Abstract
Objective
The COVID-19 pandemic saw promotion of novel virus transmission-reduction behaviours, and discouragement of familiar transmission-conducive behaviours. Understanding changes in the automatic nature of such behaviours is important, because habitual behaviours may be more easily reactivated in future outbreaks and disrupting old habits may discontinue unwanted behaviours.
Design
A repeated-measures, multi-national design tracked virus-transmission habits and behaviour fortnightly over six months (Apr–Sept 2020) among 517 participants (age M = 42 ± 16y, 79% female).
Main Outcome Measures
Within-participant habit trajectories across all timepoints, and engagement in transmission-reduction behaviours (handwashing when entering home; handwashing with soap for 20 seconds; physical distancing) and transmission-conducive behaviours (coughing/sneezing into hands; making physical contact) summed over the final two timepoints.
Results
Three habit trajectory types were observed. Habits that remained strong (‘stable strong habit’) and habits that strengthened (‘habit formation’) were most common for transmission-reduction behaviours. Erosion of initially strong habits (‘habit degradation’) was most common for transmission-conducive behaviours. Regression analyses showed ‘habit formation’ and ‘stable strong habit’ trajectories were associated with greater behavioural engagement at later timepoints.
Conclusion
Participants typically maintained or formed transmission-reduction habits, which encouraged later performance, and degraded transmission-conducive habits, which decreased performance. Findings suggest COVID-19-preventive habits may be recoverable in future virus outbreaks.
Transmission of viruses such as SARS-CoV-2, the pathogenic Coronavirus that causes COVID-19, is driven by human behaviour (West et al., Citation2020). Unhygienic actions such as coughing or sneezing into hands transmit viruses, whereas hygienic actions such as washing hands for 20 seconds with soap and water halt transmission (Alzyood et al., Citation2020). In Spring 2020, early in the COVID-19 pandemic, infection control guidance focussed on discouraging engagement in familiar ‘transmission-conducive’ behaviours, such as sneezing into hands), and promoting uptake of potentially unfamiliar ‘transmission-reduction behaviours’, such as maintaining distance from others (Centers for Disease Control & Prevention, Citation2020; World Health Organization [WHO], 2020a). While the focus of recommendations was SARS-CoV-2, such behaviours have the potential to influence transmission of many viruses (Oster et al., Citation2021; Rabie & Curtis, Citation2006). Maintenance of transmission-related behaviour changes prompted by the COVID-19 pandemic could aid efforts to contain future outbreaks of SARS-Cov-2 and other viruses. Research is needed to understand whether behavioural adaptations made during the COVID-19 pandemic may have become ingrained in memory.
Habit is a key hypothesised predictor of behaviour maintenance (Kwasnicka et al., Citation2016). Although often used in lay discourse to denote repetitive behaviour, psychologists define habit as a process through which encountering a cue automatically triggers a non-conscious impulse to perform a specific action, due to activation of learned cue-action associations (Gardner, Citation2015). Habit forms through consistent repetition of a specific action (e.g. washing hands) following exposure to a specific cue (e.g. entering the home) (Keller et al., Citation2021; Lally et al., Citation2010). Owing to its automation, once formed, habit can compensate for temporary lapses in attention or motivation, facilitating performance when the actor might otherwise forget or lack the momentary desire to act (Danner et al., Citation2008; Gardner et al., Citation2020; Neal et al., Citation2013). A person with a stronger habit for a given behaviour is less likely to be derailed by competing goals or indecisiveness, so is more likely to enact the behaviour in associated settings (Verplanken & Melkevik, Citation2008). Habit formation has been proposed as a mechanism for maintaining desired behaviours (Rothman et al., Citation2009). Conversely, cessation of unwanted behaviours may be aided by disrupting pre-existing habits (Quinn et al., Citation2010).
While it is unrealistic to expect all transmission-reduction behaviours to persist indefinitely after the COVID-19 pandemic, forming transmission-reduction habits is likely to be beneficial for personal and public health in future virus outbreaks. The distinction between habit, as a process that generates behaviour based on learned associations, and habitual behaviour, as the output of this process, is important (Gardner, Citation2015). While there is debate around the role of goals in habitual behaviour (Kruglanski & Szumowska, Citation2020; Wood et al., Citation2022), a base level of conscious motivation is likely to be necessary to support habitual behaviours (Gardner et al., Citation2020; Marien et al., Citation2019). Although habitual behaviours are less sensitive to changes in conscious motivation and goals than non-habitual actions (Verplanken et al., Citation1997), they are not wholly insensitive; if motivation erodes completely, habitual behaviours will diminish over time (Wood et al., Citation2022). Transmission-reduction behaviours may continue indefinitely if they are viewed as relevant to goals that remain valued after the COVID-19 pandemic ends; washing hands upon entering the home, for example, might be expected to persist if viewed as integral to personal hygiene more broadly (Verplanken & Sui, Citation2019). However, habitual transmission-reduction behaviours will likely be discontinued if they are perceived to have become redundant when the COVID-19 pandemic passes, such that people are no longer motivated to perform them (e.g. physical distancing), or they actively want to perform counterhabitual actions (e.g. hugging a family member, despite having a habit for physical distancing). In such instances however, despite changes in habitual behaviour, underlying habit associations may remain stored in memory (Bouton, Citation2000). Such associations are thought to retain the potential to be reactivated when motivation increases, leading to rapid recovery of the learned habitual action (Wood & Rünger, Citation2016). Knowing whether and which transmission-reduction habits formed in response to the COVID-19 pandemic could inform strategies to reactivate such actions in future virus outbreaks.
Similarly, declines in habitual transmission-conducive behaviours during the COVID-19 pandemic could provide useful information for public health initiatives in future outbreaks. Habits can be disrupted by overwriting habit associations, avoiding cues, or wilfully inhibiting the translation of unwanted habit impulses into action (Gardner et al., Citation2021; Quinn et al., Citation2010). Of these strategies, learning a new association between a transmission-reduction response (e.g. maintaining physical distance) and an existing cue (e.g. greeting family members), and so directly displacing an old, transmission-conducive habitual response (e.g. making physical contact), is thought to produce most long-lasting change (Gardner et al., Citation2021). Discontinuing cue exposure (e.g. avoiding family members), or suppressing responses to such cues (e.g. avoiding making physical contact), can block habitual transmission-conducive behaviour, but may not change underlying habit memory traces (Gardner et al., Citation2021). Nonetheless, understanding whether and which transmission-conducive habitual behaviours were disrupted during the COVID-19 pandemic, regardless of how this was achieved, would be insightful, because it would establish the potential for such habits to be discontinued, if only temporarily, during major outbreaks.
The present study
Documenting changes in virus-transmission habit strength, and associations between habit change and behavioural engagement, may help to identify whether and which habits are likely to remain ingrained in memory beyond the pandemic. This longitudinal study was set up in the early phases of the COVID-19 pandemic (Spring 2020) to track virus-transmission habits and behaviour across participants in multiple countries over the course of six months.
We focussed on five target behaviours, relating to hand hygiene and physical distancing, which were emphasised by the WHO (Citation2020a, Citation2020b) when the study was designed. We focussed on three transmission-reduction behaviours for which consistent performance would likely develop ‘good’ habits (handwashing for 20 seconds with soap and water; handwashing on entering the home; maintaining physical distance from others), and two transmission-conducive behaviours for which discontinuation would erode ‘bad’ habits (coughing or sneezing into handsFootnote1; making physical contact with others). Two handwashing behaviours were included to capture two different forms of habitual behaviour: one in which habit guides selection of action (handwashing) upon exposure to a cue (entering the home; ‘habitual instigation’), and another in which habit likely facilitates efficient performance of an action sequence (i.e. 20 seconds of handwashing), such that completion of a component of the sequence (e.g. applying soap) habitually cues the next (e.g. turning on tap; ‘habitual execution’) (Gardner et al., Citation2016).
Our primary research question was: ‘How did virus-transmission habits change over the course of the pandemic?’ To address this question, we extracted habit trajectory clusters, and categorised observed patterns of habit change for each behaviour for each participant into these clusters. We assumed that, given the salience of the COVID-19 pandemic when the study began, participants would be motivated to comply with public health guidelines in everyday settings (Wright et al., Citation2021), such that, knowingly or not, for many participants, ‘good’ habits would form and ‘bad’ habits would be eroded (Lally & Gardner, Citation2013). Despite willingness to engage in recommended behaviours, some people struggle to form strong habits for some behaviours in some settings, despite consistent repetition (Lally et al., Citation2010). Assuming that transmission-reduction behaviours were unfamiliar to participants, or not performed consistently, at the study outset, we therefore expected that participants would either successfully or unsuccessfully form transmission-reduction habits. Thus:
Hypothesis 1: For transmission-reduction behaviours, two habit trajectory clusters will emerge, corresponding to habit formation, and stable negligible habits.
Relatedly, we assumed transmission-conducive behaviours would be familiar to many - but not all - participants at the study outset, such that they would have pre-existing strong habits or no habits. People can struggle to overcome unwanted habits, due to their automaticity (Orbell & Verplanken, Citation2010). We therefore expected that those with pre-existing strong habits would either successfully or unsuccessfully break those habits. Specifically:
Hypothesis 2: For transmission-conducive behaviours, three habit trajectory clusters will emerge, corresponding to habit degradation among those with pre-existing strong habits, stable pre-existing strong habits, and stable pre-existing negligible habits.
Once formed, habit is predicted to consistently trigger behaviour in associated settings, such that habit strength typically correlates positively with behaviour frequency (Triandis, Citation1977). To verify that observed changes in habit over the study period were related to subsequent behaviour frequency, we posed a secondary research question: ‘Were changes in habit associated with behavioural engagement at later timepoints?’ To address this question, we tested whether cluster category membership was associated with behavioural engagement at later timepoints, which we supplemented with analyses of associations with engagement at early timepoints, prior to any predicted habit change. We expected that:
Hypothesis 3: For transmission-reduction behaviours, participants who subsequently formed habits will typically show the same level of behavioural engagement at early timepoints, but will engage more at later points, than those who maintained pre-existing negligible habits.
Hypothesis 4a: For transmission-conducive behaviours, those who subsequently degraded pre-existing strong habits would show the same level of behavioural engagement at early timepoints, but less engagement at later points, as those who maintained pre-existing strong habits.
Hypothesis 4b: For transmission-conducive behaviours, those who subsequently degraded pre-existing strong habits would show greater behavioural engagement at early timepoints, but the same the level of engagement at later points, as those with who maintained pre-existing negligible habits.
Hypothesis 4c: For transmission-conducive behaviours, those who maintained pre-existing strong habits would show greater behavioural engagement at both early and later timepoints than those who maintained pre-existing negligible habits.
Within the extant literature, tests of habit-behaviour associations typically involve correlating behaviour frequency at one timepoint with habit strength as measured at the same, or an earlier, timepoint (see Gardner, Citation2015). Our analyses assessed whether changes in habit over an extended period affected later behavioural engagement. Crucially, documenting associations between trajectories with behavioural engagement permits a unique, exploratory comparison, for which no hypotheses were formulated, regarding whether those who experienced declines in transmission-conducive habits during the pandemic reached the same low level of behavioural engagement as those with no pre-existing habits.
Methods
Design and procedure
The study used a repeated-measures survey design. Adults aged 18 years or older were recruited through social media, local advertisements, and email lists at academic institutions, in the UK, Italy, Germany, Australia, and Canada. The baseline survey was open to new participants from April–September 2020. Every 14-days post-baseline, baseline completers were sent automated invitations to follow-up surveys, hosted on Qualtrics (Qualtrics, Citation2005), until a predetermined end date (30 September 2020). Participants completed the survey in one of three languages (English, German, Italian). Survey opening dates were staggered across countries, but the study end date was identical across countries in accordance with institutionally approved procedures. Thus, participants could complete a maximum of 13 English, 12 German, or 11 Italian language surveys.
Study adverts, and all documentation circulated to participants during the study, depicted the research as pertaining to ‘hygiene behaviours during and beyond the Covid-19 pandemic’. The term ‘habit’ was not used, to avoid evoking negative or positive connotations that might have led to selection bias or socially desirable responding. Procedures were approved by local ethics committees of host institutions prior to recruitment.
Study timeline
The study was designed by a predominantly UK-based team in mid-March 2020, at which time the UK public was advised to avoid non-essential travel and social contact, and to work at home if possible (see Hale et al., Citation2021). The English language survey went live on 1 April 2020, by which time the UK was in national lockdown (announced 23 March 2020), with all residents instructed to stay at home except for essential purposes. UK lockdown restrictions were relaxed from May 2020 until the end of the study period in September. The English survey opened when, in Australia and Canada, borders were closed to non-residents and non-native citizens, physical distancing had been imposed and some non-essential services had shut. Australian and Canadian borders remained closed throughout the study period.
Although originally envisaged as a study of a UK sample, interest from colleagues led to expansion to other English and non-English speaking countries (Italy, Germany). Surveys were translated both backward and forward by native Italian and German researchers, both fluent in English. The Italian translation opened on 18 April 2020, five weeks after Italy imposed a national lockdown, which ended in June 2020. The German translation opened on 28 April 2020, five weeks after Germany closed its schools and nursing homes, and borders, and one week before restrictions began to be eased. Containment measures of some kind were effective throughout the study period in all countries from which data were collected.
Measures
All measures were self-reported. Demographics (age, country of residence, gender, education status) were measured at baseline only. Behaviour engagement and habit strength were assessed at all timepoints, for five behaviours. The three transmission-reduction behaviours described were: ‘washing my hands with soap and water for at least 20 seconds’ (hereafter, handwashing for 20 seconds); ‘washing my hands when I enter my home’ (handwashing on entering home); and ‘when I am around other people, staying at least [1.5m/2m] away from them’Footnote2 (maintaining physical distance). The two transmission-conducive behaviours were: ‘coughing or sneezing into my hands’; and ‘making physical contact when I meet other people’ (making physical contact with others). ‘Physical contact’ was defined as ‘hugging, kissing, or shaking hands’.
Behavioural engagement was assessed by asking how consistently each of the five behaviours was performed on the previous day (‘None of the time’, 0; ‘Almost none of the time’, 1; ‘Some of the time’, 2; ‘Most of the time’, 3; ‘Every time’, 4; ‘Not applicable’, treated as missing). For each behaviour, habit strength was assessed as the mean of two automaticity items from the Self-Report Habit Index (Gardner et al., Citation2012; Verplanken & Orbell, Citation2003): ‘[Behaviour X, e.g. ‘washing my hands when I enter my home’] is something I do automatically’ and ‘[Behaviour X] is something I do without thinking’ (strongly disagree [1] – strongly agree [7]). Although habit-related automaticity is typically self-reported using four items, to reduce participant burden over repeated assessments, we used two items previously judged to best represent automaticity (Gardner et al., Citation2012). Reliability (α) of two-item scales, across behaviours and timepoints, ranged from .88 to .93.
Data management and analyses
Data preparation
All analyses were conducted using R version 3.6.2 (R Core Team, Citation2019). To enable meaningful observations of habit change over time, data were only analysed from participants with data from at least four timepoints (Leffondré et al., Citation2004). Mean differences were tested using t-tests for between-person variables and multilevel modelling for within-person variables, with Bonferroni corrections for multiple comparisons. ‘Early’ behavioural engagement was calculated as the mean of the baseline and first subsequently completed survey per participant and ‘late’ behavioural engagement was calculated as the mean of the final two assessments completed by that individual. Our analysis treated the ‘early’ time points as the starting point of habit trajectories for each individual, and the ‘late’ time points as the end point of the habit trajectory for each person.
Analysis overview
First, cluster analysis was undertaken to identify patterns of per-behaviour habit trajectories. Each participant’s trajectory, for each behaviour, was then classified into one of the identified clusters. The cluster analysis allowed for differences in trajectories across different behaviours for each participant and accounted for within-participant nesting of data. Second, a linear regression model was run for each behaviour to predict behavioural engagement from participants’ habit cluster membership for that behaviour.
How did virus-transmission habits change over the course of the pandemic? This was addressed via a three-step cluster analysis, undertaken using the traj package (Sylvestre et al., Citation2006), to identify discrete patterns of within-person per-behaviour habit trajectories as proposed by Leffondré et al. (Citation2004). Step 1 consisted of calculating 24 habit strength trajectory parameters for each behaviour for each participant using data from all timepoints available for that participant (see Supplemental Table). The aim of calculating the parameters was to comprehensively capture possible patterns of longitudinal change across four or more measurement points. The parameters pertained to variation over time (e.g. standard deviation of all scores), direction of change (e.g. slope of linear model), fluctuation and non-linearity (e.g. maximum of the first differences; i.e. whether at least one large increase was observed between scores at two consecutive timepoints), and relative measures of change (e.g. ratios of difference, which compare changes at different stages of, or summarised across, the study period; Leffondré et al., Citation2004). Parameters found to correlate strongly (r ≥ .95) were omitted from Step 2. Step 2 was a principal factor analysis, with varimax rotation of the trajectory parameters, and was run to determine which parameters best discerned habit trajectories (such that parameter eigenvalues were greater than 1.0; Leffondré et al., Citation2004; Sylvestre et al., Citation2006). Step 3 was run to identify habit trajectory clusters, via a k-means cluster analysis (using the NbClust package; Charrad et al., Citation2014) of factors identified in Step 2. Euclidean distance was used to compute the dissimilarity matrix, and the number of clusters was determined based on the Friedman index (Charrad et al., Citation2014; Friedman & Rubin, Citation1967). Nominal cluster variables were formed to identify which cluster best fitted each participant’s habit trajectory for each behaviour.
Were changes in habit associated with behavioural engagement at later timepoints? This was addressed by using nominal cluster variables as predictors in linear regression models, run for each behaviour, to model early and later behavioural engagement. This analysis was run with planned comparisons to explore whether the habit trajectory cluster that best fitted each behaviour for each participant predicted their engagement in the corresponding behaviour at later measurement points. Models of early engagement were run to investigate whether differences existed in behavioural engagement between trajectory clusters prior to potential changes in habit strength.
Post-hoc power analysis was conducted to test whether the obtained sample size allowed for sufficiently powered hypotheses testing (Faul et al., Citation2007, Citation2009). At a conservative significance level of α = 0.05, the study was powered to 1 − β = 0.97 for a medium-sized effect (f2 = 0.15), 1 − β = 0.94 for a small effect (f2 = .06), and 1 − β = 0.36 for a very small effect (f2 = 0.02).
Results
Sample description
Of 961 participants that completed the baseline survey, 517 (53.8%) completed assessments at four or more timepoints, so were entered into the study. Those who were excluded from the study for completing fewer than four assessments were younger (non-completers M age = 35.35, completers M age = 41.77; t(946.85) = 6.38, p < .01) and reported weaker habit for maintaining physical distance (non-completers M = 4.33, completers M = 4.76, p < .01), and weaker habit for making physical contact with others (non-completers M = 2.85, completers M = 3.20, p < .01), at baseline. There were no other baseline differences in behavioural engagement or habit strength between study completers and non-completers (all p’s > .01).
Of the 517 participants, most resided in Germany (39.7%), the United Kingdom (32.9%), Australia (7.9%), Italy (5.4%), or one of 25 other countries with <3% prevalence (e.g. Belgium, Canada, China, Georgia, Netherlands, Spain, Switzerland, USA). Most surveys were completed in English (54.2%); 39.8% completed the German translation, and 6.0% the Italian translation. Most participants identified as female (79.1%; 19.1% male, 1.5% other or not reporting), and average age was 42 y (SD = 16). Most participants had completed higher education (68.1%), though some were in full-time education (19.1%).
Means, standard deviations, and mean change between early and later measurement points for behavioural engagement for each behaviour are shown in . At both early and later measurement points, behavioural engagement was higher for all transmission-reduction behaviours (washing hands for 20 seconds, handwashing on entering home, and maintaining physical distance), than for transmission-conducive behaviours (coughing or sneezing into hands, making physical contact with others). Between early and later points, overall behavioural engagement did not change for transmission-reduction behaviour but unexpectedly increased for transmission-conducive behaviours.
Table 1. Descriptive statistics of early (first two completed surveys per participant) and late (last two completed surveys per participant) behavioural engagement.
How did virus-transmission habits change over the course of the pandemic?
Of the 24 parameters used to quantify change, habit trajectories were discernible using four indicators. These were: overall habit strength (i.e. mean habit score over time); overall change in habit strength across study timepoints; the standard deviation of the first differences (i.e. whether the magnitude of differences between scores at consecutive timepoints varied across timepoints); and the ratio of the mean absolute second difference to the mean absolute first difference (i.e. a comparison between [a] average differences between scores at consecutive timepoints [‘first difference’] and [b] general trends across multiple ‘first differences’ over time [‘second difference’]).
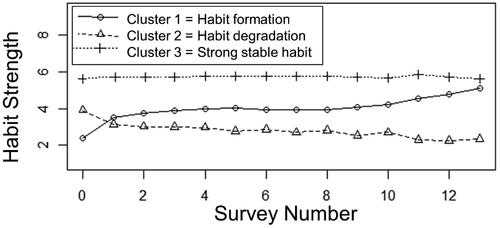
Factor analyses extracted three distinct habit trajectory clusters, which together explained 70% of variability in habit trajectory data (Factor 1 eigenvalue = 9.60, 42% variability explained; Factor 2 eigenvalue = 4.23, 19% variability explained, Factor 3 eigenvalue = 1.68, 9% variability explained). A fourth factor did not meet Friedman criteria (eigenvalue = 1.23, 7% variability explained). The parameter estimates that characterised the three clusters, as summarised across behaviours, are shown in the top half of , and average trajectory plots are in .
Table 2. Habit trajectory parameter measures, and frequencies and percentages of trajectories per behaviour.
We interpreted the first cluster to depict ‘habit formation’, with an overall increase in mean habit strength underpinned by initially steep increases followed by more gradual increases over time. The second cluster depicted ‘habit degradation’, with an overall decrease in mean habit strength underpinned by initially steep declines followed by a continual more gradual decline over time. The third cluster depicted ‘stable strong habit’, with values reflecting negligible changes in pre-existing strong habit over time. Overall mean habit strength was lowest for habit degradation and highest for strong stable habit clusters. The last two parameters showed less variability of change in first differences for stable strong habit relative to habit formation or degradation trajectories.
The bottom half of shows the frequency with which observed trajectories were categorised into each habit cluster group, for each behaviour. For all transmission-reduction behaviours, all three clusters were observed, with stable strong habit the most common cluster, and habit formation the second most common. Hypothesis 1 received mixed support: while habit formation was observed for transmission-reduction behaviours, stable strong habits unexpectedly emerged, whereas predicted stable negligible habit trajectories did not.
For transmission-conducive behaviours, habit degradation was the most common cluster. Surprisingly, habit formation was the second most common (coughing or sneezing into hands: 23.6%; making physical contact with others: 37.5%). Strong stable habit trajectories were also observed for coughing or sneezing into hands (23.4%), but were rare for making physical contact with others (<0.05%). Hypothesis 2 received mixed support: habit degradation was observed for both transmission-conducive behaviours, but stable strong habits were notable for only one behaviour, and stable negligible habits were not found.
Were changes in habit associated with behavioural engagement at later timepoints?
illustrates differences in early and late behavioural engagement in each behaviour across habit trajectory clusters. The lack of observed trajectories corresponding to stable negligible habits precluded testing of Hypotheses 3, 4 b and 4c. The following analyses were therefore largely exploratory and post-hoc in nature.
Table 3. Estimations of associations between habit trajectory clusters and early and late behavioural engagement.
Engagement in transmission-reduction behaviours
For handwashing for 20 seconds, people with stable strong habit showed greater early and later engagement than those who underwent either habit formation or habit degradation, and there was no difference between those undergoing habit formation and habit degradation in early behavioural engagement, but those who underwent habit formation showed greater later engagement than did those who underwent habit degradation. Models explained 11% and 13% of variability in early and late behavioural engagement, respectively.
For handwashing on entering home, those with stable strong habit showed greater early and late behavioural engagement than did those who underwent habit formation or habit degradation. There was no difference between those undergoing habit formation or habit degradation in either early or late behavioural engagement. Models explained 5% and 3% of variability in early and late behavioural engagement, respectively.
For maintaining physical distance, there were no differences in early behavioural engagement between habit trajectory groups; however, those with stable strong habit and those undergoing habit formation showed greater late behavioural engagement than those undergoing habit degradation. Models explained <1% of early behavioural engagement and 2% of late behavioural engagement.
Hypothesis 4a received mixed support. For all transmission-reduction behaviours, habit degradation trajectories were associated with lesser engagement at later timepoints than stable strong habit. However, for two transmission-reduction behaviours, those who subsequently degraded their habits also reported lesser engagement at early timepoints than did those with stable strong habit.
Engagement in transmission-conducive behaviours
For coughing or sneezing into hands, those with stable strong habit showed greater early and late behavioural engagement than did those who underwent habit formation or habit degradation. There was no difference between those undergoing habit formation or habit degradation in early behavioural engagement. Those with stable strong habits displayed greater late behavioural engagement than those in other clusters, and those who underwent habit formation had greater late behavioural engagement than those who underwent habit degradation. Models explained 12% and 18% of variability in early and late behavioural engagement, respectively.
For making physical contact with others, there were no differences between trajectory clusters in early or later behavioural engagement. Models explained < 1% of variability in both early and late behavioural engagement.
Summary
Across all behaviours, those with stable strong habits tended to report greater behavioural engagement than those undergoing habit formation or habit degradation, at both early and late time periods. At early time points, there were no differences between those undergoing habit formation and those undergoing habit degradation. At later time points however, those undergoing habit formation tended to engage more in associated behaviour than those undergoing habit degradation.
Discussion
We tracked virus transmission-related habits, and the relationship between habit trajectories and later behavioural engagement, over six months of the COVID-19 pandemic in 2020. Across five behaviours – representing encouraged actions that reduce transmission (handwashing, physical distancing) and discouraged actions conducive to transmission (coughing or sneezing into hands, making physical contact with others) – three habit trajectory clusters were observed. These incorporated two patterns of change (habit formation, habit degradation) and one pattern of no change (stable strong habits). Although participants typically reported strong stable habits for transmission-reduction behaviours, the most common change patterns indicated habit formation for transmission-reduction behaviours, and habit degradation for transmission-conducive behaviours. Forming a habit was associated with greater subsequent behavioural engagement, and habit degradation was associated with reduced performance. Those who maintained pre-existing strong habits and those who formed habits engaged more in the target behaviours at later timepoints than did those for whom habit eroded. Findings suggest that promoting repeated, context-consistent performance of transmission-reduction behaviours, and disrupting the automatic enactment of transmission-conducive behaviours, may limit transmission during virus outbreaks. Additionally, observed formation of new transmission-reduction habits suggests that virus-control initiatives during future outbreaks may be able to reactivate habits developed in response to the COVID-19 pandemic.
We found that 49–65% of participants maintained pre-existing strong transmission-reduction habit, 23–30% formed new transmission-reduction habits, and 53–64% weakened old, transmission-conducive habits (). Participants who formed habits or maintained prior strong transmission-reduction habits were likely to subsequently engage more in associated behaviours at a later point than those who experienced declines in habit strength. Conversely, for one of the two transmission-conducive behaviours (coughing or sneezing into hands), those who demonstrated declines in habit subsequently engaged less often than did those who formed or maintained strong habits. The relationship between habit change and behaviour change over time is complex; for example, increased behavioural engagement in stable contexts promotes habit formation, which in turn promotes subsequent behavioural engagement (Gardner, Citation2015). Additionally, the timepoints from which behavioural engagement and habit trajectories were derived overlapped, such that behavioural engagement at the final two timepoints was regressed on to habit trajectories that were at least partly informed by habit data observed at the final two timepoints. Definitive conclusions regarding the directionality of effects cannot therefore be reached. Nonetheless, there were no differences in early behavioural engagement between those who subsequently underwent habit formation and those who underwent habit degradation, yet those who formed habits typically displayed greater engagement at later timepoints than did those whose habits eroded. This suggests that changes in behavioural engagement can be attributed to changes in habit, rather than pre-existing baseline differences between groups. Interestingly, we found that, for handwashing behaviours, participants with habit formation trajectories did not achieve the same high level of behavioural engagement at later timepoints as those who maintained strong pre-existing habits. This likely reflects that those for whom habit strengthened failed to attain the same strength levels as those with prior strong habits; across all behaviours, mean habit strength at each timepoint was higher in those with stable strong habits relative to those who formed habits. Overall however, our results support theory in suggesting that strengthening habit facilitates performance, and degrading habits disrupts performance (Rothman et al., Citation2009; Verplanken & Wood, Citation2006).
Several unexpected findings emerged. A sizeable minority reported weakening transmission-reduction habits (∼20%) or strengthening transmission-conducive habits (23–38%) over the study period. Our data cannot explain why these changes occurred. Erosion of ‘good’ habits may perhaps indicate that participants with pre-existing transmission-reduction habits began acting more attentively. People often misbelieve that deliberative performances are more effective than habitual responses, so mindfully undertake actions deemed important (Carden et al., Citation2017). The formation of ‘bad’ habits may perhaps reflect psychological reactance, whereby perceived threats to personal freedom from hygiene guidelines lead people to respond contrarily (Brehm, Citation1966). We assumed participants would be motivated to comply with public health guidance to control the spread of SARS-CoV-2 but, while public compliance has overall been high (Wright et al., Citation2021), studies have documented resistance to virus control measures seen to limit personal autonomy (Taylor & Asmundson, Citation2021).
While we did not aim to probe differences between behaviours in habit change, or habit-behaviour relationships, it was also puzzling that habit trajectories had no impact on behavioural engagement for making physical contact with others. Similarly, the variance in maintaining physical distance explained by habit was minimal. One possibility is that participants may have formed habits for distancing from strangers but found it challenging to distance from family or friends. Distinguishing between emotionally close and distant non-household members may perhaps have generated different results.
The formation or maintenance of transmission-reduction habits that we observed overall is encouraging for future virus-control initiatives. Unfamiliar virus-control behaviours can be cognitively effortful (Xie et al., Citation2020). By delegating control over such actions to environmental cues, forming habit should alleviate cognitive burden and so, as seen in our sample, enhance the likelihood of later action, even when motivation declines (Verplanken & Wood, Citation2006). Habitual transmission-reduction behaviours that serve valued post-pandemic goals (e.g. handwashing on entering the home, for personal hygiene) may be more likely to persist beyond the pandemic, aided by automaticity. Physical distancing is unlikely to persist indefinitely when the COVID-19 pandemic ends, given the cultural, social and interpersonal value of physical contact with others (Forsell & Åström, Citation2012). Nonetheless, the formation of physical distancing habits that we observed will likely leave valuable ingrained cue-response memory traces that persist after the pandemic (Humphreys et al., Citation1989). Such memory traces are thought to retain the potential to be recovered in future, if motivation to enact such behaviours returns (Gardner et al., Citation2021). Habit associations learned during the pandemic should, in theory, aid reactivation of physical distancing in any future outbreaks. In future virus pandemics, public health campaigns should promote performance of the same actions recommended during the COVID-19 pandemic, in the same settings. This would not only promote the development of new hygienic habits for younger population segments, but also encourage recovery of such habits acquired during the COVID-19 pandemic for others.
The habit degradation patterns we typically observed also hold promise for future outbreaks. Behaviours that facilitate virus transmission, such as coughing or sneezing into hands, were reportedly habitual for many participants, but they nonetheless were able to discontinue these actions during a pandemic. We assessed habit via reflections on behavioural performance (Verplanken & Orbell, Citation2003), which do not reveal the mechanisms through which habitual behaviour degraded. Habits may be disrupted by preventing the activation or enactment of habit impulses, or by overwriting the habit associations that generate such impulses (Gardner et al., Citation2020). Crucially, habitual behaviours disrupted by blocking impulses are thought to be more likely to re-emerge over the longer-term, whereas acquiring new habit associations in direct displacement of old ones offers a more lasting route to behaviour maintenance (Gardner et al., Citation2021). While further work is needed to assess the longevity of and mechanisms for declines in transmission-related habits, our findings demonstrate that habitual behaviours can be disrupted, even if only temporarily, during virus outbreaks. Future public health campaigns might facilitate the habit disruption process by training people in how to mindfully inhibit cued habit impulses in associated settings (Quinn et al., Citation2010), or avoid settings that trigger unwanted actions – though the ubiquitous nature of cues to many transmission-conducive actions, such as the urge to sneeze, or the presence of others, may render the latter impractical. Alternatively, people can be encouraged to displace unhygienic habits with more hygienic alternatives – such as coughing or sneezing into elbows instead of hands – so that new habit associations come to dominate over old ones.
Limitations must be acknowledged. Our convenience sample was predominantly female, and highly educated, so does not represent the general population. A worldwide survey conducted around the time that our study opened found that women, and those with more education, were more willing to adopt COVID-protective behaviours (Anaki & Sergay, Citation2021). This may explain why, for example, stable negligible habit trajectories did not emerge.
We operationalised ‘later’ behavioural engagement as the final two observations per participants, and so the specific dates on which these data were reported, and the total number of assessments, varied between participants. Our approach of aggregating data collected across multiple dates and stages of the pandemic obscures the potential influence of real-world events that occurred during the study period, such as the lifting of social restrictions. This limits the interpretability of the data. Furthermore, we assumed that, at the study outset, transmission-reduction behaviours would be either unfamiliar (e.g. physical distancing) or not performed consistently enough for habit to form (e.g. handwashing on returning home). Yet, participants most commonly reported pre-existing strong enduring habits for transmission-reduction behaviours. Although those with habit change trajectories posted notable differences in habit between the first and second timepoints, our study – which launched in April 2020, after many participating countries had mandated COVID-19-related restrictions (Hale et al., Citation2021) – may have begun too late to capture pandemic-related changes in habit for many participants. Relatedly, sizeable habit differences found between the first two timepoints among those with habit change trajectories raise the possibility that survey completion may have prompted changes in behaviour and habits (see Godin et al., Citation2008).
All data were self-reported, and participants may perhaps have been motivated to provide socially desirable responses, which may have overestimated apparent motivation towards and engagement in transmission-reduction behaviours, given widespread encouragement of COVID-preventive behaviours during the study period. Concerns have been raised around the validity of self-reporting automatic processes, such as habit, which occur outside of awareness (Hagger et al., Citation2015). Relatedly, conceptual overlap between behavioural engagement and our habit measure, which focuses on experiences of behavioural performance, may have artificially inflated observed associations, rendering those reporting maintaining or forming habits likely to report greater engagement. Other measures better discern habit and behaviour, but tend to be ill-suited to survey designs (Rebar et al., Citation2018). Finally, the five focal habits were assessed at varying levels of specificity, with some featuring cues (handwashing on entering home) and others not (e.g. handwashing for 20 seconds). Habit measures that exclude cues estimate the overall automaticity of action across contexts but provide little insight into the specific cue-action associations that underpin such actions (see Gardner et al., Citation2022). Some people may, for example, habitually wash their hands for 20 seconds when in the presence of others but wash less thoroughly when alone. Work is needed to identify the specific cue-action associations acquired in response to the COVID-19 pandemic, and so inform interventions to recover such habits in future outbreaks.
Our study showed that people who maintained pre-existing stable strong habits, or formed habits, were more likely to engage in those behaviours at later timepoints than those who experienced decreases in habit strength. Habit formation and disruption may offer important explanatory mechanisms for behaviour change and maintenance. Future virus-transmission behaviour change initiatives should promote performance in specific opportune contexts, to form ‘good’ habits or reactivate such habits learned during the COVID-19 pandemic, and promote transmission-reduction alternatives to transmission-conducive behaviours, to disrupt the ‘bad’ habits that can prevent long-term behaviour change.
Supplemental Material
Download MS Word (14 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Data and analysis code used in this study are available at https://osf.io/4g6sb/?view_only=9df363ec88a346c7b8076aed17b91df6.
Additional information
Funding
Notes
1 Although preferable to coughing or sneezing into the air, coughing or sneezing into hands was explicitly discouraged during the pandemic, in favour of coughing or sneezing into elbows, or tissues that are then hygienically disposed of.
2 There was no consensus on optimal physical distance when we designed the study; for example, the WHO (2020a) recommended maintaining at least 1m distance, whereas many European governments recommended at least 1.5m (see Hale et al., Citation2021). Two metres’ distance was chosen for the English and Italian language survey in line with UK government guidance when the study was designed (Hale et al., Citation2021). In the German survey, 1.5m distance was used in accordance with German recommendations (Bundeszentrale für gesundheitliche Aufklärung, Citation2021).
References
- Alzyood, M., Jackson, D., Aveyard, H., & Brooke, J. (2020). COVID-19 reinforces the importance of handwashing. Journal of Clinical Nursing, 29(15–16), 2760–2761. https://doi.org/10.1111/jocn.15313
- Anaki, D., & Sergay, J. (2021). Predicting health behavior in response to the coronavirus disease (COVID-19): Worldwide survey results from early March 2020. PloS One, 16(1), e0244534. https://doi.org/10.1371/journal.pone.0244534
- Bouton, M. E. (2000). A learning theory perspective on lapse, relapse, and the maintenance of behavior change. Health Psychology, 19(1S), 57–63. https://doi.org/10.1037/0278-6133.19.suppl1.57
- Brehm, J. W. (1966). A theory of psychological reactance. Academic Press.
- Bundeszentrale für gesundheitliche Aufklärung. (2021). Alltag in Zeiten von Corona: Schutz durch AHA + L+A [Every-day life in the time of Corona: Protection by DistanceHygieneMasks + Ventilation + App]. https://www.infektionsschutz.de/coronavirus/alltag-in-zeiten-von-corona.html
- Carden, L., Wood, W., Neal, D. T., & Pascoe, A. (2017). Incentives activate a control mind-set: Good for deliberate behaviors, bad for habit performance. Journal of the Association for Consumer Research, 2(3), 279–290. https://doi.org/10.1086/695325
- Centers for Disease Control and Prevention. (2020). Hand hygiene recommendations guidance for healthcare providers about hand hygiene and COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html
- Charrad, M., Ghazzali, N., Boiteau, V., & Niknafs, A. (2014). NbClust Package: Finding the relevant number of clusters in a dataset. Journal of Statistical Software, 61(6), 1–36. https://doi.org/10.18637/jss.v061.i06
- Danner, U. N., Aarts, H., & de Vries, N. K. (2008). Habit vs. Intention in the prediction of future behaviour: The role of frequency, context stability and mental accessibility of past behaviour. The British Journal of Social Psychology, 47(Pt 2), 245–265. https://doi.org/10.1348/014466607X230876
- Faul, F., Erdfelder, E., Buchner, A., & Lang, A.-G. (2009). Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. https://doi.org/10.3758/BRM.41.4.1149
- Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
- Forsell, L. M., & Åström, J. A. (2012). Meanings of hugging: From greeting behavior to touching implications. Comprehensive Psychology, 1, 13. https://doi.org/10.2466/02.17.21.CP.1.13
- Friedman, H. P., & Rubin, J. (1967). On some invariant criteria for grouping data. Journal of the American Statistical Association, 62(320), 1159–1178. https://doi.org/10.1080/01621459.1967.10500923
- Gardner, B. (2015). A review and analysis of the use of ‘habit’in understanding, predicting and influencing health-related behaviour. Health Psychology Review, 9(3), 277–295. https://doi.org/10.1080/17437199.2013.876238
- Gardner, B., Abraham, C., Lally, P., & de Bruijn, G.-J. (2012). Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. The International Journal of Behavioral Nutrition and Physical Activity, 9(1), 102. https://doi.org/10.1186/1479-5868-9-102
- Gardner, B., Lally, P., & Rebar, A. L. (2020). Does habit weaken the relationship between intention and behaviour? Revisiting the habit-intention interaction hypothesis. Social and Personality Psychology Compass, 14(8), e12553. https://doi.org/10.1111/spc3.12553
- Gardner, B., Phillips, L. A., & Judah, G. (2016). Habitual instigation and habitual execution: Definition, measurement, and effects on behaviour frequency. British Journal of Health Psychology, 21(3), 613–630. https://doi.org/10.1111/bjhp.12189
- Gardner, B., Rebar, A., & Lally, P. (2022). How does habit form? Guidelines for tracking real-world habit formation. Cogent Psychology, 9(1), 2041277. https://doi.org/10.1080/23311908.2022.2041277
- Gardner, B., Richards, R., Lally, P., Rebar, A., Thwaite, T., & Beeken, R. J. (2021). Breaking habits or breaking habitual behaviours? Old habits as an undervalued factor in weight loss maintenance. Appetite, 162, 105183. https://doi.org/10.1016/j.appet.2021.105183
- Godin, G., Sheeran, P., Conner, M., & Germain, M. (2008). Asking questions changes behavior: Mere measurement effects on frequency of blood donation. Health Psychology, 27(2), 179–184. https://doi.org/10.1037/0278-6133.27.2.179
- Hagger, M. S., Rebar, A. L., Mullan, B., Lipp, O. V., & Chatzisarantis, N. L. D. (2015). The subjective experience of habit captured by self-report indexes may lead to inaccuracies in the measurement of habitual action. Health Psychology Review, 9(3), 296–302. https://doi.org/10.1080/17437199.2014.959728
- Hale, T., Angrist, N., Goldszmidt, R., Kira, B., Petherick, A., Phillips, T., Webster, S., Cameron-Blake, E., Hallas, L., Majumdar, S., & Tatlow, H. (2021). A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nature Human Behaviour, 5(4), 529–538. https://doi.org/10.1038/s41562-021-01079-8
- Humphreys, M. S., Bain, J. D., & Pike, R. (1989). Different ways to cue a coherent memory system: A theory for episodic, semantic, and procedural tasks. Psychological Review, 96(2), 208–233. https://doi.org/10.1037/0033-295X.96.2.208
- Keller, J., Kwasnicka, D., Klaiber, P., Sichert, L., Lally, P., & Fleig, L. (2021). Habit formation following routine-based versus time-based cue planning: A randomized controlled trial. British Journal of Health Psychology, 26(3), 807–824. https://doi.org/10.1111/bjhp.12504
- Kruglanski, A. W., & Szumowska, E. (2020). Habitual behavior is goal-driven. Perspectives on Psychological Science, 15(5), 1256–1271. https://doi.org/10.1177/1745691620917676
- Kwasnicka, D., Dombrowski, S. U., White, M., & Sniehotta, F. (2016). Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychology Review, 10(3), 277–296. https://doi.org/10.1080/17437199.2016.1151372
- Lally, P., & Gardner, B. (2013). Promoting habit formation. Health Psychology Review, 7(Supp1), S137–S158. https://doi.org/10.1080/17437199.2011.603640
- Lally, P., van Jaarsveld, C. H. M., Potts, H. W. W., & Wardle, J. (2010). How are habits formed: Modelling habit formation in the real world. European Journal of Social Psychology, 40(6), 998–1009. https://doi.org/10.1002/ejsp.674
- Leffondré, K., Abrahamowicz, M., Regeasse, A., Hawker, G. A., Badley, E. M., McCusker, J., & Belzile, E. (2004). Statistical measures were proposed for identifying longitudinal patterns of change in quantitative health indicators. Journal of Clinical Epidemiology, 57(10), 1049–1062. https://doi.org/10.1016/j.jclinepi.2004.02.012
- Marien, H., Custers, R., & Aarts, H. (2019). Studying human habits in societal context: Examining support for a basic stimulus–response mechanism. Current Directions in Psychological Science, 28(6), 614–618. https://doi.org/10.1177/0963721419868211
- Neal, D. T., Wood, W., & Drolet, A. (2013). How do people adhere to goals when willpower is low? The profits (and pitfalls) of strong habits. Journal of Personality and Social Psychology, 104(6), 959–975. https://doi.org/10.1037/a0032626
- Orbell, S., & Verplanken, B. (2010). The automatic component of habit in health behavior: Habit as cue-contingent automaticity. Health Psychology, 29(4), 374–383. https://doi.org/10.1037/a0019596
- Oster, Y., Michael-Gayego, A., Rivkin, M., Levinson, L., Wolf, D. G., & Nir-Paz, R. (2021). Decreased prevalence rate of respiratory pathogens in hospitalized patients during the COVID-19 pandemic: Possible role for public health containment measures? Clinical Microbiology and Infection, 27(5), 811–812. https://doi.org/10.1016/j.cmi.2020.12.007
- Qualtrics, X. M. (2005). Qualtrics. www.qualtrics.com
- Quinn, J. M., Pascoe, A., Wood, W., & Neal, D. T. (2010). Can’t control yourself? Monitor those bad habits. Personality & Social Psychology Bulletin, 36(4), 499–511. https://doi.org/10.1177/0146167209360665
- R Core Team. (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/
- Rabie, T., & Curtis, V. (2006). Handwashing and risk of respiratory infections: a quantitative systematic review. Tropical Medicine & International Health: TM & IH, 11(3), 258–267. https://doi.org/10.1111/j.1365-3156.2006.01568.x
- Rebar, A., Gardner, B., Rhodes, R. E., & Verplanken, B. (2018). The measurement of habit. In B. Verplanken (Ed.), The psychology of habit (pp. 31–49). Springer.
- Rothman, A. J., Sheeran, P., & Wood, W. (2009). Reflective and automatic processes in the initiation and maintenance of dietary change. Annals of Behavioral Medicine, 38(S1), 4–17. https://doi.org/10.1007/s12160-009-9118-3
- Sylvestre, M.-P., McCusker, J., Cole, M., Regeasse, A., Belzile, E., & Abrahamowicz, M. (2006). Classification of patterns of delirium severity scores over time in an elderly population. International Psychogeriatrics, 18(4), 667–680. https://doi.org/10.1017/S1041610206003334
- Taylor, S., & Asmundson, G. J. G. (2021). Negative attitudes about facemasks during the COVID-19 pandemic: The dual importance of perceived ineffectiveness and psychological reactance. PloS One, 16(2), e0246317. https://doi.org/10.1371/journal.pone.0246317
- Triandis, H. C. (1977). Interpersonal behavior. Brooks/Cole Pub. Co.
- Verplanken, B., Aarts, H., & Van Knippenberg, A. (1997). Habit, information acquisition, and the process of making travel mode choices. European Journal of Social Psychology, 27(5), 539–560. https://doi.org/10.1002/(SICI)1099-0992(199709/10)27:5 < 539::AID-EJSP831 > 3.0.CO;2-A
- Verplanken, B., & Melkevik, O. (2008). Predicting habit: The case of physical exercise. Psychology of Sport and Exercise, 9(1), 15–26. https://doi.org/10.1016/j.psychsport.2007.01.002
- Verplanken, B., & Orbell, S. (2003). Reflections on past behavior: A self-report index of habit strength. Journal of Applied Social Psychology, 33(6), 1313–1330. https://doi.org/10.1111/j.1559-1816.2003.tb01951.x
- Verplanken, B., & Sui, J. (2019). Habit and identity: Behavioral, cognitive, affective, and motivational facets of an integrated self. Frontiers in Psychology, 10, 1504. https://doi.org/10.3389/fpsyg.2019.01504
- Verplanken, B., & Wood, W. (2006). Interventions to break and create consumer habits. Journal of Public Policy & Marketing, 25(1), 90–103. https://doi.org/10.1509/jppm.25.1.90
- West, R., Michie, S., Rubin, G. J., & Amlôt, R. (2020). Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nature Human Behaviour, 4(5), 451–459. https://doi.org/10.1038/s41562-020-0887-9
- Wood, W., Mazar, A., & Neal, D. T. (2022). Habits and goals in human behavior: Separate but interacting systems. Perspectives on Psychological Science, 17(2), 590–605. https://doi.org/10.1177/1745691621994226
- Wood, W., & Rünger, D. (2016). Psychology of habit. Annual Review of Psychology, 67, 289–314. https://doi.org/10.1146/annurev-psych-122414-033417
- World Health Organization. (2020a). Modes of transmission of virus causing COVID-19: Implications for IPC precaution recommendations. https://apps.who.int/iris/bitstream/handle/10665/331616/WHO-2019-nCoV-Sci_Brief-Transmission_modes-2020.2-eng.pdf?sequence=1&isAllowed=y
- World Health Organization (2020b). COVID-19 technical mission of experts to the Republic of Belarus: 8–11 April 2020. https://www.euro.who.int/__data/assets/pdf_file/0004/440608/Belarus-Mission-Report-Executive-Summary.pdf
- Wright, L., Steptoe, A., & Fancourt, D. (2021). Patterns of compliance with COVID-19 preventive behaviours: a latent class analysis of 20,000 UK adults. Journal of Epidemiology and Community Health, 76(3), 247-253. http://dx.doi.org/10.1136/jech-2021-216876
- Xie, W., Campbell, S., & Zhang, W. (2020). Working memory capacity predicts individual differences in social-distancing compliance during the COVID-19 pandemic in the United States. Proceedings of the National Academy of Sciences of the United States of America, 117(30), 17667–17674. https://doi.org/10.1073/pnas.2008868117