Abstract
Objective
Fibromyalgia syndrome (FMS) is a chronic condition with symptoms known to be exacerbated by stress. Individuals with FMS may be experiencing particular distress under Covid-19 pandemic-related lifestyle restrictions. The present study examined wellbeing, perceived symptom change and coping in individuals with and without FMS during pandemic-related social lockdown in the UK.
Design
Participants with a diagnosis of FMS (N = 390) and a general public sample with no FMS (N = 151) completed questionnaires at three time points.
Main Outcome Measures
BBC Wellbeing Scale, Cognitive-Emotional Regulation Questionnaire measure of coping, perception of extent to which symptoms have worsened or improved over time.
Results
Contrary to expectations, FMS participants reported no worsening of symptoms and an increase in wellbeing over the study period. Non-FMS participants experienced worsening health symptoms and no change in wellbeing. Coping strategies involving positive reappraisal, refocussing and planning were positively associated with wellbeing in the FMS group.
Conclusion
The unpredictable symptom profile in FMS, and the regular readjustment this necessitates, may support a form of resilience which has been adaptive during the pandemic. The results have implications for supporting people with FMS, and potentially other chronic conditions, especially at times of stress.
Keywords:
Introduction
Fibromyalgia syndrome (FMS) is characterised by chronic widespread pain although most patients report a wide range of somatic, cognitive and psychological symptoms (Di Tella et al., Citation2017; Marangell et al., Citation2011; Thieme et al., Citation2004). FMS can result in considerable physical and psychosocial impairments that impact significantly on wellbeing, and on health and social care services (Bateman et al, 2016; Creed et al., Citation2012; Spaeth, Citation2009). The heterogeneous and highly idiosyncratic nature of FMS has led to recommendations for individualised support and treatment and the more we understand about the factors contributing to symptom levels and wellbeing, the better placed we are to offer this.
The aetiology and pathophysiology of FMS have been the subject of much debate, leading to its general classification as a functional disorder (one with medically unexplained symptoms), alongside other conditions such as Chronic Fatigue Syndrome and Irritable Bowel Syndrome, with which it shares symptomology. However, there is increasing evidence that these disorders are examples of central sensitivity syndrome (CSS), whereby the amplification of sensory input to the central nervous system results in a perception of pain from stimuli which are usually non-painful, such as clothing against the skin (allodynia), and greater pain than would be expected from painful stimuli (hyperalgesia; Sluka & Clauw, Citation2016; Turk & Monarch, Citation2018). A possible contributor to development of CSS in genetically predisposed individuals is stress. Research has suggested that people with fibromyalgia present abnormal levels of stress reactivity linked to functional abnormalities in the autonomic nervous system and hypothalamic–pituitary adrenal axis (Martinez-Lavin, Citation2007; Woda et al., Citation2016, for reviews). This in turn can negatively influence severity of symptoms, physical and psychological adjustment, coping and eventual health outcomes (Adams & Turk, Citation2015; Daniels et al., Citation2006; Dell’Osso et al., Citation2011; Griep et al., Citation1993; Light et al., Citation2009). Furthermore, living with FMS is stressful in itself because of the wider impact on employment, socialising, relationships and family life, (Galvez-Sanchez et al., 2018). Stress in FMS may be further exacerbated by illness uncertainty, defined by Mishel (Citation1999) as an inability to determine the meaning of illness-related events or accurately predict outcomes because of insufficient information. Illness uncertainty is found to be significantly higher in FMS compared to other chronic conditions (Reich et al., Citation2006), and is stressful because unpredictable symptoms, unclear aetiology and few treatment options result in feelings of uncontrollability. Uncertainty is known to increase symptom burden and influence the efficacy of coping (Johnson et al., Citation2006), a key focus of the present research.
Many people with FMS tend to use maladaptive coping processes such as catastrophising (exaggerated thoughts about the seriousness of events and their potential consequences), a strategy which results in amplified negative somatic hypervigilance, increased pain perception, negative affect and disruption to cognitive processing (Galves-Sanchez et al., Citation2018). Most recently, Galvez-Sánchez et al. (2020) have shown that catastrophising mediates the effect of pain and anxiety on physical functioning, general health perception, vitality, mental health, and overall quality of life in FMS. Conversely, strategies such as positive reframing or reappraising the situation (seeing it in a positive light, as an opportunity for insight or personal growth) can be emotionally beneficial, reducing hyperarousal in the central nervous system and supporting symptom management (Edwards et al., Citation2009; Feliu-Soler et al., Citation2017; Galves-Sanchez et al., Citation2018; Geenen et al., Citation2012, 2015; Houdenhove & Luyten, Citation2007; Malfliet et al., Citation2017). The present study employed the model of coping defined by Garnefski et al. (Citation2001, Citation2002) who identified nine distinct cognitive strategies which support the regulation of emotion. Five strategies are classed as adaptive: Putting into Perspective (emphasising severity in relation to worse possibilities), Positive Refocusing (thinking about more joyful and pleasant issues); Positive Reappraisal (finding a positive meaning in terms of personal growth), Acceptance (accepting and resigning to what has happened) and Planning (thinking about how to handle the situation proactively). Four other strategies can be classed as maladaptive: Self- and-other blame (putting blame for the event on the self or another person respectively), Rumination (repeatedly dwelling on feelings and thoughts associated with the negative event) and Catastrophising (emphasising the terror and extremity of the experience). Research has supported these classifications, and the potential for positive or negative emotional outcomes respectively, across a range of applied health settings (e.g. Garnefski & Kraaij, Citation2012; Garnefski et al., Citation2013; Kraaij & Garnefski, Citation2015), though only one study to our knowledge specifically concerned FMS. Feliu-Soler et al. (Citation2017) examined the psychometric properties of the Cognitive Emotional Regulation Questionnaire (CERQ: Garnefski et al., Citation2001) and found it to be a reliable instrument for use with a FMS population both in terms of the nine strategy factor structure and when items were classified into two factors, adaptive and less-adaptive. Catastrophising, Rumination, and Self-blame emerged as counterproductive strategies whilst Positive refocusing seemed most helpful in terms of the relationship with pain experience and depression.
The present research examines the association between coping and wellbeing in a sample of UK adults with a diagnosis of FMS. What is novel about this study is that it was conducted in the context of a specific and novel, contemporary, stressful situation - the 2020 coronavirus (COVID-19) pandemic. At the time of the study, research was suggesting rising levels of pandemic-related psychological distress in the general population worldwide (e.g. Asmundson & Taylor, Citation2020; Bueno-Notivol et al. Citation2021 ; Pan et al., 2020; Wang et al., Citation2021). This concords with evidence from the severe acute respiratory syndrome (SARS) pandemic of the early 2000s, and the 2009 H1N1 (swine flu) outbreak, which also showed elevated symptoms of stress, general and health-related anxiety (Chong et al., Citation2004; Taylor, Citation2019; Wheaton et al., Citation2012; Wu et al., Citation2009). Three weeks before the present study commenced, the UK Government embarked on legislative restrictions aimed at constraining the spread of coronavirus. The new regulations required people to only leave home for essential reasons, namely, shopping for basic necessities, one form of exercise a day, medical needs, or for work only where work from home was not possible (NHS , 2020). Similar restrictions were in place in many countries across the world, including the USA and elsewhere in Europe (World Health Organization, Citation2020). What has become widely referred to as ‘lockdown’ (leaving home only infrequently and for very specific and essential reasons) has resulted in stressful circumstances for many people (Droit-Volet et al., Citation2020; Kang et al., Citation2020; Rubin & Wessely, Citation2020). When our study commenced in late April 2020, 3300 people in the UK had tested positive for coronavirus and 114 had died (Public Health England, Citation2020). Across the world, over 1 million cases had been reported. At the time of our final data collection in the first week of June 2020, these figures had risen to 274,762 confirmed cases and 38,489 deaths in the UK. Cases worldwide had risen to over six million with over 370,000 deaths.
Given the known association between FMS and psychological distress, we might expect the Covid pandemic and associated restrictions to be especially difficult for people living with the condition. The lack of a treatment or vaccine (at the time this study was conducted) together with frequently changing social guidelines also give rise to a high level of uncertainty. We examined cognitive-emotional coping strategies, FMS symptomology and overall wellbeing in a sample of people with FMS and a healthy population at three time points: first in the third week of lockdown in the UK, then twice more over the subsequent six weeks. Overall, given the evidence above, we predicted that participants with FMS would report a higher symptom burden and lower wellbeing compared to participants with no FMS at first testing (Prediction 1). The main area of interest was how they fared over time under lockdown conditions. It was predicted that for participants with FMS, we would observe: worsening of symptoms (Prediction 2), decreasing levels of wellbeing (Prediction 3) and greater use of maladaptive coping strategies, compared to adaptive strategies (Prediction 4). In addition, we examined whether variance in wellbeing was accounted for by coping strategies, over and above that explained by symptoms.
Methods
Ethical approval was obtained from the university faculty ethical committee. The study was conducted online over three time points.
Time 1: Week commencing 6 April 2020, the third week of compulsory lockdown requirements in the UK.
Participants
FMS group
Three hundred and ninety participants were recruited through online support groups for individuals living with FMS (367 identified as female, 20 as male, 3 as other; Mage = 43.90, SD = 12.02, range 18-72). Socio-economic status (SES) was assessed with the MacArthur Ladder Scale, which ranks self-reported social class on a ladder with 10 rungs (Adler et al., Citation2000) – the higher rungs represent individuals who have more money, education and prestigious jobs. The mean report was 5.11 (SD = 1.82) with 69 people (17.7%) placing themselves on the bottom three rungs, and 16 (4.1%) on the top three rungs. Ninety-two (23.6%) lived alone, 243 (62.3%) with a spouse/partner, 33 (8.5%) with parents or carer and 22 (5.6%) with friends/others. One hundred and forty participants (35.9%) had children aged under 18 living with them. Inclusion criteria was that they had to be aged 18 or over, living in the UK and have a current clinical diagnosis of FMS.
Non-FMS group
One hundred and fifty-one members of the UK public were recruited though Prolific, an online research participant platform, found to be representative of the general population (Woods et al., Citation2015): 96 identified as female, 55 male (Mage = 30.57, SD = 10.33, range 18-63). The mean SES report on the ladder scale was 4.62 (SD = 1.70) with 19 people (12.5%) placing themselves on the bottom three rungs, and 9 (5.9%) on the top three rungs. Twenty-one participants (13.9%) lived alone, 66 (43.7%) with a spouse/partner, 48 (31.8%) with parents or carer and 16 (10.6%) with friends/other. Fifty-nine participants (39%) had children aged under 18 living with them. Inclusion criteria was age 18 or over, living in the UK and never to have had a clinical diagnosis of FMS, CFS or IBS. They were paid £2.
Materials and procedures
Support group organisers circulated details to their members, including a link to the study. Participants were presented with details of the research and were required to give informed consent by checking a box before the study could commence. After providing the demographic details above, they completed the following measures:
General symptom questionnaire (GSQ-65; Hyland et al., Citation2019)
This scale was developed specifically for assessing a wide range of symptoms associated with FMS, chronic fatigue syndrome and irritable bowel syndrome, all polysymptomatic, and often co-morbid, conditions presenting a wide range of overlapping symptoms, many of which are unrelated to diagnostic criteria. Sixty-five commonly reported symptoms are listed and participants asked to rate the frequency with which they experience each symptom on a scale from 1 = never, or almost never to 6 = every day. Frequency ratings are averaged to provide an overall score. For the non-FMS group the questionnaire was described as measuring frequency of commonly reported health complaints. Reliability was excellent (FMS group α = .95; Non-FMS group α = .97).
BBC subjective wellbeing scale (BBC-SWB; Pontin et al., Citation2013)
This 24-item measure assesses wellbeing in terms of three dimensions: psychological wellbeing (e.g. Do you feel optimistic about the future?), physical health and wellbeing (e.g. Are you happy with your ability to perform daily living activities) and relationships (e.g. Are you comfortable about way you relate and connect with others?). The measure was developed for inclusion in an online population survey hosted by the BBC but has since been validated as a reliable and psychometrically robust measure for the online assessment of subjective well-being in the general population. It was chosen for the present study because of its accessibility and user-friendly language. Reliability was good in the present study, FMS group psychological health α = .86, physical health α = .71, relationships α = .77; non-FMS group psychological health α = .88, physical health α = .81, relationships α = .84.
Cognitive emotion regulation questionnaire short (CERQ-short; Garnefski & Kraaij, Citation2006)
This 18-item version of the CERQ measures nine coping strategies, with two items per scale. Each item reflects what individuals may think when experiencing a stressful or threatening event and participants respond on a scale ranging from 1 (almost never) to 5 (almost always). A subscale score is obtained by summing responses to the items, hence the maximum score is 10. The higher the subscale score, the more that specific cognitive strategy is used. The subscales showed adequate or good reliability: FMS group: self-blame α = .67, acceptance α = .79, rumination α = .62, positive refocussing α = .78, planning α = .76, positive reappraisal α = .72, putting into perspective α = .65, catastrophising α = .83, other-blame α = .84. Non-FMS group: self-blame α = .82, acceptance α = .81, rumination α = .72, positive refocussing α = .84, planning α = .72, positive reappraisal α = .74, putting into perspective α = .67, catastrophising α = .84, other-blame α = .82.
Participants were finally presented with an item stating, ‘Please think about your fibromyalgia symptoms [or health for the non-FMS group] in general and indicate how much your symptoms have changed over the last 3 weeks’. We presented a response scale where 1 = a lot worse and 5 = a lot better. Participants were then given more details about the follow-up phases and asked if they would agree to be contacted again about these. If so, they were asked to provide a contact email address: 321 (82%) of the FMS group and 147 (97%) of the non-FMS sample did so.
Time point 2: Week commencing 4 May 2020, three weeks after time point 1. Participants who had agreed to take part were emailed using the addresses they had provided and sent a link to the second part of the study. On accessing the study, participants were reminded of their ethical rights and checked a box to give further consent.
Participants at time 2
FMS group
One hundred and seventy-four people took part (54% of those contacted; 14 male, 159 female, 1 other; Mage = 45.51, SD = 12.22, range 18-77). Non-FMS group: One hundred and sixty-three people took part (84% of those contacted; 51 males, 112 females; Mage = 32.26, SD = 11.16, range 18-80).
Materials and procedures
BBC-SWB (Pontin et al., Citation2013) as described above. FMS group psychological health α = .85, physical health α = .68, relationships α = .81; non-FMS group psychological health α = .87, physical health α = .80, relationships α = .83.
CERQ (Garnefski & Kraaij, Citation2006) as described above. FMS group: self-blame α = .71, acceptance α = .74, rumination α = .62, positive refocussing α = .84, planning α = .69, positive reappraisal α = .74, putting into perspective α = .65, catastrophising α = .70, other-blame α = .85. Non-FMS group: self-blame α = .85, acceptance α = .84, rumination α = .66, positive refocussing α = .82, planning α = .68, positive reappraisal α = .74, putting into perspective α = .71, catastrophising α = .81, other-blame α = .87.
Finally, participants were presented with the question asking whether they perceived symptoms to have improved or worsened since time 1 in terms of the scale where 1 = a lot worse and 5 = a lot better. They were given details about the final follow-up phase and asked if they would agree to be contacted again and, if so, to provide their email address: 150 (86%) of the FMS group and 122 (75%) of the non-FMS sample did so.
Time point 3: Week commencing 1 June 2020.
Participants
FMS group
One hundred and sixty-four people took part (94% of those at Time 2; 5 male, 158 female, 1 other; Mage = 47.43, SD = 11.88, range 21-77). Non-FMS group: One hundred and forty-two people took part (87% of those at Time 2; 41 males, 101 females; Mage = 32.80, SD = 10.18, range 18-57).
Materials and procedures
BBC-SWB (Pontin et al., Citation2013) as described above. FMS group psychological health α = .85, physical health α = .68, relationships α = .81; non-FMS group psychological health α = .87, physical health α = .80, relationships α = .83.
CERQ (Garnefski & Kraaij, Citation2006) as described above. FMS group: self-blame α = .71, acceptance α = .74, rumination α = .62, positive refocussing α = .84, planning α = .69, positive reappraisal α = .74, putting into perspective α = .65, catastrophising α = .70, other-blame α = .85. Non-FMS group: self-blame α = .85, acceptance α = .84, rumination α = .66, positive refocussing α = .82, planning α = .68, positive reappraisal α = .74, putting into perspective α = .71, catastrophising α = .81, other-blame α = .87. Finally, participants reported perceived changes in the severity of their FMS symptoms/general health since time 2 using the same scale as previously.
Statistical analyses
The dataset related to this research is available at https://doi.org/10.5281/zenodo.4399469. All analyses were conducted using IBM SPSS v25. A significant p value was set at α = .05. Descriptive statistics were calculated to determine frequencies, means, and standard deviations of all study variables. We adopted an intention-to-treat approach at time points 2 and 3 such that baseline data was included in analysis for participants who took part at time 1 but dropped out subsequently. This method avoids bias, as attrition may be more frequent in participants with certain characteristics, for instance, particularly severe physical symptoms or poor mental health. ITT also preserves sample size and minimises type 1 error, as results tend to be conservative (Gupta, Citation2011). We combined the three wellbeing scores (physical health, psychological health and relationships) to create an overall mean wellbeing score for each time point. We compared groups on this variable over time using 2 (group) x 3 (time) repeated measures Analysis of Variance (RMANOVA). Finally, three linear regression analyses were computed to examine how much variance in overall wellbeing was accounted for at each time point. Power analysis using GPower software v.3.1.9 suggested a sample size of 120 was required for our analysis. Although attrition occurred between time one and time three, the ITT approach helped to ensure the sample size remained adequate. All analyses controlled for age, sex and socioeconomic status (SES)
Results
presents descriptive statistics for both groups across all three time points. In line with Prediction 1, at Time 1 the FMS group reported higher symptom burden, F (1, 157) = 198.45, p < .001, η2 = .27, and lower overall wellbeing, F (1, 157) = 90.92, p < .001, η2 = .15, compared to the non-FMS group, controlling for age, sex and SES.
Table 1. Descriptive statistics for all measures across three time points.
A 3 (time) x 2 (group) repeated measures Analysis of Variance (ANOVA) on the symptom change data showed significant main effects of group F (1, 517) = 299.01, p < .001, η2 = .37, and a significant two-way interaction between group and time: F (2, 1034) = 6.33, p =.002, η2 = .01. Contrary to Prediction 2, the FMS group showed no significant perception of worsening symptoms over time (p > .70; see also means in ). The non-FMS group reported a significant worsening of symptoms between Times 1 and 2, F (1, 191) = 4.03, p = .05, η2 = .02, though not between Times 2 and 3 (p = .14). They reported stronger perceptions of worsening throughout the study compared to the participants with FMS and the between-group differences were significant at Time 2, (p < .001, η2 = .33) and Time 3 (p < .001, η2 = .27).
A 3 (time) x 2 (group) ANOVA on wellbeing data revealed a significant main effect of group, F (1, 517) = 86.77, p < .001, η2 = .14 (reflecting that wellbeing was lowest for the FMS group throughout) and a significant two-way interaction, F (2, 1034) = 10.33, p < 04 η2 = .01. Simple main effects analysis, showed no significant effects in the non-FMS group (p = .57), but a significant effect of time on wellbeing in the FMS group, F (2, 658) = 4.28, p = .01, η2 = .01. Further post-hoc tests indicated that although wellbeing in FMS did not change significantly between Times 1 and 2 (p = .79) or between Times 2 and 3 (p = .15), over the total time of the study there was a significant overall increase (p = .04, η2 =.01), contrary to Prediction 3.
A 9 (coping strategy) x 3 (time) x 2 (group) ANOVA showed significant main effects of time, F (2, 1084) = 13.62, p < .001, η2 = .03, strategy type, F (8, 4136) = 6.91, p < .001, η2 = .01, and group, F (1, 517) = 5.83, p < .001, η2 = .01. Two-way interactions between time and strategy, F (16, 8272) = 3.49, p < .001, η2 = .01, time and group F (2, 1084) = 24.53, p < .001, η2 = .05, strategy and group, F (8, 4136) = 6.89, p < .001, η2 = .01, were also observed as was a significant three-way interaction, F (16, 8272) = 2.30, p = .002, η2 = .004. illustrates the reported usage of each strategy across time.
Figure 1. A comparison of reported CERQ coping strategy use across three time points.
Cat = catastrophising; rum = rumination; OB = other-blame; SB = self-blame; acc = acceptance; plan = planning; reap = positive reappraisal; ref = positive refocussing; pers = putting into perspective
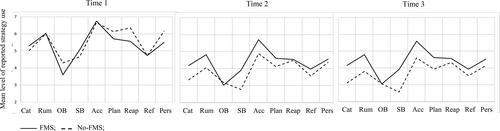
Prediction 4 proposed that the FMS group would use mostly maladaptive strategies however, as shows, the picture is not definitive. At Time 1, the groups reported similar levels of all strategies except for other-blame (p < .001, η2 = .04), planning (p = .01, η2 = .01), positive reappraisal (p < .001, η2 = .04) and putting into perspective (p = .001, η2 = .02) where the FMS group reported lower usage. At Time 2, the FMS group are presenting higher rates of catastrophising (p = .01, η2 = .01), rumination (p = .002, η2 = .02) and self-blame (p = .001, η2 = .02) but also higher acceptance (p = .001, η2 = .02) and positive refocussing (p = .003, η2 = .02). At time 3, participants with FMS again reported higher catastrophising (p < .001, η2 = .02), rumination (p < .001, η2 = .02), self-blame (p < .001, η2 = .03), acceptance (p < .001, η2 = .03), positive refocussing (p = .01, η2 = .01), and also planning (p = .03, η2 = .01). What also illustrates is that reported strategy use declined in both groups after Time 1 and showed barely any change between Times 2 and 3.
Finally, we conducted three linear regressions for each group to examine whether coping strategies could account for variance in wellbeing over and above symptom levels at each time point. We entered age, sex, SES and baseline symptom levels as covariates, together with symptom change (perceptions of improvement/worsening) and coping strategy scores. Results are shown in . For the group with FMS, at all three time points, positive reappraisal and refocussing account for a significant level of variance in wellbeing. The data also suggest negative influences of catastrophising at time 2, and of acceptance at times 2 and 3. For the non-FMS group, reappraisal was also important throughout, with refocussing a significant factor at time 2 and planning at time 3. Other-blame presented a negative effect at time 1, as did catastrophising at time 2.
Table 2. Results of regression on overall wellbeing at three time points.
Discussion
This study aimed to examine the relationship between wellbeing, FMS symptom burden and use of coping strategies during the COVID-19 pandemic lockdown in the UK. Specifically we predicted that a sample with FMS would be experiencing worse health symptoms and wellbeing at baseline, and that these would continue to deteriorate over time, compared to a non-FMS sample. We also expected that participants with FMS would report the use of maladaptive coping strategies and this would account for variance in wellbeing over and above the effects of symptom level. We tested participants at three time points and obtained reports of their coping, wellbeing and changes in symptom severity, compared to a sample of participants with no FMS diagnosis. Firstly, as per Prediction 1, FMS participants reported higher symptom levels and lower wellbeing than controls at Time 1. However, contrary to Prediction 2, participants with FMS reported no significant worsening of symptoms over time, and wellbeing showed a significant increase (contrary to Prediction 3). In contrast, the non-FMS group reported an overall worsening of health symptoms over time and no significant change in wellbeing.
In terms of coping, reported use of the nine CERQ strategies showed a broadly similar trend in both groups, although some differences emerged over time. Prediction 4 had expected participants with FMS to report greater use of maladaptive coping strategies compared to the non-FMS group and at times two and three, this was the case in terms of catastrophising, rumination and self-blame. However, they also reported acceptance and positive refocussing (supposedly adaptive strategies) and at time three, they were additionally reporting higher levels of planning compared to the control group suggesting that by this point they were actively coping and adjusting. At all three time points, adaptive strategies Positive Reappraisal and Refocussing accounted for variance in wellbeing over and above the negative effects of symptoms. These are exactly the type of cognitive behaviours which are suggested to reduce the physiological hyperarousal typical of CSS and thus support symptom management (e.g. Edwards et al., Citation2009; Geenen et al., Citation2012). Overall, contrary to our expectations, these results suggest an association between adoption of certain adaptive cognitive-emotional coping strategies and wellbeing in FMS during the present pandemic and lockdown.
However, as shows, the types of coping strategies reported over time were broadly similar in both groups. Moreover, the non-FMS data also showed significant effects of positive reappraisal on wellbeing throughout the time of the study, and of positive refocussing at times two and three. However, for this group, overall wellbeing remained stable over time while reported health symptoms became worse, suggesting that these strategies may not have been as adaptive for them as for the FMS participants. One possible explanation might lie in how accustomed to lifestyle change the participants were. In dealing with long-term health issues and associated stress, people with FMS have learnt forms of adaptive coping which maintain general wellbeing in ways we may not observe in the general population. If participants with FMS have indeed developed ways of managing the constantly shifting symptom profile typical of the condition, they may be accustomed to focusing on adaption. Conversely, participants in the general population may be more focused on maintaining a sense of normality during lockdown. Recent research by Bacon and Corr (Citation2020) has suggested this may be the aim of coping activities such as hoarding ‘necessities’ and panic buying. The very nature of how the situation was reframed or refcussed may be qualitatively different in people with FMS and this may be reflected in their resilience and ability to cope with their symptoms under stress. Estévez-López et al. (Citation2017) defined five FMS profiles which identify individuals with differing levels of symptomology and resilience. Cognitive behavioural approaches related to helpful thoughts and activities that bring pleasure and satisfaction were shown to be important aspects of resilience. However, there is limited research on resilience in FMS, partly because of the heterogeneity of its symptoms, and complex biopsychosocial underpinnings (Casale et al., Citation2019; Stellar et al., Citation2015). Further research might usefully focus on how coping strategies highlighted as important in the present study are implicated in resilience in the face of stressful events for people with FMS.
Two major factors predict adaptation to change; meaning making and change information (Kwasnicka et al., Citation2016; Van Den Heuvel et al., Citation2013). Adaptation to change is more effective if communications are clear, understandable and timely, and people are most likely to embrace and maintain change if they can clearly see the benefit of it. During the current pandemic, information has not always been perceived as clear and has often changed rapidly as the Government struggled to manage unclear risks while balancing the tension between public health and economic interests. Add to this the prolifery of sometimes inaccurate and contradictory social media information, the so-called COVID-19 infodemic (Mheidly & Fares, Citation2020), it is perhaps unsurprising that some people find difficulty in making meaning and adjusting to changing parameters of behaviour and social norms. One of the reasons we initially predicted that individuals with FMS might adjust poorly was because of increased illness uncertainty and associated Covid-related stressors. In the event, it may be their very familiarity with uncertainty which has benefited them during the pandemic. Conversely, uncertainty, plus the restrictions on working, relationships, etc. are more novel experiences for the non-FMS group and hence potentially more stressful. Uncertainty is known to increase symptom burden and influence the efficacy of coping (Johnson et al., Citation2006) and we suggest this may have affected our non-FMS participants particularly.
One aspect of coping where the two groups clearly appeared to differ was in use of Acceptance and it is important to consider the characteristics of this strategy. The FMS groups reported use of acceptance at times two and three, and it also accounted for independent variance in wellbeing at those times. However, the effects were negative, despite this being a supposedly adaptive way of coping. This finding may not be as anomalous as it seems. Although acceptance was initially conceptualised as adaptive (Garnefski et al., Citation2001), research has suggested that it is often negatively associated with wellbeing and positively associated with psychological distress (Bacon & Charlesford, Citation2018; Jermann et al., Citation2006; Martin & Dahlen, Citation2005). Items that make up the acceptance subscale (e.g., ‘I think that I cannot change anything about it’; ‘I think that I must learn to live with it’) may reflect feelings of hopelessness, or resignation, rather than adjustment. Feliu-Soler et al. (Citation2017) reported similar effects in participants with FMS and concluded that acceptance cannot be considered an adaptive cognitive emotion regulation strategy. Qualitative investigations have highlighted the existence of distinct forms of acceptance (resignation, automatic counteracting and behavioural adapting; Liersch, Citation2020). While behavioural adapting is associated with positive coping, both resignation and automatic counteracting are more synonymous with maladaptive coping. In the present study, any detriment in the FMS group seems to have been offset by the benefits of other adaptive strategies, nevertheless, further investigation into the nature of acceptance in coping would be beneficial.
Limitations
Our data were drawn from self-report measures which may be subject to bias and are correlational in nature, meaning we cannot categorically state a causal relationship between coping and wellbeing. In addition, the participant groups were not formally matched. Although their demographic characteristics were notably similar, the groups did differ significantly in age.
Conclusions
Overall, this study has highlighted some important differences in how people with and without FMS have adapted to life during the pandemic. A strength of the research is that it was conducted over three time points enabling a longitudinal, rather than purely cross-sectional, view. Results suggest that the assumption that individuals with pre-existing health conditions may fare worse during the COVID-19 pandemic may not always hold. Being accustomed to uncertainty, social restrictions, and learning new ways to cope in chronic ill health may build a form of resilience which can support wellbeing in the face of Covid-related challenges. Individuals in good health may be hit harder by new stressors they are emotionally unprepared for, and unused to coping with. A lack of effective treatment options in FMS means there is a need to develop new therapeutic targets to support resilience (Casale et al., Citation2019). Understanding more about how individuals with FMS can adapt in exceptional circumstances, may reveal some useful possibilities.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Adams, L. M., & Turk, D. C. (2015). Psychosocial factors and central sensitivity syndromes. Current Rheumatology Reviews, 11(2), 96–108. https://doi.org/10.2174/1573397111666150619095330
- Adler, N. E., Epel, E. S., Castellazzo, G., & Ickovics, J. R. (2000). Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy, White women. Health Psychology, 19(6), 586–592. https://doi.org/10.1037/0278-6133.19.6.586
- Asmundson, J. G., & Taylor, S. (2020). Coronaphobia revisted: A state-of-the-art on pandemic-related fear, anxiety, and stress. Journal of Anxiety Disorders, 76, 102326. https://doi.org/10.1016/j.janxdis.2020.102326
- Bacon, A. M., & Charlesford, J. J. (2018). Investigating the association between fantasy proneness and emotional distress: the mediating role of cognitive coping strategies. Personality and Individual Differences, 135, 157–165. https://doi.org/10.1016/j.paid.2018.07.003
- Bacon, A. M., & Corr, P. J. (2020). Coronavirus (COVID-19) in the United Kingdom: A personality-based perspective on concerns and intention to self-isolate. British Journal of Health Psychology, 25(4), 839–848. https://doi.org/10.1111/bjhp.12423
- Bueno-Notivol, J., Gracia-García, P., Olaya, B., Lasheras, I., López-Antón, R., & Santabárbara, J. (2021). Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. International Journal of Clinical and Health Psychology, 21(1), 100196. https://doi.org/10.1016/j.ijchp.2020.07.007
- Casale, R., Sarzi-Puttini, P., & Botto, R. (2019). Fibromyalgia and the concept of resilience. Clinical Experimental Rheumatology, 37 (Suppl. 116), S105–S113.
- Chong, M., Wang, W., Hsieh, W., Lee, C., Chiu, N., Yeh, W., Huang, T., Wen, J., & Chen, C. (2004). Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. British Journal of Psychiatry, 185(2), 127–133. doi: https://doi.org/10.1192/bjp.185.2.127
- Creed, F. H., Davies, I., Jackson, J., Littlewood, A., Chew-Graham, C., Tomenson, B., Macfarlane, G., Barsky, A., Katon, W., & McBeth, J. (2012). The epidemiology of multiple somatic symptoms. Journal of Psychosomatic Research, 72(4), 311–317. https://doi.org/10.1016/j.jpsychores.2012.01.009
- Daniels, H., Murray, C., & Murray, T. (2006). Differentiation of self, perceived stress, and symptom severity among patients with fibromyalgia syndrome. Families, Systems, & Health, 24(2), 147–159. https://doi.org/10.1037/1091-7527.24.2.147
- Dell’Osso, L., Carmassi, C., & Consoli, C. (2011). Lifetime posttraumatic stress symptoms are related to the health-related quality of life and severity of pain/fatigue in patients with fibromyalgia. Clinical and Experimental Rheumatology, 29(Suppl. 69), S73–S78.
- Di Tella, M., Ghiggia, A., Tesio, V., Romeo, A., Colonna, F., Fusaro, E., Torta, R., & Castelli, L. (2017). Pain experience in fibromyalgia syndrome: The role of alexithymia and psychological distress. Journal of Affective Disorders, 208, 87–93. https://doi.org/10.1016/j.jad.2016.08.080
- Droit-Volet, S., Sandrine, G. I. L., Martinelli, N., Andant, N., Clinchamps, M., Parreira, L., … Pereira, B. (2020). Time and Covid-19 stress in the lockdown situation: Time free, dying of boredom and sadness. PLoS ONE, 15(8), e0236465. https://doi.org/10.31234/osf.io/efdq5
- Edwards, R. R., Campbell, C., Jamison, R. N., & Wiech, K. (2009). The neurobiological underpinnings of coping with pain. Current Directions in Psychological Science, 18(4), 237–241. https://doi.org/10.1111/j.1467-8721.2009.01643.x
- Estévez-López, F., Segura-Jiménez, V., Álvarez-Gallardo, I. C., Borges-Cosic, M., Pulido-Martos, M., Carbonell-Baeza, A., Aparicio, V. A., Geenen, R., & Delgado-Fernández, M. (2017). Adaptation profiles comprising objective and subjective measures in fibromyalgia: The al-Ándalus project. Rheumatology (Oxford, England), 56(11), 2015–2024. https://doi.org/10.1093/rheumatology/kex302
- Feliu-Soler, A., Reche, E., Borràs, X., Pérez-Aranda, A., Andrés-Rodríguez, L., Peñarrubia-María, M., Navarro-Gil, M., García-Campayo, J., Bellón, J., & Lucian O, J. V. (2017). Psychometric properties of the Cognitive Emotion Regulation Questionnaire (CERQ) in patients with fibromyalgia syndrome. Frontiers Psychology, 8, 2075. https://doi.org/10.3389/fpsyg.2017.02075
- Galves-Sanchez, C. M., Reyes del Paso, G. A., & Duschek, S. (2018). cognitive impairments in fibromyalgia syndrome: Associations with positive and negative affect, alexithymia, pain catastrophizing and self-esteem. Frontiers Psychology, 22, 377. https://doi.org/10.3389/fpsyg.2018.00377
- Garnefski, N., & Kraaij, V. (2006). Cognitive emotion regulation questionnaire – Development of a short 18-item version (CERQ-short). Personality and Individual Differences, 41(6), 1045–1053. https://doi.org/10.1016/j.paid.2006.04.010
- Garnefski, N., & Kraaij, V. (2012). Cognitive coping and goal adjustment are associated with symptoms of depression and anxiety in people with acquired hearing loss. International Journal of Audiology, 51(7), 545–550.
- Garnefski, N., Kraaij, V., Benoist, M., Bout, Z., Karels, E., & Smit, A. (2013). Effect of a cognitive behavioral self-help intervention on depression, anxiety, and coping self-efficacy in people with rheumatic disease. Arthritis Care & Research, 65(7), 1077–1084.
- Garnefski, N., Kraaij, V., & Spinhoven, P. (2001). Negative life events, cognitive emotion regulation and emotional problems. Personality and Individual Differences, 30(8), 1311–1327. https://doi.org/10.1016/S0191-8869(00)00113-6
- Garnefski, N., Kraaij, V., & Spinhoven, P. (2002). Manual for the use of the cognitive emotion regulation questionnaire. DATEC.
- Geneen, L. J., Martin, D. J., Adams, N., Clarke, C., Dunbar, M., Jones, D., McNamee, P., Schofield, P., & Smith, B. H. (2015). Effects of education to facilitate knowledge about chronic pain for adults: A systematic review with meta-analysis. Systematic Reviews, 4, 132. https://doi.org/10.1186/s13643-015-0120-5
- Geenen, R., van Ooijen-van der Linden, L., Lumley, M. A., Bijlsma, J. W. J., & van Middendorp, H. (2012). The match-mismatch model of emotion processing styles and emotion regulation strategies in fibromyalgia. Journal of Psychosomatic Research, 72(1), 45–50. https://doi.org/10.1016/j.jpsychores.2011.09.004
- Griep, E. N., Boersma, J. W., & De Kloet, E. R. (1993). Altered reactivity of the hypothalamic-pituitary-adrenal axis in the primary fibromyalgia syndrome. The Journal of Rheumatology, 20(3), 469–474.
- Gupta, S. K. (2011). Intention-to-treat concept: A review. Perspectives in Clinical Research, 2(3), 109–112. https://doi.org/10.4103/2229-3485.83221
- Houdenhove, B., & Luyten, P. (2007). Fibromyalgia and related syndromes characterized by stress intolerance and pain hypersensitivity: Do we need a new nosology? Current Rheumatology Reviews, 3(4), 304–308. https://doi.org/10.2174/157339707782408937
- Hyland, M. E., Bacon, A. M., Lanario, J. W., & Davies, A. F. (2019). Symptom frequency and development of a generic functional disorder symptom scale suitable for use in studies of patients with irritable bowel syndrome, fibromyalgia syndrome or chronic fatigue syndrome. Chronic Diseases and Translational Medicine, 5(2), 129–138. https://doi.org/10.1016/j.cdtm.2019.05.003
- Jermann, F., Van der Linden, M., d’Acremont, M., & Zermatten, A. (2006). Cognitive emotion regulation questionnaire (CERQ). European Journal of Psychological Assessment, 22(2), 126–131. https://doi.org/10.1027/1015-5759.22.2.126
- Johnson, L. M., Zautra, A. J., & Davis, M. C. (2006). The role of illness uncertainty on coping with fibromyalgia symptoms. Health Psychology : official Journal of the Division of Health Psychology, American Psychological Association, 25(6), 696–703.https://doi.org/10.1037/0278-6133.25.6.696
- Kang, M., Choi, Y., Kim, J., Lee, K. O., Lee, S., Park, I. K., Park, J., & Seo, I. (2020). COVID-19 impact on city and region: What’s next after lockdown? International Journal of Urban Sciences, 24(3), 297–315. https://doi.org/10.1080/12265934.2020.1803107
- Kraaij, V., & Garnefski, N. (2015). Cognitive, behavioral and goal adjustment coping and depressive symptoms in young people with diabetes: A search for intervention targets for coping skills training. Journal of Clinical Psychology in Medical Settings, 22(1), 45–53.
- Kwasnicka, D., Dombrowski, S. U., White, A., & Sniehotta, F. (2016). Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychology Review, 10(3), 277–296. https://doi.org/10.1080/17437199.2016.1151372
- Liersch, U. (2020). Chronic pain acceptance does not equal accepting chronic pain. The Psychologist, 12, 42–45.
- Light, K. C., Bragdon, E. E., Grewen, K. M., Brownley, K. A., Girdler, S. S., & Maixner, W. (2009). Adrenergic dysregulation and pain with and without acute beta-blockade in women with fibromyalgia and temporomandibular disorder. The Journal of Pain, 10(5), 542–552. https://doi.org/10.1016/j.jpain.2008.12.006
- Malfliet, A., Coppieters, I., Van Wilgen, P., Kregel, J., De Pauw, R., Dolphens, M., & Ickmans, K. (2017). Brain changes associated with cognitive and emotional factors in chronic pain: a systematic review. European Journal of Pain (London, England), 21(5), 769–786. https://doi.org/10.1002/ejp.1003
- Marangell, L. B., Clauw, D. J., Choy, E., Wang, F., Shoemaker, S., Bradley, L., Mease, P., & Wohlreich, M. M. (2011). Comparative pain and mood effects in patients with comorbid fibromyalgia and major depressive disorder: Secondary analyses of four pooled randomized controlled trials of duloxetine. Pain, 152(1), 31–37. https://doi.org/10.1016/j.pain.2010.05.029
- Martin, R. C., & Dahlen, E. R. (2005). Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences, 39(7), 1249–1260. https://doi.org/10.1016/j.paid.2005.06.004
- Martinez-Lavin, M. (2007). Biology and therapy of fibromyalgia. Stress, the stress response system, and fibromyalgia. Arthritis Research & Therapy, 9(4), 216. https://doi.org/10.1186/ar2146
- Mheidly, N., & Fares, J. (2020). Leveraging media and health communication strategies to overcome the COVID-19 infodemic. Journal of Public Health Policy, 41(4), 410–420. https://doi.org/10.1057/s41271-020-00247-w
- Mishel, M. H. (1999). Uncertainty in chronic illness. Annual Review of Nursing Research, 17(1), 269–294. https://doi.org/10.1891/0739-6686.17.1.269
- NHS (2020). Advice for everyone Coronavirus (COVID19). https://www.nhs.uk/conditions/coronavirus-covid-19/
- Pontin, E., Schwannauer, M., Tai, S., & Kinderman, P. (2013). A UK validation of a general measure of subjective well-being: the modified BBC subjective well-being scale (BBC-SWB). Health and Quality of Life Outcomes, 11, 150–159. http://www.hqlo.com/content/11/1/150.
- Public Health England (2020). Number of coronavirus (COVID-19) cases and risk in the UK. https://www.gov.uk/guidance/coronavirus-covid-19-information-for-the-public
- Reich, J. W., Olmsted, M. E., & Van Puymbroeck, C. M. (2006). Illness uncertainty, partner caregiver burden and support, and relationship satisfaction in fibromyalgia and osteoarthritis patients. Arthritis and Rheumatism, 55(1), 86–93. https://doi.org/10.1002/art.21700
- Rubin, G. J., & Wessely, S. (2020). The psychological effects of quarantining a city. BMJ (Clinical Research ed.), 368, 313. https://doi.org/10.1136/bmj.m313
- Sluka, K. A., & Clauw, D. J. (2016). Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience, 338, 114–129. https://doi.org/10.1016/j.neuroscience.2016.06.006
- Spaeth, M. (2009). Epidemiology, costs, and the economic burden of fibromyalgia. Arthritis Research & Therapy, 11(3), 117. https://doi.org/10.1186/ar2715
- Stellar, J. E., John-Henderson, N., Anderson, C., L., Gordon, A. M., McNeil, G. D., & Keltner, D. (2015). Positive affect and markers of inflammation: Discrete positive emotions predict lower levels of inflammatory cytokines. Emotion (Washington, D.C.), 15(2), 129–133. https://doi.org/10.1037/emo0000033
- Taylor, S. (2019). The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing.
- Thieme, K., Turk, D. C., & Flor, H. (2004). Comorbid depression and anxiety in fibromyalgia syndrome: Relationship to somatic and psychosocial variables. Psychosomatic Medicine, 66(6), 837–844. https://doi.org/10.1097/01.psy.0000146329.63158.40
- Turk, D. C., & Monarch, E. S. (2018). Biopsychosocial perspective on chronic pain. In D. C. Turk & R. J. Gatchel (Eds.), Psychological approaches to pain management: A practitioner’s handbook (p. 3–24). The Guilford Press.
- Van Den Heuvel, M., Demerouti, E., Bakker, A. B., & Schaufeli, W. B. (2013). Adapting to change: The value of change information and meaning making. Journal of Vocational Behavior, 83(1), 11–21. https://doi.org/10.1016/j.jvb.2013.02.004
- Wang, Y., Di, Y., Ye, J., & Wei, W. (2021). Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychology, Health & Medicine, 26(1), 13–22. https://doi.org/10.1080/13548506.2020.1746817
- Wheaton, M. G., Abramowitz, J. S., Berman, N. C., Fabricant, L. E., & Olatunji, B. O. (2012). Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research, 36(3), 210–218. https://doi.org/10.1007/s10608-011-9353-3
- Woda, A., Picard, P., & Dutheil, F. (2016). Dysfunctional stress responses in chronic pain. Psychoneuroendocrinology, 71, 127–135. https://doi.org/10.1016/j.psyneuen.2016.05.017
- Woods, A. T., Velasco, C., Levitan, C. A., Wan, X., & Spence, C. (2015). Conducting perception research over the internet: A tutorial review. PeerJ., 3, e1058. https://doi.org/10.7717/peerj.1058
- World Health Organization (2020). Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
- Wu, P., Fang, Y., Guan, Z., Fan, B., Kong, J., Yao, Z., Liu, X., Fuller, C. J., Susser, E., Lu, J., & Hoven, C. W. (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 54(5), 302–311.
