Abstract
Objective
Psycho-oncological institutions offer specialized care for cancer patients. Little is known how this care might impact fatigue. This study aimed to identify fatigue trajectories during psychological care, examined factors distinguishing these trajectories and predicted fatigue severity after nine months of psychological care.
Design
Naturalistic, longitudinal study of 238 cancer patients receiving psycho-oncological care in the Netherlands. Data were collected before initiation of psychological care (T1) and three (T2) and nine months (T3) afterwards. Latent class growth analysis, repeated measure analyses (RMA) and linear regression analysis were performed.
Main Outcome Measures
Fatigue severity: Checklist Individual Strength.
Results
Three fatigue trajectories were identified: high- (30%), moderate- (62%) and low-level fatigue (8%). While statistically significant decreases in fatigue were found, this decrease was not clinically relevant. RMA showed main effects for time for fatigue trajectories on depression, anxiety, personal control and illness cognitions. Fatigue severity and physical symptoms at T1, but not demographic or clinical factors, were predictive of fatigue severity at T3.
Conclusions
Fatigue is very common during psycho-oncological care, and notably not clinically improving. As symptoms of fatigue, depression, anxiety and physical symptoms often cluster, supplementary fatigue treatment should be considered when it is decided to treat other symptoms first.
Introduction
Fatigue is the most frequently reported symptom in cancer patients, prevalent in 14–28% of cancer patients shortly after their diagnosis, and in up to 90% during treatment (Goedendorp et al., Citation2008; Prue et al., Citation2006). Longitudinal studies on fatigue in cancer survivors that were treated for various malignancies showed that about a quarter of the survivors suffered from persistent fatigue (lasting for at least six months). Notably, in subgroups of cancer survivors with high levels of fatigue, fatigue decreased minimally over time (Beesley et al., Citation2020; Goedendorp et al., Citation2013; Müller et al., Citation2017; Person et al., Citation2020). Even though these studies are not a representation of all types of cancer and treatments, fatigue has considerable impact on cancer patients’ daily activities and their quality of life (Donovan et al., Citation2013; Medysky et al., Citation2020; Schmidt et al., Citation2012), and therefore appropriate care is crucial.
Cancer patients suffering from fatigue often experience additional psychological symptoms (Prue et al., Citation2006; Stepanski et al., Citation2009). Numerous studies have found associations between fatigue and depressive and anxiety symptoms (Brown & Kroenke, Citation2009; Li et al., Citation2020). A reduction of these psychological symptoms and enhancement of psychological cognitions (e.g. the feeling of personal control and having a healthy perception of their illness) are central to an overall successful reduction in fatigue in cancer patients (Donovan & Jacobsen, Citation2007; Gielissen et al., Citation2006), and therefore psychological care often has a broad approach aiming to address multiple symptoms and cancer-related cognitions.
Addressing illness cognitions is key in psychological care for cancer patients. Previous studies have shown that how symptoms are perceived and how cancer is interpreted determine how patients cope with their health problems (Rozema et al., Citation2009). Important illness cognitions centre around accepting the disease, finding benefits and feeling less helpless (Evers et al., Citation2001). Several studies found associations between these illness cognitions and fatigue (Pertl et al., Citation2014; Westbrook et al., Citation2016; Schellekens et al., Citation2020), and more perceived control was also found to be predictive of lower levels of distress in cancer patients (Barez et al., Citation2009; Zhu et al., Citation2015). However, fatigue trajectories and relationships with illness cognitions and perceived control during psychological care, have not been investigated before.
In the Netherlands, psycho-oncological institutions offer psychological care for cancer patients and families, irrespective of age, cancer stage or prognosis. These institutions specialize in care for patients suffering from cancer-related anxiety disorders, depression, persistent severe fatigue or cancer-related trauma. Therapists help to organize questions, thoughts and emotions of patients individually or in groups (Psycho-Oncological Institutions [Instellingen PsychoSociale Oncologie], Citation2019). The present study focuses on patients treated in these institutions.
It is important to investigate trajectories of fatigue during psychological care in the Netherlands, because there seems to be a discrepancy in the prevalence and treatment of fatigue during psychological care. Many of the patients, in fact half of them (Zhu et al., Citation2017), have elevated levels of fatigue before the start of psychological care, although, in only 13% of the patients, therapists indicate that fatigue was a predominant symptom they dealt with during psycho-oncological care (Garssen & van der Lee, Citation2011). In the majority of cases (53%), therapists deal with anxiety and depression during psycho-oncological care. Because symptoms of depression, anxiety and fatigue often cluster, and because fatigue is one of the symptoms of depression in cancer patients (Integraal Kankercentrum Nederland, Citation2009), therapists could have reasoned that with treating anxiety and depression, symptoms of fatigue will automatically reduce too. However, there are indications that fatigue seems to be an independent problem for some cancer patients. Zhu et al. (Citation2017) demonstrated that during nine months of psychological care, fatigue improved in 22% of the subgroup of patients with depression, anxiety and fatigue at baseline, while additional fatigue was developed by 8% of the subgroup of patients with depression and anxiety at baseline. So, fatigue trajectories might not run parallel to trajectories of depression and anxiety during psychological care. Identifying fatigue trajectories during psychological care could facilitate tailoring and help to optimize future care for cancer patients.
As stated above, several studies showed that many cancer patients treated for various malignancies suffer from severe fatigue and that in subgroups of patients with high levels of fatigue it deceases minimally over time (Beesley et al., Citation2020; Goedendorp et al., Citation2013; Müller et al., Citation2017; Person et al., Citation2020). To tailor psychological care for cancer patients with fatigue it is not only important to identify various fatigue trajectories, but also what factors are related to these trajectories, and which factors predict fatigue during psychological care. Therefore, we had the following research aims: (1) identify fatigue trajectories in cancer patients during psychological care, (2a) examine which demographic and clinical factors distinguished these fatigue trajectories, (2b) examine if these fatigue trajectories determine the course of psychological factors; depressive and anxiety symptoms, illness cognitions and personal control, (3) examine which factors predicted fatigue severity after nine months of psychological care.
Materials and methods
Participants
This study is part of a larger longitudinal study investigating distress in cancer patients during psychological care (Zhu et al., Citation2017). Participants were cancer patients who sought psychological care at one of seven specialized psycho-oncology institutions in the Netherlands. Between September 2008 and March 2010, staff informed patients about the study at these psycho-oncology institutions. Data were collected as part of normal clinical routine of psychological care for cancer patients, and therefore the study did not fall under The Medical Research Involving Human Subjects Act.
Patients were eligible if they (1) were diagnosed with cancer, irrespective of stage and treatment of cancer, and seeking psychological care, (2) were older than 18 years and (3) were able to complete Dutch questionnaires. A total of 611 patients were approached, 524 patients agreed to participate and signed informed consent, of which 384 patients completed baseline questionnaires. Of these participants, 143 dropped out. Given reasons from patients to dropout were: no continuation after intake, too ill, or decided to quit the study. A flow diagram with detailed information can be found elsewhere (Zhu et al., Citation2017). Three participants were excluded because of missing fatigue data. Hence, the analysis was conducted with 238 participants. The dropouts differed significantly from the 238 participants on sex (more men), prognosis (less favourable) and cancer treatment (fewer surgeries received) at p < .05. Dropouts were not significantly different from participants in severity of depression, anxiety or fatigue at baseline (Zhu et al., Citation2017).
Design
The longitudinal naturalistic intervention study was composed of three assessments. The baseline assessment took place before psychological care (T1). After three months, the second assessment was conducted (T2), because effects of psychological care were expected after this period. The third assessment (T3) was conducted after nine months, because a group of the patients will receive psychological care for this long period.
Psychological care
Patients were offered appropriate psychological care based on their problems and needs, according to existing guidelines for treatment of depressive disorders, anxiety disorders and post-traumatic stress disorder. No guideline for treatment of severe cancer-related fatigue was available during this study. Patients may have received more than one type of care. At T2 and T3, patients were asked to indicate whether they had received individual, group or other therapy, and the number of sessions. Individual care could consist of individual sessions with a therapist, or psychiatrist, sessions with the partner or with family. Group care could focus on stress-reduction by means of meditation, relaxation and mindfulness, coping with (consequences of) cancer, increasing physical activity, or could be oncological rehabilitation. Other types of care were haptotherapy or creative therapy. Patients could combine types of care. Psychological care was categorized as follows: individual, group, individual and group (all with/without other therapy) and other therapy only.
Measures
Demographic and clinical characteristics (age, sex, cancer type and treatment, education level, perceived prognosis, years since diagnosis, presence of metastasis, recurrence, under medical treatment, co-morbid diseases, etc.) were assessed at baseline with a self-report questionnaire. At all three assessment points, participants were asked whether they used anti-depressants. Changes in disease history were asked at the follow-up assessments. Physical symptom severity was measured with a 10-item checklist (e.g. pain, shortness of breath, dizziness and nausea) using the Rotterdam Symptom Checklist (de Haes et al., Citation1990). None of these 10 symptoms related to somatic symptoms of depression. Cancer patients indicated on a scale from 1 (not at all) to 4 (very much) to what extent they experienced these symptoms.
Fatigue severity was assessed with the eight-item Checklist Individual Strength (CIS). The CIS measures fatigue severity and received validation among several different populations. An example item is: ‘I feel tired’. The sum score varies between 8 and 56 with a cut-off score of ≥35 indicating severe fatigue and a score between 27 and 35 indicating heightened fatigue, based on a sample of the Dutch population (Vercoulen et al., Citation1999; Vercoulen et al., Citation1994). Cronbach’s alphas for this study were between .91 and .92.
Depressive symptoms were assessed with the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, Citation1977). The sum score ranges from 0 to 46 with increasing scores indicating greater depression. An example item is: ‘I felt depressed’. For the 16-item CES-D, the reliability and validity were found to be good especially for people with cancer (Schroevers et al., Citation2000).
Anxiety symptoms were measured with the State-Trait Anxiety Inventory (STAI). For this study, the six-item version was used, which was found to have good reliability and validity (Marteau & Bekker, Citation1992). An example item is: ‘I feel nervous’. Higher scores ranging from 6 to 24 indicate higher anxiety.
Illness cognitions was measured with the Illness Cognition Questionnaire for chronic diseases. The questionnaire has three subscales: helplessness, acceptance and perceived benefits. An example item for helplessness is: ‘My illness frequently makes me feel helpless’, for acceptance is: ‘I have learned to live with my illness’ and for perceived benefits is: ‘I have learned to live with my illness’. Higher scores indicate greater helplessness, acceptance or perceived benefits with total scores ranging from 6 to 24 (Evers et al., Citation2001).
Personal control was assessed using the Mastery Scale with seven items (Pearlin & Schooler, Citation1978). An example item is: ‘I have little control over the things that happen to me’. Final scores ranged from 7 to 35 with higher scores indicated greater mastery.
Statistical methods
To identify classes of cancer patients with distinct fatigue trajectories during psychological care latent class growth analysis (LCGA) was performed in Latent Gold 2.X. LCGA is useful to find inherent differences in growth trajectories over time (Jung & Wickrama, Citation2008). For this study, time was treated as categorical variable, because dates of assessments were not registered for individual participants. It can also indicate intercepts and linear slopes for the individual trajectories (Nagin, Citation1999). To find the most representative model, we compared models with one to four classes. No power analysis was done beforehand. The Akaike Information Criterion (AIC), the Bayesian Information Criterion (BIC) and entropy will be compared between the four models to identify the best model. The relative fit of models is indicated by the BIC and the AIC with lower values indicating better fit. A model with better class separation indicates a higher entropy (Asparouhov & Muthén, Citation2014). A minimum class size of ≥5% can be considered as orientation to identify a class as valuable and clinically relevant (Henselmans et al., Citation2010). Despite considering statistical criteria, the conceptual meaning and face validity of the classes should be evaluated (Masyn, Citation2009; Muthén, Citation2003). Based on the final model, the class membership was exported to IBM SPSS Statistics 23 for further analysis. Cohen’s d was calculated to determine the size of the difference between T1 and T3 where a Cohen’s d ≤ .2 is considered a small effect, .5 a medium effect and ≥.8 a large effect (Cohen, Citation1998).
To examine which demographic and clinical factors distinguished these fatigue trajectories, we compared the fatigue classes on demographic and clinical factors at baseline. Therefore, we used Chi-square to compare fatigue classes for categorical factors, and additionally multinomial logistic regression analyses when there were more than two categories within a factor. We used ANOVA to compare fatigue classes on continuous factors.
Third, to examine courses of depression, anxiety, illness cognition and personal control for the fatigue trajectories separate GLMs (repeated measures analyses) were performed to investigate main effects for time and interaction effects between time and fatigue classes.
Fourth, to examine which factors predicted fatigue severity after nine months of psychological care, linear regression analysis was performed with fatigue severity at T3 as dependent variable and significant demographic, clinical psychological factors and fatigue at T1 as predictors.
Results
Sample characteristics
From the total of 238 participants, the majority were women (80%) with breast cancer (46%), the average age was 52 years old, and the majority (59%) received oncological treatment at baseline. At T2, 14 participants indicated changes in their disease. Five of them reported disease progression, four reported to be disease free and five reported unclear changes. At T2, 41 participants reported changes in their cancer treatment. Seventeen reported that they finished cancer treatment, nine reported a change in the type of treatment, seven reported they had surgery, six reported they started a new treatment and two reported that they stopped treatment. At T3, 25 participants indicated changes in their disease. Thirteen of them reported disease progression, eight reported to be disease free, one reported an improvement, two reported disease recurrence and one reported unclear changes. At T3, 58 participants reported changes in their cancer treatment. Thirty reported that they finished treatment, four reported a change in the type of treatment, six reported they had surgery, one reported bone marrow transplantation, 14 reported they started a new treatment and three reported that they stopped treatment.
The majority (58%) of participants indicated they followed only individual sessions with a therapist. Participants who followed psychological care in groups most frequently followed sessions that focussed on stress-reduction or coping with (consequences) of cancer. At T2, 14 participants reported having received zero sessions, however six of these participants reported receiving one (n = 1) or more (4–18) sessions at T3. At T2, four participants reported having received one session, of which one participant reported to have received more (eight) sessions at T3. Demographic and clinical characteristics are shown in .
Table 1. Demographic and clinical characteristics of the sample, and the high fatigue group.
Identification of fatigue trajectories in cancer patient during psychological care
According to the BIC, the AIC and the entropy level the four-class model would be considered as the best fit (see ). However, when considering the class size of the four-class model one class only contains 3% of the total sample, which is below the clinically relevant size of 5%. Since the entropy level of the three-class model is nearly as high as for the four-class model, indicating adequate class separation, the three-class model was chosen. The three classes can be considered as the following clinically meaningful classes: high fatigue (n = 72, 30.3%), moderate fatigue (n = 146, 61.3%) and low fatigue (n = 20, 8.4%).
Table 2. Latent class growth modelling selection criteria.
The high fatigue and moderate fatigue classes showed significant decreases in fatigue from T1 to T3, with 0.38 (small to medium) and 0.58 (medium) effect sizes, where the high fatigue class exhibited the smallest decrease. Despite these decreases, the high fatigue class was above the cut-off of ≥35 for severe fatigue, and the moderate fatigue class was above the cut-off of 27 for heightened fatigue at T3. The effect size of the decrease in the low-fatigue class was 0.46 (medium), but not significant over time. The courses of the three fatigue trajectories and effect sizes are shown .
Table 3. Courses of the three fatigue trajectories during psychological care.
Which demographic and clinical factors distinguished fatigue trajectories during psychological care?
Since the entropy level was found to be high, class membership was considered as distinct variable. On most demographic and clinical factors, such as type of cancer, prognosis or the presence of comorbidities (see ), no differences were found between the three fatigue classes. However, sex (Chi-square = 7.2, p = .027), type of oncological treatment (Chi-square = 31.5, p = .005), anti-depressant use at T1 (Chi-square = 4.04, p = .044) and type of psychological care between T2 and T3 (Chi-square = 17.2, p = .029) was significantly related to fatigue class. Men and anti-depressant users were more likely to be in the high fatigue class. Multinomial logistic regression analyses showed that compared to the moderate and low-fatigue class, people in the high fatigue class more often underwent a combination of cancer treatments; either radiotherapy with surgery (B = −2.40, p = .028; B = −4.09, p = .008) or radiotherapy with chemotherapy (B = −3.09, p = .011, B = −3.18, p = .043). People in the high fatigue class also underwent a combination of surgery, radiotherapy and chemotherapy more often, compared to the low-fatigue class (B = −2.83, p = .031). People who received group psychological care between T2 and T3 that focussed mostly on stress-reduction or coping with (consequences) of cancer, were more likely to belong to the low-fatigue class B = 19.6, p < .001.
Do fatigue trajectories determine the course of psychological factors during psychological care?
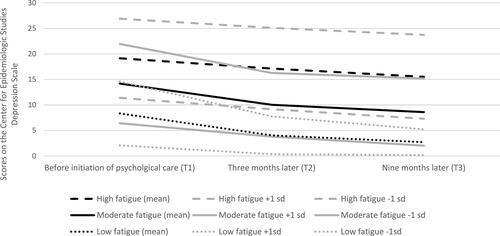
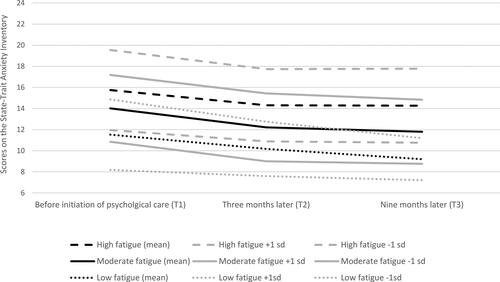
Repeated measures analysis showed significant changes over time of depressive symptoms for the three fatigue trajectories [main effect: Ftime(1.89, 1085.58) = 21.24, p < .001]. These changes did not show differential courses for the distinct fatigue trajectories [interaction effect: Ftime x group(3.77, 184.21) = 1.80, p = .13] (see ). Repeated measures analysis also showed significant changes over time of anxiety symptoms for the three fatigue trajectories [Ftime(1.88, 167.51) = 15.59, p < .001]. These changes also did not show differential courses for the distinct fatigue trajectories [Ftime x group(3.76, 184.21) = 1.20, p = .31] (see ).
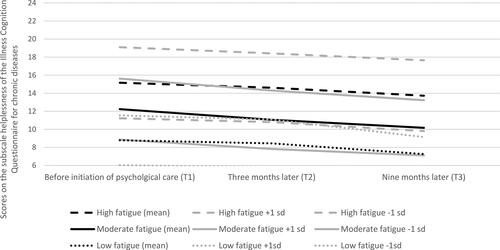
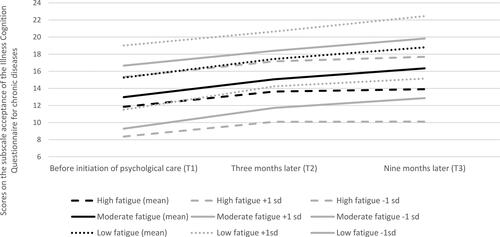
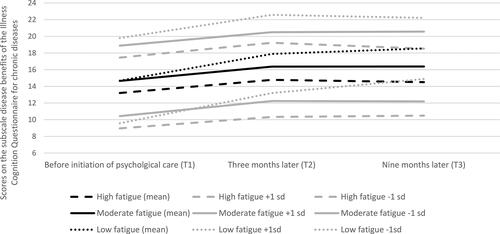
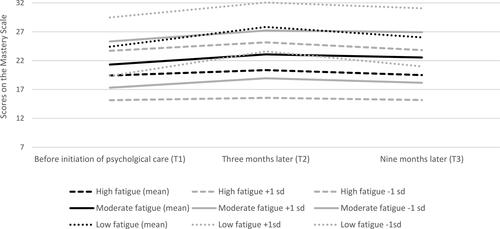
The repeated measure analyses showed the same results for illness cognitions and personal control (see ). These analyses showed significant changes over time for helplessness [F(1.94, 163.04) = 15.77, p < .001], acceptance [F(1.94, 457.27) = 44.28, p < .001], perceived benefits [F(1.97, 316.58) = 27.20, p < .001] and personal control [F(1.99, 154.77) = 9.73, p < .001]. These changes did not show differential courses for the distinct fatigue trajectories: helplessness [Ftime x group(3.87, 21.47) = 1.04, p = .39], acceptance [Ftime x group(3.88, 40.36) = 1.95, p = .10], perceived benefit [Ftime x group(3.93, 44.97) = 1.93, p = .11] and personal control [Ftime x group(3.98, 43.06) = 1.35, p = .25]. So overall, depressive symptoms, anxiety symptoms, illness cognitions and personal control were related the course of fatigue (main effects), but we found no differences in the courses of these psychological factors between the three fatigue trajectories (no interaction effects).
Predictors of fatigue severity after nine months of psychological care
Linear regression analysis showed that fatigue severity at T3 was predicted by fatigue severity at T1 and physical symptoms, but not by other demographic or any other clinical factor (see ).
Table 4. Predictors of fatigue severity in cancer patients after nine months of psychological care.
Discussion
In this study, we investigated fatigue trajectories in cancer patients during psychological care in which three distinct trajectories were identified: high-level fatigue (30%), moderate-level fatigue (62%) and low-level fatigue (8%). Fatigue levels in the high and moderate-level fatigue classes decreased significantly, but modestly over time. Predictors of fatigue severity after nine months of psychological care were baseline severity of fatigue and other physical symptoms, such as pain, shortness of breath, nausea and dizziness.
Looking more closely at the course of fatigue, we noticed several differences between the three trajectories. First, judged by the size of the effect the decrease in fatigue was smaller in the high fatigue class during psychological care, although we did not test the differences. The finding that the decrease in fatigue was smaller in the high fatigue class during psychological care seems more in line with longitudinal studies that investigated fatigue trajectories in cancer patients that do not receive psychological care (Beesley et al., 2020; Goedendorp et al., Citation2013; Müller et al., Citation2017; Person et al., Citation2020). Second, the decreases in the moderate and high fatigue classes do not seem to be clinically relevant. Not only were decreases small to medium in size, we also observed that the mean score in the high fatigue class, remained far above the cut-off for severe fatigue based on a sample of the Dutch population, and the mean score in the moderate fatigue class, remained above the cut-off for heightened fatigue (Vercoulen et al., Citation1999, Citation1994; Worm-Smeitink et al., Citation2017). A previous study that investigated the course of symptoms among the whole sample already indicated that the number of patients with clinical levels of fatigue was rather high after nine months of psychological care (Garssen et al., Citation2016).
Our second aim was to investigate which demographic, clinical and psychological factors distinguished these three fatigue trajectories, and we only found three significant factors. We found that men and patients who had received radiotherapy together with surgery, chemotherapy or all three, were more fatigued than people with other types of treatment. One could reason that there might be differences between cancer patients’ prognosis on fatigue trajectories, as was found in a study following a more homogeneous group of cancer patients consisting of women who received chemotherapy for ovarian cancer (Beesley et al., Citation2020), although our results did not confirm this. Unfortunately, details on cancer staging were not collected. However, our sample size is most likely too small and the diversity in cancer types and treatments too large, to confirm possible effects of these clinical differences on our results. Our results indicate that other physical symptoms were stronger predictors of fatigue than sex and cancer treatment, or other assessed clinical factors. A review of studies confirms that much of the variability in fatigue in cancer patients is not explained by disease-related or treatment-related characteristics, but that host factors seem to be important in the development and persistence of this symptom (Bower, Citation2014).
Based on previous studies, we knew that fatigue is partly associated with anxiety and depressive symptoms, and that the course of fatigue does not always follow the course of anxiety and depressive symptoms during psychological care (Brown & Kroenke, Citation2009; Zhu et al., Citation2017). Therefore, we identified trajectories of fatigue in the current study and investigated if the courses of anxiety and depressive symptoms would be different for the three fatigue classes. If one of the fatigue trajectories would have been more strongly related to anxiety or depressive symptoms, the psychological care for patients could be tailored accordingly. However, repeated measures analyses only showed significant main effects, indicating that anxiety or depressive symptoms did decrease, but not more strongly for any of the three fatigue classes. Our finding is consistent with a study that investigated the directionality of the relationship between depressive symptoms and fatigue, which demonstrated that neither symptom preceded and predicted the other. Therefore, it was suggested that depression-specific treatments might not be sufficient to treat cancer-related fatigue (Brown et al., Citation2013).
Changing illness cognitions and gaining personal control are important aspects of psychological care, and therefore we investigated the course of helplessness, acceptance, perceived benefits and personal control for the three fatigue trajectories. To our knowledge no other studies investigated the course of these psychological factors in relations to fatigue trajectories in cancer patients during psychological care, however, several studies did demonstrate relationships between illness cognition and fatigue in cancer patients (Andrykowski et al., Citation2010; Peters et al., Citation2016). Our results only showed main effects between illness cognitions, personal control and the three fatigue trajectories, and no interaction effects. This indicates that fatigue severity was related with personal control and illness cognitions, but we did not find that the courses of these factors were different for the three fatigue trajectories. This implies that these psychological factors need to be addressed during psychological care, but there seems no need for different approaches in care for these three fatigue groups.
Our results showed that the severity of fatigue and physical symptoms at baseline were the strongest and significant predictors of fatigue severity after nine months of psychological care. There was a trending significance of the group being treated with a combination of surgery, radiotherapy and chemotherapy for cancer compared to other cancer treatments, single or in combinations, predicting fatigue severity at T3. To our knowledge these relationships have not been previously demonstrated in cancer patients receiving psychological care, but are in line with research showing that initial fatigue and pain are predictive of long-term fatigue (Goedendorp et al., Citation2013; Pertl et al., Citation2014; Reinertsen et al., Citation2010). The findings that fatigue at the start of psychological care is the strongest predictor of fatigue nine months later points out that it might be helpful for patients, if therapists explicitly inquire about the severity and impact of these symptoms, and discusses treatment options with patients before starting psychological care.
This study has several limitations that need to be considered when evaluating the findings. First, since cancer-related fatigue can be persistent for several years, a follow-up of nine months may not be sufficient to understand how fatigue develops over time and to detect substantial changes. Second, the study followed cancer patients who sought psychological care and did not include a control group of cancer patients who did not receive psychological care. Thus, it is not deductible whether changes in fatigue or psychological functioning are due to natural changes, changes in cancer staging, cancer treatment or a consequence of psychological care. Patients received psychological care based on their problems and needs according to guidelines, and it seems that patients in the low-fatigue group, compared to the other fatigue groups, received more often group psychological care between the follow-up assessments, which was focussed mostly on stress-reduction or coping with (consequences) of cancer. However, it should be noted that unfortunately, the duration and exact content of the psychological care per individual was not registered or verified, the time between T1 and start of psychological care was not registered, and a large part of the participants did not complete the items concerning psychological care. Therefore, no conclusion about the effectiveness or impact of psychological care on fatigue or outcomes can be drawn.
This cohort consisted of cancer patients seeking help at psycho-oncological institutions, and had for a large part an above average education, were relatively young compared to the general cancer population, and were predominantly women with breast cancer. Unfortunately, no data on race or ethnicity were collected, although from clinical practice we know that the majority of cancer patients seeking psycho-oncological care are from native Dutch origin. Even with this in mind, it is important not to generalize the results of this study to other samples or settings.
Due to the small sample size, identifying distinct fatigue trajectories was limited. We could only identify three clinically relevant fatigue trajectories, with only 20 participants in the low-fatigue group. This small number could explain why no significant decrease in fatigue was found over nine months of psychological care in the low-fatigue group, while in the high fatigue group the decrease was smaller but significant.
Unfortunately, only a limited number of factors were assessed that could have explained the persistence of fatigue in cancer patients during psychological care. From other non-intervention longitudinal studies we know that obesity, physical inactivity, sleeping problems, negative social interactions, fatigue catastrophizing, focussing on physical symptoms and non-acceptance of cancer are predictive of severe fatigue (Abrahams et al., Citation2018; Andrykowski et al., Citation2010; Goedendorp et al., Citation2013; Peters et al., Citation2016; Reinertsen et al., Citation2010).
Clinical implications
This study showed that fatigue is very common in cancer patients receiving psychological care. Three fatigue trajectories were identified in which 30% had high levels of fatigue and 62% had elevated levels of fatigue. Only 8% had levels of fatigue comparable with the general Dutch population. Fatigue levels decreased significantly during nine months of psychological care, but only modestly. In other words, patients with severe or moderate fatigue remained severely or moderately fatigued. Notably the improvement was the smallest in the group with severe fatigue.
This study showed that the three fatigue trajectories were related with anxiety and depressive symptoms, personal control and illness cognitions, but we did not find that the courses of these psychological factors were different for the three fatigue trajectories. This implies that these psychological factors need to be addressed during psychological care, but that no specific focus is needed for specific fatigue groups.
Severity of fatigue and other physical symptoms at the start of psychological care were the strongest predictors of fatigue severity nine months later. Special attention might be needed for treatment of these symptoms such as pain, shortness of breath, nausea and dizziness in fatigued cancer patients, for which collaboration between physicians and psychologists seems advisable.
As stated in the introduction about half of the cancer patients have elevated levels of fatigue before the start of psycho-oncological care, while according to therapists, fatigue is only a predominant symptom they dealt with among 13% of these patients (Garssen & van der Lee, Citation2011). So, seems to be is a discrepancy between the numbers of patients reporting heightened fatigue, and the number of patients receiving care for fatigue. Although there are currently national and international guidelines for fatigue (Integraal Kankercentrum Nederland, Citation2019; National Comprehensive Cancer Network, Citation2019), depression and anxiety in cancer patients (Integraal Kankercentrum Nederland, Citation2009), as well as (e)interventions, such as (mindfulness-based) cognitive behaviour therapy for persistent fatigue (Abrahams et al., Citation2017; Bruggeman-Everts et al., Citation2017; Gielissen et al., Citation2006), these interventions were not widely available at the time of this study. Moreover, advice on how to handle when symptoms of depression, anxiety and fatigue are all present is still lacking. One could reason that because patients were offered psychological care based on their problems and needs, symptoms of depression and anxiety were treated first. This study showed that with this approach fatigue only decreased moderately. For future cases, when it is decided that depression and anxiety is treated first, fatigue should not be forgotten. It seems advisable for therapists to diagnose fatigue again after treating depression and anxiety, to see if supplementary treatment is required for fatigue.
Acknowledgements
We would like to thank all the Dutch IPSO institutions for their participation.
Disclosure statement
No potential conflict of interest was reported by the author.
Data availability statement
The data that support the findings of this study are available from the corresponding author MG, upon reasonable request.
References
- Abrahams, H. J. G., Gielissen, M. F. M., Donders, R. R. T., Goedendorp, M. M., van der Wouw, A. J., Verhagen, C. A. H. H. V. M., & Knoop, H. (2017). The efficacy of internet-based cognitive behavioral therapy for severely fatigued survivors of breast cancer compared with care as usual: A randomized controlled trial. Cancer, 123(19), 3825–3834. https://doi.org/https://doi.org/10.1002/cncr.30815
- Abrahams, H. J. G., Gielissen, M. F. M., Verhagen, C. A. H. H. V. M., & Knoop, H. (2018). The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: A systematic review. Clinical Psychology Review, 63, 1–11. https://doi.org/https://doi.org/10.1016/j.cpr.2018.05.004
- Andrykowski, M. A., Donovan, K. A., Laronga, C., & Jacobsen, P. B. (2010). Prevalence, predictors, and characteristics of off-treatment fatigue in breast cancer survivors. Cancer, 116(24), 5740–5748. https://doi.org/https://doi.org/10.1002/cncr.25294
- Asparouhov, T., & Muthén, B. (2014). Auxiliary variables in mixture modeling: Three-step approaches using M plus. Structural Equation Modeling – A Multidisciplinary Journal, 0, 1–13. https://doi.org/https://doi.org/10.1080/10705511.2014.915181
- Barez, M., Blasco, T., Fernandez-Castro, J., & Viladrich, C. (2009). Perceived control and psychological distress in women with breast cancer: A longitudinal study. Journal of Behavioral Medicine, 32(2), 187–196. https://doi.org/https://doi.org/10.1007/s10865-008-9180-5
- Beesley, W., Nagle, D., Obermair, W., & OPAL Study group. (2020). When will I feel normal again? Trajectories and predictors of persistent symptoms and poor wellbeing after primary chemotherapy for ovarian cancer. Gynecologic Oncology, 159, 179–186. https://doi.org/https://doi.org/10.1016/j.ygyno.2020.07.029
- Bower, J. E. (2014). Cancer-related fatigue-mechanisms, risk factors, and treatments. Nature Reviews Clinical Oncology, 11(10), 597–609. https://doi.org/https://doi.org/10.1038/nrclinonc.2014.127
- Brown, L. F., & Kroenke, K. (2009). Cancer-related fatigue and its associations with depression and anxiety: A systematic review. Psychosomatics, 50(5), 440–447. https://doi.org/https://doi.org/10.1176/appi.psy.50.5.440
- Brown, L. F., Rand, K. L., Bigatti, S. M., Stewart, J. C., Theobald, D. E., Wu, J., & Kroenke, K. (2013). Longitudinal relationships between fatigue and depression in cancer patients with depression and/or pain. Health Psychology, 32(12), 1199–1208. https://doi.org/https://doi.org/10.1037/a0029773
- Bruggeman-Everts, F. Z., Wolvers, M. D. J., van de Schoot, R., Vollenbroek-Hutten, M. M. R., & Van der Lee, M. L. (2017). Effectiveness of two web-based interventions for chronic cancer-related fatigue compared to an active control condition: Results of the "Fitter na kanker”. Randomized Controlled Trial. Journal of.Medical.Internet Reseach, 19(10), e336. https://doi.org/https://doi.org/10.2196/jmir.7180
- Cohen, J. (1998). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Earlbaum Associates.
- de Haes, J. C., van Knippenberg, F. C., & Neijt, J. P. (1990). Measuring psychological and physical distress in cancer patients: Structure and application of the Rotterdam symptom checklist. British Journal of Cancer, 62(6), 1034–1038.
- Donovan, K. A., & Jacobsen, P. B. (2007). Fatigue, depression, and insomnia: Evidence for a symptom cluster in cancer. Seminars in Oncology Nursing, 23(2), 127–135. https://doi.org/https://doi.org/10.1016/j.soncn.2007.01.004
- Donovan, K. A., McGinty, H. L., & Jacobsen, P. B. (2013). A systematic review of research using the diagnostic criteria for cancer-related fatigue. Psycho-Oncology, 22(4), 737–744. https://doi.org/https://doi.org/10.1002/pon.3085
- Evers, A. W., Kraaimaat, F. W., van Lankveld, W., Jongen, P. J., Jacobs, J. W., & Bijlsma, J. W. (2001). Beyond unfavorable thinking: The illness cognition questionnaire for chronic diseases. Journal of Consulting and Clinical Psychology, 69(6), 1026–1036.
- Garssen, B., & van der Lee, M. (2011). Problems addressed during psycho-oncological therapy: A pilot study. Journal of Psychosocial Oncology, 29(6), 657–663. https://doi.org/https://doi.org/10.1080/07347332.2011.615379
- Garssen, B., Van der Lee, M., Van der Poll, A., Ranchor, A. V., Sanderman, R., & Schroevers, M. J. (2016). Characteristics of patients in routine psycho-oncological care, and changes in outcome variables during and after their treatment. Psychology & Health, 31(10), 1237–1254. https://doi.org/https://doi.org/10.1080/08870446.2016.1204447
- Gielissen, M. F., Verhagen, S., Witjes, F., & Bleijenberg, G. (2006). Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: A randomized controlled trial. Journal of Clinical Oncology, 24(30), 4882–4887. https://doi.org/https://doi.org/10.1200/JCO.2006.06.8270
- Goedendorp, M. M., Gielissen, M. F., Verhagen, C. A., & Bleijenberg, G. (2013). Development of fatigue in cancer survivors: A prospective follow-up study from diagnosis into the year after treatment. Journal of Pain and Symptom Management, 45(2), 213–222. https://doi.org/https://doi.org/10.1016/j.jpainsymman.2012.02.009
- Goedendorp, M. M., Gielissen, M. F., Verhagen, C. A., Peters, M. E., & Bleijenberg, G. (2008). Severe fatigue and related factors in cancer patients before the initiation of treatment. British Journal of Cancer, 99(9), 1408–1414. https://doi.org/https://doi.org/10.1038/sj.bjc.6604739
- Henselmans, I., Helgeson, V. S., Seltman, H., de Vries, J., Sanderman, R., & Ranchor, A. V. (2010). Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychology: Official Journal of the Division of Health Psychology. American Psychological Association, 29(2), 160–168. https://doi.org/https://doi.org/10.1037/a0017806
- Integraal Kankercentrum Nederland. (2009). Oncoline: Depression and anxiety [depressie en angst]. https://www.oncoline.nl/index.php?pagina=/richtlijn/item/pagina.php&id=29988&richtlijn_id=658
- Integraal Kankercentrum Nederland. (2019). Oncoline: Fatigue [vermoeidheid]. https://www.oncoline.nl/vermoeidheid
- Jung, T., & Wickrama, K. A. (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317.
- Li, H., Marsland, A. L., Conley, Y. P., Sereika, S. M., & Bender, C. M. (2020). Genes involved in the HPA axis and the symptom cluster of fatigue, depressive symptoms, and anxiety in women with breast cancer during 18 months of adjuvant therapy. Biological Research for Nursing, 22(2), 277–286.
- Marteau, T. M., & Bekker, H. (1992). The development of a six-item short-form of the state scale of the spielberger state-trait anxiety inventory (STAI). The British Journal of Clinical Psychology, 31(3), 301–306.
- Masyn, K. E. (2009). Discrete-time survival factor mixture analysis for low-frequency recurrent event histories. Research in Human Development, 6(2–3), 165–194.
- Medysky, M. E., Dieckmann, N. F., Winters-Stone, K. M., Sullivan, D. R., & Lyons, K. S. (2020). Trajectories of self-reported physical functioning and symptoms in lung cancer survivors. Cancer Nursing. https://doi.org/https://doi.org/10.1097/NCC.0000000000000765
- Müller, F., Tuinman, M. A., Janse, M., Almansa, J., Sprangers, M. A. G., Smink, A., … Hagedoorn, M. (2017). Clinically distinct trajectories of fatigue and their longitudinal relationship with the disturbance of personal goals following a cancer diagnosis. British Journal of Health Psychology, 22(3), 627–643. https://doi.org/https://doi.org/10.1111/bjhp.12253
- Muthén, B. (2003). Statistical and substantive checking in growth mixture modeling. Psychological Methods, 8(3), 369–377.
- Nagin, D. S. (1999). Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods, 4(2), 139–157.
- National Comprehensive Cancer Network. (2019). Cancer-related fatigue. https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf
- Pearlin, L. I., & Schooler, C. (1978). The structure of coping. Journal of Health and Social Behavior, 19(1), 2–21.
- Person, H., Guillemin, F., Conroy, T., Velten, M., & Rotonda, C. (2020). Factors of the evolution of fatigue dimensions in patients with breast cancer during the 2 years after surgery. International Journal of Cancer, 146(7), 1827–1835. https://doi.org/https://doi.org/10.1002/ijc.32527
- Pertl, M. M., Hevey, D., Collier, S., Lambe, K., & O’Dwyer, A. M. (2014). Predictors of fatigue in cancer patients before and after chemotherapy. Journal of Health Psychology, 19(6), 699–710. https://doi.org/https://doi.org/10.1177/1359105313477675
- Peters, M. E. W. J., Goedendorp, M. M., Verhagen, C. A. H. H. V. M., Bleijenberg, G., & van der Graaf, W. T. A. (2016). Fatigue and its associated psychosocial factors in cancer patients on active palliative treatment measured over time. Supportive Care in Cancer, 24(3), 1349–1355.
- Prue, G., Rankin, J., Allen, J., Gracey, J., & Cramp, F. (2006). Cancer-related fatigue: A critical appraisal. European Journal of Cancer, 42(7), 846–863. https://doi.org/10.1016/j.ejca.2005.11.026
- Psycho-Oncological Institutions. (2019). [Instellingen PsychoSociale Oncologie]. https://www.ipso.nl/psycho-oncologische-zorg/psycho-oncologische-centra
- Radloff, L. S. (1977). The CES-D scale: A self report depression scale for research in the general. Applied Psychological Measurement, 1(3), 385–401.
- Reinertsen, K. V., Cvancarova, M., Loge, J. H., Edvardsen, H., Wist, E., & Fossa, S. D. (2010). Predictors and course of chronic fatigue in long-term breast cancer survivors. Journal of Cancer Survivorship: Research and Practice, 4(4), 405–414. https://doi.org/https://doi.org/10.1007/s11764-010-0145-7
- Rozema, H., Vollink, T., & Lechner, L. (2009). The role of illness representations in coping and health of patients treated for breast cancer. Psycho-Oncology, 18(8), 849–857. https://doi.org/https://doi.org/10.1002/pon.1488
- Schellekens, M. P. J., Wolvers, M. D. J., Schroevers, M. J., Bootsma, T. I., Cramer, A. O. J., & van der Lee, M. L. (2020). Exploring the interconnectedness of fatigue, depression, anxiety and potential risk and protective factors in cancer patients: a network approach. Journal of Behavioral Medicine, 43(4), 553–563.
- Schmidt, M. E., Chang-Claude, J., Vrieling, A., Heinz, J., Flesch-Janys, D., & Steindorf, K. (2012). Fatigue and quality of life in breast cancer survivors: Temporal courses and long-term pattern. Journal of Cancer Survivorship: Research and Practice, 6(1), 11–19. https://doi.org/https://doi.org/10.1007/s11764-011-0197-3
- Schroevers, M. J., Sanderman, R., van Sonderen, E., & Ranchor, A. V. (2000). The evaluation of the center for epidemiologic studies depression (CES-D) scale: Depressed and positive affect in cancer patients and healthy reference subjects. Quality of Life Research, 9(9), 1015–1029.
- Stepanski, E. J., Walker, M. S., Schwartzberg, L. S., Blakely, L. J., Ong, J. C., & Houts, A. C. (2009). The relation of trouble sleeping, depressed mood, pain, and fatigue in patients with cancer. Journal of Clinical Sleep Medicine, 5(2), 132–136.
- Vercoulen, J. H. M. M., Alberts, M., & Bleijenberg, G. (1999). De checklist individual strength (CIS). Gedragstherapie, 32, 131–136.
- Vercoulen, J. H., Swanink, C. M., Fennis, J. F., Galama, J. M., van der Meer, J. W., & Bleijenberg, G. (1994). Dimensional assessment of chronic fatigue syndrome. Journal of Psychosomatic Research, 38(5), 383–392.
- Westbrook, T. D., Maddocks, K., & Andersen, B. L. (2016). The relation of illness perceptions to stress, depression, and fatigue in patients with chronic lymphocytic leukaemia. Psychology & Health, 31(7), 891–902. https://doi.org/https://doi.org/10.1080/08870446.2016.1158259
- Worm-Smeitink, M., Gielissen, M., Bloot, L., van Laarhoven, H. W. M., van Engelen, B. G. M., van Riel, P., Bleijenberg, G., Nikolaus, S., & Knoop, H. (2017). The assessment of fatigue: Psychometric qualities and norms for the Checklist individual strength. Journal of Psychosomatic Research, 98, 40–46.
- Zhu, L., Ranchor, A. V., van der Lee, M., Garssen, B., Almansa, J., Sanderman, R., & Schroevers, M. J. (2017). Co-morbidity of depression, anxiety and fatigue in cancer patients receiving psychological care. Psycho-Oncology, 26(4), 444–451. https://doi.org/https://doi.org/10.1002/pon.4153
- Zhu, L., Schroevers, M. J., van der Lee, M., Garssen, B., Stewart, R. E., Sanderman, R., & Ranchor, A. V. (2015). Trajectories of personal control in cancer patients receiving psychological care. Psycho-Oncology, 24(5), 556–563. https://doi.org/https://doi.org/10.1002/pon.3688