Abstract
Objective
Grounded Theory has previously been used to explore breastfeeding practices amongst average birthweight infants and these working hypotheses can be ‘tested’ in new contexts. A pre-existing Grounded Theory was applied to the context of women who gave birth to larger birthweight infants (≥4,000 g) to understand whether perceptions and practices of infant feeding were distinct.
Design
A nested qualitative study analysed data from N = 10 women with a larger birthweight infant (≥4,000 g). Face-to-face, semi-structured interviews were audio-recorded and transcribed verbatim. Grounded Theory methodology was used to analyse data.
Results
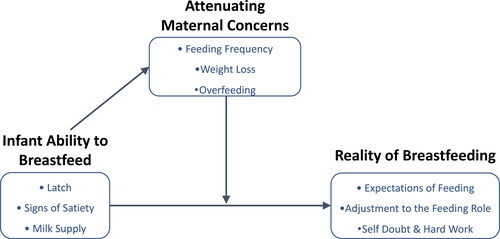
A pre-existing Grounded Theory of breastfeeding experiences derived from women with average birthweight infants did not hold true among women with larger birthweight infants. An alternative Grounded Theory was therefore proposed comprised of three discrete themes: Infant Ability to Breastfeed; Attenuating Maternal Concerns; and Reality of Breastfeeding.
Conclusions
Larger infant birthweight is potentially a protective factor against breastfeeding latch and lactation difficulties. It is associated with alleviating maternal concerns, helping to reduce disparities between expectations of breastfeeding and reality, but does not alleviate the demands breastfeeding places on women. Healthcare professionals help to attenuate women’s concerns, however the support needs for women with larger birthweight infants may not differ from existing care recommendations.
Introduction
As a global public health priority, women are recommended to exclusively breastfeed their infants for the first six months of life and extend breastfeeding up to two years (World Health Organization (WHO), Citation2013). Despite evidence-based guidelines for breastfeeding support (World Health Organization (WHO), United Nations Children’s Fund (UNICEF), 2018), prevalence rates worldwide remain low and breastfeeding rates rapidly decline across the postpartum period (Victora et al., Citation2016). In the UK, breastfeeding rates are amongst the lowest in the world with only 23% of women exclusively breastfeeding at six-to-eight weeks postpartum, declining to less than 1% at six months (McAndrew et al., Citation2012). Barriers and facilitators to breastfeeding intention, initiation, and continuation are well documented among populations of healthy women who give birth to healthy, term infants (Dennis, Citation2002; McFadden et al., Citation2017). However, there is a paucity of evidence specifically designed to investigate breastfeeding practices among women who give birth to healthy, larger birthweight infants.
The term macrosomic defines infants with a birthweight greater than 4,000 g or 4,500 g (weight limits across definitions vary), whereas the term large-for-gestational-age (LGA) describes infants with birthweights greater than the 90th or 95th centile (Koyanagi et al., Citation2013; National Institute for Health and Care Excellence (NICE), Citation2019a). Centile definitions control for infant sex and gestational age, can be country-specific or tailored to individuals (Koyanagi et al., Citation2013; Royal College of Paediatrics and Child Health (RCPCH), Citation2013). A lack of standardized definition of larger infant birthweight contributes to the complexity of the evidence currently available (National Institute for Health and Care Excellence (NICE), Citation2019a) for the influence of larger infant birthweight on infant feeding practices.
Cross-sectional research from Indonesia found breastfeeding initiation rates (within 24 hours of birth) were significantly higher among macrosomic infants (100%) than average (94.9%) birthweight infants (Ayukarningsih & Dwinanda, Citation2015). In a USA cohort of women giving birth to macrosomic infants, breastfeeding initiation rates varied between 53% and 75% depending on maternal BMI (Cordero et al., Citation2015). Longitudinal evidence from the USA, Norway, and China suggested larger birthweight infants received breastmilk exclusively for both longer (Chiavaroli et al., Citation2016; Leonard & Rasmussen, Citation2011) and shorter durations (Lande et al., Citation2005; Yu et al., Citation2008) than average birthweight infants. Existing evidence also found larger birthweight infants were significantly more likely to be introduced to solid foods before six months of age compared to average birthweight infants (Lande et al., Citation2005; Yu et al., Citation2008). Evidence to date is limited and not yet explored women’s experiences of feeding larger birthweight infants.
The World Health Organization (WHO) (Citation2018) has identified tailored breastfeeding counselling as a priority for research, as breastfeeding support strategies may be more effective when tailored to women and their experiences (Lumbiganon et al., Citation2016; McAndrew et al., Citation2012). Understanding whether women who give birth to larger birthweight infants experience unique barriers to breastfeeding is crucial to inform how care and support may be (re-)developed to improve breastfeeding outcomes in a group where the benefits of breastfeeding may be particularly valuable. For example, evidence suggests a larger infant birthweight is associated with an increased lifetime risk of obesity, diabetes, and cardiovascular disease (Poston, Citation2012). Breastfeeding has been found to attenuate the risk of such morbidities (Horta & Victora, Citation2013; Victora et al., Citation2016), providing an early life intervention to support the optimal growth and health of infants across the lifespan.
Breastfeeding is a unique health behaviour which relies on combined physical and psychological abilities of mother and infant, and often requires external support from healthcare professionals and women’s social community. Breastfeeding behaviour is of interest to multidisciplinary healthcare teams where physiological and clinical factors may be priorities in efforts to support breastfeeding. However, understanding breastfeeding through women’s own perspectives and experiences remains important in ensuring they are empowered and supported socially and psychologically to breastfeed their infants for as long as they desire. In the absence of existing qualitative evidence aimed at understanding women’s experiences of feeding larger birthweight infants, Grounded Theory provides a suitable methodology to contribute new theory to the limited evidence-base (Glaser & Strauss, Citation1967; Holton & Walsh, Citation2016).
Research using Grounded Theory has explored women’s perceptions and practices of infant feeding behaviours in the early postpartum period and found women make personal and practical provisions for breastfeeding (Oosterhoff et al., Citation2014). Further Grounded Theory research has identified that challenges in the postnatal period impact antenatal intentions and present competing goals for breastfeeding women (Sheehan et al., Citation2013). A nested qualitative study found women predominantly experienced breastfeeding latch difficulties and insufficient milk supply, which continue to create barriers to breastfeeding (Teich et al., Citation2014). Recent research has elaborated on this evidence by specifically exploring breastfeeding experiences among healthy women with healthy, average birthweight infants (Davie et al., Citation2021). The theory outlined barriers to positive breastfeeding experiences. Women were found to perceive infant behaviours as signs of ‘good’ or ‘problematic’ feeding, and a painful breastfeeding latch led woman to experience breastfeeding negatively with pronounced physical and psychological distress. The current study aimed to test this existing grounded theory (Davie et al., Citation2021) to understand whether perceptions and practices of infant feeding are distinct among women who give birth to larger birthweight infants. The original theory and methodology used to compare the existing theory are described in the following section.
Methods
Setting and participants
This was a nested qualitative interview study within a longitudinal cohort study. Women were purposively sampled based on eligibility criteria following completion of the cohort study, and invited to take part via email. Study advertisements were also displayed in local healthcare centres. Eligible women were ≥18 years old, currently living in London (UK), and had a healthy larger birthweight infant aged between four and twelve months. In the absence of a standardised definition, a larger infant birthweight was defined a priori as infants with a birthweight of 4,000 g or above (Koyanagi et al., Citation2013; National Institute for Health and Care Excellence (NICE), Citation2019a). Women were not eligible to take part if they had a diagnosed mental health condition, or if their infant was premature (<37+0 weeks gestation) or admitted to a neonatal intensive care unit. Recruitment was open between June and December 2019. Women were offered a £20 shopping voucher as a ‘thank you’ for participating. A total of 13 women were interviewed and 10 women’s data were included in analyses. Two women were excluded from analysis because their babies’ birthweight was reported to be <4,000 g during interviews, and one woman had a feeding experience that differed significantly from the phenomena explored here (see ). Face-to-face, semi-structured interviews were conducted in participants’ homes or university meeting rooms, where infants were welcome. The women who took part in this study were older (MAge = 35.2 years), predominantly White, cisgender, worked in professional occupations, and all completed university education. All women were either married/civilly partnered or cohabiting with a long-term partner, and eight women were born outside the UK. Infants were born between October 2018 and April 2019 and weighed M = 4,186 g at birth (see ).
Figure 1. Flow Diagram of Participant Recruitment. Women were recruited from an existing longitudinal cohort study and poster advertisements displayed in local healthcare centres. *One woman interviewed was recommended by healthcare professionals to use formula milk in hospital, and exclusively expressed breastmilk (i.e. no direct breastfeeding) from hospital-discharge onwards to combination-feed her infant. As the experiences and support needs of women who exclusively express breastmilk are unique and not well understood (O’Sullivan et al., Citation2017; Strauch et al., Citation2019), and differed from the phenomena explored here, data from this interview were not included in analyses.
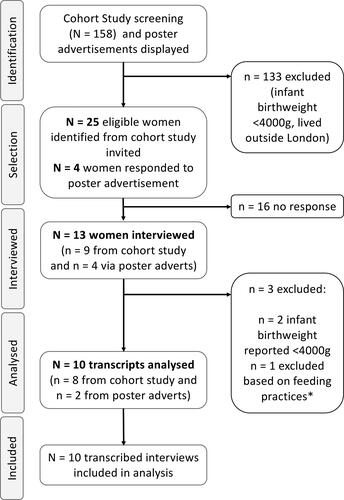
Table 1. Demographic characteristics of participants.
Data collection
An interview schedule was used to collect data about five aspects of infant feeding: Starting feeding, decision making, barriers and facilitators, infant birthweight, and support. The same scheduled developed for use in the original theory (Davie et al., Citation2021) was used in this study. The semi-structured nature allowed interviewers [PD , LJ] to explore key aspects of women’s perceptions and practices of feeding across all participants, and probe unique experiences raised by women. Interviews were audio-recorded, transcribed verbatim by the research team [PD , LJ], and pseudo-anonymised (see ). A short, structured questionnaire collected demographic data on women and their infants. Interviews lasted between 42-100mins (M = 68.72mins). An interdisciplinary health research team from psychology and women’s health enabled diverse interpretations of the data whilst ensuring any preconceived notions about the data or theory generation did not go without challenge.
Testing a pre-existing grounded theory
A recent study explored experiences of breastfeeding among women who gave birth to healthy full-term, average birthweight infants (Davie et al., Citation2021). Grounded Theory analysis of the data revealed three distinct themes that captured women’s breastfeeding experiences. Women monitored four aspects of infant behaviours (wet and dirty nappies; infant crying; weight gain; feeding frequency and duration) as ‘Perceived indicators of ‘good’ feeding’ (Theme 1) to assess whether feeding was going well. Women also described their experiences of ‘Breastfeeding latch’ (Theme 2) as ‘good’ or ‘bad’ (i.e. with pain and discomfort). Women’s ‘Overall breastfeeding experience’ (Theme 3) were described as positive, negative or uncertain. The analysis concluded that women appeared to give precedence to their experiences of latch over indicators of ‘good’ feeding (e.g. where a painful and uncomfortable latch could outweigh perceived cues that feeding was going well) such that experiences of latch could be understood as a mediating factor in how women experienced breastfeeding overall. The theory was described as a pathway analysis where three different breastfeeding experiences were achieved through four different pathways. This study aimed to explore whether this Grounded Theory held true in the context of women who give birth to larger birthweight infants.
Guided by the principles of ‘testing’ a Grounded Theory (Corbin & Strauss, Citation1990; Silverio et al., Citation2019) a specific population, phenomenon of interest, and context are set as parameters for investigation. In the original theory (Davie et al., Citation2021) these were healthy women (population) breastfeeding (phenomena) healthy average birthweight full-term infants (context). In the present study, both the phenomenon of interest and the population were kept the same, including the demographic characteristics of women in the samples. In both samples, women were predominantly White, married/civil partnered or cohabiting with a long-term partner, all educated to degree level and working in professional occupations (see ; Davie et al., Citation2021). However, in this study the context was changed to include healthy, larger birthweight term infants. In-line with previous guidance (Corbin & Strauss, Citation1990) the theoretical perspective, data collection method, and analytical approach were retained in this study to test the theory of the original study (Davie et al., Citation2021).
In this study, an inductive, data-driven analysis (Glaser & Strauss, Citation1967; Holton & Walsh, Citation2016) generated a series of codes and focussed-codes, before super-categories and themes were developed. Initial coding saw codes such as ‘ability, latch, demand’, grouped into the focussed code of ‘breastfeeding ability’. Codes such as ‘shock, anticipate, plan, and prepare’ were grouped into the focussed code of ‘expectations’, whereas the focussed code of ‘weight monitoring’ included codes of ‘track, monitor, centile’. Focussed codes were used throughout subsequent transcripts in-line with the constant-comparison method, before merging to form super-categories.
Attempts were made at all stages of analysis to match codes and focussed-codes from this analysis to the original theory. Whilst initial codes and super-categories were comparable (for example codes such as ‘latch’, ‘demand’, ‘weight-gain’ were observed in both analyses), this could be attributed to using the same interview schedule and investigating the same phenomenon of interest. However, when focussed-codes were formed and super-categories were collapsed into themes in order to generate a theory, the relationship between these themes was fundamentally different from the original theory (Davie et al., Citation2021), meaning the original theory is unlikely to “apply to a broad range of situations” (Corbin & Strauss, Citation1990. p15). For example, ‘latch’ appeared in codes and focussed codes in both analyses, but as a super-category in this study it was not associated with pain or emotional valence and did not feature as a predominant theme throughout transcripts. Similarly, women monitored infants’ behaviours as cues of feeding success, but the data here are distinct because these behaviours were attributed to infants’ ability to feed rather than an assessment of feeding success as observed in the original theory. Women in this sample also expressed considerably less concern and anxiety about infant weight loss compared to the context of women who gave birth to average birthweight infants. Finally, notions of worry, anxiety, distress, and inherently negative experiences were not prevalent in these data. Therefore, a new theory was proposed, grounded in the data available, and specific for this context (larger birthweight infants).
Data analysis
The specific approach and methodology adopted in this study was designed for use in interdisciplinary health research (Silverio et al., Citation2019). An iterative constant comparison method was used meaning each transcript was compared to the preceding transcript(s) before coding the next (Glaser, Citation1992; Holton & Walsh, Citation2016; Silverio et al., Citation2019). Focused codes, super-categories, and theory generation were discussed and debated amongst the research team [PD, DB, SAS, JC]. Theoretical saturation was accepted when analysing data from additional transcripts did not introduce any new concepts (Holton & Walsh, Citation2016; Vasileiou et al., Citation2018). Due to the iterative nature of analysis, data saturation was initially discussed amongst the team after seven transcripts were coded and agreed upon at the end of analysing ten transcripts. Thematic diagrams facilitated theory generation and guided final theory formation. In finalising the grounded theory, the research team debated the theory to establish a coherent narrative which outlined the processes and patterns observed in the thematic diagram (see ).
Figure 2. Thematic Grounded Theory map illustrating themes and subsumed super-categories (boxes). Women experienced and attributed their infants as having ability to breastfeed (Theme 1: Infant Ability to Breastfeed). Where women expressed concerns with breastfeeding, these were attenuated by larger infant birthweight and healthcare advice (Theme 2: Attenuating Maternal Concerns). Women’s experiences of baby ability to breastfeed helped to reduce discordance between expectations and the Reality of Breastfeeding (Theme 3), and the association was facilitated through attenuated maternal concerns.
Ethical approval
Ethical approval was awarded by a national Research Ethics Committee (Ref: 18/LO/0740) and data were handled in-line with EU Data Protection Regulation guidelines. Women provided fully informed written consent before the interview.
Results
In theory generation using data from all participants, nine super-categories were merged, collapsed, and/or split to form three themes (see ): Infant Ability to Breastfeed (latch, signs of satiety, milk supply); Attenuating Maternal Concerns (feeding frequency, weight loss, overfeeding); and Reality of Breastfeeding (expectations of feeding, adjustment to the feeding role, self-doubt and hard work). The findings of each theme are presented first, followed by an interpretation of theory which describes the interrelationships between themes. Illustrative quotations from each participant are used in the narrative below to example key components of the theory.
Theme 1. Infant ability to breastfeed
All women in the study reported intending to breastfeed and referenced three signs of effective feeding (breastfeeding latch; signs of satiety; milk supply), which contributed to being able to successfully breastfeed from the early postnatal period. Women directly and indirectly attributed infants as having ability to breastfeed, independent of maternal desire, which contributed to the successful initiation and maintenance of breastfeeding.
Breastfeeding latch
Women experienced infants were able to latch without pain, and perceived their infants as capable of latching efficiently without difficulties:
“I think so because he was, he was such a big boy and he had, he was strong, besides being big, he was very, very strong… you know his mouth was big, he was able to, he had the strength to suck properly, to hold on, he could hold his head up basically when he was born. So, I think that that did make a difference…” – Lauren, first baby
Table 2. Supplementary quotations providing evidence for themes and super-categories.
“I mean ‘cause she kind of latched on straight away…Um, but she could always find my nipple, she would always feed, she would always, you know, she’d been on for a little bit at a time and then you know, seemed satisfied when she came away. Um… yeah… She just seemed to know what she was doing.” – Vivienne, first baby
When women did experience pain or discomfort, this was perceived to be ‘normal’ or ‘expected’ pain that would be time limited:
“Um, so yeah it was kind of like the normal pain of ‘okay I know this is gonna be on for a few days’, a week, or whatever, but it did pass….” – Marissa, third baby
“So, I suppose once we kind of got out of the issues with the tongue tie, that he was satisfied after feeds, so he would kind of come off and he’d be happy to, to do other things and to wait those hour and a half, two hours without kind of demanding or crying for more food…he seemed content I suppose.” – Olivia, first baby
Signs of satiety
Women perceived multiple aspects of infant behaviour as signs that infants were feeding sufficiently, including infants falling asleep after feeds, being content, weight gain, having good output and feeding for sufficient durations (see ):
“So, first, you know all the physical things and I was noticing he was sucking properly, he was latching on properly, erm he was obviously increasing weight so that was good. I noticed that he wasn’t uncomfortable. I was happy with the position that I was in, the position that he was in.” – Lauren, first baby
“And so, I think I’ve been lucky that my personality type has been more, more willing to kind of remain calm and just trust the baby’s instinct and trust their appetite. Give them, try my best to give them what they want, when they want it…” – Katia, third baby
Milk Supply
Through perceived signs of satiety, women were reassured by infant behaviours that they were receiving adequate nutrition and subsequently did not express worry about breastmilk production, even when they could not quantify milk intake:
“Yeah, I mean I feel like he’s growing, and he’s healthy and he’s happy and he’s alert so I’m like well he seems to be getting what he needs so. Yeah, so I mean for me he seems like he’s, you know, getting what he needs from the milk so far.” – Marissa, third baby
“…so the knowing when he’s finished, I think I’ve always found a bit difficult, but I don’t think that fed through to worrying about whether he’d had enough milk or not. And I can’t rationally explain that…” – Sarah, first baby
“…that one day that I mentioned where she wouldn’t stop feeding, that was probably the only day where I was like… ‘How much? Will it run dry?! I’ve got no idea!’ And then I do remember at one-point kind of squeezing and there’s still a bit of milk, I was like, ‘still milk in here!’ [Laughs]. So… Yeah, that was not something I really thought about or worried about.” – Vivienne, first baby
Theme 2. Attenuating maternal concerns
Although women perceived infants were able to breastfeed and did not experience persistent difficulties, women still expressed some concerns about feeding frequency, infant weight loss, and overfeeding. However, infants’ larger birthweight was perceived as a sign of adequate nutrition and helped to reduce maternal concerns. These perceptions were affirmed by advice from healthcare professionals, which further attenuated maternal concern about feeding.
Feeding frequency
Women raised concerns when their infants were perceived as feeding too frequently, or not frequent enough, but reasoned their infants ‘needed more nutrients’ or ‘could go for longer’ due to their size (see ):
“So, when other babies were kind of bringing it down to maybe every three, four hours, he was still wanting to feed every two, two and a half hours and I think that was literally just he needed the food.” – Olivia, first baby
“Yeah. Also, we also asked the personnel at the hospital, the midwives ‘what’s going on? Baby’s feeding constantly, not giving us sleep!’. [They said] It’s cluster feeding relax [laughs]” – Megan, first baby
“…if someone had explicitly said, you’ve got a big baby, if he hadn’t kept up his weight trajectory there might be a problem but he has, and that means he’s feeding fine and you really don’t need to worry about it… Yeah, but if someone had said the reason he is doing that [feeding frequently] is because you’re feeding is going well then I would have felt better about it I think.” – Sarah, first baby
Weight loss
When infant’s growth did not track on their birthweight centile, and they gained weight at a slower rate, women raised some initial concern about infants ‘dropping down’ the centiles:
“Um, I was worried because they say that that’s something that is a potential worry… you kind of expect to see them putting on weight at a certain rate and she put on weight at less than that rate…” – Vivienne, first baby
“…but I wasn’t ever really worried about his weight because he’s such a, because I, rationally could always say to myself, he has weight to lose, it’s fine, I don’t need to worry about this.” – Sarah, first baby
“When the GP said to me, that’s because their birth percentile doesn’t necessarily reflect the size that they’re meant to be, it just reflects they’ve had a really good time in the womb [laughs] the last few weeks before they were born. They’ve had a good pregnancy but not necessarily that they’re going to be that big all throughout their life.” – Katia, third baby
Overfeeding concerns
Women also reported concerns about overfeeding their infants due to their larger birthweight. However, maternal concerns were attenuated if infants had slowed weight gain or did not continue to grow exponentially.
“I didn’t think he was going to be that big… I don’t want him obviously to be obese or you know, have problems with his weight and so on but to be honest by now, I think he dropped almost to sixty percentile, sixty… so I think he was just bigger because he was two weeks older when he was born and that’s really…Yes, so the midwives, they don’t have any issues with him dropping…” – Erica, first baby
Women’s concerns about overfeeding were reassured by advice from healthcare professionals and health services that breastfeeding was protective and that ‘breastfed babies could not be overfed’ (see ):
“…Yeah, that he was putting on so much weight and then came back to no ‘you can’t overfeed a breastfed baby’; we kind of need to all have the same awareness” – Olivia, first baby
Theme 3. Reality of breastfeeding
Women described their expectations about what they thought breastfeeding would entail. However, the expectations and the representations of ideals which women held about breastfeeding were somewhat discordant with their lived experiences of breastfeeding. While infant ability to feed and attenuated concerns helped to reduce discordance between expectations and reality, women still had to ‘adjust to the feeding role’. Throughout their experiences, women described ‘self-doubt’ and acknowledged breastfeeding was not achieved without hard work and perseverance.
Expectations of breastfeeding
Women held explicit expectations about what breastfeeding would be like, which accounted for a level of physical difficulty and demand, and helped women to anticipate potential problems:
“I have quite a lot of friends who have babies so I’d heard some stories that it doesn’t always go naturally, and it’s not always very easy in terms of latching, there can be problems… So I was prepared for that I knew that, you know, it’s not going to be 100% perfect latching and things like that” – Megan, first baby
“The first few weeks are really like, really the most demanding I find in terms of setting up a rhythm with them. Um so yeah, so that’s what I expected, not being able to get really anything done but sit around with the baby and have them feed for most of the day.” – Marissa, third baby
“I had that mentality that I wasn’t going to mind if things didn’t go one way and I had to change it but luckily erm, it was, it was all easy so that increased my confidence seeing that the first day he was able to feed…” – Lauren, first baby
“the fact that she could feed and that that was easy was-, is-, you know it wasn’t even a ‘Oh I’m really satisfied’, you don’t kind of think of it, or I didn’t think of it in a “Great. This is absolutely what I wanted”. It was more, ‘Good. What else have I got to worry about?’” – Vivienne, first baby
“And I think having had more awareness of that beforehand, would kind of prepare you better for it, so actually just knowing right, you’re going to have a month of literally barely leaving the seat, but this is why, and then it gets easier from there… I knew it was going to be intense but it was more than I expected it was going to be” – Marissa, third baby
“I think it’s always emotional talking about baby…but also there’s something so much more emotional about the feeding thing which I didn’t really expect” – Sarah, first baby
Adjustment to the feeding role
The reality of breastfeeding required women to adjust to the responsibility of feeding and incorporate the needs of the infant alongside their own:
“But I definitely… in my own life I reorganised a little bit more, so I spent less time going out and doing things and more time sitting at home with her making sure that she was having a good go at feeding on a regular basis.” – Katia, third baby
“I think before I had a baby, I didn’t understand that, that think how hard it is for the mother… I think that because I anyway look after him, that’s sort of a natural impulse. But to look after myself, it’s like the hardest part because he always comes first even though it was a lot like ‘put your life jacket on yourself first and then the baby’ but in practice I, I would do him first.” – Monica, first baby
“I would say actually now my main driver is as much as anything for the closeness and the emotional bond and then, like before you have a baby you think things matter, like convenience and like not washing bottles and nutrition [laughs] and then when you have a baby, erm you’re perfectly willing to do loads of inconvenient things in your life…” – Katia, third baby
“…there are so many different possibilities as to why he’s upset and you have absolutely no control over the vast majority of them….I think one of the things I found, so there was the kind of understanding, understanding that your baby may be difficult for kind of a week at a time and actually that’s fine and it doesn’t mean that your breastfeeding is failing, or that you can’t carry on doing it.” – Sarah, first baby
Self-doubt and hard work
Even though women did not experience overriding difficulties with breastfeeding, they still experienced self-doubt about whether breastfeeding was going well or not (see ):
“…all these transitions make you of course a little bit insecure, uncomfortable or unbalanced but know that it’s going to be okay.” – Monica, first baby
“…I hadn’t realised what a burden it would be solely on me. And the thing is, it is, and it isn’t… biologically I, you know, I’m… I’m her food source… So again, it’s something that I’m pretty conflicted about, but then I… I feel really privileged that I’ve been able to…that I’m able to do this.” – Vivienne, first baby
“Yes, er, probably not the first month because there was kind of a rough start and you’re not sure what you’re doing with your first baby. Enjoyed to an extent, yes, maybe sort of 80% enjoyed it and 20, 20 not because it is demanding…So yeah kind of mixed feelings probably mostly enjoyed but it’s not, not the easiest thing to do.” – Megan, first baby
Interpretation of theory: Easier, but not easy
Women perceived and experienced their infants had ability to breastfeed (Theme 1). Where women did express concern, they were reassured by larger infant birthweight and affirmations from healthcare professionals (Theme 2: Attenuating maternal concern). Maternal experiences of ‘Infant’s Ability to Breastfeed’ (Theme 1) were observed to reduce disparities between women’s expectations and ‘Reality of Breastfeeding’ (Theme 3), and this association between Theme 1 and Theme 3 was facilitated through ‘Attenuating Maternal Concerns’ (Theme 2). Women held explicit expectations about breastfeeding which accounted for a threshold of physical difficulty and demand, but still experienced unanticipated changes and challenges. Women’s experiences of ‘Infant’s Ability to Breastfeed’ helped to reduce discordances between expectations and reality, but women still had to adjust to the lived reality of breastfeeding. This required women to adjust to the responsibility of feeding, and despite women being able to breastfeed without overriding difficulty, women still experienced self-doubt and acknowledged breastfeeding was hard work. Overall, breastfeeding may have been easier for women with larger birthweight infants, in comparison to the observed experiences of women with average birthweight infants (Davie et al., Citation2021), but breastfeeding was by no means ‘easy’.
Discussion
This study aimed to qualitatively ‘test’ a Grounded Theory of breastfeeding experiences in a new context. The pre-existing theory of breastfeeding experiences among women with average birthweight infants (Davie et al., Citation2021) was not found to hold true in the context of women who gave birth to larger (≥4000 g) birthweight infants.
In this study, women did not experience persistent difficulties with breastfeeding latch or lactation, and directly or indirectly attributed infants as having ability to breastfeed. Even when pain had a recognised physiological origin (e.g. tongue tie), women did not experience persistent difficulties once the issues were addressed. This is distinct from experiences observed in the context of average birthweight infants where women reported persistent pain and difficulties with breastfeeding latch that did not always resolve, and caused physical and psychological distress (Davie et al., Citation2021). It is possible a larger infant birthweight may protect against latch difficulties as infants may have larger mouths and increased strength and head control movement, making the physiology of latching easier and reducing the likelihood of nipple pain and trauma; a common reason for early breastfeeding cessation (McClellan et al., Citation2012). By latching effectively, infants facilitate the demand and supply relationship of lactation, stimulating adequate milk production (Riordan, Citation2010a). This may also explain why women with larger birthweight infants perceived infants were feeding sufficiently and did not express concern over milk supply. This is distinct from patterns of behaviour observed in women with average birthweight infants (Davie et al., Citation2021), who monitored infant behaviours as signs of feeding success and questioned their milk supply when infant behaviours were perceived as problematic.
In the context of women who gave birth to average birthweight infants, women also responded to infant weight loss with anxiety and distress (Davie et al., Citation2021). Although women who gave birth to larger birthweight infants raised some initial concerns about infant weight and growth, the same anxiety and distress was not observed. Women perceived larger birthweight infants were expected to have or ‘could afford’ slowed weight gain. These perceptions were repeatedly affirmed by advice from healthcare professionals, which helped to alleviate concerns about feeding sufficiency and potentially avoided unnecessary supplementation. According to WHO-UK guidance, sustained slowed weight gain dropping two or more centiles (or three centiles for infants with a birthweight above the 91st centile) is used for a threshold of concern and calls for primary care assessment (National Institute for Health and Care Excellence (NICE), Citation2017; Royal College of Paediatrics and Child Health (RCPCH), 2013). While a larger infant birthweight reassures women, healthcare professionals should take care to ensure infant feeding and growth is assessed holistically, as reassurance through birthweight alone may conceal suboptimal growth due to physiological issues (e.g. tongue tie) or underlying morbidity.
Maternal concerns about overfeeding infants is unique to this context and women referenced concerns over childhood obesity. Larger infant birthweight is a recognised risk factor for childhood obesity, which may be attenuated through exclusive breastfeeding and exacerbated through formula supplementation and early introduction of solid foods (Çamurdan et al., Citation2011; Lande et al., Citation2005). Breastmilk is uniquely tailored to infants’ nutritional needs and its complex composition means infants do not receive excess nutrition than required, regardless of feeding frequency (Riordan, Citation2010b). Evidence-based healthcare advice that breastfed infants cannot be overfed reassured women in their ability to breastfeed and reduced concerns about overfeeding. However, for women with larger birthweight infants who are combination- or formula-feeding, concerns about overfeeding cannot be effectively attenuated with the same advice, and should be investigated in future research.
As observed across previous research (Fox et al., Citation2015; Hoddinott et al., Citation2012), women in this study held explicit expectations about breastfeeding that helped to manage experiences and prepare for difficulties. For example, women anticipated a threshold of physical difficulty when establishing breastfeeding. Antenatal education that discusses the realities of motherhood and actively prepares women for challenges, provides women with the knowledge, confidence and management practices necessary to breastfeed successfully ( Leurer & Misskey, Citation2015; McFadden et al., Citation2017; World Health Organization (WHO), United Nations Children’s Fund (UNICEF) Citation2018). Antenatal care and education (such as the UNICEF Baby Friendly Initiative) and positive previous breastfeeding experiences are recognised to increase the likelihood of breastfeeding in the early postnatal period (McAndrew et al., Citation2012; McFadden et al., Citation2017; World Health Organization (WHO), United Nations Children’s Fund (UNICEF), 2018). Women in this study may have received sufficient antenatal education (and knowledge from previous experience) that meant they were well-prepared for the realities of breastfeeding, and feeding success may therefore be unrelated to larger infant birthweight. Women in this study were also older, married/cohabiting with a long-term partner, and educated to degree level, increasing the likelihood of maintaining breastfeeding (Dennis, Citation2002; McAndrew et al., Citation2012) independent of infant birthweight.
Breastfeeding is valuable to women and infants, but as a health behaviour it places additional demands on women during a vulnerable time in the postnatal period. Previous research highlights breastfeeding is considered an idealism of motherhood (Shloim et al., Citation2015) and incurs unexpected psychological challenges for women as they attempt to assimilate needs of their infant alongside their own, as observed here. Evidence from this study also support previous observations that breastfeeding behaviour gives rise to competing goals for women (Sheehan et al., Citation2013) as they make personal and practical adjustments to account for the importance of the new behaviour (Oosterhoff et al., Citation2014). Furthermore, women in this study continued to experience self-doubt in the absence of breastfeeding difficulties and required reassurance from healthcare professionals to alleviate their concerns. It is therefore unlikely these experiences are unique to women with larger birthweight infants, and suggests women’s support needs for breastfeeding may not be distinct from existing care recommendations advocating for consistent and predictable postnatal care tailored to women’s individual care needs (National Institute for Health and Care Excellence (NICE), Citation2019b; World Health Organization (WHO), United Nations Children’s Fund (UNICEF) (WHO) Citation2018; World Health Organization (WHO), Citation2018).
Implications for practice
Findings from this study provide some insight into effective support for breastfeeding women, and direction for future research.
In this sample of women with larger birthweight infants, women did not experience persistent difficulties with breastfeeding latch or lactation, which helped to make breastfeeding easier for women. Previous Grounded Theory research found breastfeeding latch difficulties and insufficient milk supply were predominant barriers to breastfeeding success and contributed to women having negative breastfeeding experiences (Davie et al., Citation2021; Teich et al., Citation2014). In addition, latch pain is one of the most common reasons women cease breastfeeding early (Hauck et al., Citation2011; McClellan et al., Citation2012). Supporting women to have a pain-free and comfortable breastfeeding latch, and punctual assessment of physiological issues with lactation, can help to establish breastfeeding early in the postnatal period and support women to have a positive breastfeeding experience overall. These findings and implications for practice are complemented in conclusions from the original theory (Davie et al., Citation2021).
Findings from this study also highlight the necessity of reassurance and consistent support, even in the absence of breastfeeding difficulties. For example, women with average and larger birthweight infants worried about feeding frequency when intervals between feeds were perceived as too short or too long. These concerns are common amongst new mothers and existing evidence highlights women often lack clarity and confidence in determining how long and how often to breastfeed (Fallon et al., Citation2014; Leurer & Misskey, Citation2015). Women with larger birthweight infants attributed feeding frequency to their larger birthweight and provided heuristic reasons for feeding patterns (e.g. ‘needed the food’). When women recognise a reason for feeding frequency (perceived or actual) they are reassured in their ability to breastfeed (Marshall et al., Citation2007) and maternal concerns are attenuated, as observed in this study. Previous Grounded Theory exploring breastfeeding experiences also suggested when maternal interpretations of infant feeding cues are accurate, the demand and response positive feedback loop between mothers and infants is harmonious and supports breastfeeding (Waller et al., Citation2015).
Healthcare professionals can help to reassure women by normalising cluster feeding, promoting evidence-based guidance for on-demand breastfeeding not constrained by frequency of duration (World Health Organization (WHO), 2013; World Health Organization (WHO), United Nations Children’s Fund (UNICEF) Citation2018). Similar patterns in attenuating maternal concerns were also noted with infant weight gain, and suggest consistent and evidence-based reassurance from healthcare professionals help to provide women with confidence in their own abilities to breastfeed (Fox et al., Citation2015; Hoddinott et al., Citation2012). This is consistent with existing evidence that advocates for good quality breastfeeding support and counselling in the absence of breastfeeding difficulties (McFadden et al., Citation2017; World Health Organization (WHO), United Nations Children’s Fund (UNICEF) Citation2018). This includes health education available to women in the antenatal period. Unrealistic expectations about infant feeding can cause postnatal conflict between ideals and realities and create needs that are unmet by the current healthcare systems (Fox et al., Citation2015; Hoddinott et al., Citation2012). A previous Grounded Theory has highlighted how women’s experiences of breastfeeding and breastfeeding support are shaped by the discordance between their expectations and reality (Hunt & Thomson, Citation2017). As discussed above, ensuring women are well-prepared for the realities of breastfeeding will provide women with the confidence and skill to breastfeed long-term.
Limitations
All women recruited for this study intended to breastfeed and exclusively breastfed for at least four months, but women were not sampled based on their feeding practices. This suggests a self-sampling bias was present, meaning women included had capacity and capability to breastfeed and may have been more open to discussing breastfeeding experiences. In line with Grounded Theory methodology (Glaser & Strauss, Citation1967; Holton & Walsh, Citation2016), the experiences of women observed here may only be transferred or contextualised among breastfeeding women, and further research is required to understand combination- or formula-feeding experiences among women who give birth to larger birthweight infants. Existing evidence suggests predisposing factors for macrosomia (i.e. maternal obesity and diabetes) present additional barriers to breastfeeding (Haile et al., Citation2016; Turcksin et al., Citation2014), which were not accounted for or explored in this study. In addition, this study specifically targeted breastfeeding women in the recruitment strategy rather than parents. As we acknowledge that not all breastfeeding parents may identify as women, this limits how these findings can be transferred or contextualised
A lack of standardized definition of larger infant birthweight introduces complexity to data presented. As larger infant birthweight was defined by weight limit, it is difficult to distinguish whether breastfeeding patterns and experiences are related to absolute birthweight or gestational development. Among infants included, although all were ≥4,000 g, only five were also considered LGA according to WHO-UK growth charts (Royal College of Paediatrics and Child Health (RCPCH), 2013). The sample was homogenous in terms of sociodemographic characteristics, but homogeneity of the sample is crucial to Grounded Theory methodology which aims to generate theoretical explanations for a specific phenomenon in a specific cohort (Glaser, Citation1992; Silverio et al., Citation2019).
Conclusion
A pre-existing Grounded Theory of breastfeeding experiences derived from women with average birthweight infants was not found to hold true in the context of women who gave birth to larger (≥4000 g) birthweight infants. A new Grounded Theory suggested women with larger birthweight infants perceived and experienced infants had ability to breastfeed with effective latch, which likely facilitated lactation and breastfeeding establishment from early in the postnatal period. Women’s concerns about breastfeeding were attenuated by larger infant birthweight and affirmative advice from healthcare professionals. Unique concerns about overfeeding observed in this context were reassured by evidence-based healthcare advice and breastfeeding practices. Women with larger birthweight infants did not experience comparable levels of worry and distress as observed in women with average birthweight infants (Davie et al., Citation2021). However, this did not alleviate the burden that breastfeeding behaviour placed on women as they still had to adjust to the lived reality of breastfeeding.
The role of healthcare professionals as providers of reassurance and evidence-based care throughout the postnatal period was crucial, even in the absence of breastfeeding difficulties. This study supports observations that women require good breastfeeding knowledge and encouragement to achieve their goals, and contributes further evidence to support prolonged and individualised postnatal care. It is feasible that breastfeeding may be easier for women with larger birthweight infants, in comparison to the observed experiences of women with average birthweight infants (Davie et al., Citation2021), but that did not mean breastfeeding was easy for women. This study expanded on the currently limited evidence base for associations between larger birthweight and perceptions and practices of infant feeding, and suggests the support needs of women with healthy, larger birthweight infants may not be distinct from support and care recommendations currently available.
Acknowledgements
The authors wish to thank Ms Louise Jones (LJ) for her contributions to data collection and analysis, and extend their thanks and gratitude to all the women enrolled in the PIPINS study for their time and contribution to this research.
Disclosure statement
The authors declare no conflict(s) of interest.
Data availability statement
Due to the qualitative nature of this research, participants in this study did not agree for their data to be shared publicly. Therefore, full transcripts of supporting data are not available.
Additional information
Funding
References
- Ayukarningsih, Y., & Dwinanda, A. (2015). Early initiation of breastfeeding at Dustira hospital. Paediatrica Indonesiana, 55(3), 126–130. https://doi.org/10.14238/pi55.3.2015.126-30
- Çamurdan, M. O., Çamurdan, A. D., Polat, S., & Beyazova, U. (2011). Growth patterns of large, small, and appropriate for gestational age infants: impacts of long-term breastfeeding: a retrospective cohort study. Journal of Pediatric Endocrinology & Metabolism, 24(7-8), 463–468. https://doi.org/10.1515/jpem.2011.168
- Chiavaroli, V., Derraik, J. G. B., Hofman, P. L., & Cutfield, W. S. (2016). Born Large for Gestational Age: Bigger Is Not Always Better. The Journal of Pediatrics, 170(3), 307–311. https://doi.org/10.1016/j.jpeds.2015.11.043
- Corbin, J., & Strauss, A. (1990). Grounded theory research: procedures, canons, and evaluative criteria. Qualitative Sociology, 13(1), 3–21. https://doi.org/10.1007/BF00988593
- Cordero, L., Oza-Frank, R., Landon, M. B., & Nankervis, C. A. (2015). Breastfeeding initiation among macrosomic infants born to obese nondiabetic mothers. Breastfeeding Medicine, 10(5), 239–245. https://doi.org/10.1089/bfm.2015.0028
- Davie, P., Chilcot, J., Jones, L., Bick, D., & Silverio, S. A. (2021). Indicators of ‘good’ feeding, breastfeeding latch, and feeding experiences among healthy women with healthy infants: A qualitative pathway analysis using Grounded Theory. Women and Birth, 34(4), e357–e367. https://doi.org/10.1016/j.wombi.2020.08.004
- Dennis, C. L. (2002). Breastfeeding initiation and duration: A 1990-2000 literature review. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 31(1), 12–32. https://doi.org/10.1111/j.1552-6909.2002.tb00019.x
- Fallon, A., Van der Putten, D., Dring, C., Moylett, E. H., Fealy, G., & Devane, D. (2014). Baby-led compared with scheduled (or mixed) breastfeeding for successful breastfeeding. Cochrane Database of Systematic Reviews, 2014(7). https://doi.org/10.1002/14651858.CD009067.pub2
- Fox, R., McMullen, S., & Newburn, M. (2015). UK women’s experiences of breastfeeding and additional breastfeeding support: a qualitative study of Baby Café services. BMC Pregnancy and Childbirth, 15(1), 1-12. https://doi.org/10.1186/s12884-015-0581-5
- Glaser, B. G. (1992). Basics of grounded theory analysis. Sociology Press.
- Glaser, B. G., & Strauss, A. L. (1967). The discovery of Grounded Theory: Strategies for qualitative research. Aldine.
- Haile, Z. T., Oza-Frank, R., Chertok, I. R. A., & Passen, N. (2016). Association between history of gestational diabetes and exclusive breastfeeding at hospital discharge. Journal of Human Lactation, 32(3), 36–43. https://doi.org/10.1177/0890334415618936
- Hauck, Y. L., Fenwick, J., Dhaliwal, S. S., & Butt, J. (2011). A western Australian survey of breastfeeding initiation, prevalence and early cessation patterns. Maternal and Child Health Journal, 15(2), 260–268. https://doi.org/10.1007/s10995-009-0554-2
- Hoddinott, P., Craig, L. C., Britten, J., & McInnes, R. M. (2012). A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open, 2(2), e000504. https://doi.org/10.1136/bmjopen-2011-000504
- Holton, J. A., & Walsh, I. (2016). Classic grounded theory: Applications with qualitative and quantitative data. Sage Publications.
- Horta, B. L., Victora, C., G. (2013). Long-term effects of breastfeeding: A systematic review. Geneva: World Health Organization. Available from: https://www.who.int/maternal_child_adolescent/documents/breastfeeding_long_term_effects/en/
- Hunt, L., & Thomson, G. (2017). Pressure and judgement within a dichotomous landscape of infant feeding: a grounded theory study to explore why breastfeeding women do not access peer support provision. Maternal & Child Nutrition, 13(2), e12279. https://doi.org/10.1111/mcn.12279
- Koyanagi, A., Zhang, J., Dagvadorj, A., Hirayama, F., Shibuya, K., Souza, J. P., & Gülmezoglu, A. M. (2013). Macrosomia in 23 developing countries: an analysis of a multicounty, facility-based, cross-sectional survey. The Lancet, 381(9865), 476–483. https://doi.org/10.1016/S0140-6736(12)61605-5
- Lande, B., Andersen, L. F., Henriksen, T., Baerug, A., Johansson, L., Trygg, K. U., Bjørneboe, G.-E., & Veierød, M. B. (2005). Relations between high ponderal index at birth, feeding practices and body mass index in infancy. European Journal of Clinical Nutrition, 59(11), 1241–1249. https://doi.org/10.1038/sj.ejcn.1602235
- Leonard, S. A., & Rasmussen, K. M. (2011). Larger infant size at birth reduces the negative association between maternal pre-pregnancy body mass index and breastfeeding duration. The Journal of Nutrition, 141(4), 645–653. https://doi.org/10.3945/jn.110.129874
- Leurer, M. D., & Misskey, E. (2015). "Be positive as well as realistic": a qualitative description analysis of information gaps experienced by breastfeeding mothers”: . International Breastfeeding Journal, 10(10), 1–11. https://doi.org/10.1186/s13006-015-0036-7
- Lumbiganon, P., Martis, R., Laopaiboon, M., Festin, M. R., Ho, J. J., & Hakimi, M. (2016). Antenatal breastfeeding education for increasing breastfeeding duration. Cochrane Database of Systematic Reviews, 2016(12), https://doi.org/10.1002/14651858.CD006425.pub4
- Marshall, J. L., Godfrey, M., & Renfrew, M. J. (2007). Being a ‘good mother’: managing breastfeeding and merging identities. Social Science & Medicine (1982), 65(10), 2147–2159. https://doi.org/10.1016/j.socscimed.2007.06.015
- McAndrew, F., Thompson, J., Fellows, L., Large, A., Speed, M., & Renfrew, M. J. (2012). Infant feeding survey 2010. Health and Social Care Information Centre. Retrieved from http://www.hscic.gov.uk/catalogue/PUB08694/Infant-Feeding-Survey-2010-Consolidated-Report.pdf
- McClellan, H. L., Hepworth, A. R., Garbin, C. P., Rowan, M. K., Deacon, J., Hartmann, P. E., & Geddes, D. T. (2012). Nipple pain during breastfeeding with or without visible trauma. Journal of Human Lactation, 28(4), 511–521. https://doi.org/10.1177/0890334412444464
- McFadden, A., Gavine, A., Renfrew, M. J., Wade, A., Buchanan, P., Taylor, J. L., … MacGillivray, S. (2017). Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews, 2017(2). https://doi.org/10.1002/14651858.CD001141.pub5
- National Institute for Health and Care Excellence (NICE). (2017). Faltering growth: recognition and management of faltering growth in children (NG75): 1.2 Faltering growth after the early days of life. Retrieved from https://www.nice.org.uk/guidance/ng75/chapter/Recommendations#weight-loss-in-the-early-days-of-life
- National Institute for Health and Care Excellence (NICE). (2019a). Intrapartum care for women with existing medical conditions or obstetric complications and their babies (NG121): 1.17 Large-for-gestational-age baby. Retrieved from https://www.nice.org.uk/guidance/ng121/chapter/Recommendations
- National Institute for Health and Care Excellence (NICE). (2019b). Antenatal care for uncomplicated pregnancies clinical guidance (CG62): 1.1.1 Women-centred care and informed decision-making: Antenatal information. Retrieved from https://www.nice.org.uk/guidance/cg62/chapter/1-Guidance
- Oosterhoff, A., Hutter, I., & Haisma, H. (2014). It takes a mother to practise breastfeeding: Women’s perceptions of breastfeeding during the period of intention. Women and Birth, 27(4), E43–E50. https://doi.org/10.1016/j.wombi.2014.08.003
- O’Sullivan, E. J., Geraghty, S. R., & Rasmussen, K. M. (2017). Human milk expression as a sole or ancillary strategy for infant feeding: a qualitative study. Maternal & Child Nutrition, 13(3), e12332. https://doi.org/10.1111/mcn.12332
- Poston, L. (2012). Maternal obesity, gestational weight gain and diet as determinants of offspring long term health. Best Pract Res Clin Endocrinol Metab, 26(5), 627–639. https://doi.org/10.1016/j.beem.2012.03.010
- Riordan, J. (2010a). Anatomical and Biological Imperatives: Chapter 3: Anatomy and Physiology of Lactation. In J. Riordan & K. Wambach (Eds.), Breastfeeding and Human Lactation. (5th ed., pp. 77–112). Jones and Bartlett Publishers International.
- Riordan, J. (2010b). Anatomical and Biological Imperatives: Chapter 4: Biological Specificity of Breastmilk. In J. Riordan & K. Wambach (Eds.), Breastfeeding and Human Lactation (5th ed., pp. 121–170). Jones and Bartlett Publishers International.
- Royal College of Paediatrics and Child Health (RCPCH). (2013). Early years UK-WHO growth charts and resources: 0- 4years (2nd ed., January 2013). Retrieved from https://www.rcpch.ac.uk/growthcharts/
- Sheehan, A., Schmied, V., & Barclay, L. (2013). Exploring the process of women’s infant feeding decisions in the early postbirth period. Qualitative Health Research, 23(7), 989–998. https://doi.org/10.1177/1049732313490075
- Shloim, N., Hugh-Jones, S., Rudolf, M. C. J., Feltbower, R. G., Lans, O., & Hetherington, M. M. (2015). "It’s like giving him a piece of me.": Exploring UK and Israeli women’s accounts of motherhood and feeding.”.Appetite, 95, 58–66. https://doi.org/10.1016/j.appet.2015.06.004
- Silverio, S. A., Gauntlett, W., Wallace, H., & Brown, J. (2019). (Re)discovering Grounded Theory for Cross-Disciplinary Qualitative Health Research. In B. Clift, J. Gore, S. Bekker, I.C. Batlle, K. Chudzikowski, J. Hatchard (Eds), Qualitative research symposium (Edited Volume 1, pp. 41–60). University of Bath.
- Strauch, L., Sweet, L., Scott, H., & Müller, A. (2019). Mechanisms of support for exclusive breastmilk expressers in the community: a scoping review. BMC Pregnancy and Childbirth, 19(1), 511. https://doi.org/10.1186/s12884-019-2667-y
- Teich, A. S., Barnett, J., & Bonuck, K. (2014). Women’s Perceptions of Breastfeeding Barriers in Early Postpartum Period: A Qualitative Analysis Nested in Two Randomized Controlled Trials. Breastfeeding Medicine : The Official Journal of the Academy of Breastfeeding Medicine, 9(1), 9–15. https://doi.org/10.1089/bfm.2013.0063
- Turcksin, R., Bel, S., Galjaard, S., & Devlieger, R. (2014). Maternal obesity and breastfeeding intention, initiation, intensity and duration: a systematic review. Maternal & Child Nutrition, 10(2), 166–183. https://doi.org/10.1111/j.1740-8709.2012.00439.x
- Vasileiou, K., Barnett, J., Thorpe, S., & Young, T. (2018). Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Medical Research Methodology, 18(1), 148–118. https://doi.org/10.1186/s12874-018-0594-7
- Victora, C. G., Bahl, R., Barros, A. J. D., França, G. V. A., Horton, S., Krasevec, J., Murch, S., Sankar, M. J., Walker, N., & Rollins, N. C. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475–490. https://doi.org/10.1016/S0140-6736(15)01024-7
- Waller, J., Bower, K. M., Spence, M., & Kavanagh, K. F. (2015). Using grounded theory methodology to conceptualize the mother-infant communication dynamic: potential application to compliance with infant feeding recommendations. Maternal & Child Nutrition, 11(4), 749–760. https://doi.org/10.1111/mcn.12056
- World Health Organization (WHO). (2013). WHO recommendations on postnatal care of the mother and newborn. Geneva: World Health Organization. Retrieved from https://www.who.int/maternal_child_adolescent/documents/postnatal-care-recommendations/en/
- World Health Organization (WHO), United Nations Children’s Fund (UNICEF). (2018). Protecting, promoting, and supporting breastfeeding in facilities providing maternity and newborn services: The revised baby-friendly hospital initiative implementation guidance. Geneva: World Health Organization. Retrieved from https://www.who.int/nutrition/publications/infantfeeding/bfhi-implementation/en/
- World Health Organization (WHO). (2018). Guideline: Counselling of women to improve breastfeeding practices. Geneva: World Health Organization. Retrieved from https://www.who.int/nutrition/publications/guidelines/counselling-women-improve-bf-practices/en/
- Yu, Z., Sun, J. Q., Haas, J. D., Gu, Y., Li, Z., & Lin, X. (2008). Macrosomia is associated with high weight-for-height in children aged 1-3 years in Shanghai, China. International Journal of Obesity (2005), 32(1), 55–60. https://doi.org/10.1038/sj.ijo.0803765
