Abstract
Objective: The incidence of skin cancer can be reduced by increasing sun protective behaviours. Based on the Common-Sense Model and the Intervention Mapping approach, a brief intervention targeting illness representations about skin cancer to increase the intention to conduct sun protective behaviours was developed and evaluated regarding its effectiveness.
Design: A randomized pre-post control group design with 509 healthy participants (69% women, mean age 39 years).
Main outcome measures: Changes in illness representations about skin cancer (emotional representations, illness coherence, and prevention control) and the intention to conduct sun protective behaviours, i.e. UV protection and sun avoidance.
Results: ANCOVAs showed that the intervention increased illness coherence and perceived prevention control as well as the intention to conduct sun protective behaviours. Mediation analyses revealed that the increase in illness coherence and/or perceived prevention control partially mediated the effect of the intervention on the increase of the intention to use UV protection (indirect effects: .02*, .06*) and to avoid sun exposure (indirect effects: .01 ns, .04*).
Conclusion: The intervention was successful in changing illness representations and thereby increasing the intention to conduct sun protective behaviours. The findings provide evidence for the usefulness of the Common-Sense Model in the context of illness prevention.
Skin cancer as behaviour-related disease
Skin cancer, including malignant melanoma and non-melanoma skin cancers, ranks among the top five most prevalent types of cancer both globally and in Germany (Bray et al., Citation2018; Robert Koch-Institut (RKI) & Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. (GEKID), Citation2017). According to the most recent GLOBOCAN statistics, there have been more than 1 million new non-melanoma skin cancer cases and about 288,000 new malignant melanoma skin cancer cases worldwide in 2018 (Bray et al., Citation2018). Over the past decades, the incidence of skin cancer has significantly increased (Apalla et al., Citation2017). For example, in Germany, the incidence of malignant melanoma skin cancers has more than quintupled since 1970 (RKI & GEKID, Citation2017).
Although skin cancer has a relatively low mortality rate (Bray et al., Citation2018; RKI & GEKID, Citation2017), the personal consequences for the patients and the economic burden for the society should not be underestimated. Skin cancer patients and skin cancer survivors experience physical symptoms, such as pain, fatigue, and insomnia, as well as limitations in physical, role, emotional, cognitive, and social functioning (Beutel et al., Citation2015; Linden et al., Citation2012; Mayer et al., Citation2017). This might be attributed to the treatment that often causes visible scarring and disfigurement (Sobanko et al., Citation2015) as well as the severe concerns of patients that the cancer could spread, recur, or develop (Burdon-Jones, Thomas, & Baker, Citation2010). As regards the economic burden, skin cancer carries considerable direct and indirect costs that will soar as incidence rates increase (Gordon & Rowell, Citation2015; Guy et al., Citation2015; Mofidi et al., Citation2018; RKI, Citation2016; Stang, Stausberg, Boedeker, Kerek-Bodden, & Jöckel, Citation2008). Direct costs arise from the multifaceted treatment of skin cancer (National Cancer Institute (NCI), Citation2018a, Citation2018b), while indirect costs are caused by productivity loss due to temporary or permanent incapacity for work, and premature death (Mofidi et al., Citation2018; RKI, Citation2016).
The main external risk factor for developing skin cancer is repeated excessive exposure to intensive solar ultraviolet (UV) radiation and subsequent sunburns (Armstrong et al., Citation2017; Gandini et al., Citation2005; de Gruijl, Citation1999), which is the reason why skin cancer mostly occurs on body parts that are usually exposed to the sun, such as face, neck, ears, chest, and forearms. As sun exposure and sunburns are avoidable by appropriate behaviours, i.e., sun protective behaviours, experts assume that the majority of skin cancer cases could be prevented (German Guideline Program in Oncology of the Association of Medical Scientific Societies (AWMF), German Cancer Society (DKG), & German Cancer Aid (DKH), Citation2014; World Health Organization (WHO), Citation2019a). Sun protective behaviours range from avoiding sun exposure at all (e.g., seeking shade and staying out of the midday sun) to taking precautions against overexposure when exposed to the sun (e.g., wearing protective clothing and regularly using sunscreen with a sun protection factor of at least 15) (AWMF et al., Citation2014; Cooley & Quale, Citation2013; Skin Cancer Foundation, Citation2019; WHO, Citation2019c).
Even though much effort has been put in primary prevention campaigns over the last decades (e.g., Doran et al., Citation2016; Nguyen et al., Citation2019; Stratigos et al., Citation2012), the regular engagement in sun protective behaviours is not yet widespread and sunburns are still prevalent. For example, three German studies found that 41% of the respondents had at least 1 sunburn in the previous year, that up to 17% of the respondents never use sunscreen, that only 30% of the respondents avoid sunbathing, and that only about half of the respondents regularly wear long-sleeved clothes, stay in the shade, and use sunscreen, respectively (Forsa & DAK Gesundheit, Citation2016; Engelhardt, Citation2016; Görig et al., Citation2018). These figures are similar in other countries, such as the United States, Denmark, and Australia (Fischer et al., Citation2016; Køster et al., Citation2010; Volkov et al., Citation2013). Therefore, identifying factors and processes that determine sun protective behaviours is highly valuable in order to develop effective interventions that promote sun protective behaviours to eventually prevent skin cancer.
Illness representations of skin cancer as determinants of sun protective behaviours
As the Common-Sense Model of self-regulation of health and illness (CSM; Leventhal et al., Citation2003; Leventhal et al., Citation2016; McAndrew et al., Citation2008) describes factors and processes that are involved in the management of current and future health threats, it is a suitable framework in the context of sun protective behaviours and skin cancer prevention. The CSM proposes that illness representations, i.e., subjective beliefs and emotions about an illness, determine the selection and initiation of coping responses in order to manage current and prevent future threats to health. Illness representations are primarily derived from own experiences with an illness, but also from observations of an illness in others as well as from presentations of an illness in mass media (Leventhal et al., Citation2016). According to the assumption of the CSM, patients as well as individuals who are not (yet) personally affected by an illness develop illness representations that guide their behaviours to deal with a health threat, i.e., behaviours to enhance health, to prevent illness, to cure or control illness, and to rehabilitate from illness (Figueiras & Alves, Citation2007; Leventhal et al., Citation1998).
Sun protective behaviours can be considered as an effort to deal with the threat of skin cancer as research showed that most individuals who conduct sun protective behaviours do so to prevent sunburn and skin cancer (Forsa & DAK Gesundheit, Citation2016; Mahler, Citation2014). According to the assumptions of the CSM (Leventhal et al., Citation2016), sun protective behaviours are determined by illness representations of skin cancer, and the few existing empirical findings indicate that illness representations about skin cancer of healthy individuals are indeed associated with intended and actual sun protective behaviours. The number of symptoms attributed to skin cancer as well as perceptions of more negative consequences, more personal, treatment and prevention control, a longer duration, and a better understanding of skin cancer were positively associated with the intention to conduct sun protective behaviours. More negative emotions and more concern about skin cancer were also positively related to the intention to conduct sun protective behaviours (Cameron, Citation2008; Engelhardt, Citation2016; Figueiras & Alves, Citation2007; Vollmann, Citation2015). For actual sun protective behaviours, a positive association with the intention to conduct sun protective behaviours and a negative association with the perception that skin cancer is controllable through treatment was found (Cameron, Citation2008).
Changing illness representations of skin cancer in order to increase sun protective behaviours
The processes described in the CSM (Leventhal et al., Citation2003, Citation2016; McAndrew et al., Citation2008) imply that changes in illness representations lead to changes in self-regulatory behaviours and eventually in health outcomes. Empirical findings confirm that illness representations are actually changeable through interventions and that interventions targeting illness representations in patients and in healthy individuals indeed result in changes in self-regulatory behaviours and health outcomes (Broadbent et al., Citation2015; Chilcot & Moss-Morris, Citation2013; Lee et al., Citation2011; Glattacker et al., Citation2012; Petrie et al., Citation2002; Weldam et al., Citation2017).
Based on the assumptions of the CSM, the findings regarding the relationship between illness representations about skin cancer and sun protective behaviours, and the findings regarding the impact of interventions targeting illness representations on self-regulatory behaviour, it seems reasonable to suggest that the engagement in sun protective behaviours can be increased by changing illness representations about skin cancer. To our knowledge, no interventions explicitly aiming at changing illness representations about skin cancer in order to increase sun protective behaviours exist.
The present study
The aims of the present study were to develop an intervention targeting illness representations about skin cancer to increase the intention to conduct sun protective behaviours and to investigate the effectiveness of the newly developed intervention. To this end, we partly made use of the Intervention Mapping approach, a framework for the development, implementation, and evaluation of theory- and evidence-informed health promotion interventions (Bartholomew et al., Citation2011).
In a first step, the general adult population, i.e., people who conduct sun protective behaviours unassistedly, was defined as the target group of the intervention, as excessive exposure to sunlight can damage all skin types at any age (WHO, Citation2019b). Also, aiming to change illness representations in order to increase the intention to conduct sun protective behaviours is more meaningful in adults, since illness representations are much more elaborated in adulthood than in younger ages (Schmidt & Fröhling, Citation2000). In a second step, the relevant sun protective behaviours were specified and the illness representation dimensions that should be targeted were selected. In line with various recommendations (AWMF et al., Citation2014; Skin Cancer Foundation, Citation2019; WHO, Citation2019c) as well as the earlier reported findings about the prevalence of sun protective behaviours in the German population, the intervention aimed at increasing using sunscreen with a sun protection factor of at least 15, wearing long-sleeved clothes, sunglasses, and headgear, informing about the actual UV radiation, staying indoors or in shade during noontime, and avoiding sunbathing. Based on the few earlier reported empirical findings on the relationship between illness representations about skin cancer and intentions to conduct sun protective behaviours (Cameron, Citation2008; Engelhardt, Citation2016; Figueiras & Alves, Citation2007; Vollmann, Citation2015), the illness representation dimensions emotional representations, illness coherence, and prevention control were identified as most important and therefore selected as targets of the intervention. In a third step, general program ideas were generated as well as theory-informed intervention methods and practical applications were selected. The intervention was conceptualized as an interactive one-session online intervention. In order to increase emotional representations, prevention control, coherence, and eventually the intention to conduct sun protective behaviours, the following theory-informed methods were chosen: fear arousal, scenario based risk information, advanced organizers, modelling, persuasive communication, arguments, reinforcement, punishment, and active learning (Bartholomew et al., Citation2011). These methods were translated into practical applications, i.e., the elements of the intervention such as videos, quizzes, examples, pictures, peer-model stories, summaries. In a fourth step, the structure of the intervention was determined and the intervention material was designed.1 The description of the intervention can be found in the method section. The last step was the evaluation of the intervention using a randomized pre-post control group design with one group receiving the intervention (intervention group) and one group receiving a placebo intervention (control group).
It was expected that the intervention would lead to a stronger increase in the illness representations (emotional representations, illness coherence, and prevention control) as well as a stronger increase in the intention to conduct sun protective behaviours in the intervention group compared to the control group. Further, based on the assumptions of the CSM, it was expected that the positive effects of the intervention on the increase in the intention to conduct sun protective behaviours are at least partially due to an increase in illness representations.
Method
Procedure
The online study was programmed in Questback’s survey software Unipark and had a randomized pre-post control group design. Directly after a detailed instruction, participants were randomly assigned to the intervention group or the control group by the software. In order to avoid missing data, all items were mandatory and could not be skipped. The study started with the assessment of socio-demographic and skin cancer related data as well as baseline measurements of illness representations about skin cancer and the intention to conduct sun protective behaviours (t0). In the next step, the intervention group received an intervention aiming at changing illness representations and the intention to conduct sun protective behaviours, whereas the control group received a placebo intervention, i.e., general information about (skin) cancer. The intervention phase lasted approximately 10 minutes. Finally, the follow-up measurements of illness representations about skin cancer and the intention to conduct sun protective behaviours (t1) were assessed. After a detailed debriefing, participants allocated to the control group were offered access to the ‘real’ intervention.
Interventions
Intervention group
The intervention provided to the intervention group contained five elements. The first element was the video “Protect your skin” from a campaign of the German Cancer Aid (Citation2015) against skin cancer. In this video the symptoms, causes, and consequences of skin cancer were shortly introduced by a medical doctor and a famous German skin cancer patient. The second, third, and fourth element focussed on information about the aetiology, incidence, and prevalence of skin cancer, the UV index, and different sun protective behaviours to prevent sunburn and skin cancer. Information was provided through written text, pictures, figures, quiz questions, and role models. The last element was the video “UV radiation” of the Federal Office for Radiation Protection (Citation2014) in which much of the provided information was summarized.1
Control group
The control group was provided with a placebo intervention that did not aim at changing illness representations of skin cancer and the intention to conduct sun protective behaviours. The placebo intervention contained four elements that were related to (skin) cancer, i.e., a questionnaire assessing possible causes of skin cancer (Gaab et al., Citation2008; Moss-Morris et al., Citation2002), general information about skin cancer with a focus on uncommon types of skin cancer (Wikipedia, Citation2016), the history of the German Cancer Aid (Citation2019), and the video “Physical activity against cancer” from a campaign of the German Cancer Aid (Citation2014) against cancer.
Participants
In order to obtain a large and heterogeneous sample, participants were invited to take part in the study via posts on the internet (e.g., social media, electronic university blackboard), via e-mails that were spread among the social networks of the researchers including the request to pass the e-mail on, and via postcards from the Hessian Cancer Association (Citation2012) themed “You are precious” that were posted in different boroughs of Berlin. After opening the provided link, participants received a detailed description of the study and an instruction in which voluntary participation and anonymity were emphasized. Participants could take part in a raffle for eight gift vouchers. Students of the University of Hagen could receive course credit for participation. Participants signed an informed consent and were treated according to the American Psychological Association (APA) ethical standards.
Inclusion criteria were a minimum age of 18 years and currently not diagnosed with skin cancer. A total of 523 participants who met the inclusion criteria completed all questionnaires. Of these, 14 participants were excluded because of response inconsistency (Johnson, Citation2005). The final sample consisted of 509 participants, of which 353 were female (69.4%) and 156 were male (30.6%). The mean age of the participants was 39 years (SD = 13.96, range 18–92 years). The sample was highly educated with 86.8% having at least a higher education entrance qualification. About half of the participants was employed or self-employed (50.5%), while the remaining participants were students or in training (36.5%), retired (5.1%), homemakers (3.1%), or did not specify their employment status (4.9%).
Measures
Illness representations about skin cancer
A modified German version of the Illness Perception Questionnaire (IPQ-R; Gaab et al., Citation2008; Moss-Morris et al., Citation2002) was used to measure the three illness representation dimensions that were identified as most influential in the context of sun protective behaviours. Following the recommendation of Moss-Morris et al. (Citation2002) to adapt the IPQ-R to specific illnesses, the word ‘illness’ was replaced with ‘skin cancer’. Also, as in the IPQ-R for healthy people (IPQ-RH; Figueiras & Alves, Citation2007), the wording of the items was adapted so that they can be answered by people who are not diagnosed with skin cancer. Responses were given on a 5-point scale ranging from 1 ‘strongly disagree’ to 5 ‘strongly agree’.
Emotional representations
Emotional representations about skin cancer were assessed with 5 items (e.g., ‘Skin cancer makes me feel afraid’). Items were averaged with higher scores indicating stronger emotional responses to skin cancer. Cronbach’s alphas were .89 at t0 and .93 at t1. Also, a change score was calculated (t1-t0), with higher scores indicating an increase in emotional representations.
Illness coherence
Illness coherence was measured with 6 items (e.g., ‘I have a clear understanding of skin cancer’). Items were recoded if appropriate and averaged with higher scores indicating a greater extent of understanding skin cancer. Cronbach’s alpha was .87 at t0 and t1. Also, a change score was calculated (t1-t0), with higher scores indicating an increase in illness coherence.
Prevention control
Following Cameron (Citation2008), beliefs about prevention control were measured with 6 newly formulated items (e.g., ‘Skin cancer can be prevented by own behaviour’ and ‘You can do something against getting skin cancer’). Items were averaged with higher scores indicating stronger beliefs about prevention control. Cronbach’s alphas were .84 at t0 and .90 at t1. Also, a change score was calculated (t1-t0), with higher scores indicating an increase in prevention control.
Intention to conduct sun protective behaviours
The intention to conduct sun protective behaviours was measured with 10 items focusing on different behaviours that have been identified as protective or risk behaviours (AWMF et al., Citation2014; Skin Cancer Foundation, Citation2019; WHO, Citation2019c). Participants were asked to envisage that the upcoming weekend will be sunny and warm, and to indicate how they probably will behave on a 7-point scale ranging from 1 ‘by no means’ to 7 ‘by all means’. The factor structure of the behaviours was examined by a principal component analysis with VARIMAX-rotation. The analysis suggested a two-factor solution (eigenvalues 3.60, 1.75, 0.95, 0.81, 0.74 …) with the two factors accounting for 53.5% of the total variance. The first factor, labelled as UV protection, included 5 items representing active behaviours to protect the body from UV radiation (i.e., ‘protecting the head with a hat or other headgear’, ‘wearing sunglasses’, ‘regularly using sunscreen with a sun protection factor of at least 15′, ‘inform about the actual UV radiation’, ‘adapt the sun protection according to the actual UV radiation’). The second factor, named sun avoidance, included 4 items related to proactive behaviours to avoid sun exposure at all (i.e., ‘seek shade during noontime’, ‘stay indoors during noontime’, ‘taking a sunbath’ (reverse), ‘soak up sun’ (reverse)). The item ‘wearing clothes with long sleeves and pant legs’ was excluded due to high loadings on both factors. Items of each factor were recoded if appropriate and averaged so that higher scores indicate a greater intention to use UV protection and to avoid sun exposure, respectively. Cronbach’s alphas of the two scales were .72 and .79 for t0 and .79 and .82 for t1. Also, change scores were calculated (t1-t0), with higher scores indicating an increase in the intention to use UV protection and to avoid sun exposure, respectively.
Socio-demographic and skin cancer related data
Basic socio-demographic characteristics were assessed, i.e., age, gender, highest education level, and employment status. Also, participants were asked whether they are currently diagnosed with skin cancer and whether they were diagnosed with skin cancer in the past. Finally, participants had to indicate their skin type according to Fitzpatrick’s classification system (Citation1988). Skin type 1 (pale white; blond or red hair; blue eyes; freckles) and skin type 2 (white; fair; blond or red hair; blue, green, or hazel eyes) were coded as high risk skin type, while the other 4 skin types (3–6) were coded as low risk skin type (WHO, Citation2019b).
Data analyses
Statistical analyses were performed with SPSS 25 and the SPSS macro PROCESS. In a first step, it was examined whether the randomization succeeded in producing two equal groups with regard to socio-demographic characteristics, skin cancer related variables and baseline measurements by means of t-tests and χ-tests.
In all subsequent analyses, skin type was entered as control variable because, although excessive exposure to sunlight can damage all skin types, individuals with pale or freckled skin (skin types I and II, Fitzpatrick, Citation1988) are more vulnerable (WHO, Citation2019b) and therefore more likely to engage in sun protective behaviours (Görig et al., Citation2018).
In a second step, after checking the assumptions, five 2 (group: control group vs. intervention group) x 2 (time: t0 vs. t1) mixed design analyses of covariance (ANCOVAs) with skin type as covariate were calculated in order to investigate whether group affiliation had a differential effect on changes in the three illness representation dimensions and in the intention to conduct the two forms of sun protective behaviours. Significant differential effects of group affiliation, indicated by a significant interaction term (group x time), were further explored by Bonferroni adjusted simple main effects of time for each of the groups.
In a third step, after checking the assumptions, two parallel multiple mediation analyses with group (control group vs. intervention group) as independent variable, the change in emotional representations, illness coherence, and prevention control as mediators, the change in the intention to use UV protection and in the intention to avoid sun exposure, respectively, as dependent variable, and skin type as control variable were calculated in order to investigate whether the effects of the intervention on the increase in the intention to conduct the two forms of sun protective behaviours are due to an increase in illness representations. The mediation analyses comprised the following steps (Hayes, Citation2018): First, the effects of the intervention on changes in illness representations were estimated by three multiple regression analyses with skin type and group as independent variables and the change in the respective illness representation dimension as dependent variable. Second, in order to estimate the total and direct effect of the intervention on the changes in the intention to conduct sun protective behaviours, two hierarchical regression analyses with skin type and group (step 1) and the change in emotional representations, illness coherence, and prevention control (step 2) as predictors, and the change in the intention to use UV protection and in the intention to avoid sun exposure, respectively, as dependent variable were calculated. Total effects refer to the impact of the intervention on the change in the intention to use UV protection and in the intention to avoid sun exposure (step 1), while direct effects refer to the impact of the intervention on the change in the intention to use UV protection and in the intention to avoid sun exposure while controlling for changes in all three illness representation dimensions (step 2). Also, the direct effects of the changes in illness representations on the change in the intention to use UV protection and in the intention to avoid sun exposure were calculated (step 2). Third, the indirect effects of the intervention on changes in the intention to conduct sun protective behaviours through changes in all three illness representation dimensions and through each single illness representation dimension were determined by means of bootstrap analyses with 5000 bootstrap samples. All coefficients are reported in standardized form.
Results
Randomization
The randomization resulted in 255 and 254 participants being assigned to the intervention group (coded as 1) and control group (coded as 0), respectively. The two groups did not differ with regard to demographic characteristics and baseline measures (see ).
Table 1. Socio-demographic and skin cancer related variables as well as baseline measurements for the intervention group and the control group.
Effects of the intervention on illness representations and sun protective behaviours
In both groups, skewness and kurtosis estimates for all variables were within the acceptable range, indicating normal distribution. Also, in both groups the covariate was linearly related to all variables. The evaluation of the homogeneity of variance-covariance matrices was not necessary as the sample sizes were equal.
The results of the ANCOVAs are presented in as well as in .
Figure 1. Mean values of illness representations (left) and intention to conduct sun protective behaviours (right) for the intervention group and control group at t0 and t1. Skin type was included as covariate.
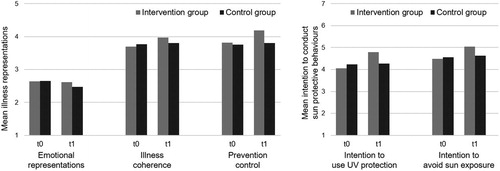
Table 2. Results of the 2 (group: control group vs. intervention group) x 2 (time: t0 vs. t1) analyses of covariance.
All three ANCOVAs with regard to the illness representations revealed a significant interaction between group and time, indicating that group affiliation had a differential effect on changes in the three illness representation dimensions. The simple main effects indicated that emotional representations remained stable in the intervention group, p = .398, and significantly decreased in the control group, p = .029; that illness coherence significantly increased in the intervention group, p < .001, and remained stable in the control group, p = .226; and that prevention control significantly increased in both groups, with a stronger increase for the intervention group, p < .001, than for the control group, p = .041.
Also, both ANCOVAs regarding the intention to conduct sun protective behaviours obtained a significant interaction effect, indicating that group affiliation had a differential effect on changes in the intention to conduct the two forms of sun protective behaviours. The simple main effects indicated that both the intention to use UV protection and the intention to avoid sun exposure significantly increased in the intervention group, ps < .001, and remained stable in the control group, p = .475 and p = .069.
Effects of the intervention on the increase in the intention to conduct sun protective behaviours through the change in illness representations
All assumptions of multiple regression analysis, i.e., normality, homoscedasticity, linearity, and multicollinearity, were met.
Because the intervention failed to increase emotional representations, this illness representation dimension was excluded from the mediation analyses. Thus, the mediation analyses were calculated with group as independent variable, the change in illness coherence and prevention control as mediators, the change in the intention to use UV protection and in the intention to avoid sun exposure, respectively, as dependent variable, and skin type as control variable. The coefficients obtained from the regression analyses are presented in .
Figure 2. Results of the regression analyses as part of the mediation analyses. Coefficients before the slash refer to the intention to use UV protection as outcome, while coefficients after the slash refer to the intention to avoid sun exposure as outcome. Total effects derived from step 1 of the hierarchical regression analyses are displayed in parentheses. Skin type was included as control variable (coefficients not shown). *** p <.001, ** p <.01,* p <.05.
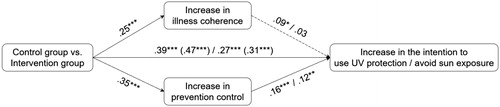
First, the multiple regression analyses yielded a significant positive effect of group affiliation on the change of illness coherence and the change of prevention control, indicating that participants in the intervention group had a stronger increase in the understanding of skin cancer and in the perception that skin cancer can be prevented by own behaviour than participants in the control group. In total, 6.1% and 12.4% of the variance in the change of illness coherence and prevention control, respectively, could be explained.
Second, the hierarchical regression analyses showed that group affiliation had a positive total (step 1) and direct effect (step 2) on the change in the intention to use UV protection and in the intention to avoid sun exposure, indicating that participants in the intervention group reported a stronger increase in the intention to conduct both forms of sun protective behaviours than participants in the control group. Further, the changes in illness coherence and prevention control (step 2) were positively related to the change in the intention to use UV protection, while only the change in prevention control was positively related to the change in the intention to avoid sun exposure. This indicates that an increase in the understanding of skin cancer results in an increase in the intention to use UV protection and that an increase in the perception that skin cancer can be prevented by own behaviour results in an increase in the intention to use UV protection and in the intention to avoid sun exposure. In total, 26% and 11% of the variance in the change in the intention to use UV protection and in the intention to avoid sun exposure, respectively, could be explained.
Third, bootstrap analyses revealed significant positive total indirect effects of group affiliation on the change in the intention to conduct both forms of sun protective behaviours via the two illness representation dimensions, .08, bias corrected (BC) 95% confidence interval (CI) [.0412, .1231] for UV protection and .05, BC 95% CI [.0101, .0906] for sun avoidance. Additionally, significant specific indirect effects of group affiliation on the change in the intention to use UV protection through the change in illness coherence, .02, BC 95% CI [.0025, .0511], and the change in prevention control, .06, BC 95% CI [.0234, .0954] as well as of group affiliation on the change in the intention to avoid sun exposure through the change in prevention control, .04, BC 95% CI [.0070, .0779], were found. This indicates that the intervention leads to an increase in the intention to conduct sun protective behaviours due to a better understanding of skin cancer (in case of UV protection) and due to an increase in the perception that skin cancer can be prevented by own behaviour (in case of UV protection and sun avoidance).
Discussion
The present study investigated the effectiveness of a newly developed brief multimodal online intervention in changing illness representations about skin cancer and thereby increasing the intention to conduct sun protective behaviours by using a randomized pre-post control group design.
Our findings indicate that the intervention successfully changed illness representations about skin cancer and increased the intention to conduct sun protective behaviours. This is in line with previous research showing that illness representations are changeable through interventions and that interventions targeting illness representations result in changes in the intention to conduct and/or in the actual health and illness behaviours (Broadbent et al., Citation2015; Chilcot & Moss-Morris, Citation2013; Glattacker et al., Citation2012; Lee et al., Citation2011; Petrie et al., Citation2002; Weldam et al., Citation2017). Since the development of the brief intervention was guided by the principles of the Intervention Mapping approach (Bartholomew et al., Citation2011), there is reason to assume that its effectiveness is partly due to the theory- and evidence-based footing.
As expected, the understanding of skin cancer and the perception that skin cancer can be prevented by own behaviour as well as the intention to use UV protection and to avoid sun exposure increased as a result of the intervention. However, emotional representations of skin cancer remained stable in the intervention group, which is contrary to the expectations. This result might be due to the logic pattern of interrelations between the three illness representation dimensions, more specifically, the generic negative relationships of illness coherence and control perceptions with emotional representations (Hagger et al., Citation2017). This pattern indicates that higher levels of understanding and perceived control usually come along with lower levels of negative emotions, which makes it apparently impossible to simultaneously increase all three dimensions. Thus, to frighten people and to make them more educated and self-effective is incompatible within one intervention. Accordingly, it can be speculated that emotional representations increased in the beginning of the intervention after the provision of fear-arousal messages, but dropped back in the course of the intervention when coping options and role models were provided that increased the understanding of skin cancer and the perception of prevention control through own behaviour.
More importantly, in accordance with the expectations, our findings imply that the positive effects of the intervention on increasing intentions to conduct sun protective behaviours are partially due to changes in illness representations. More specifically, the intervention led to an increase in the intention to use UV protection and to avoid sun exposure through increasing the understanding of skin cancer and/or the perception that skin cancer can be prevented by own behaviour. This is in line with research on the relevance of psychoeducation for supporting behaviour change (Lukens & McFarlane, Citation2004). It can be assumed that the information provided in the intervention helped the participants to develop more elaborated illness representations of skin cancer, including effective prevention measures, that subsequently impacted their intention to conduct sun protective behaviours. Also, the importance of operationalizing prevention control as an independent dimension of illness representations, at least for some health risks, is supported by the results obtained in the present study. In the past, the CSM has mostly been used as a framework in research on diseases with a multifaceted and complex aetiology, like heart disease (e.g., Hirani & Newman, Citation2005) or diabetes (Hudson et al., Citation2014). For health threats with relatively circumscribed and well-known, comparatively easily applicable prevention strategies such as skin cancer or influenza (Mo & Lau, Citation2015), it seems promising to consider prevention control as an additional dimension of illness representations that enhances the amount of variance explained in intended and actual preventive behaviours.
Not unexpectedly, changes in illness representations only partially accounted for the effect of the intervention on the increased intention to conduct sun protective behaviours, indicating that additional processes underlie the effectiveness of the intervention. These processes might be changes in other illness representation dimensions, such as perception about consequences and duration, and changes in other well-known determinants of self-regulatory behaviours, such as self-efficacy and attitudes, as the intervention contained elements that also affect these processes (Bartholomew et al., Citation2011).
Taken together, the findings are predominantly in line with the assumption of the CSM that changes in illness representations would lead to changes in self-regulation (Leventhal et al., Citation2003, Citation2016; McAndrew et al., Citation2008) and provide support for our proposition that the CSM might be a useful framework in the context of sun protective behaviours and skin cancer prevention. Accordingly, including illness representations about skin cancer as additional determinants of behaviour change might contribute to the effectiveness of campaigns aiming at the promotion of sun protective behaviours.
Limitations
Some limitations of the present study need to be acknowledged. First, the present convenience sample consisted of highly educated adults, and so the findings may not generalize to populations with different educational backgrounds. Second, short-term changes in the intention to conduct sun protective behaviours have been investigated as outcome, while an increase in the intention does not guarantee an increase in actual sun protective behaviours in the long run (intention-behaviour gap; e.g., Sheeran & Webb, Citation2016). On the other hand, previous research showed that up to 26% of the variance in actual sun protective behaviours could be explained by behavioural intentions (Allom et al., Citation2013; Cameron, Citation2008), indicating that an increase in the intention to conduct sun protective behaviours might translate to some extent into an increase in actual sun protective behaviours. Third, only the changes of three illness representation dimensions have been investigated as mechanisms underlying the effectiveness of the intervention. However, as the illness representation dimensions are systematically interrelated (Hagger et al., Citation2017), it is reasonable to assume that other dimensions (e.g., consequences, causes) have changed through the interventions as well. Additionally, it is most likely that not only illness representations, but also other determinants of preventive behaviours (e.g., self-efficacy, attitudes) have changed, as the intervention development was based on a number of theoretical methods and practical applications. Future studies would profit from investigating the effectiveness of the intervention in increasing actual sun protective behaviours in a more heterogeneous sample and in the long run while considering multiple determinants of preventive behaviours as underlying mechanisms.
Conclusions
The Intervention Mapping-guided intervention showed to be effective in increasing the understanding of skin cancer and the perception that skin cancer can be prevented by own behaviour, and subsequently in increasing the intention to use UV protection and to avoid sun exposure. Our results lend support to the assumption that illness representations are changeable by appropriate interventions and that changes in illness representations translate into changes in behavioural intentions that might result in behaviour change. Also, our findings provide evidence for the notion that prevention control should be considered as a relevant illness representation dimension when studying prevention of health threats with similar characteristics.
Disclosure statement
No potential conflict of interest was reported by the authors.
Note
Notes
1 Detailed information about the intervention development following the Intervention Mapping approach (Bartholomew et al., Citation2011) and the intervention materials can be requested from the corresponding author.
References
- Allom, V., Mullan, B., & Sebastian, J. (2013). Closing the intention-behaviour gap for sunscreen use and sun protection behaviours. Psychology & Health, 28(5), 477–494. https://doi.org/10.1080/08870446.2012.745935
- Apalla, Z., Nashan, D., Weller, R. B., & Castellsagué, X. (2017). Skin cancer: Epidemiology, disease burden, pathophysiology, diagnosis, and therapeutic approaches. Dermatology and Therapy, 7(Suppl 1), 5–19. https://doi.org/10.1007/s13555-016-0165-y
- Armstrong, B. K., & Cust, A. E. (2017). Sun exposure and skin cancer, and the puzzle of cutaneous melanoma: A perspective on Fears et al. Mathematical models of age and ultraviolet effects on the incidence of skin cancer among whites in the United States. American Journal of Epidemiology 1977; 105: 420-427. Cancer Epidemiology, 48, 147–156. https://doi.org/10.1016/j.canep.2017.04.004
- Bartholomew, L. K., Parcel, G. S., Kok, G., Gottleib, N. H., & Fernández, M. E. (2011). Planning health promotion programs: An intervention mapping approach. Jossey-Bass.
- Beutel, M. E., Fischbeck, S., Binder, H., Blettner, M., Brähler, E., Emrich, K., Friedrich-Mai, P., Imruck, B. H., Weyer, V., & Zeissig, S. R. (2015). Depression, anxiety and quality of life in long-term survivors of malignant melanoma: A register-based cohort study. PLOS One, 10(1), e0116440. https://doi.org/10.1371/journal.pone.0116440
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a Cancer Journal for Clinicians, 68(6), 394–424. https://doi.org/10.3322/caac.21492
- Broadbent, E., Wilkes, C., Koschwanez, H., Weinman, J., Norton, S., & Petrie, K. J. (2015). A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychology & Health, 30(11), 1361–1385. https://doi.org/10.1080/08870446.2015.1070851
- Burdon-Jones, D., Thomas, P., & Baker, R. (2010). Quality of life issues in nonmetastatic skin cancer. British Journal of Dermatology, 162(1), 147–151. https://doi.org/10.1111/j.1365-2133.2009.09469.x
- Cameron, L. D. (2008). Illness risk representations and motivations to engage in protective behavior: The case of skin cancer risk. Psychology & Health, 23(1), 91–112. https://doi.org/10.1080/14768320701342383
- Chilcot, J., & Moss-Morris, R. (2013). Changes in illness-related cognitions rather than distress mediate improvements in irritable bowel syndrome (IBS) symptoms and disability following a brief cognitive behavioural therapy intervention. Behaviour Research and Therapy, 51(10), 690–695. https://doi.org/10.1016/j.brat.2013.07.007
- Cooley, J. H., & Quale, L. M. (2013). Skin cancer preventive behavior and sun protection recommendations. Seminars in Oncology Nursing, 29(3), 223–226. https://doi.org/10.1016/j.soncn.2013.06.008
- de Gruijl, F. R. (1999). Skin cancer and solar UV radiation. European Journal of Cancer, 35(14), 2003–2009. https://doi.org/10.1016/S0959-8049(99)00283-X
- Doran, C. M., Ling, R., Byrnes, J., Crane, M., Shakeshaft, A. P., Searles, A., & Perez, D. (2016). Benefit cost analysis of three skin cancer public education mass-media campaigns implemented in New South Wales, Australia. PLoS One, 11(1), e0147665. https://doi.org/10.1371/journal.pone.0147665
- Engelhardt, G. (2016). Subjektive Krankheitstheorien gesunder Menschen und Prävention [Illness representations of healthy people and prevention] [Unpublished data]. Available upon request from the corresponding author.
- Federal Office for Radiation Protection. (2014). UV Strahlung [UV radiation]. https://youtu.be/3G8f4FN7qyM
- Figueiras, M. J., & Alves, N. C. (2007). Lay perceptions of serious illnesses: An adapted version of the Revised Illness Perception Questionnaire (IPQ-R) for healthy people. Psychology & Health, 22(2), 143–158. https://doi.org/10.1080/14768320600774462
- Fischer, A. H., Wang, T. S., Yenokyan, G., Kang, S., & Chien, A. L. (2016). Sunburn and sun-protective behaviors among adults with and without previous nonmelanoma skin cancer (NMSC): A population-based study. Journal of the American Academy of Dermatology, 75(2), 371–379. e5. https://doi.org/10.1016/j.jaad.2016.02.1236
- Fitzpatrick, T. B. (1988). The validity and practicality of sun-reactive skin types I through VI. Archives of Dermatology, 124(6), 869–871. https://doi.org/10.1001/archderm.1988.01670060015008
- Forsa & DAK Gesundheit. (2016). Verhalten in Bezug auf Sonnenschutz [Sun protective behaviours]. https://docplayer.org/42120084-Verhalten-in-bezug-auf-sonnenschutz.html
- Gaab, J., Latanzia-Bunschoten, S., Sprott, H., & Ehlert, U. (2008). IPQ - Illness Perception Questionnaire (deutsche Version) [IPQ - Illness Perception Questionnaire (German version)]. In J. Bengel, M. Wirtz, & C. Zwingmann (Eds.), Diagnostische verfahren in der rehabilitation [Diagnostic instruments in rehabilitation] (pp. 109–111). Hogrefe.
- Gandini, S., Sera, F., Cattaruzza, M. S., Pasquini, P., Picconi, O., Boyle, P., & Melchi, C. F. (2005). Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. European Journal of Cancer, 41(1), 45–60. https://doi.org/10.1016/j.ejca.2004.10.016
- German Cancer Aid. (2014). Bewegung gegen Krebs: Spot mit Britta Heidemann [ Spot with Britta Heidemann]. https://youtu.be/VCTJV3f0uQM
- German Cancer Aid. (2015). Schütz’ deine Haut [Protect your skin]. https://youtu.be/0iIYbDUa69w
- German Cancer Aid. (2019). About us: Deutsche Krebshilfe/German Cancer Aid. https://www.krebshilfe.de/informieren/ueber-uns/deutsche-krebshilfe/about-us-deutsche-krebshilfegerman-cancer-aid/
- German Guideline Program in Oncology of the Association of Medical Scientific Societies (AWMF), German Cancer Society (DKG), & German Cancer Aid (DKH). (2014). Evidence-based guideline on prevention of skin cancer, long version 1.1. https://www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/Downloads/Leitlinien/Hautkrebspraeventationsleitlinie_1.1/Long_version_-_Guideline_on_prevention_of_skin_cancer.pdf
- Glattacker, M., Heyduck, K., & Meffert, C. (2012). Illness beliefs, treatment beliefs and information needs as starting points for patient information-evaluation of an intervention for patients with chronic back pain. Patient Education and Counseling, 86(3), 378–389. https://doi.org/10.1016/j.pec.2011.05.028
- Gordon, L. G., & Rowell, D. (2015). Health system costs of skin cancer and cost-effectiveness of skin cancer prevention and screening: A systematic review. European Journal of Cancer Prevention : The Official Journal of the European Cancer Prevention Organisation (Ecp)), 24(2), 141–149. https://doi.org/10.1097/cej.0000000000000056
- Görig, T., Diehl, K., Greinert, R., Breitbart, E. W., & Schneider, S. (2018). Prevalence of sun-protective behaviour and intentional sun tanning in German adolescents and adults: Results of a nationwide telephone survey. Journal of the European Academy of Dermatology and Venereology, 32(2), 225–235. https://doi.org/10.1111/jdv.14376
- Guy, G. P., Jr., Machlin, S. R., Ekwueme, D. U., & Yabroff, K. R. (2015). Prevalence and costs of skin cancer treatment in the U.S., 2002-2006 and 2007-2011. American Journal of Preventive Medicine, 48(2), 183–187. https://doi.org/10.1016/j.amepre.2014.08.036
- Hagger, M. S., Koch, S., Chatzisarantis, N. L. D., & Orbell, S. (2017). The Common Sense Model of self-regulation: Meta-analysis and test of a process model. Psychological Bulletin, 143(11), 1117–1154. https://doi.org/10.1037/bul0000118
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis. A regression-based approach. Guilford Press.
- Hessian Cancer Association. (2012). Du bist kostbar [You are precious]. http://www.du-bist-kostbar.de/
- Hirani, S. P., & Newman, S. P. (2005). Patients' beliefs about their cardiovascular disease. Heart, 91(9), 1235–1239. https://doi.org/10.1136/hrt.2003.025262
- Hudson, J. L., Bundy, C., Coventry, P. A., & Dickens, C. (2014). Exploring the relationship between cognitive illness representations and poor emotional health and their combined association with diabetes self-care. A systematic review with meta-analysis. Journal of Psychosomatic Research, 76(4), 265–274. https://doi.org/10.1016/j.jpsychores.2014.02.004
- Johnson, J. A. (2005). Ascertaining the validity of individual protocols from web-based personality inventories. Journal of Research in Personality, 39, 103–129. https://doi.org/10.1016/j.jrp.2004.09.009
- Køster, B., Thorgaard, C., Philip, A., & Clemmensen, I. H. (2010). Prevalence of sunburn and sun-related behaviour in the Danish population: A cross-sectional study. Scandinavian Journal of Public Health, 38(5), 548–552. https://doi.org/10.1177/1403494810371250
- Lee, T. J., Cameron, L. D., Wünsche, B., & Stevens, C. (2011). A randomized trial of computer-based communications using imagery and text information to alter representations of heart disease risk and motivate protective behaviour. British Journal of Health Psychology, 16(1), 72–91. https://doi.org/10.1348/135910710x511709
- Leventhal, H., Brissette, I., & Leventhal, E. A. (2003). The common-sense model of self-regulation of health and illness. In L. D. Cameron & H. Leventhal (Eds.), The self-regulation of health and illness behaviour (pp. 42–65). Routledge.
- Leventhal, H., Leventhal, E. A., & Contrada, R. J. (1998). Self-regulation, health, and behaviour: A perceptual-cognitive approach. Psychology & Health, 13(4), 717–733. https://doi.org/10.1080/08870449808407425
- Leventhal, H., Phillips, L., & Burns, E. (2016). The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. Journal of Behavioral Medicine, 39(6), 935–946. https://doi.org/10.1007/s10865-016-9782-2
- Linden, W., Vodermaier, A., MacKenzie, R., & Greig, D. (2012). Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. Journal of Affective Disorders, 141(2-3), 343–351. https://doi.org/10.1016/j.jad.2012.03.025
- Lukens, E. P., & McFarlane, W. R. (2004). Psychoeducation as evidence-based practice: Considerations for practice, research, and policy. Brief Treatment and Crisis Intervention, 4(3), 205–225. https://doi.org/10.1093/brief-treatment/mhh019
- Mahler, H. I. M. (2014). Reasons for using and failing to use sunscreen: Comparison among Whites, Hispanics, and Asian/Pacific Islanders in Southern California. JAMA Dermatology, 150(1), 90–91. https://doi.org/10.1001/jamadermatol.2013.4992
- Mayer, S., Teufel, M., Schaeffeler, N., Keim, U., Garbe, C., Eigentler, T. K., Zipfel, S., & Forschner, A. (2017). The need for psycho-oncological support for melanoma patients: Central role of patients' self-evaluation. Medicine, 96(37), e7987. https://doi.org/10.1097/md.0000000000007987
- McAndrew, L. M., Musumeci-Szabó, T. J., Mora, P. A., Vileikyte, L., Burns, E., Halm, E. A., Leventhal, E. A., & Leventhal, H. (2008). Using the common sense model to design interventions for the prevention and management of chronic illness threats: From description to process. British Journal of Health Psychology, 13(2), 195–204. https://doi.org/10.1348/135910708x295604
- Mo, P. K., & Lau, J. T. (2015). Illness representation on H1N1 influenza and preventive behaviors in the Hong Kong general population. Journal of Health Psychology, 20(12), 1523–1533. https://doi.org/10.1177/1359105313516031
- Mofidi, A., Tompa, E., Spencer, J., Kalcevich, C., Peters, C. E., Kim, J., Song, C., Mortazavi, S. B., & Demers, P. A. (2018). The economic burden of occupational non-melanoma skin cancer due to solar radiation. Journal of Occupational and Environmental Hygiene, 15(6), 481–491. https://doi.org/10.1080/15459624.2018.1447118
- Moss-Morris, R., Weinman, J., Petrie, K. J., Horne, R., Cameron, L. D., & Buick, D. (2002). The revised Illness Perception Questionnaire (IPQ-R). Psychology & Health, 17(1), 1–16. https://doi.org/10.1080/08870440290001494
- National Cancer Institute (NCI). (2018a). Melanoma treatment (PDQ®)-health professional version. https://www.cancer.gov/types/skin/hp/melanoma-treatment-pdq#section/_885
- National Cancer Institute (NCI). (2018b). Skin cancer treatment (PDQ®)-health professional version. https://www.cancer.gov/types/skin/hp/skin-treatment-pdq#section/_497
- Petrie, K. J., Cameron, L., Ellis, C. J., Buick, D., & Weinman, J. (2002). Changing illness perceptions after myocardial infarction: An early intervention randomized controlled trial. Psychosomatic Medicine, 64, 580–586.
- Nguyen, J., Gilbert, L., Priede, L., & Heckman, C. (2019). The reach of the “Don’t Fry Day” twitter campaign: Content analysis. JMIR Dermatology, 2(1), e14137. https://doi.org/10.2196/14137
- Robert Koch-Institut (RKI). (2016). Bericht zum Krebsgeschehen in Deutschland 2016 [German Cancer Report 2016]. https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebsgeschehen/Krebsgeschehen_download.pdf?__blob=publicationFile https://doi.org/10.17886/rkipubl-2016-014
- Robert Koch-Institut (RKI) & Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. (GEKID). (2017). Krebs in Deutschland für 2013/2014 [Cancer in Germany 2013/2014]. https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebs_in_Deutschland/kid_2017/krebs_in_deutschland_2017.pdf?__blob=publicationFile https://doi.org/10.17886/rkipubl-2017-007
- Schmidt, L. R., & Fröhling, H. (2000). Lay concepts of health and illness from a developmental perspective. Psychology & Health, 15(2), 229–238. https://doi.org/10.1080/08870440008400303
- Skin Cancer Foundation. (2019). Prevention guidelines. https://www.skincancer.org/prevention/sun-protection/prevention-guidelines
- Sheeran, P., & Webb, T. L. (2016). The intention–behavior gap. Social and Personality Psychology Compass, 10(9), 503–518. https://doi.org/10.1111/spc3.12265
- Sobanko, J. F., Sarwer, D. B., Zvargulis, Z., & Miller, C. J. (2015). Importance of physical appearance in patients with skin cancer. Dermatologic Surgery, 41(2), 183–188. https://doi.org/10.1097/dss.0000000000000253
- Stang, A., Stausberg, J., Boedeker, W., Kerek-Bodden, H., & Jöckel, K.-H. (2008). Nationwide hospitalization costs of skin melanoma and non-melanoma skin cancer in Germany. Journal of the European Academy of Dermatology and Venereology, 22(1), 65–72. https://doi.org/10.1111/j.1468-3083.2007.02334.x
- Stratigos, A. J., Forsea, A. M., van der Leest, R. J. T., de Vries, E., Nagore, E., Bulliard, J.-L., Trakatelli, M., Paoli, J., Peris, K., Hercogova, J., Bylaite, M., Maselis, T., Correia, O., & del Marmol, V. (2012). Euromelanoma: A dermatology-led European campaign against nonmelanoma skin cancer and cutaneous melanoma. Past, present and future. British Journal of Dermatology, 167, 99–104. https://doi.org/10.1111/j.1365-2133.2012.11092.x
- Vollmann, M. (2015). Application of the Common-Sense Model of self-regulation of health and illness on sun protection behaviours as prevention of skin cancer [Unpublished data]. Available upon request from the corresponding author.
- Volkov, A., Dobbinson, S., Wakefield, M., & Slevin, T. (2013). Seven-year trends in sun protection and sunburn among Australian adolescents and adults. Australian and New Zealand Journal of Public Health, 37(1), 63–69. https://doi.org/10.1111/1753-6405.12012
- Weldam, S. W., Schuurmans, M. J., Zanen, P., Heijmans, M. J., Sachs, A. P., & Lammers, J.-W J. (2017). The effectiveness of a nurse-led illness perception intervention in COPD patients: A cluster randomised trial in primary care. ERJ Open Research, 3(4), 00115–2016–02016. https://doi.org/10.1183/23120541.00115-2016
- Wikipedia. (2016). Hautkrebs [Skin cancer]. https://de.wikipedia.org/wiki/Hautkrebs
- World Health Organization (WHO). (2019a). Protecting oneself from skin cancer: Is UV damage avoidable? https://www.who.int/news-room/q-a-detail/protecting-oneself-from-skin-cancer
- World Health Organization (WHO). (2019b). Ultraviolet (UV) radiation and skin cancer: Who is most at risk of getting skin cancer? https://www.who.int/news-room/q-a-detail/ultraviolet-(uv)-radiation-and-skin-cancer
- World Health Organization (WHO). (2019c). Sun protection. . https://www.who.int/news-room/q-a-detail/sun-protection
