure is proposed. Journal of Clinical Epidemiology, 64(1), 79–89. doi:10.1016/j.jclinepi.2010.02.008
- Dekker, J., & de Groot, V. (2018). Psychological adjustment to chronic disease and rehabilitation–An exploration. Disability and Rehabilitation, 40(1), 116–120. doi:10.1080/09638288.2016.1247469
- Dewsaran-van der Ven, C., Van Broeckhuysen-Kloth, S., Thorsell, S., Scholten, R., De Gucht, V., & Geenen, R. (2018). Self-compassion in somatoform disorder. Psychiatry Research, 262, 34–39. doi:10.1016/j.psychres.2017.12.013
- Dodds, S. E., Pace, T. W., Bell, M. L., Fiero, M., Negi, L. T., Raison, C. L., & Weihs, K. L. (2015a). Erratum to: Feasibility of cognitively-based compassion training (CBCT) for breast cancer survivors: A randomized, wait list controlled pilot study. Supportive Care in Cancer, 23(12), 3609–3611. doi:10.1007/s00520-015-2926-z
- Dodds, S. E., Pace, T. W., Bell, M. L., Fiero, M., Negi, L. T., Raison, C. L., & Weihs, K. L. (2015b). Feasibility of cognitively-based compassion training (CBCT) for breast cancer survivors: A randomized, wait list controlled pilot study. Supportive Care in Cancer, 23(12), 3599–3608. doi:10.1007/s00520-015-2888-1
- Dunne, S., Sheffield, D., & Chilcot, J. (2018). Brief report: Self-compassion, physical health and the mediating role of health-promoting behaviours. Journal of Health Psychology, 23(7), 993–999. doi:10.1177/1359105316643377
- Friis, A. M., Johnson, M. H., Cutfield, R. G., & Consedine, N. S. (2015). Does kindness matter? Self-compassion buffers the negative impact of diabetes-distress on HbA1c. Diabetic Medicine, 32(12), 1634–1640. doi:10.1111/dme.12774
- Friis, A. M., Johnson, M. H., Cutfield, R. G., & Consedine, N. S. (2016). Kindness matters: A randomized controlled trial of a mindful self-compassion intervention improves depression, distress, and HbA1c among patients with diabetes. Diabetes Care, 39(11), 1963–1971. doi:10.2337/dc16-0416
- Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15(3), 199–208. doi:10.1192/apt.bp.107.005264
- Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53(1), 6–41. doi:10.1111/bjc.12043
- Gilbert, P., Basran, J., MacArthur, M., & Kirby, J. N. (2019). Differences in the semantics of prosocial words: An exploration of compassion and kindness. Mindfulness, 10(11), 2259–2271. doi:10.1007/s12671-019-01191-x
- Gilbert, P., McEwan, K., Matos, M., & Rivis, A. (2011). Fears of compassion: Development of three self-report measures. Psychology and Psychotherapy: Theory, Research and Practice, 84(3), 239–255. doi:10.1348/147608310X526511
- Gonzalez-Hernandez, E., Romero, R., Campos, D., Burychka, D., Diego-Pedro, R., Baños, R., … Cebolla, A. (2018). Cognitively-based compassion training (CBCT®) in breast cancer survivors: A randomized clinical trial study. Integrative Cancer Therapies, 17(3), 684–696.
- Haj Sadeghi, Z., Yazdi-Ravandi, S., & Pirnia, B. (2018). Compassion-focused therapy on levels of anxiety and depression among women with breast cancer: A randomized pilot trial. International Journal of Cancer Management, 11, e67019. doi:10.5812/ijcm.67019
- Harden, A. (2010). Mixed-methods systematic reviews: Integrating quantitative and qualitative findings. FOCUS, 2010;25.
- Heinze, J. E., Kruger, D. J., Reischl, T. M., Cupal, S., & Zimmerman, M. A. (2015). Relationships among disease, social support, and perceived health: A lifespan approach. American Journal of Community Psychology, 56(3-4), 268–279. doi:10.1007/s10464-015-9758-3
- Heo, S., McSweeney, J., Ounpraseuth, S., Shaw-Devine, A., Fier, A., & Moser, D. K. (2018). Testing a holistic meditation intervention to address psychosocial distress in patients with heart failure: A pilot study. The Journal of Cardiovascular Nursing, 33(2), 126–134. doi:10.1097/JCN.0000000000000435
- Homan, K. J., & Sirois, F. M. (2017). Self-compassion and physical health: Exploring the roles of perceived stress and health-promoting behaviors. Health Psychology Open, 4(2), 205510291772954. doi:10.1177/2055102917729542
- Hong, Q. N., Pluye, P., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., … Vedel, I. (2018). Mixed Methods Appraisal Tool (MMAT) version 2018
- Imrie, S., & Troop, N. A. (2012). A pilot study on the effects and feasibility of compassion-focused expressive writing in day hospice patients. Palliative and Supportive Care, 10(2), 115–122. doi:10.1017/S1478951512000181
- Jones, D. J., Anton, M., Gonzalez, M., Honeycutt, A., Khavjou, O., Forehand, R., & Parent, J. (2015). Incorporating mobile phone technologies to expand evidence-based care. Cognitive and Behavioral Practice, 22(3), 281–290. doi:10.1016/j.cbpra.2014.06.002
- Katon, W., & Ciechanowski, P. (2002). Impact of major depression on chronic medical illness. Journal of Psychosomatic Research, 53(4), 859–863. doi:10.1016/S0022-3999(02)00313-6
- Kelders, S. M., & Howard, M. (2018). Opportunities of technology to promote health and well-being. In J. E. W. C. van Gemert-Pijnen, S. M. Kelders, H. Kip, & R. Sanderman (Ed.), eHealth research, theory and development: A multidisciplinary approach (1st ed., pp. 48–68). London: Routledge.
- Kirby, J. N. (2017). Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychology and Psychotherapy: Theory, Research and Practice, 90(3), 432–455. doi:10.1111/papt.12104
- Kirby, J. N., Day, J., & Sagar, V. (2019). The ‘Flow’ of compassion: A meta-analysis of the fears of compassion scales and psychological functioning. Clinical Psychology Review, 70, 26–39. doi:10.1016/j.cpr.2019.03.001
- Kirby, J. N., Tellegen, C. L., & Steindl, S. R. (2017). A meta-analysis of compassion-based interventions: Current state of knowledge and future directions. Behavior Therapy, 48(6), 778–792. doi:10.1016/j.beth.2017.06.003
- Lamers, S. M., Westerhof, G. J., Bohlmeijer, E. T., ten Klooster, P. M., & Keyes, C. L. (2011). Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). Journal of Clinical Psychology, 67(1), 99–110. doi:10.1002/jclp.20741
- Lathren, C., Bluth, K., Campo, R., Tan, W., & Futch, W. (2018). Young adult cancer survivors' experiences with a mindful self-compassion (MSC) video-chat intervention: A qualitative analysis. Self and Identity, 17(6), 646–665. doi:10.1080/15298868.2018.1451363
- Luxton, D. D., McCann, R. A., Bush, N. E., Mishkind, M. C., & Reger, G. M. (2011). mHealth for mental health: Integrating smartphone technology in behavioral healthcare. Professional Psychology: Research and Practice, 42(6), 505–512. doi:10.1037/a0024485
- Marzano, L., Bardill, A., Fields, B., Herd, K., Veale, D., Grey, N., & Moran, P. (2015). The application of mHealth to mental health: Opportunities and challenges. The Lancet Psychiatry, 2(10), 942–948. doi:10.1016/S2215-0366(15)00268-0
- Montero-Marín, J., Navarro-Gil, M., Puebla-Guedea, M., Luciano, J. V., Van Gordon, W., Shonin, E., & García-Campayo, J. (2018). Efficacy of “attachment-based compassion therapy” in the treatment of fibromyalgia: A randomized controlled trial. Frontiers in Psychiatry, 8, 307. doi:10.3389/fpsyt.2017.00307
- Neff, K. (2011). Self-compassion: Stop beating yourself up and leave insecurity behind. New York, NY: William Morrow/Harper Collins.
- Neff, K. D. (2016). The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness, 7(1), 264–274. doi:10.1007/s12671-015-0479-3
- Neff, K. D., & Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69(1), 28–44. doi:10.1002/jclp.21923
- Nery-Hurwit, M., Yun, J., & Ebbeck, V. (2018). Examining the roles of self-compassion and resilience on health-related quality of life for individuals with Multiple Sclerosis. Disability and Health Journal, 11(2), 256–261. doi:10.1016/j.dhjo.2017.10.010
- Ohman, M., Soderberg, S., & Lundman, B. (2003). Hovering between suffering and enduring: The meaning of living with serious chronic illness. Qualitative Health Research, 13, 528–542. doi:10.1177/1049732302250720
- Parry, S. L., & Malpus, Z. (2017). Reconnecting the mind and body: A pilot study of developing compassion for persistent pain. Patient Experience Journal, 4(1), 145–153. doi:10.35680/2372-0247.1175.
- Patten, S. B. (2001). Long-term medical conditions and major depression in a Canadian Population study at waves 1 and 2. Journal of Affective Disorders, 63(1-3), 35–41. doi:10.1016/S0165-0327(00)00186-5
- Penlington, C. (2019). Exploring a compassion-focused intervention for persistent pain in a group setting. British Journal of Pain, 13(1), 59–66. doi:10.1177/2049463718772148
- Perasso, G., & Velotti, P. (2017). Difficulties in emotion regulation scale. In V. Zeigler-Hill & T. K. Shackelford (Eds.), Encyclopedia of personality and individual differences (pp. 1–3). Cham: Springer International Publishing.
- Petrie, K. J., Buick, D. L., Weinman, J., & Booth, R. J. (1999). Positive effects of illness reported by myocardial infarction and breast cancer patients. Journal of Psychosomatic Research, 47(6), 537–543. doi:10.1016/S0022-3999(99)00054-9
- Pinto-Gouveia, J., Duarte, C., Matos, M., & Fráguas, S. (2014). The protective role of self‐compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clinical Psychology & Psychotherapy, 21, 311–323. doi:10.1002/cpp.1838
- Przezdziecki, A., & Sherman, K. A. (2016). Modifying affective and cognitive responses regarding body image difficulties in breast cancer survivors using a self-compassion-based writing intervention. Mindfulness, 7(5), 1142–1155. doi:10.1007/s12671-016-0557-1
- Rzeszutek, M., & Gruszczyńska, E. (2018). Posttraumatic growth among people living with HIV: A systematic review. Journal of Psychosomatic Research, 114, 81–91. doi:10.1016/j.jpsychores.2018.09.006
- Sedighimornani, N., Rimes, K. A., & Verplanken, B. (2019). Exploring the relationships between mindfulness, self-compassion, and shame. SAGE Open, 9(3), 215824401986629. doi:10.1177/2158244019866294
- Sherman, K. A., Przezdziecki, A., Alcorso, J., Kilby, C. J., Elder, E., Boyages, J., … Mackie, H. (2018). Reducing body image–related distress in women with breast cancer using a structured online writing exercise: Results from the my changed body randomized controlled trial. Journal of Clinical Oncology, 36(19), 1930–1940. doi:10.1200/JCO.2017.76.3318
- Sirois, F. M., & Hirsch, J. K. (2019). Self-compassion and adherence in five medical samples: The role of stress. Mindfulness, 10(1), 46–54. doi:10.1007/s12671-018-0945-9
- Sirois, F. M., Molnar, D. S., & Hirsch, J. K. (2015). Self-compassion, stress, and coping in the context of chronic illness. Self and Identity, 14(3), 334–347. doi:10.1080/15298868.2014.996249
- Stirman, S. W., Miller, C. J., Toder, K., & Calloway, A. (2013). Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implementation Science, 8(1), 65. doi:10.1186/1748-5908-8-65
- Strauss, C., Lever Taylor, B., Gu, J., Kuyken, W., Baer, R., Jones, F., & Cavanagh, K. (2016). What is compassion and how can we measure it? A review of definitions and measures. Clinical Psychology Review, 47, 15–27. doi:10.1016/j.cpr.2016.05.004
- Thomas, J., & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8(1), 45. doi:10.1186/1471-2288-8-45
- Trindade, I. A., Duarte, J., Ferreira, C., Coutinho, M., & Pinto-Gouveia, J. (2018). The impact of illness‐related shame on psychological health and social relationships: Testing a mediational model in students with chronic illness. Clinical Psychology & Psychotherapy, 25, 408-414. doi:10.1002/cpp.2175
- Trindade, I. A., Ferreira, C., Borrego, M., Ponte, A., Carvalho, C., & Pinto-Gouveia, J. (2018). Going beyond social support: Fear of receiving compassion from others predicts depression symptoms in breast cancer patients. Journal of Psychosocial Oncology, 36(4), 520–528. doi:10.1080/07347332.2018.1440275
- Trompetter, H. R., de Kleine, E., & Bohlmeijer, E. T. (2017). Why does positive mental health buffer against psychopathology? An exploratory study on self-compassion as a resilience mechanism and adaptive emotion regulation strategy. Cognitive Therapy and Research, 41(3), 459–468. doi:10.1007/s10608-016-9774-0
- Van Gemert-Pijnen, J. E. W. C., Kip, H., & Kelders, S. M. (2018). Introducing eHealth. In J. E. W. C. van Gemert-Pijnen, S. M. Kelders, H. Kip, & R. Sanderman (Ed.), eHealth research, theory and development: A multidisciplinary approach (1st ed., pp. 3–26). London: Routledge.
- Van Houtum, L., Rijken, M., & Groenewegen, P. (2015). Do everyday problems of people with chronic illness interfere with their disease management? BMC Public Health, 15, 1000. doi:10.1186/s12889-015-2303-3
- Wensing, M., Oxman, A., Baker, R., Godycki-Cwirko, M., Flottorp, S., Szecsenyi, J., … Eccles, M. (2011). Tailored implementation for chronic diseases (TICD): A project protocol. Implementation Science, 6(1), 103. doi:10.1186/1748-5908-6-103
- Wierenga, K. L., Lehto, R. H., & Given, B. (2017). Emotion regulation in chronic disease populations: An integrative review. Research and Theory for Nursing Practice, 31(3), 247–271. doi:10.1891/1541-6577.31.3.247
- Williams, G. C., Lynch, M., & Glasgow, R. E. (2007). Computer-assisted intervention improves patient-centered diabetes care by increasing autonomy support. Health Psychology, 26(6), 728–734. doi:10.1037/0278-6133.26.6.728
- Ziemer, K. S., Fuhrmann, A., & Hoffman, M. A. (2015). Effectiveness of a positive writing intervention for chronic pain: A randomized trial. MYOPAIN, 23(3-4), 143–154. doi:10.1080/24708593.2017.1307893