?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
Understanding the impact of the COVID-19 pandemic on mental health and the psychological factors associated can help inform subsequent interventions to protect psychological health. In particular, psychological flexibility has been shown to be an important target for intervention. The current study aimed to investigate associations between protective factors (state mindfulness, values and self-compassion) and risk factors (COVID-19 stress, worry and rumination) for mental health during the early stages of the COVID-19 pandemic.
Design
439 participants completed three online surveys during the 1st wave of the pandemic in the UK: Time 1 (April 1–5th 2020), Time 2 (April 15–19th April), Time 3 (May 13–17th 2020).
Main outcome measures
Measures of wellbeing, burnout and life satisfaction.
Results
Psychological health outcome measures were found to be lower (worse) than normative comparison data during the early stages of the UK lockdown, while COVID-19 stress and worry reduced over time. Multilevel models found that higher levels of trait and state measures of psychological flexibility and self-compassion were associated with better psychological health across time points. Higher levels of COVID-19 stress, worry and rumination were also associated with poorer psychological health.
Conclusion
The results showed that mindfulness, values and self-compassion are potential targets for intervention.
Introduction
Public health emergencies are a substantial threat to healthcare systems and the health and wellbeing of both patients and the general public (Quinn, Citation2008). In January 2020, a novel coronavirus outbreak spread from China to more than 215 other countries, including the United Kingdom (UK). The novel coronavirus was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), while the disease associated with it was named COVID-19 (Ciotti et al., Citation2020). COVID-19 has brought significant changes and serious challenges to mental and physical health worldwide (e.g. COVID fatigue, long COVID, changes to job roles, hours and redeployment, bereavements at scale) (Holmes et al., Citation2020; O’Connor et al., Citation2020a; Xiong et al., Citation2020). Moreover, recent reports in the UK suggest that one in three NHS staff suffered mental health issues related to the pandemic (Al-Ghunaim et al., Citation2021; Cullen et al., Citation2020; Pfefferbaum et al., 2020).
The emerging psychological evidence on COVID-19 has mainly focussed on understanding the negative effects of the pandemic on psychological health (e.g. Fullana et al., Citation2020; Li et al., Citation2020; Wang et al., Citation2020). These studies confirmed data from previous infectious diseases (e.g. Brooks et al., Citation2020), showing that public health measures such as isolation, quarantine and community containment are effective in slowing down the spread of the disease (Wilder-Smith & Freedman, Citation2020). However, restrictive measures are also likely to give rise to poorer mental health (e.g. Cheng & Tang, Citation2004; García-Fernández et al., Citation2020; Holmes et al., Citation2020; O’Connor et al., Citation2020a; O’Connor et al., Citation2020b; Wang et al., Citation2020; Xiong et al., Citation2020; Yu et al., Citation2005) especially in healthcare professionals (e.g. Al-Ghunaim et al., Citation2021; Cartwright & Thompson, Citation2020; Kadhum et al., Citation2020; Kannampallil et al., Citation2020; Khalafallah et al., Citation2020; Salazar de Pablo et al., Citation2020; Wu et al., Citation2020).
During the COVID-19 pandemic, behavioural scientists and psychologists have played an important role in advising governments on how to implement lockdown and social distancing measures (Chater et al., Citation2021; O’Connor et al., Citation2020a). However, as argued by O’Connor and colleagues (Citation2020a) in their COVID-19 psychological research priorities position paper, there was an urgent need for further evidence that informs governments and policies not only about the effects of the COVID-19 pandemic on the health and wellbeing of populations but also on the psychological factors that may be associated with increased wellbeing and life satisfaction during the pandemic. Indeed, whilst a large amount of the emerging evidence has focussed on understanding the negative effects of the pandemic on psychological health, less has investigated which psychological factors may protect or confer resilience (Xiong et al., Citation2020, for a review). One such factor is psychological flexibility.
Psychological flexibility can be defined as ‘the capacity to persist or to change behaviour in a way that includes conscious and open contact with thoughts and feelings, appreciates what the situation affords, and is guided by one’s goals and values’ (McCracken & Morley, Citation2014, p. 8). As may be apparent in this definition, psychological flexibility is a broad process that is often considered to include several sub-processes, such as: values, knowing and doing activities that enrich one’s life; mindfulness, awareness of the present moment; and, self-compassion, approaching oneself with kindness and acceptance.
Recent studies have shown that at times of great difficulty, such as wars (Tol et al., Citation2020), school shootings, devastating storms, or violent crime (e.g. Brockman et al., Citation2016; Gold & Marx Citation2007; Kumpula et al., Citation2011), higher psychological flexibility can help people function effectively even when experiencing strong emotions such as fear and anxiety. Presti et al. (Citation2020) have argued that psychological flexibility skills can help individuals cope with understandable anxious and fearful responses that were often apparent in the early stages of the pandemic. For example, in an uncertain situation, such as the early days of the COVID-19 outbreak, a normal and common response included getting caught up in our thoughts and fears about what could happen—to worry and ruminate. However, being able to catch ourselves unhelpfully getting caught up in our thoughts, and instead choosing to bring our attention into the present moment, to who or what is in front of us (mindfulness), with a stance of self-kindness (self-compassion) may help people maintain engagement in activities they find meaningful (values).
In support of this, a small number of cross-sectional studies have investigated the relationship between psychological flexibility and the negative effects of mental health during the COVID-19 pandemic. For example, Landi and colleagues (2020) assessed psychological flexibility, trait health anxiety, COVID-19 distress, anxiety, and depression in Italian adults. Results from this study showed that overall psychological flexibility was associated with reduced negative effects of trait health anxiety during the nationwide lockdown. In another study in Italian adults, four sub-processes of psychological flexibility (self-as context, defusion, values, committed action), were found to be positively associated with mental health (Pakenham et al., Citation2020). In a study of UK residents (Dawson & Golijani-Moghaddam, Citation2020), overall psychological flexibility was positively related to wellbeing and negatively associated with depression, anxiety, COVID-19 stress and worry.
To the best of our knowledge, no studies have longitudinally examined the specific psychological flexibility processes that may help mitigate the rising levels of mental ill-health as a result of COVID-19 (Cullen et al., Citation2020) and there has been an over-reliance on cross-sectional methodologies. A longitudinal assessment and investigation with alternative methods (e.g. multilevel modelling) may offer a deeper understanding of whether psychological flexibility can lessen the detrimental effects of COVID-19 on psychological health.
The current study
The early stages of the pandemic represented a novel context—that included sudden and unknown risks to health, local and international lockdowns, mass movement to home-working, bereavements and social isolation (e.g. Holmes et al., Citation2020; O’Connor et al., 2020). By employing a multilevel modelling approach with longitudinal data collected across three time-points during the first wave of the COVID-19 pandemic, we aimed to assess whether specific components of psychological flexibility were differentially predictive of wellbeing. Unlike other studies conducted during the pandemic, we have included three reasonably distinct components within these analyses (i.e. state mindfulness, values and self-compassion).
Given the robustness of psychological flexibility as a construct and promoter of psychological health (Kashdan & Rottenberg, Citation2010 for a review), in this study, we hypothesised that dispositional psychological flexibility may help individuals face the challenging environments driven by the pandemic and be associated with more adaptive responses to the COVID-19 related stressors people experienced during the early stages of the crisis. We hypothesised that individuals with greater dispositional psychological flexibility may have had more internal personal resources to deal with emotions, anxiety or stress when COVID-19 related stressors arose. Furthermore, given that how one tends to respond to challenging situations may differ from how one responds to novel challenges (as with the pandemic), we anticipated that state-level psychological flexibility (how one is behaving now) could differ from trait-level psychological flexibility (how one tends to behave), and we expected that both state and trait-level variables would also show significant positive relationships with mental health. In this study if, as hypothesised, psychological factors (mindfulness, values, self-compassion) have a positive influence on facilitating better psychological health and mitigate the negative effects of lockdown, targeting these factors that are modifiable by an intervention can inform and determine what psychological support is available throughout the pandemic, especially for the most vulnerable (immediate action). This study will also help inform interventions to protect mental wellbeing, including frontline staff, in the post-COVID-19 pandemic (long-term action).
Given the aforementioned theoretical position of psychological flexibility as a means to function well in the context of a stressful situation that includes uncertainty and lends itself to worry and rumination, we expected that psychological flexibility would be an important predictor of mental health in addition to worry and rumination regarding the specifics of COVID-19.
Lastly, we theorised that individuals with higher dispositional psychological flexibility would be better equipped to deal with challenging situations in stressful environments and also be better able to respond more mindfully and according to one’s values and goals regardless of the stressors they may experience. Given the multiple COVID-19 contextual factors that may have occurred during the early stages of the pandemic, the association between how one tends to behave (dispositional psychological flexibility) and how one behaves (state psychological flexibility) may not be direct and, thus, needs further exploration. Therefore, we sought to assess whether dispositional characteristics of psychological flexibility were associated with state-level psychological flexibility during the early stages of the COVID-19 pandemic.
Therefore, in summary, we set out to explore the following aims and hypotheses.
Preregistered primary aims
To investigate the association between state mindfulness, values and self-compassion and psychological health during COVID-19 pandemic, and test whether these relationships are moderated by trait mindfulness, values and self-compassion.
To examine whether trait mindfulness, values, and self-compassion are associated with better psychological health during the COVID-19 pandemic.
To examine whether higher levels of COVID-19 stress, worry and rumination are associated with poorer psychological health during COVID-19 pandemic.
To examine whether trait mindfulness, values and self-compassion are associated with state mindfulness, values and self-compassion during COVID-19 pandemic.
Hypotheses
Informed by these aims, the following hypotheses were tested:
Higher levels of state mindfulness, values and self-compassion will be associated with better psychological health during the early stages of the COVID-19 pandemic and these relationships will be moderated by trait mindfulness, values and self-compassion (such that, the relationships will be stronger in individuals higher on these traits).
Higher levels of trait mindfulness, values and self-compassion will be associated with better psychological health during the early stages of the COVID-19 pandemic.
Higher levels of COVID-19 stress, worry and rumination will be associated with poorer psychological health during the early stages of the COVID-19 pandemic.
Higher levels of trait mindfulness, values and self-compassion will be associated with higher levels of state mindfulness, values and self-compassion.
Method
Ethics and preregistration
This study received ethical approval (reference number: PSYC-23) from the School of Psychology (University of Leeds) Ethics Committee. The hypotheses for this study were preregistered at AsPredicted (URL: https://aspredicted.org/blind.php?x=xh9es6). The data were collected prior to preregistration, however, importantly, preregistration was completed before the research team viewed the data and the analysis commenced.
Participants
Participants were recruited through advertisements on Prolific, social media (e.g. Twitter, Facebook) and a university participant pool lists. Eligible participants were identified if they satisfied the general inclusion criteria—UK residents, fluent in English language and aged over 18 years old.
Five hundred and fifty-seven participants agreed to take part in this study. However, four hundred and thirty-nine participants returned questionnaires at three time-points. In this study we took a pragmatic approach and only included participants who returned questionnaires for all three time-points (n = 439). Participants were aged between 18 and 75 years-old (M = 35.05; SD = 13.65) and consisted of 346 females (78.8%) and 93 males (21.2%). 77 (17.54%) participants were healthcare professionals, and of these 62 (80.52%) were NHS workers. 18% of the participants were employed in a professional occupation, 11.7% were technicians and 20.6% were students. 15.2% of the participants were retired or unemployed because of COVID-19 at the start of the pandemic. 10.9% of the sample declared to have lost their jobs at the start of the pandemic (two weeks after the start of the lockdown), 16.2% to have had a pay cut, and 0.7% declared to be still working but with a pay cut. The sample consisted predominantly of White British (91.3%).
Design
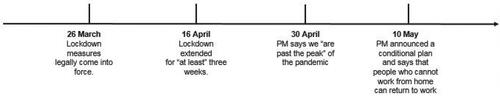
Longitudinal questionnaire study with measures taken at three time-point measurements (see for details of the government restrictions in place) during the 1st wave of COVID-19 pandemic: T1 (April 1st–5th 2020), T2 (April 15th–19th April) and T3 (May 13th–17th 2020). This study employed an intensive repeated-measures design during the early stages of the UK lockdown in order to allow us to examine changes during this time window.
Procedure
Participants who were interested in the study were given an online participant information sheet which outlined the nature of the study. Interested participants also received a consent form, with a link and the baseline survey to complete. Participants who wished to take part in the study were asked to return an online pre-survey that asked to confirm if they were over 18 year-old and reside in the UK. Participants returned a total of three surveys. All of the surveys were administered using the Online Surveys platform, with the anonymous data stored in the Online surveys servers in accordance with GDPR governance. Participants who completed the study were then debriefed and given a chance of winning £100 Amazon voucher upon completion of the study. Psychological health was measured with three questionnaires capturing wellbeing, life satisfaction and burnout.
Measures
Wellbeing
A brief seven-item self-report inventory scale, The Warwick-Edinburgh Mental Wellbeing scale (Tennant et al., Citation2007), was used to assess wellbeing in the general population (e.g. ‘Over the past two weeks have you been feeling optimistic about the future?’). Items were rated on a scale that extended from 1 (none of the time) to 5 (all of the time). Raw scores were then converted to metric scores, as published in Stewart-Brown et al. (Citation2009), to allow for comparisons with previous studies. This scale showed good content validity with a Cronbach’s alpha score of 0.89 (student sample) and 0.91 (population sample) (Clarke et al., Citation2011; Stewart-Brown et al., Citation2009; Tennant et al., Citation2007). Cronbach’s alphas for the summed scale in the current study were .84 for the first survey, .86 for the second survey and .86 for the third survey.
Life satisfaction
One item was used ‘How satisfied are you with your life today?’ ranging from 0 (not at all satisfied) to 10 (extremely satisfied) (Hegarty et al., Citation2019). This single item measure has been shown to be reliable and valid (Hegarty et al., Citation2019).
Burnout
A brief 10-item scale was employed to assess job burnout, the Burnout Measure Short version (BMS) (Malach-Pines, Citation2005). Participants were asked to rate how often they felt tired or disappointed with others (e.g. ‘During the past two weeks, when thinking about your work overall, how often have you felt tired or disappointed with people?’) for example, and to rate how often they felt burnout from 1 (never) to 7 (always). The scale demonstrates good internal consistency (α = 0.86; Malach-Pines, Citation2005). Cronbach’s alphas for the summed scale in the current study were .90 for the first survey, .93 for the second survey and .94 for the third survey.
Trait measures of mindfulness, values and self-compassion were only assessed by participants in the first survey.
Trait mindfulness
A brief 15-item scale, the 15-item Five Facet Mindfulness Questionnaire (Gu et al., Citation2016), was employed to assess trait mindfulness (e.g. ‘I pay attention to sensations, such as the wind in my hair and the sun in on my face’). Items were rated on a scale that extended from 1 (never true) to 5 (always true). This scale is composed of 5 subscales that assess different aspects of mindfulness; observing, describing, acting with awareness, non-judging of experience and non-reactivity to difficult inner experience. The factor structure of this scale is consistent with the longer version (FFMQ-39) and has good internal consistency across a range of samples (.72–.92, Gu et al., Citation2016; Baer et al., Citation2006, Citation2008). Cronbach’s alpha for the scale was .77 in the current study.
Trait values
Trait values were assessed with an adapted version of the Chronic Pain Values Inventory (CPVI; McCracken & Yang, Citation2006) published in Hegarty et al. (Citation2019). Participants were asked to rate how important a series of values were for them such as health, family and friends, and work (e.g. ‘How important are family and friendship, work or health and self-care for you?’) on a scale from 0 (not at all) to 10 (extremely important)). The CPVI demonstrates very good internal consistency (Cronbach’s alpha = .82, McCracken & Yang, Citation2006; Hegarty et al., Citation2019). Cronbach’s alpha for the scale was .68 in the current study.
Trait self-compassion
State self-compassion was assessed with the 12-item Self-Compassion Scale (Raes et al., Citation2011). This measure captures the dispositional ability to treat oneself with kindness and compassion (e.g. ‘I try to be understanding and patient towards those aspects of my personality I don’t like’). Items were rated on a scale that extended from 1 (almost never) to 5 (almost always). The scale demonstrates high internal consistency (α ≥ 0.86, Hayes et al., Citation2016; Raes et al., Citation2011). Cronbach’s alpha for the scale was .89 in the current study.
Participants completed state measures of mindfulness, values and self-compassion at three time-points.
State mindfulness
Participants rated state mindfulness by completing an adapted version of the Mindful Attention Awareness Scale (MAAS; Brown & Ryan, Citation2003). In this study, this scale captured the present-to-present awareness experience over the past two weeks (e.g. ‘During the past two weeks, I found it difficult to stay focused on what was happening in the present’. Items were rated on a scale that extended from 0 (extremely) to 6 (not at all)). The scale demonstrates good internal consistency (α ≥ 0.86, Brown & Ryan, Citation2003). Cronbach’s alphas for the scales were .86 for the first survey, .91 for the second survey and .91 for the third survey.
State values
The engagement with personal values was rated on a three-item scale which was an adapted version of the Chronic Pain Values Inventory (CPVI; McCracken & Yang, Citation2006). Participants rated how engaged they were with their values (e.g. ‘During the past two weeks, how successful have you been living according to your values?’) on a scale from 0 (not at all engaged) to 10 (extremely engaged)). The CPVI demonstrates very good internal consistency (Cronbach’s alpha = .82, McCracken & Yang, Citation2006). Cronbach’s alphas for the scales were .68 for the first survey, .67 for the second survey and .67 for the third survey.
State self-compassion
State self-compassion was assessed with an adapted version of the 12-item Self-Compassion Scale (Neff et al., Citation2021). This measure captured the ability to treat oneself with kindness and compassion (e.g. ‘During the past two weeks, I have tried to be kind and reassuring to myself’). Items were rated on a scale that extended from 1 (almost never) to 5 (almost always). The scale demonstrates good internal consistency (Cronbach’s alpha = 0.86 in all samples, Neff et al., Citation2021). Cronbach’s alphas for the scales were .83 for the first survey, .80 for the second survey and .82 for the third survey.
COVID-19 stress, worry and rumination
COVID-19 related factors were assessed by investigating COVID-19 related stress, worry and rumination during the pandemic. To assess COVID-19 stress, the participants were asked ‘In the past two weeks, to what extent has life become more stressful, difficult or upsetting because of the COVID-19 outbreak?’ on a scale from 0 (not at all stressful, bothersome, upsetting) to 7 (very stressful, bothersome, upsetting). COVID-related rumination and worry were assessed using single item measures rated on a scale of 1 (never) to 7 (very often) informed by previous research (e.g. Clancy et al., Citation2020c, Citation2016). Worry was first defined as: ‘Negative, repetitive thoughts about future events which have the potential to be stressful or upsetting. These worrisome thoughts are usually distressing, can be difficult to control and can lead to a spiral of different worries’. Then participants were asked ‘Over the last two weeks, how often did you worry or focus on COVID-19-related things that may occur or happen in the future?’ and invited to respond on a scale from 0 (never) to 7 (often). Rumination was defined as: ‘Negative, repetitive thoughts about upsetting emotions or events which have happened in the past (including today). These ruminative thoughts are usually distressing, can be difficult to control and can lead to a spiral of different ruminations’. Then participants were asked: ‘Over the last two weeks, how often did you ruminate over COVID-19-related things that have happened to you, or upset you in the past?’ on a scale from 0 (never) to 7 (often). Single item measures of stress, rumination and worry have been used successfully in previous research and have been shown to be reliable and valid (Clancy et al., CitationCitation2020a; O’Connor & Ferguson, Citation2016; Zoccola et al., Citation2011).
Other measures
A demographics questionnaire asked questions about participants’ age, gender, occupation, job loss, keyworker status, healthcare professional or not.
Data analysis
Preliminary analyses were conducted to explore data distributions and missingness. Outliers were visually assessed by computing boxplots. Little’s missing completely at random (MCAR) test was performed to explore whether data were missing completely at random. Simple imputation by using variable mean substitution was employed to replace missing data. For level 2 (baseline measures) data, Little’s MCAR test showed that the data were missing completely at random (X2 = 35.370, df = 27, p >.05). For level 1 data, Little’s MCAR test showed that the data were also missing completely at random (X2 = 60.348, df = 181, p > .05). Because Little’s test showed the data were missing at random, it was decided that dealing with the missing data by column and person means was acceptable and pragmatic.
Multilevel modelling analyses were employed using hierarchical linear modelling software (HLM version 7) (Raudenbush et al., Citation2011). HLM allows for analyses of both within and between-person processes. Multilevel modelling was chosen as the preferred statistical method of analysis as the data under consideration were hierarchical in nature and had two levels. Level 1 capturing the within-person relations between the time-point variables (e.g. state mindfulness, values and self-compassion and each of the psychological health outcomes) and level 2 capturing the between-person variability in the trait variables (trait mindfulness, self-compassion and values). Moreover the multilevel modelling approach allows the researcher to examine whether within-person level 1 slopes (or relationships) are moderated by the between-person level 2 variables in the same model. More generally, multilevel modelling helps to avoid making erroneous conclusions based on the ecological fallacy—the inappropriate assumption that relationships at one level in a hierarchy apply at another (see Kreft & De Leeuw, Citation2006 for further discussion). In the current study, level 1 variables (state measure of stress, worry, rumination, wellbeing, burnout, mindfulness, values, and self-compassion) were group mean centred. Level 2 variables (trait mindfulness, trait values, trait self-compassion) were grand mean centred. Note that for the burnout analyses we only included participants who were currently at work (375 out of 439).
Following calculating the descriptive statistics, we investigated whether there were any significant changes in the main study variables using repeated measures ANOVAs with Time as the within-subjects factor. The main analyses were conducted using HLM version 7.0. In order to reduce the number of comparisons and to be parsimonious, the first and second hypotheses were tested in the same models. First, we tested whether the state measures of mindfulness, values and self-compassion were associated with each of psychological health outcome measures (wellbeing, life satisfaction, and burnout) across the time points by examining the level 1 within-participant slopes (H1). The trait measures of mindfulness, values and self-compassion were also included as level 2 variables in each of these models in order to examine their cross-level effects on each of the outcomes (H2). Therefore, the general form for the cross-level HLM model for each of the outcomes variables was:
Outcome variables (e.g. wellbeing, life satisfaction, burnout) =
For the third hypothesis, we tested whether COVID-19 stress, worry and rumination were associated with each of the psychological health outcome measures (wellbeing, life satisfaction, and burnout) across the time points by examining the level 1 within-participant slopes (H3). The general form for the cross-level HLM model for each of the outcomes variables was:
For the fourth hypothesis, we examined whether the trait mindfulness, values and self-compassion measures had cross-level associations with the state measures of mindfulness, values and self-compassion.
The general form for the cross-level HLM model for each of the outcomes variables was:
Results
Descriptive statistics
Descriptive statistics for the main study outcomes and psychological flexibility variables are presented in . Overall, at the start of the pandemic, the level of positive wellbeing reported by participants at T1 fell in the bottom 20% of responses meaning that wellbeing levels at T1 were low by comparison with comparable UK normative data (M = 23.60; SD = .05) available for the Warwick-Edinburgh Mental Wellbeing scale (pre-pandemic). Life satisfaction (4.54/10) was lower compared to the mean average for the UK population in 2019 (6.8/10; Helliwell et al., Citation2019) and levels declined from T1 to T3. Overall burnout levels were low and were not markedly different by comparison to relevant normative data (Malach-Pines, Citation2005). Inspection of also reveals that COVID stress, rumination and worry levels appeared to decrease throughout the six-week assessment period.
Table 1. Means, standard deviations for main study variables.
Repeated measures ANOVAs with a Greenhouse-Geisser correction were performed to explore whether these changes in psychological health (wellbeing, life satisfaction, and burnout), COVID-19 stress, worry and rumination (see and and ) were statistically significant. From T1 to T3 there was a significant effect of Time on life satisfaction, F (1.913, 837.837) = 262.727, p = <.001, partial η2 = .38, COVID-19 worry, F (1.975, 865.170) = 76.133 p = <.001, partial η2 = .15, and COVID-19 stress, F (1.908, 839.195) = 58.145 p = <.001, partial η2=.12. From T1 to T3, participants reported a significant decrease in COVID-19 stress, COVID-19 worry and life satisfaction. Wellbeing, F (1.902, 833.140) = .698 p = .491, partial η2 = .00, burnout, F (1.69, 630.57) = .71 p = .47, partial η2 = .00, and COVID-19 rumination, F (1.978, 866.532) = 2.349 p = .10 partial η2 = .01, did not change throughout the lockdown.
Figure 2. Levels of wellbeing, life satisfaction and burnout at Time 1 (April 1–5th 2020), Time 2 (April 15–19th, 2020) and Time 3 (May 13–17th 2020) with published norms for comparison. Error bars represent standard errors.
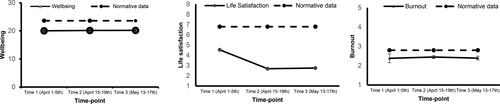
Figure 3. Levels of COVID-19 stress, worry and rumination at Time 1 (April 1–5th 2020), Time 2 (April 15–19th, 2020), and Time 3 (May 13–17th 2020). Error bars represent standard errors.
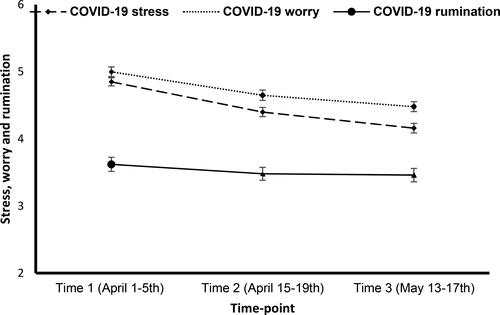
Pairwise comparisons using Bonferroni correction revealed that life satisfaction declined substantially from T1 (M = 4.54; SD = 2.20) to T2 (M = 2.69; SD = 2.02) and T3 (M = 2.76; SD = 2.09). This difference was statistically significant from T1 (p = <.001) to T2 and from T1 to T3 (p = <.001), but was not significant from T2 to T3 (p = 1.000). COVID-19 stress (M = 4.85; SD = 1.28) and COVID-19 worry (M = 5.00 SD = 1.28) were higher at T1 than when these were measured at T2, for the former (M = 4.16; SD = 1.53) and the latter (M = 4.48; SD = 1.38), and these differences were statistically significant (p = <.001). COVID-19 stress (M = 4.40; SD = 1.45) and COVID-19 worry (M = 4.65; SD = 1.39) were also higher at T2 than at T3 and these differences were significant (p = <.001).
Hypotheses 1 and 2
Higher levels of trait and state mindfulness, values and self-compassion will be associated with better psychological health during the early stages of the COVID-19 pandemic and the state relationships will be moderated by trait mindfulness, values and self-compassion.
The results for these analyses are presented in and and they show that higher levels of trait mindfulness (β = 0.125, p = <.001), trait values (β = 0.422, p = <.001) and trait self-compassion (β = 0.218, p = <.001) were significantly associated with better wellbeing during the early stages of the UK lockdown. Higher levels of trait mindfulness (β = 0.025, p = <.001), trait values (β = 0.150, p = <.001) and trait self-compassion (β = 0.074, p = <.001) were also significantly associated with greater life satisfaction scores. Similarly, higher levels of trait mindfulness (β = −0.021, p = .017), and trait self-compassion (β = −0.043, p = <.001) were also significantly associated with lower burnout.
Figure 4. Relationship between low, medium and high levels of trait mindfulness, values and self-compassion and mean scores for wellbeing, life satisfaction and burnout during the early stages of the UK lockdown (three-time points between April 1st and May 17th 2020). Error bars represent standard errors.

Table 2. Effects of trait and state mindfulness, values and self-compassion on psychological health outcomes and moderating effects of trait variables on the level 1 slope relationships.
The HLM analyses also found that state mindfulness (β = 0.491, p = <.001), state values (β = 0.335, p = <.001) and state self-compassion (β = 1.639, p = <.001) were all significantly associated with wellbeing during the early stages of UK lockdown (), such that higher scores in state values, state mindfulness and state self-compassion were associated with better wellbeing across time points. State self-compassion (β = .537, p = <.001) and state values (β = 0.212, p = <.001) had a significant relationship with life satisfaction with higher scores being associated with higher life satisfaction. State mindfulness (β = −1.998, p = <.001), state values (β = −0.839, p = .002), and state self-compassion (β = −2.835, p = .002) had a significant relationship with burnout. Higher scores in state mindfulness, state values and state self-compassion were associated with lower burnout scores.
Trait mindfulness, trait values and trait self-compassion did not moderate any of the relationships between state mindfulness, state values, state self-compassion and wellbeing, life satisfaction and burnout in any of the models ().
Hypothesis 3
Higher levels of COVID-19 stress, worry and rumination will be associated with poorer psychological health during the early stages of the COVID-19 pandemic.
The results of these analyses are presented in and they showed that COVID-19 stress (β = −0.524, p < .001) and COVID-19 rumination (β = −0.190, p = .029) were associated with wellbeing. Lower scores in COVID-19 stress and COVID-19 rumination were associated with higher wellbeing across the time points. COVID-19 stress (β = −0.199, p < .001), but not COVID-19 rumination (β = −0.076, p = .068), was associated with life satisfaction. Lower scores in COVID-19 stress were associated with higher scores in life satisfaction. COVID-19 stress (β = 2.069, p < .001) and COVID-19 rumination (β = 0.996, p = .002) were associated with burnout. COVID-19 stress and COVID-19 rumination were associated with higher scores in burnout. COVID-19 worry was not associated with wellbeing (β = 0.023, p = .799), life satisfaction (β = −0.086, p = 0.072) or burnout (β = 0.484, p = 0.132).
Table 3. Associations between COVID stress, worry and rumination and psychological health.
Hypothesis 4
Higher levels of trait mindfulness, values and self-compassion will be associated with higher levels of state mindfulness, values and self-compassion.
The results of these analyses are presented in and show that trait mindfulness (β = 3.401, p < .001) and trait self-compassion (β = 0.043, p < .001) had a significant positive association with state mindfulness. Trait mindfulness (β = 0.032, p < .001), trait values (β = 0.440, p < .001) and trait self-compassion (β = 0.063, p < .001) had a significant positive association with state values. Trait mindfulness (β = 0.011, p < .001), trait values (β = 0.061, p < .001) and trait self-compassion (β = 0.047, p < .001) had also a significant positive association with state self-compassion.
Table 4. Associations between trait and state measures of mindfulness, values and self-compassion.
Discussion
Three main findings emerged from the current study. First, the results showed that psychological flexibility processes may mitigate the negative psychosocial effects of the pandemic on mental health and help with better psychological adjustment throughout the first wave of the pandemic. Second, this study also confirmed that COVID-19 stress and rumination are important vulnerability factors for psychological health. Third, the findings also showed trait psychological flexibility influenced state levels of these variables. In terms of changes in psychological outcome measures during the early stages, we also found that life satisfaction decreased, while wellbeing and burnout levels did not change significantly throughout the six weeks of assessment. Nevertheless, when compared with normative comparison data, wellbeing levels, in particular, remained lower than the published norms and COVID-19 stress and worry decreased over time.
Our results for life satisfaction are in line with emerging (Satici et al., Citation2020) and previous studies (e.g. Yu et al., Citation2005; Cheng & Tang, Citation2004) showing that the pandemic may be a significant threat for different aspects of wellbeing. Results from our study show a large decline in life satisfaction in the UK from 4.54/10 to 2.56/10 six weeks after the start of the pandemic. It is noteworthy that average life satisfaction levels in the UK in 2019 were 6.8 out of 10 (Helliwell et al., Citation2019). While the design of our study cannot allow us to infer that changes in these measures were caused by the pandemic, these findings are commensurate with the aforementioned studies, and might be explained by the impact of physical distancing measures in place during the first weeks of UK lockdown, the limited ability to stay connected to family and friends, and higher unemployment rates. Conversely, a different pattern of results emerged for wellbeing and burnout. Although it is not possible to make direct comparisons with the levels of wellbeing pre-pandemic, the reported levels of wellbeing across the three time points were poor by comparison with the UK general population norms (Fat et al., Citation2017). In terms of burnout, levels at T1 reflected good levels of burnout as indicated by the normative data reported by Malach-Pines (Citation2005). In comparison with data pre-pandemic (M = 2.8; SD = 1.2) (Malach-Pines, Citation2005), burnout levels did not worsen in the current study.
As outlined above, the current study found that psychological flexibility processes may mitigate the negative psychosocial effects of the pandemic on mental health and may have helped individuals to adjust better during the first wave of the pandemic. This finding is important and suggests that the hypothesised psychological factors (i.e. state mindfulness, values and self-compassion) might be protective of wellbeing and help individuals adjust to changes when faced with an uncertain, challenging and stressful environment (Calhoun & Tedeschi, Citation1999; Prudenzi et al., 2021b). In addition, these results are consistent with a number of previous studies (Brockman et al., Citation2016; Gold & Marx Citation2007; Kumpula et al., Citation2011) and build upon and improve the cross-sectional evidence that is emerging from pandemic (Dawson & Golijani-Moghaddam, Citation2020; Landi et al., Citation2020; Pakenham et al., Citation2020).
Psychological flexibility may function as a resilience resource and help with the ability to shift perspectives and actions when unexpected events, such as the COVID-19 pandemic, arise. Moreover, in the current study we were able to identify specific processes of psychological flexibility (mindfulness, values and self-compassion) that emerged as significant protective factors that may have helped to adapt more easily to stressful and difficult situations. These novel results suggest that those who have been better able to bring more present-to-present awareness into their daily lives, have been kinder to themselves or behave according to their personal values experienced better levels of wellbeing and life satisfaction and decreased burnout. Therefore, these findings suggest that incorporating these processes into future psychological interventions may help to improve mental health in residents during and post the COVID-19 pandemic. For example, promoting ACT-based training more widely in the NHS and in communities could help lessen the negative effects of the pandemic on people’s wellbeing and on healthcare staffs’ mental health (Hayes et al., Citation2006; Prudenzi et al., Citation2021b).
Another important finding from the current study was that it confirmed that COVID-19 stress and rumination are important vulnerability factors for psychological health during the pandemic (e.g. Baiano et al., 2020; Satici et al., Citation2020; Zysberg & Zisberg, Citation2020). Individuals who reported the highest levels of COVID related rumination and stress experienced higher levels of psychological distress during the first UK lockdown. The latter findings are unsurprising given that the effects of stress and rumination on mental health, as well as on physical health outcomes, are well established (e.g. Clancy et al., Citation2016, Citation2020b; Lyubomirsky et al., Citation2015; McCarrick et al., Citation2021; O’Connor et al., Citation2021). However, these outcomes are also concerning given that behaviours driven by stress and fear (e.g. stockpiling goods or not wearing a face covering) may accelerate the spread of the disease or exacerbate its impact (Shultz et al., Citation2016) and can influence health behaviours including sleep (Clancy et al., Citation2020c). On the positive side, the current study showed that COVID-19 stress, worry and rumination decreased over the six-week assessment during the early stages of the UK lockdown. This is an interesting finding suggesting that, for example, instead of constantly thinking about not being able to see or spend time with family members, it may be that mindfulness, values and self-compassion may have helped to strengthen the relationship with others, especially the most vulnerable, and may have increased a self-perception of vulnerability ‘it’s normal to feel vulnerable and wanting to spend time with family and friends in isolation’, facilitating acceptance of negative emotions. These possibilities ought to be investigated in future research. In addition, the identification of COVID-19 stress and rumination as important vulnerabilities factors suggest that future mental health interventions should include components that specifically target stress and ruminative tendencies (Hansen et al., Citation2021; McCarrick et al., Citation2021).
Finally, we also found that people with higher trait psychological flexibility reported higher state levels of psychological flexibility during the early stages of the pandemic, suggesting that how one is behaving now (state-level psychological flexibility) was associated with how one tends to behave (trait-level psychological flexibility). These findings are important as they support the robustness of psychological flexibility as a construct. Although several studies have showed that dispositional psychological flexibility is a key ingredient of psychological health (Kashdan & Rottenberg, Citation2010 for a review), to our knowledge this is the first study that shows that state and trait measures are strongly related, and in our earlier analyses, that both trait and state components are significantly associated with psychological health outcomes.
Dispositional psychological flexibility is associated with a greater ability to pursue meaningful goals and adaptive responses despite experiencing distressing events (e.g. COVID-19 pandemic). Therefore, it may be that individuals with greater dispositional psychological flexibility may have been more willing to experience negative emotions or have employed more flexible response patterns (e.g. state psychological flexibility) when negative emotions or emotional distress arose. These findings align with daily diary studies conducted in real-life and laboratory settings by Cheng (Citation2001, Citation2003). Cheng et al. (Citation2001, 2003) found, on multiple occasions, that psychological flexibility (one’s intentions to display situation-appropriate behaviours, Cheng, Citation2001, p. 814) was a robust predictor of both problem-focused and emotion-focused coping strategies during stressful events (one’s behaviours about coping effectively in situations, Cheng, Citation2001).
This current study had a number of strengths. First, the longitudinal observation window assessed in this study through a repeated assessment of the relationship between psychological health (wellbeing, burnout and life satisfaction) and psychological coping mechanisms or resilience skills (state mindfulness, values and self-compassion) over time may help build up an accurate and ordered account of the participants’ inner experiences during the pandemic. Second, the sample size of this study could be considered large by comparison with other psychological research studies in the area (see Xiong et al., Citation2020 for a review of COVID-19 studies). Third, this study adopted a within-participant design, using participants as their own controls. Fourth, the main observed effects were maintained when controlling for trait measures of mindfulness, values and self-compassion. This is an important finding and adds additional weight to the robustness of the current results.
Some limitations should also be noted. First, given the unprecedented speed at which the disease spread, it was not possible for us to include appropriate baseline measurements prior to lockdown. Without an appropriate baseline, there is not sufficient information to attribute any findings to lockdown specifically because participants might have felt the same during a ‘typical’ six week period (although, this is unlikely). Second, this study aimed at assessing short-term psychological health during the pandemic. We believe that understanding and raising awareness of the impact of the COVID-19 pandemic on health and mental health of people during the pandemic, would help stakeholders, healthcare organisations and research funders prioritise mental health as a key health priority during any future pandemics or public health crises. A longer follow-up would have been beneficial and would help to understand whether the adverse effects of the pandemic on health and wellbeing are long-lasting or limited to the post-pandemic period. Third, including more detailed assessments of each of the main study outcomes may have provided more nuanced relationships between the main study variables. However, we were mindful of balancing the reliability and validity of the measures with participant burden.
Conclusion
The current study aimed to investigate associations between protective factors (state mindfulness, values and self-compassion) and risk factors (COVID-19 stress, worry and rumination) for mental health during the early stages of the COVID-19 pandemic. Psychological health outcome measures were found to be lower (worse) than normative comparison data during the early stages of the UK lockdown, while COVID-19 stress and worry reduced overtime. Higher levels of trait and state measures of psychological flexibility and self-compassion were associated with better psychological health across time points. Higher levels of COVID-19 stress, worry and rumination were also associated with poorer psychological health. These findings have implications for informing the design of psychological interventions during and post COVID-19 pandemic and are relevant to both practitioners and policy-makers.
Data availability
The data that support the findings of this study are available from the corresponding author [AP], upon reasonable request.
Disclosure statement
The views expressed in this article are those of the authors and not necessarily those of the NIHR, the Department of Health and Social Care or University. The funders played no role in design, data collection, analyses, interpretation of data, writing the report or in the submission of the paper. They accept no responsibility for the content.
Additional information
Funding
References
- Al-Ghunaim, T. A., Johnson, J., Biyani, C. S., & O’Connor, D. (2021). Psychological and occupational impact of the COVID-19 pandemic on UK surgeons: A qualitative investigation. BMJ Open, 11(4), e045699. https://doi.org/10.1136/bmjopen-2020-045699
- Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
- Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., Walsh, E., Duggan, D., & Williams, J. M. G. (2008). Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment, 15(3), 329–342. https://doi.org/10.1177/1073191107313003
- Baiano, C., Zappullo, I., Conson, M., & The LabNPEE Group. (2020). Tendency to worry and fear of mental health during Italy’s COVID-19 lockdown. International Journal of Environmental Research and Public Health, 17(16), 5928. https://doi.org/10.3390/ijerph17165928
- Brockman, C., Snyder, J., Gewirtz, A., Gird, S. R., Quattlebaum, J., Schmidt, N., Pauldine, M. R., Elish, K., Schrepferman, L., Hayes, C., Zettle, R., & DeGarmo, D. (2016). Relationship of service members’ deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. Journal of Family Psychology: JFP, 30(1), 52–62.
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. https://doi.org/10.1016/S0140-6736(20)30460-8
- Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848.
- Calhoun, L. G., & Tedeschi, R. G. (1999). Facilitating posttraumatic growth: A clinician’s guide. Routledge.
- Cartwright, J., & Thompson, A. (2020). Introducing psychological strategies for healthcare professionals during COVID-19: An overview of the face COVID intervention. Dermatological Nursing, 19(2), 18–21.
- Chater, A. M., Shorter, G. W., Swanson, V., Kamal, A., Epton, T., Arden, M. A., Hart, J., Byrne-Davis, L. M. T., Drury, J., Whittaker, E., Lewis, L. J. M., McBride, E., Chadwick, P., O’Connor, D. B., & Armitage, C. J. (2021). Template for rapid iterative consensus of experts (TRICE). International Journal of Environmental Research and Public Health, 18 (19), 10255. https://doi.org/10.3390/ijerph181910255
- Cheng, C. (2001). Assessing coping flexibility in real-life and laboratory settings: A multimethod approach. Journal of Personality and Social Psychology, 80(5), 814. https://doi.org/10.1037/0022-3514.80.5.814
- Cheng, C. (2003). Cognitive and motivational processes underlying coping flexibility: A dual-process model. Journal of Personality and Social Psychology, 84(2), 425. https://doi.org/10.1037/0022-3514.84.2.425
- Cheng, C., & Tang, C. S. K. (2004). The psychology behind the masks: Psychological responses to the severe acute respiratory syndrome outbreak in different regions. Asian Journal of Social Psychology, 7(1), 3–7.
- Ciotti, M., Ciccozzi, M., Terrinoni, A., Jiang, W. C., Wang, C. B., & Bernardini, S. (2020). The COVID-19 pandemic. Critical Reviews in Clinical Laboratory Sciences, 57(6), 365–388. https://doi.org/10.1080/10408363.2020.1783198
- Clancy, F., O’Connor, D. B., & Prestwich, A. (2020a). Do worry and brooding predict health behaviors? A daily diary investigation. International Journal of Behavioral Medicine, 27(5), 591–601.
- Clancy, F., Prestwich, A., Ferguson, E., & O’Connor, D. B. (2020b). Cross-sectional and prospective associations between perseverative cognition, stress and health behaviours. Psychology and Health, 1–18.
- Clancy, F., Prestwich, A., Caperon, L., & O’Connor, D. B. (2016). Perseverative cognition and health behaviors: A systematic review and meta-analysis. Frontiers in Human Neuroscience, 10, 534.
- Clancy, F., Prestwich, A., Caperon, L., Tsipa, A., & O’Connor, D. B. (2020c). The association between worry and rumination with sleep in non-clinical populations. A systematic review and meta-analysis. Health Psychology Review, 14(4), 427–448.
- Clarke, A., Friede, T., Putz, R., Ashdown, J., Martin, S., Blake, A., Adi, Y., Parkinson, J., Flynn, P., Platt, S., & Stewart-Brown, S. (2011). Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health, 11(1), 1–9. https://doi.org/10.1186/1471-2458-11-487
- Cullen, W., Gulati, G., & Kelly, B. D. (2020). Mental health in the COVID-19 pandemic. QJM, 113(5), 311–312. https://doi.org/10.1093/qjmed/hcaa110
- Dawson, D. L., & Golijani-Moghaddam, N. (2020). COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science, 17, 126–134.
- Fat, L. N., Scholes, S., Boniface, S., Mindell, J., & Stewart-Brown, S. (2017). Evaluating and establishing national norms for mental wellbeing using the short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS): Findings from the Health Survey for England. Quality of Life Research, 26(5), 1129–1144. https://doi.org/10.1007/s11136-016-1454-8
- Fullana, M. A., Hidalgo-Mazzei, D., Vieta, E., & Radua, J. (2020). Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. Journal of Affective Disorders, 275, 80–81.
- García-Fernández, L., Romero-Ferreiro, V., López-Roldán, P. D., Padilla, S., & Rodriguez-Jimenez, R. (2020). Mental health in elderly Spanish people in times of COVID-19 outbreak. The American Journal of Geriatric Psychiatry, 28(10), 1040–1045. https://doi.org/10.1016/j.jagp.2020.06.027
- Gold, S. D., Marx, B. P., & Lexington, J. M. (2007). Gay male sexual assault survivors: The relations among internalized homophobia, experiential avoidance, and psychological symptom severity. Behaviour Research and Therapy, 45(3), 549–562.
- Gu, J., Strauss, C., Crane, C., Barnhofer, T., Karl, A., Cavanagh, K., & Kuyken, W. (2016). Examining the factor structure of the 39-item and 15-item versions of the Five Facet Mindfulness Questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychological Assessment, 28(7), 791–802. https://doi.org/10.1037/pas0000263
- Hansen, S. R., Wetherell, M. A., & Smith, M. A. (2021). Written benefit finding for improving psychological health during the Covid-19 pandemic first wave lockdown. Psychology & Health, 1–18. https://doi.org/10.1080/08870446.2021.1936521
- Hayes, J. A., Lockard, A. J., Janis, R. A., & Locke, B. D. (2016). Construct validity of the Self-Compassion Scale-Short Form among psychotherapy clients. Counselling Psychology Quarterly, 29(4), 405–422. https://doi.org/10.1080/09515070.2016.1138397
- Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25.
- Hegarty, R. S., Treharne, G. J., Stebbings, S., Graham, K., & Conner, T. S. (2019). Optimising daily diary questionnaires about fatigue, psychological flexibility and well-being: Perspectives of people with rheumatic disease. Psychology & Health, 34(2), 181–199.
- Helliwell, J. F., Huang, H., & Wang, S. (2019). Changing world happiness. World Happiness Report, 2019, 11–46.
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Cohen Silver, R., Everall, I., Ford, T., John, A., Kabir, T., King, K., Madan, I., Michie, S., Przybylski, A. K., Shafran, R., Sweeney, A., … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. https://doi.org/10.1016/S2215-0366(20)30168-1
- Kadhum, M., Farrell, S., Hussain, R., & Molodynski, A. (2020). Mental wellbeing and burnout in surgical trainees: Implications for the post-COVID-19 era. The British Journal of Surgery, 107(8), e264.
- Kannampallil, T. G., Goss, C. W., Evanoff, B. A., Strickland, J. R., McAlister, R. P., & Duncan, J. (2020). Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS One, 15(8), e0237301.
- Kashdan, T. B., & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878.
- Khalafallah, A. M., Lam, S., Gami, A., Dornbos, I. I. I., D. L., Sivakumar, W., Johnson, J. N., & Mukherjee, D. (2020). Burnout and career satisfaction among attending neurosurgeons during the COVID-19 pandemic. Clinical Neurology and Neurosurgery, 198, 106193.
- Kreft, I., & De Leeuw, J. (2006). Introducing multilevel modeling. Sage.
- Kumpula, M. J., Orcutt, H. K., Bardeen, J. R., & Varkovitzky, R. L. (2011). Peritraumatic dissociation and experiential avoidance as prospective predictors of posttraumatic stress symptoms. Journal of Abnormal Psychology, 120(3), 617–627.
- Landi, G., Pakenham, K. I., Boccolini, G., Grandi, S., & Tossani, E. (2020). Health anxiety and mental health outcome during COVID-19 lockdown in Italy: The mediating and moderating roles of psychological flexibility. Frontiers in Psychology, 11, 2195. https://doi.org/10.3389/fpsyg.2020.02195
- Li, W., Yang, Y., Liu, Z.-H., Zhao, Y.-J., Zhang, Q., Zhang, L., Cheung, T., & Xiang, Y.-T. (2020). Progression of mental health services during the COVID-19 outbreak in China. International Journal of Biological Sciences, 16(10), 1732–1738.
- Lyubomirsky, S., Layous, K., Chancellor, J., & Nelson, S. K. (2015). Thinking about rumination: The scholarly contributions and intellectual legacy of Susan Nolen-Hoeksema. Annual Review of Clinical Psychology, 11(1), 1–22. https://doi.org/10.1146/annurev-clinpsy-032814-112733
- Malach-Pines, A. (2005). The burnout measure, short version. International Journal of Stress Management, 12(1), 78–88. https://doi.org/10.1037/1072-5245.12.1.78
- McCarrick, D. J., Prestwich, A., Prudenzi, A., & O’Connor, D. B. (2021). Health effects of psychological interventions for worry and rumination: A meta-analysis. Health Psychology, 40(9), 617–630. https://doi.org/10.1037/hea0000985
- McCracken, L. M., & Morley, S. (2014). The psychological flexibility model: A basis for integration and progress in psychological approaches to chronic pain management. The Journal of Pain, 15(3), 221–234.
- McCracken, L. M., & Yang, S.-Y. (2006). The role of values in a contextual cognitive-behavioral approach to chronic pain. Pain, 123(1), 137–145. https://doi.org/10.1016/j.pain.2006.02.021
- Neff, K. D., Tóth-Király, I., Knox, M. C., Kuchar, A., & Davidson, O. (2021). The development and validation of the state self-compassion scale (long-and short form). Mindfulness, 12(1), 121–140. https://doi.org/10.1007/s12671-020-01505-4
- O’Connor, D. B., & Ferguson, E. (2016). Stress and stressors. In Y. Benyamini, M. Johnston, & E.C. Karademas (Eds.), Assessment in health psychology (pp. 104–118). Hogrefe.
- O’Connor, D. B., Aggleton, J. P., Chakrabarti, B., Cooper, C. L., Creswell, C., Dunsmuir, S., Fiske, S. T., Gathercole, S., Gough, B., Ireland, J. L., Jones, M. V., Jowett, A., Kagan, C., Karanika-Murray, M., Kaye, L. K., Kumari, V., Lewandowsky, S., Lightman, S., Malpass, D., Meins, E., Morgan, B. P., Morrison Coulthard, L. J., Reicher, S. D., Schacter, D. L., Sherman, S. M., Simms, V., Williams, A., Wykes, T., & Armitage, C. J. (2020a). Research Priorities for the COVID-19 pandemic and beyond: A call to action for psychological science. British Journal of Psychology, 111(4), 603–629. https://doi.org/10.1111/bjop.12468
- O’Connor, D. B., Thayer, J. F., & Vedhara, K. (2021). Stress and health: A review of psychobiological processes. Annual Review of Psychology, 72(1), 663–688. https://doi.org/10.1146/annurev-psych-062520-122331
- O’Connor, R. C., Wetherall, K., Cleare, S., McClelland, H., Melson, A. J., Niedzwiedz, C. L., O’Carroll, R. E., O’Connor, D. B., Platt, S., Scowcroft, E., Watson, B., Zortea, T., Ferguson, E., & Robb, K. A. (2020b). Mental health and wellbeing during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. The British Journal of Psychiatry, 1–8.
- Pakenham, K. I., Landi, G., Boccolini, G., Furlani, A., Grandi, S., & Tossani, E. (2020). The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science, 17, 109–118.
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383(6), 510–512. https://doi.org/10.1056/NEJMp2008017
- Presti, G., McHugh, L., Gloster, A., Karekla, M., & Hayes, S. C. (2020). The dynamics of fear at the time of COVID-19: A contextual behavioural science perspective. Clinical Neuropsychiatry, 17(2), 65–71.
- Prudenzi, A., Graham, C. D., Clancy, F., Hill, D., O’Driscoll, R., Day, F., & O’Connor, D. B. (2021a). Group-based acceptance and commitment therapy interventions for improving general distress and work-related distress in healthcare professionals: A systematic review and meta-analysis. Journal of Affective Disorders, 295, 192–202. https://doi.org/10.1016/j.jad.2021.07.084
- Prudenzi, A., Graham, C. D., Flaxman, P., & O’Connor, D. B. (2021b). Wellbeing, burnout, and safe practice among healthcare professionals: Predictive influences of mindfulness, values, and self-compassion. Psychology, Health & Medicine. 1–14.
- Quinn, C. S. (2008). Crisis and emergency risk communication in a pandemic: A model for building capacity and resilience of minority communities. Health Promotion Practice, 9(4_suppl), 18S–25S.
- Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology & Psychotherapy, 18(3), 250–255. https://doi.org/10.1002/cpp.702
- Raudenbush, S. W., Bryk, A. S., & Congdon, R. (2011). HLM 7 for Windows. Scientific Software International.
- Salazar de Pablo, G., Vaquerizo-Serrano, J., Catalan, A., Arango, C., Moreno, C., Ferre, F., Shin, J. I., Sullivan, S., Brondino, N., Solmi, M., & Fusar-Poli, P. (2020). Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. Journal of Affective Disorders, 275, 48–57.
- Satici, B., Saricali, M., Satici, S. A., & Griffiths, M. D. (2020). Intolerance of uncertainty and mental wellbeing: Serial mediation by rumination and fear of COVID-19. International Journal of Mental Health and Addiction, 1–12.
- Shultz, J. M., Cooper, J. L., Baingana, F., Oquendo, M. A., Espinel, Z., Althouse, B. M., Marcelin, L. H., Towers, S., Espinola, M., McCoy, C. B., Mazurik, L., Wainberg, M. L., Neria, Y., & Rechkemmer, A. (2016). The role of fear-related behaviors in the 2013–2016 West Africa Ebola virus disease outbreak. Current Psychiatry Reports, 18(11), 104. https://doi.org/10.1007/s11920-016-0741-y
- Stewart-Brown, S., Tennant, A., Tennant, R., Platt, S., Parkinson, J., & Weich, S. (2009). Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): A Rasch analysis using data from the Scottish Health Education Population Survey. Health and Quality of Life Outcomes, 7(1), 1–8. https://doi.org/10.1186/1477-7525-7-15
- Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., Parkinson, J., Secker, J., & Stewart-Brown, S. (2007). The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health and Quality of Life Outcomes, 5(1), 63.
- Tol, W. A., Leku, M. R., Lakin, D. P., Carswell, K., Augustinavicius, J., Adaku, A., Au, T. M., Brown, F. L., Bryant, R. A., Garcia-Moreno, C., Musci, R. J., Ventevogel, P., White, R. G., & van Ommeren, M. (2020). Guided self-help to reduce psychological distress in South Sudanese female refugees in Uganda: A cluster randomised trial. The Lancet. Global Health, 8(2), e254–e263.
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., Choo, F. N., Tran, B., Ho, R., Sharma, V. K., & Ho, C. (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48. https://doi.org/10.1016/j.bbi.2020.04.028
- Wilder-Smith, A., & Freedman, D. O. (2020). Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of Travel Medicine, 27(2), taaa020. https://doi.org/10.1093/jtm/taaa020
- Wu, W., Zhang, Y., Wang, P., Zhang, L., Wang, G., Lei, G., Xiao, Q., Cao, X., Bian, Y., Xie, S., Huang, F., Luo, N., Zhang, J., & Luo, M. (2020). Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. Journal of Medical Virology, 92(10), 1962–1970. https://doi.org/10.1002/jmv.25914
- Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64.
- Yu, H. Y. R., Ho, S. C., So, K. F. E., & Lo, Y. L. (2005). The psychological burden experienced by Hong Kong midlife women during the SARS epidemic. Stress and Health, 21(3), 177–184. https://doi.org/10.1002/smi.1051
- Zoccola, P. M., Dickerson, S. S., & Yim, I. S. (2011). Trait and state perseverative cognition and the cortisol awakening response. Psychoneuroendocrinology, 36(4), 592–595. https://doi.org/10.1016/j.psyneuen.2010.10.004
- Zysberg, L., & Zisberg, A. (2020). Days of worry: Emotional intelligence and social support mediate worry in the COVID-19 pandemic. Journal of Health Psychology, 1–10.