Abstract
Objective
To further understand the barriers and facilitators to attending colonoscopy examination following a positive routinely offered stool test result, from the perspective of patients and Specialist Screening Practitioners (SSPs).
Methods
Qualitative semi-structured interviews were conducted. Participants (N = 32) were patients (n = 20) who, as part of the Bowel Cancer Screening Programme (BCSP) in England, were invited to attend a colonoscopy examination, and SSPs (n = 12), who worked for the BCSP in England. Framework analysis included inductive and deductive coding.
Results
Anxiety was as a key barrier cited by patients and SSPs, arising from the moment the patient received the invitation letter. Notably, procedural-related anxieties centred upon the fear of pain and discomfort and test invasiveness. The role of family, friends and the SSP were recognised by patients and SSPs to facilitate participation. Many patients, yet not SSPs, emphasised an obligation to attend all medical test invitations.
Conclusion
Practically orientated strategies suggested by patients and SSPs address the patient barriers identified. These include earlier information to patients on the option of sedation for pain relief, earlier notification of potential financial support for patients unable to fund their own travel costs, and fewer uses of the term cancer within written materials.
Introduction
Colorectal cancer (CRC), also known as bowel cancer is a leading cause of cancer morbidity and mortality worldwide, with 10% of all cancer cases diagnosed being CRC (Sung et al., Citation2021). It is the second most common cause of cancer death in the UK, accounting for 16,571 deaths yearly in the UK (Cancer Research UK, Citation2022). Organised asymptomatic CRC screening includes foecal immunochemical testing (FIT); a test that looks for traces of blood in a foeces sample, and follow-up colonoscopy examination; a flexible tube called a colonoscope with a camera attached, inserted into the large intestine (colon) to look for abnormalities. CRC Screening programmes are available in most European countries, Canada, regions in North and South America, Asia, and Oceania (Schreuders et al., Citation2015). The FIT is the most widely used screening test worldwide, producing increased participation rates and the detection of positive results compared with other tests like the guaiac foecal occult blood test (Navarro et al., Citation2017). If a patient receives a positive FIT result, in many national screening programmes, they will be invited to a follow-up colonoscopy (Navarro et al., Citation2017). Colonoscopy is generally considered the gold standard for the detection of colorectal neoplasia and has been associated with long-term (20–30 years) reduction in CRC mortality (Nishihara et al., Citation2013).
Inadequate follow-up of a positive FIT result with a colonoscopy examination has the potential to undermine the effectiveness of screening programmes in reducing CRC morbidity and mortality. Based on an international survey of 35 FIT screening programmes, Selby and colleagues (Citation2021) reported a mean proportion of 79% (ranging from 39% to 100%) of participants with a positive FIT attending colonoscopy as a follow-up examination test.
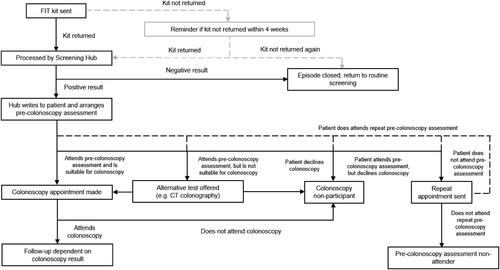
Colonoscopy examination as a diagnostic test, following a routinely offered positive FIT result, is provisioned by the National Health Service (NHS) in England as part of the Bowel Cancer Screening Programme (BCSP). Specialist Screening Practitioners (SSPs) play a key role as nurses who provide support and advice to FIT-positive patients, assessing patient suitability for colonoscopy examination. See for an overview of the patient colonoscopy examination pathway and the SSP role within this pathway.
Figure 1. The colonoscopy examination pathway. Note: Illustrates the colonoscopy pathway of the typical patient flow through the screening programme and the involvement of the Specialist Screening Practitioner (Kerrison et al., Citation2021, adapted from Plumb et al., 2017).
Empirical evidence on barriers to CRC screening include several systematic and rapid reviews among practitioners or patients regarding colonoscopy examination for primary CRC screening (Green et al., Citation2008; Kerrison et al., Citation2021; McLachlan et al., Citation2012). Previous studies and reviews have focused largely on colonoscopy as a primary screening test, with only two studies looking at barriers to colonoscopy as a follow-up test for a positive stool-based test result (Bertels et al., Citation2020, Citation2022), specifically, neither of these two studies were conducted in England. The current study is therefore novel given it investigated patient barriers and facilitators to colonoscopy as a follow-up test as opposed to as a primary screening examination, which has never been investigated through qualitative research methods in England before. The current study is the first to continue and extend this work provided by Kerrison et al. (Citation2021) by incorporating and comparing patient to SSP known barriers and facilitators. Kerrison and colleagues (Citation2021) investigated the barriers to colonoscopy attendance following a positive FIT result, from the viewpoint of SSPs. Patient concerns about the procedure, bowel preparation, and pain and discomfort were frequently cited by Kerrison and colleagues (Citation2021), as psychological factors including emotional responses during the assessment, anxiety and denial about the accuracy of the FIT result. Furthermore, Mog et al. (2022) interviewed 17 gastroenterology providers and staff, reported perceived patient barriers included concerns about the safety and invasiveness of the procedure, patient embarrassment and lack of social support.
While a useful first step, Kerrison et al. (Citation2021) and Mog et al.’s (2022) research may not have fully captured patient barriers, as there may be some, or many barriers, patients do not disclose to health care professionals. Inclusion of patients within the current study allowed for direct accounts of the barriers faced to be captured, and it was deemed likely that patients who attended screening would share other issues, not discussed at the time with their SSP. It was also anticipated that patients would provide greater insight into the facilitators that motivated and enabled them to attend a colonoscopy examination.
Patient questions within the interview schedule were informed by the Theoretical Domains Framework (TDF) (Atkins et al., Citation2017), whereby each question and prompt was mapped to one or more of the domains ahead of data collection. As guided by Michie et al. (Citation2005) this facilitated a comprehensive assessment of the determinants of the barriers to and facilitators of behaviour change, allowing questions and prompts to gain a broad understanding of the barriers and facilitators patients experienced. A recent review by McGowan at al. (2020) reported many other qualitative studies (n = 38) to have also used the TDF to inform data collection.
The current study aimed to:
undertake qualitative interviews to advance our understanding of the barriers and facilitators to attending colonoscopy examination, following a routinely offered positive FIT result, from both the perspective of patients and SSPs.
provide key procedural recommendations for consideration to reduce patient barriers which specifically focus on improving the NHS information and service provided to patients invited to attend further tests for CRC detection.
Methods
Participant eligibility criteria
Patients were members of the public who at bowel cancer screening age (60–74 years) had received an invitation to attend a colonoscopy examination (within the last 10 years), following a positive routinely offered stool test result. Both patients who had accepted this invitation and attended a colonoscopy examination and those patients who had declined this invitation were eligible participants. SSPs were employed by (or had been within the last 12 months) the NHS BCSP in England in which they support patients referred for a colonoscopy. Both patients and SSPs were able to speak and understand English and had the capacity to consent to the interview. All interested participants were sent a participant information sheet (explaining the purpose of the study) and consent form to read. For those who wished to proceed, a discussion via email took place to allow the researcher to check the participant’s eligibility. Approval was obtained from the University of Leeds Ethics committee (Reference: PSYC-134). None of the participants dropped out or withdrew from the study. The reporting of the current study adheres to the COnsolidated criteria for REporting Qualitative (COREQ) guidelines (Tong et al., Citation2007)
Sampling and recruitment
Patients
A variety of social media platforms were used with Facebook’s local community forums, and bowel cancer support groups found to be the most responsive. Leaflets were sent to members of the public living in deprived and ethnic minority communities in the North of England, issued with food parcels and on newsletters. To aim to achieve ethnic diversity in sample with regards to patient characteristics, advertisement also took place on a local Asian radio station within the North of England.
Specialist screening practitioner
Snowball sampling via word of mouth was used to recruit SSPs, first initiated via the social media platform, Twitter. No recruitment of SSPs took place via formal NHS communication channels.
The research team
The research team consisted of four researchers with an average of 13 years in academia and applied health psychology research. The team are highly experienced in researching cancer screening behaviours using various qualitative and quantitative research methods. All members of the team are non-clinical and have no direct lived experience of being invited to or have attended a colonoscopy examination for any medical reason.
Data collection
Semi-structured interviews were conducted by (ET). Topic guides were broken down into the timeline of events known to occur for patients, from receipt of the initial invitation to receiving their colonoscopy test result. The patient interview questions and prompts were informed by and mapped to the Theoretical Domains Network (TDF) (Atkins et al., Citation2017) to gain a comprehensive coverage and understanding of barriers and facilitators. Furthermore, the interview was structured to allow patients to easily share their experiences as a journey they had recently undertaken (see Supplementary Interview Guide). Due to the reports of improved quality of interviews conducted online regarding sensitive health related topics (Thunberg & Arnell, Citation2021) and Covid restrictions on face-to-face data collection, interviews were conducted and audio-recorded by the researcher (ET): via video call (in homes or private office spaces) or telephone, depending on the participant’s preference (field notes were not taken during and or after the interviews). Patients gave their consent and completed a participant demographics form together with the researcher who recorded responses before the interview began. Patients were given a £20 AMAZON voucher as a thank you for their time and contribution.
Data analysis
Data analysis was begun in parallel with data collection, to inform subsequent data collection and for the researchers to determine when sufficient data saturation was achieved to address the research questions. Framework analysis followed an iterative process in accordance with the 7 stage guidelines outlined by Gale et al. (Citation2013) and as described below.
The initial development of codes
Stage 1: Transcription. Verbatim transcription of the interviews was carried out by the primary researcher (ET), who also conducted the interviews. Stage 2: Familiarisation with the interview data. Transcripts were read and re-read, and handwritten reflections of initial thoughts and observations were captured in the page margins by the primary researcher (ET). Stage 3: Coding. Codes were developed to help describe and classify the data with reference to the research questions (i.e. a sentence or passage may be labelled ‘Level of cancer fear’ or ‘Early detection of cancer’). Two researchers (ET, RSK) initially independently developed ideas for codes using the same sample of 6 transcripts (3 patient, 3 SSP). Codes were generated inductively (i.e. from the data), but also by using Kerrison et al.’s (Citation2021) coding framework to assist with this (i.e. codes were used/adapted from Kerrison et al.’s list of codes as and when relevant to the current data). Stage 4: Development of a working analytical framework. Researchers (ET, RSK) met to compare their independently generated ideas for codes and through discussion consensually agreed on a working analytical framework (i.e. a ‘final’ set of 86 code names and the meaning of each).
The application of codes
Stage 5: Applying the analytical framework. The primary researcher (ET) then applied the agreed-upon codes to all transcripts. Where a new transcript was judged to contain text that could not be satisfactorily coded using the existing codes, new code(s) were created, 14 new codes in total were created. The transcript number at which new codes were developed was logged. The researcher (ET) subsequently revisited all transcripts to apply the new code(s) if relevant.
The use of the coded material to develop themes
Stage 6: Charting data into the framework matrix. The data were charted into a framework matrix, to provide a summary of the transcript material assigned to each code per participant (i.e. some cells could be blank should no material exist in a transcript labelled with that code). All researchers (ET, RSK, DBOC, LA) then used the charted framework matrix, and examination of interview transcripts or excerpts, to help develop themes. All stages of coding and data analysis were carried out in MS Excel. Stage 7: Interpreting the data. Themes were developed to delineate key messages in the data relevant the research questions. Data interpretation involved making comparisons between the barriers and facilitators reported by patients and SSPs. Theme development was iterative and involved all researchers, who reached a consensus through discussion on the final content and organisation of themes.
Rigor
The current study was guided by four fundamental dimensions of rigor for qualitative work, according to the Trust, Auditability, Credibility and Transferability (TACT) framework (Daniel, Citation2019). A description of each of the four dimensions according to Daniel (Citation2019) and how the current study specifically applied these is included in Supplementary Table 2. As requested during peer-review, a different researcher (RSK) to the primary researcher (who undertook stage 5 described above) judged the comprehensiveness of the final analytical framework (i.e. the final 100 codes developed after applying the initial/working coding framework to all transcripts). The researcher (RSK) independently applied the final code list to two transcripts (different to the original 6 used to develop the initial/working coding framework), and judged it to be sufficient (i.e. no new codes were required to adequately label the transcripts).
Results
Participant characteristics and data collection
Patient and SSP numbers and characteristics are summarised in . Interviews ranged from 29 to 76 min. Only patients who accepted the invitation and attended a colonoscopy examination were recruited, meaning no patients who chose to decline the invitation to attend further tests were interviewed. No participants dropped out or decided to withdraw their data. All data were collected by one researcher (ET) over a 6-month period, from December 2020 to May 2021.
Table 1. Participant numbers and characteristics (N = 32).
Description of themes
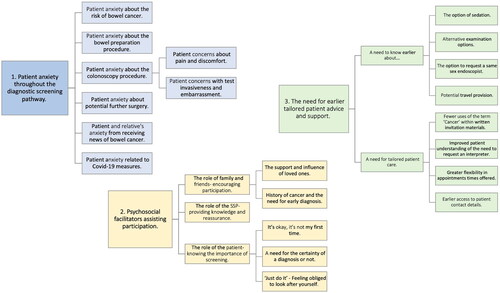
Based on the data analysis of barriers and facilitators coded, three key themes with subthemes were developed: (1) patient anxiety throughout the colonoscopy pathway, (2) psychosocial facilitators assisting participation, and (3) The need for earlier tailored patient advice and support (see ).
Theme one
Patient anxiety throughout the colonoscopy pathway
Most patients and SSPs reported feelings of anxiety from the moment they (patients) received the invitation letter to attend further tests. Patient anxiety continued to be raised as a key barrier throughout all stages of the colonoscopy examination.
“I was quite shocked and obviously it made me anxious.” P4
“They are instantly worried.” SSP2
Patient anxiety about the risk of bowel cancer
For some patients, a fear of having bowel cancer was triggered on immediate receipt of their invitation letter. Likewise, SSPs reported patients read the word cancer on the letter and jump to conclusions. Depending on the patient’s level of cancer fear, it was thought that this could inhibit or assist patient participation. Anxiety levels were reported to be lower in patients that had no symptoms or who provided alternative explanations, such as piles.
“I didn’t think it was cancer, but that was the first thing that came into my mind.” P6
“Someone who sees the word cancer, that’s it, you see that C bomb dropped, that’s it…I find people tend to go into sort of overdrive.” SSP12
“One part of me’ I’d obviously read the letter thinks ‘9 out of 10 abnormal so just piles’ which I did have piles ‘or polyps, but the other part is worried.” P13
SSPs and patients recognised that existing written materials were designed to reduce patient anxiety, by providing statistics on the low levels of bowel cancer risk. Some SSPs explained that an optimal level of reassurance in written materials is impossible to achieve, given its dependence on the patient’s own anxiety levels at the time of reading.
“I have to say reading the leaflet that came with it, was quite reassuring.” P4
“The problem is, you don’t want people to get a letter and to absolutely terrify them, but then you don’t want it to give them more reason to think that they don’t need to come and have the test.” SSP3
Patient anxiety about the bowel preparation procedure
Many patients tolerated the laxative drink well, surprisingly given their initial concerns about the bowel preparation. SSPs, in contrast, continued to view the bowel preparation as more unpleasant than the colonoscopy examination itself, for patients. Patients and SSPs equally recognised that hearing of other people’s unpleasant bowel preparation experiences contributed to these initial concerns, discouraging patient participation.
“I found it okay. I’ve spoken to some people who say ‘Oh it’s horrible, it’s horrible’ but I didn’t mind it.” P16
“The prep generally is worse than having the procedure done. So, by the time you actually come into hospital to have your test done, you’ve been through the worst of it.” SSP2
Due to the laxatives patients had taken, concerns of a bowel accident enroute to the hospital were shared by some patients. Some patients were relieved and encouraged knowing that their appointment was in the morning having taken the laxative fluid the evening before.
“I think it’s a worry that I would probably think about if I wasn’t in the profession.” SSP1
“I don’t think I would like a colonoscopy in the afternoon. Having to have to take the bowel preparation stuff in the morning, because I wouldn’t want to be leaving the flat not certain that, that something else was suddenly going to appear.” P1
Patient anxiety about the colonoscopy procedure
Many patients and SSPs spoke of greater levels of anxiety about attending the procedure compared to their risk of bowel cancer, particularly the case in patients who had never had a colonoscopy before. Morning appointments were often reported by patients and SSPs to be preferred, particularly encouraging to those patients where it was their first colonoscopy. Many reported patient nerves on arrival for their colonoscopy, any delays in their waiting time increased their anxiety.
“I was probably more anxious about having the colonoscopy than having the result.” P12
“I was anxious because I was doing something that I have never done before.” P5
“I wake up, I think right I’m going. Where if it’s in the afternoon, I’m sat all morning thinking about it.” P3
“Some people are very quiet. Some people can be angry and often, just nervous is the most common.” SSP2
Anxiety about the colonoscopy procedure itself has been broken down into the following areas of concern, acting as barriers to patient participation raised by both patients and SSPs.
Patient concerns about pain and discomfort
For most patients, the expectation of pain and discomfort were often reported, by both patients and SSPs, to be greater than the pain experienced during the procedure. For those where it was their first colonoscopy, hearing painful colonoscopy experiences from friends heightened any initial anxiety, discouraging participation.
“You’re just terrified of what they are going to do and if it’s going to hurt… but there wasn’t any pain so…the unknown, you don’t know what they are going to do, do you.” P3
“[Patient says] ‘I was really worried, but it was a really painless procedure’.” SSP5
“She just said it was that painful that she had to have painkiller, and the painkiller didn’t do anything.” P5
The availability of pain relief was reported to reduce patients concerns and encourage participation. Yet SSPs explained that the option of sedation was not always available to patients, should they live alone, need to care for a family member, or have work commitments the next day. Patients interviewed did not however share such barriers concerning their living or work circumstances. Providing distractions during the test were reported by both SSPs and patients as effective ways to reduce the anxiety and pain experienced.
“If you think you’re going to get a bit anxious, tell them they’ll give you a sedative, you’ll feel fine.” P12
“You need somebody to look after you, if you have sedation. I believe that this is a barrier, because they say, ‘Oh I don’t have anybody then, I’m not going to be able to come.” SSP9
“I was able to look at the screen, to see what they were doing, that was a distraction.” P11
One patient’s experience of a previous painful colonoscopy fostered higher levels of anxiety and inhibited participation. Likewise, SSPs recalled similar patient examples.
“I made a mental note on paper that I was never going there again, and that was the last time I was having that.” P7
“You do get a few who’ve had bad experiences and they have found it uncomfortable before and obviously those we would try and explain to them that each colonoscopy can be very different.” SSP3
Patient concerns with test invasiveness and embarrassment
Concerns with test invasiveness were reported to inhibit patient participation by patients and SSPs, a greater issue for men than women. Childbirth, and being older in age may partially explain why women reported less embarrassment than men. Interestingly, one male went so far as to say the procedure was not something men should do, suggesting underlying reasons of homophobia.
“I’m 70 and I have had two children, there is not much that embarrasses me now!” P5
“The initial embarrassment of having your bottom exposed. You don’t do that sort of thing… it was a strange sort of thing to be doing.” P20
“‘I’ve got a camera being shoved up my backside, potentially by another man, hang on, woooh!’ it could be a homosexuality kind of thing.” SSP12
For one patient with a history of sexual abuse, the thought of having a colonoscopy caused high levels of anxiety. The patient and SSPs provided details of the personalised care provided to those (patients) who had previous experiences of sexual abuse, to reduce anxiety and assist participation.
“I was scared of my reaction to the colonoscopy, that I would have attacked somebody, or hit somebody. That was my fear…They arranged an all-female team, which I thought was amazing.” P14
“She just wanted me to hold her hand, and I think that was it.” SSP4
Patient anxiety about potential further surgery
A fear of the need for a colostomy stoma, should an operation to remove a tumour result in a stoma being required, was recognised as a potential barrier for other patients, yet not personally to those interviewed.
“I think it is other things like perforation, and stoma bags, which patients probably ask about more.” SSP2
“Better a bag than a body.” P19
Patient and relative’s anxiety from receiving news of bowel cancer
Patients and SSPs reported a mixture of emotions when they (patients) received news of bowel cancer. Often, patients and SSPs cited more concern about the reactions of loved ones.
“It tends to be the relatives that get upset, more than the patient themselves.” SSP7
“My main thing was, how on earth am I going to tell < wife’s name>. That was my main concern.” P18
Patient anxiety related to covid-19 measures
At the time of colonoscopy examination, the additional burden of having to adhere to Covid measures was experienced by many patients and SSPs, increasing patient anxiety and hindering participation.
“We’ve been so careful all the way through. I just felt very nervous, just going into the hospital situation.” P9
“A lot of people, say oh I’ll wait until I’ve had my vaccine.” SSP7
“Because of Covid you can’t have anybody with you. So, you’re on your own. Yeah, not good. I cried.” P14
Theme two
Psychosocial facilitators assisting participation
This theme considered the key facilitators for patient participation. The role of family and friends, the SSP, and themselves situated as the ‘patient’ were reported to influence patient’s decision. Given the continual involvement of family, friends and the SSP, patients reported these facilitators to occur throughout the colonoscopy examination pathway.
The role of family and friends—encouraging participation
The support and influence of loved ones
The reassurance provided by family and friends encouraged patient participation and lowered initial concerns of the risk of bowel cancer and procedural anxieties. Having similar attitudes to friends and the support of family members on the day of the procedure, both in terms of travel and whilst in hospital assisted patients.
“I spoke to one of my colleagues and he said, ‘Oh I’ve had one of them, no need to worry about that…it’s nowt, very little chance of anything being found, the percentage is so low’…so I thought, we’ll go and see what happens.” P17
“My brother is 70 this year. We’re of the same opinion, in family discussions, we talked about this.” P7
“No, my husband drove. I could have driven myself, but you know, he would have wanted to drive me to make sure it was alright, especially to drive me back, so he drove and waited.” P11
Coercion by family members was cited by almost all SSPs, who described instances of patients pressurised to have a colonoscopy. SSPs described how they intervened to remind relatives that it was the patient’s decision. Equally, a patient shared pressures to attend received from their spouse.
“I just say you’ve got to stop for a minute, this is about your relative and it’s about them they’re making the decision, not you, and if this does carry on, I am going to have to ask you to leave.” SSP5
“I can’t fight my wife, she made me do it. Nagging me to do it…She came with me, yeah. She made sure I went, to tell you the truth.” P20
History of cancer and the need for early diagnosis
Patients who have experienced cancer with a family member or spouse explained how this encouraged their participation. Patients acted quickly for the early detection and prevention of any potential cancers. Likewise, SSPs confirmed ‘having a family history of cancer’ to assist patient participation.
“My brother had died in 2006 at the age of 56 with rectal cancer, and so it was it was a no brainer really. I just went. I truly believe that early diagnosis is the key to anything.” P12
“My mother died of bowel cancer, so that sort of raised the awareness in me.” P15
“They say ‘oh my mom had it, my dad had it, or my brother, and the experience with them, they delayed it and you know, and then they found it at the final stage, and I don’t want this to happen to me’.” SSP8
The role of the SSP—providing knowledge and reassurance
Before attending the SSP assessment, many patients reported knowing little about bowel cancer screening. During the assessment patients reported gaining understanding of the procedure and associated risks, according to SSPs this assisted patient participation. Patients recalled feeling reassured both following the assessment and on the day of the procedure.
“I had no idea about how it would be performed. I didn’t know if it was one person or half a dozen.” P1
“They’ve come in saying they don’t want it, but actually maybe they do want it, and they just need that bit more information.” SSP5
“She’d gone through everything from start to finish. She was just so reassuring about it, and I knew I could call her if I have any questions.” P2
“Those nurses, fantastic, in that room. They really put you at ease.” P8
The role of the patient—knowing the importance of screening
It’s okay, it’s not my first time
Patients who had previously attended medical or screening tests, had a medical work background or gone through childbirth demonstrated knowledge of the purpose and benefit of further screening tests, assisting in their participation. A patient’s medical background was not discussed by SSPs.
“Well, I had no hesitation, but you see, I suppose it’s partly to do with my background, in that I knew it was important.” P12
“It’s an alien environment. The whole thing is, but for me, it’s not an alien environment really.” P4
A need for the certainty of a diagnosis or not
Many patients explained that their reason for participation was due to a need for the certainty of a diagnosis or not, providing peace of mind. Similarly, a few SSPs shared their understanding and appreciation of patients’ innate need to know either way.
“Just to find out what was what. If you don’t go you don’t find out. And if you don’t find out what it is then the worst can happen. If you don’t go and find out, it could become untreatable.” P16
“I thought, no, I need to have it, because if I don’t have it, I would worry.” P13
“That need to know, I think, just being human. We need to know what the answer is.” SSP7
‘Just do it’—feeling obliged to look after yourself
Almost all patients demonstrated an obligation to attend anything medical or health related. Patients did not view their invitation as optional, given their initial participation. Many patients put their concerns or other priorities to one side, focusing on the necessity of medical-related tests. In comparison, a patient’s obligation to attend medical tests was not reported by SSPs.
“I just did it. I didn’t think, have I to, or haven’t I to. I just met this nurse, I got on with it!” P3
“If you’ve got a result, then I don’t see that as optional, I see that as you’ve got to do something about it. That was my view, I need to do something about it.” P10
“I’m just one of these that if they say something has got to be done, it’s got to be done, regardless of whether I feel a little bit apprehensive about it. This is all about my well-being." P2
Theme three:
The need for earlier tailored patient advice and support
This theme considered the timing of and need for tailored advice and support to further encourage patient participation. According to SSPs and patients, patient barriers were currently addressed during the SSP assessment, not earlier in the colonoscopy pathway. SSPs perceived patient nonattendance to be greater at the initial assessment stage, indicating a requirement for the earlier provision of advice and support.
“We have far more Do Not Attends (DNAs) for patients who are coming in for assessments. Then, once they’ve come for the assessment, generally, they come for the colonoscopy.” SSP1
A need to know earlier about…
The patient knowing earlier in the colonoscopy pathway of the options available to them was suggested by patients and SSPs to reduce anxieties, overcome accessibility issues, and assist participation.
“Maybe they don’t, at this stage, know enough about it, you don’t get to find out really what it is, until you go to the nurse, do you.” P12
The option of sedation
It was not until the assessment that patients and SSPs cited concerns raised of expected pain and discomfort. The potential administration of sedation is briefly mentioned in the booklet sent to patients, however to reduce immediate concerns of pain and discomfort and encourage participation it was suggested that the invitation letter signposts to patients the option of sedation.
“She effectively talked to me about what the procedure was, how it worked. What my options were in terms of sedation and pain relief.” P15
“If people think it’s going to hurt them, they might not go… maybe if people knew they could have a sedative right from the beginning, they might go.” P12
Alternative examination options
It was not until the assessment that patients and SSPs cited discussions of co-morbidities, previous unpleasant medical experiences, or concerns of test invasiveness. Alternative examination methods (a Computerised Tomography Colonography) was cited by a patient to be briefly mentioned in the booklet.
“I didn’t want the test, because of what happened previously, so I rang them up. I spoke to a nurse.” P7
“In the initial stage. You shouldn’t be able to say to people, you need to go for colonoscopy, if there are alternatives, they should be offered it, definitely. Or they should know that there are alternatives.” P14
The option to request a same sex endoscopist
According to SSPs prior to the assessment most patients had no initial awareness of the option to have a same sex endoscopist. SSPs and one patient questioned how many individuals immediately decline further tests, without sharing their reason or making specific requests of the screening team.
“Woman in Muslim cultures they don’t want to be scoped by a male endoscopist. They want a female endoscopist, which we make arrangements for that.” SSP8
“She’d had some kind of sexual abuse experience, which is why she particularly wanted a woman.” SSP3
“A cultural, kind of like a barrier really. They don’t ever really say what it is, but we do find that sometimes they just don’t participate.” SSP6
Potential travel provision
According to SSPs the assessment is the first opportunity a patient has to request financial support with travel costs. To attend this assessment, it was recognised by SSPs that the patient would need sufficient funds to travel. For the invitation letter to notify patients of potential financial support with travel costs, SSPs advised that funding would need to be sourced at a programme level. Patients interviewed recognised this to be an issue for others (not themselves) in participation.
“Some people don’t have money, and I know it’s incredible in this day and age to think that somebody can’t get to a place because of the money.” P12
“On a case-by-case basis, we can make an argument for this person to be given a funded taxi…a few occasions where that’s happened, but it puts a lot of work on to the SSP to actually make that argument, fire off all those emails, collate everything, arrange the taxi, it’s not a streamlined process.” SSP11
A need for tailored patient care
Many patients recognised the tailored information they had received from their SSP. SSPs explained that the need for information was very individualised, with some patients preferring to know very little indeed about the procedure.
“She’d gone through everything from start to finish. She was just so reassuring about it, and I knew I could call her if I had any questions.” P2
“There’s only so much you can do, only so much information that you can give people without scaring them, that sort of fine line, between what’s enough and what’s too much information.” SSP6
Fewer uses of the term ‘cancer’ within written invitation materials
The inclusion of the word cancer both within the programme title (BCSP) and written materials was cited by SSPs and patients to heighten anxiety and inhibit patient participation. It was advised that written materials should be revised given the aim of a colonoscopy examination is to look for changes and abnormalities in the large bowel.
“They just see the word cancer and that’s… I mean if you think about all the other screening programmes that are out there, they don’t actually have cancer in the title.” SSP5
“You’re looking for abnormalities rather than cancer. I don’t think cancer should be on that letter anywhere. I think it should be abnormalities or irregularities or something. But not cancer, because that would put people off.” P14
Improved patient understanding of the need to request an interpreter
SSPs shared examples of patients who had arrived for their assessment without requesting an interpreter, leading to the rescheduling of their appointment. A few SSPs questioned whether the standard invitation letter was only issued to patients in English, requiring the patient to have local resources to help them interpret and know to request an interpreter. English was the first language of all patients interviewed; therefore, no patients had experienced language barriers.
“They don’t always call us, but they might not be able to read all the information on there, anyway. If their English isn’t very good.” SSP4
“[the patient] turned up and, like the son or daughter or the friend or whoever will turn around and say oh yeah, I’m happy to translate, and you go I’m now going to have to rebook this appointment.” SSP12
“I’m not sure whether they have this letter, sent out in their native language?” SSP10
Greater flexibility in appointments times offered
Due to the bowel cancer screening age extension to 56 years (as of 2021), SSPs noted that the increase in patients with work commitments will create greater need for appointment flexibility and the option of out-of-hour appointments. A few SSPs shared how their screening centres had started offering evening appointments for the colonoscopy procedure, but not for the assessment.
“With the age extension coming in, a lot of the younger people are going to still be working and I know that that is starting to become a factor.” SSP 11
“We do have evening appointments. We have a five to nine appointments, not for clinic but for colonoscopy. We are thinking about doing out of hours Saturday lists for colonoscopy.” SSP10
Earlier access to patient contact details
SSPs explained that it is not until the patient has given their consent at assessment that they have the patient’s contact details. Should earlier access to patient details be possible, SSPs suggested the use of text messages as a helpful reminder to patients of their assessment and for bowel preparation timings. Text reminders were not discussed with patients interviewed to gather initial reactions of their potential benefit.
“Until they come to you, we don’t know anything about them. We have no idea about their health, any problems or anything which you know which is really frustrating.” SSP10
“For some people it’s [text messages] going to remind them of their appointment…Text reminders to start your prep I would love that, that would be amazing.” SSP12
Discussion
This study is the first qualitative study to examine patient barriers and facilitators experienced in attending colonoscopy examination, following a routinely offered positive FIT result, from both the perspective of patients and SSPs. These findings corroborate and extend earlier work by Kerrison et al. (Citation2021) in SSPs only, and Mog et al. (2022) in gastroenterology providers strengthening the validity of known barriers and facilitators, while also providing a greater insight into facilitators, namely the role of family, friends and the SSP and how these social and professional influences have motivated and enabled patients to attend follow-up colonoscopy.
Study findings were developed into three key themes. (1) Patient anxiety throughout the colonoscopy pathway. Anxiety was frequently cited by patients and SSPs as a key barrier, arising from the moment the patient received the invitation letter to discuss further tests. Notably, procedural-related anxieties centred upon the fear of pain and discomfort and test invasiveness. (2) Psychosocial facilitators assisting participation. The role of family, friends and the SSP were recognised to assist and in some instances force participation. Almost all patients felt obliged to attend all medical test invitations and expressed a need for the certainty of a diagnosis or not. (3) The need for earlier tailored patient advice and support to lower anxieties, make earlier contact with patients, and reduce accessibility barriers such as travel costs. Suggestions made by SSPs and patients for this additional advice and support were mostly required earlier on in the colonoscopy pathway.
Findings from reviews by Yang et al. (Citation2018) and Travis et al. (Citation2020) similarly focussed on procedural-related anxieties in patients who had undergone a colonoscopy or flexible sigmoidoscopy, with alike concerns of bowel preparation, the procedure itself, and diagnosis of cancer. Recent charity campaigns have attempted to reduce the public’s anxieties about having a colonoscopy through online videos, fact sheets and leaflets (Bowel Cancer UK, Citation2022). Patients in the current study demonstrated a sense of obligation to act soon for the early detection and prevention of any potential cancers. Further to this, Bertels et al. (Citation2022) recently found that when a patient’s decision-making process to participate in a colonoscopy examination was immediate, this was associated with high-risk perception, worry, and emotional turmoil. Family influenced participation beyond the provision of practical and emotional support, first reported by Kerrison et al. (Citation2021) was again further evidenced by SSPs in the current study. There were several barriers and facilitators SSPs raised which were not reported by patients and vice versa. For example, cultural and language barriers to colonoscopy examination previously reported by Kerrison et al. (Citation2021), were highlighted in the current study as a patient barrier by SSPs. Patients interviewed in the current study did not however report any issues experienced with their own cultural beliefs. English was the first language of all patients interviewed; therefore, no patients had experienced language barriers. Most patients explained how they felt obliged to attend all medical tests facilitating their participation, this was not something reported by SSPs. For a full comparison of all individual barriers and facilitators raised by SSPs compared to those raised by patients, see Supplementary Table. This table categorises each barrier and facilitator coded according to the psychological, sociocultural, health-related, practical and Covid-related factors reported with Kerrison et al.’s, (Citation2021) coding framework.
Limitations
This study also has several limitations. (1) It was our intention to recruit patients who have accepted and declined an invitation to attend further diagnostic tests. Despite extensive methods of recruitment, the sample did not include patient decliners. Questions were included within the interview topic guides (see Supplementary Interview Guide) to specifically ask patients and SSPs why they thought other patients choose not to attend the SSP appointment/follow-up tests. Suggested reasons as to why patients do not attend further tests, were then analysed and coded within the data as barriers and facilitators. SSPs have regular contact with patients, this enables them to share valuable insights as to the reasons decliners report to them for not attending. (2) Nearly all patients were of White British or White Irish ethnicity. Recruitment of decliners and minority ethnic groups for health research is a common issue recognised and experienced by researchers unable to engage ‘hard to reach’ groups to find out why they are not accessing certain healthcare services (Rockliffe et al., Citation2018).
Recommendations and implications for future research
Future qualitative research should work with an ethnic minority group sample to establish to what extent the collective findings thus far are generalisable, allowing for the identification of additional barriers distinct to ethnic minority groups. Future qualitative work should also target patient decliners to understand the magnitude of key barriers identified in the current study, particularly the barriers surrounding patient anxiety. Based on findings outlined, summarises key recommendations for consideration to further encourage patient participation through the improvement of the information and service provided.
Table 2. Key recommendations for consideration to reduce patient barriers through the improvement of NHS procedural information and services provided to patients invited to attend further tests for CRC detection.
Consistent with recent recommendations for using the TDF in qualitative studies (McGowan et al., Citation2020) the current study adopted flexible and optimised use of the TDF. The TDF informed the patient interview questions, yet data analysis was guided by the framework method stages and recommendations set out by Gale et al. (Citation2013). This allowed codes to be derived from the data and not predetermined or restricted to the TDF. All recommendations suggested were obtained directly from the SSP and patient interviews, not from suggestions developed by the researchers through further analysis or consideration of barriers reported. It is recommended that future work is now informed by behaviour change techniques and their mechanisms of action; processes which influence behaviour (Carey et al., Citation2019; Connell et al., Citation2019) or the integrated screening action model (Robb, Citation2021) to identify effective theory-based behavioural interventions to overcome other barriers raised by SSPs and patients. To our knowledge, this is the most comprehensive single list of such recommendations and accompanying potential strategies for consideration. The strategies have the potential to improve future equality, diversity, and inclusion of patients attending a colonoscopy examination. For instance, earlier notification of potential financial support for patients unable to fund their own travel costs, improved patient understanding of the need to request an interpreter and having greater flexibility in appointments times offered. It is advised that future research findings and chosen strategies be externally audited for validation and further development with patients, SSPs, and programme managers to ensure they are both feasible and accepted by stakeholders prior to wider programme level rollout.
Conclusion
Inadequate follow-up of positive FIT has the potential to undermine the effectiveness of screening programmes in reducing CRC morbidity and mortality. Our findings provide in depth reports of procedural-related anxiety experienced by patients who, as part of the BCSP in England, were invited to attend a colonoscopy examination. Our findings suggest there are many practically orientated strategies for onward consideration, intended to improve the equality, diversity, and inclusion of patients attending a colonoscopy examination in the future.
Supplemental Material
Download MS Word (136.3 KB)Acknowledgements
The authors would like to thank the patients and Specialist Screening Practitioners recruited for their time and for sharing their experiences with us.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
Data availability statement
Authors agree to make data and materials supporting the results or analyses presented in their paper available upon reasonable request.
References
- Atkins, L., Francis, J., Islam, R., O’Connor, D., Patey, A., Ivers, N., Foy, R., Duncan, E. M., Colquhoun, H., Grimshaw, J. M., Lawton, R., & Michie, S. (2017). A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation Science, 12(1), 1–18. https://doi.org/10.1186/s13012-017-0605-9
- Bertels, L., Lucassen, P., van Asselt, K., Dekker, E., van Weert, H., & Knottnerus, B. (2020). Motives for non-adherence to colonoscopy advice after a positive colorectal cancer screening test result: A qualitative study. Scandinavian Journal of Primary Health Care, 38(4), 487–498.
- Bertels, L., Knottnerus, B., Bastiaans, L., Danquah, A., van, H., Dekker, E., & van, K. (2022). Decision‐making in screening positive participants who follow up with colonoscopy in the Dutch colorectal cancer screening programme: A mixed‐method study. Psycho-oncology, 31(2), 245–252. https://doi.org/10.1002/pon.5814
- Bowel Cancer UK. (2022, January 18).Going for a Colonoscopy. https://www.bowelcanceruk.org.uk/about-bowel-cancer/diagnosis/hospital-tests/going-for-a-colonoscopy/
- Cancer Research UK. (2022, January 18). Bowel Cancer Statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer
- Carey, R. N., Connell, L. E., Johnston, M., Rothman, A. J., de Bruin, M., Kelly, M. P., & Michie, S. (2019). Behavior change techniques and their mechanisms of action: A synthesis of links described in published intervention literature. Annals of Behavioral Medicine, 53(8), 693–707. https://doi.org/10.1093/abm/kay078
- Connell, L. E., Carey, R. N., de Bruin, M., Rothman, A. J., Johnston, M., Kelly, M. P., & Michie, S. (2019). Links between behavior change techniques and mechanisms of action: An expert consensus study. Annals of Behavioral Medicine, 53(8), 708–720. https://doi.org/10.1093/abm/kay082
- Daniel, B. K. (2019). Using the TACT framework to learn the principles of rigour in qualitative research. Electronic Journal of Business Research Methods, 17(3), 118–129.
- Gale, N. K., Heath, G., Cameron, E., Rashid, S., & Redwood, S. (2013). Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Medical Research Methodology, 13(1), 117–118. https://doi.org/10.1186/1471-2288-13-117
- Green, A. R., Peters-Lewis, A., Percac-Lima, S., Betancourt, J. R., Richter, J. M., Janairo, M.-P R., Gamba, G. B., & Atlas, S. J. (2008). Barriers to screening colonoscopy for low-income Latino and white patients in an urban community health center. Journal of General Internal Medicine, 23(6), 834–840. https://doi.org/10.1007/s11606-008-0572-6
- Michie, S., Johnston, M., Abraham, C., Lawton, R., Parker, D., & Walker, A; “Psychological Theory” Group. (2005). Making psychological theory useful for implementing evidence-based practice: A consensus approach. Quality & Safety in Health Care, 14(1), 26–33. https://doi.org/10.1136/qshc.2004.011155
- Mog, A. C., Liang, P. S., Donovan, L. M., Sayre, G. G., Shaukat, A., May, F. P., Glorioso, T. J., Jorgenson, M. A., Wood, G. B., Mueller, C., & Dominitz, J. A. (2022). Timely colonoscopy after positive fecal immunochemical tests in the Veterans Health Administration: A qualitative assessment of current practice and perceived barriers. Clinical and Translational Gastroenterology, 13(2), e00438. Epub ahead of print. PMID: 35060937. https://doi.org/10.14309/ctg.0000000000000438
- McGowan, L. J., Powell, R., & French, D. P. (2020). How can use of the Theoretical Domains Framework be optimized in qualitative research? A rapid systematic review. British Journal of Health Psychology, 25(3), 677–694.
- McLachlan, S. A., Clements, A., & Austoker, J. (2012). Patients’ experiences and reported barriers to colonoscopy in the screening context—a systematic review of the literature. Patient Education and Counseling, 86(2), 137–146.
- Navarro, M., Nicolas, A., Ferrandez, A., & Lanas, A. (2017). Colorectal cancer population screening programs worldwide in 2016: An update. World Journal of Gastroenterology, 23(20), 3632–3642. https://doi.org/10.3748/wjg.v23.i20.3632
- Nishihara, R., Wu, K., Lochhead, P., Morikawa, T., Liao, X., Qian, Z. R., Inamura, K., Kim, S. A., Kuchiba, A., Yamauchi, M., Imamura, Y., Willett, W. C., Rosner, B. A., Fuchs, C. S., Giovannucci, E., Ogino, S., & Chan, A. T. (2013). Long-term colorectal-cancer incidence and mortality after lower endoscopy. The New England Journal of Medicine, 369(12), 1095–1105. https://doi.org/10.1056/NEJMoa1301969
- Kerrison, R. S., Sheik-Mohamud, D., McBride, E., Whitaker, K. L., Rees, C., Duffy, S., & von Wagner, C. (2021). Patient barriers and facilitators of colonoscopy use: A rapid systematic review and thematic synthesis of the qualitative literature. Preventive Medicine, 145, 106413.
- Robb, K. A. (2021). The integrated screening action model (I-SAM): A theory-based approach to inform intervention development. Preventive Medicine Reports, 23, 101427. https://doi.org/10.1016/j.pmedr.2021.101427
- Rockliffe, L., Chorley, A. J., Marlow, L. A., & Forster, A. S. (2018). It’s hard to reach the “hard-to-reach”: The challenges of recruiting people who do not access preventative healthcare services into interview studies. International Journal of Qualitative Studies on Health and Well-Being, 13(1), 1479582. https://doi.org/10.1080/17482631.2018.1479582
- Selby, K., Senore, C., Wong, M., May, F. P., Gupta, S., & Liang, P. S. (2021). Interventions to ensure follow-up of positive fecal immunochemical tests: An international survey of screening programs. Journal of Medical Screening, 28(1), 51–53. https://doi.org/10.1177/0969141320904977
- Schreuders, E. H., Ruco, A., Rabeneck, L., Schoen, R. E., Sung, J. J., Young, G. P., & Kuipers, E. J. (2015). Colorectal cancer screening: A global overview of existing programmes. Gut, 64(10), 1637–1649. https://doi.org/10.1136/gutjnl-2014-309086
- Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. https://doi.org/10.3322/caac.21660.
- Thunberg, S., & Arnell, L. (2021). Pioneering the use of technologies in qualitative research–A research review of the use of digital interviews. International Journal of Social Research Methodology, 25, 1–12.
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042
- Travis, E., Ashley, L., Pownall, M., & O’Connor, D. B. (2020). Barriers to flexible sigmoidoscopy colorectal cancer screening in low uptake socio‐demographic groups: A systematic review. Psycho-oncology, 29(8), 1237–1247. https://doi.org/10.1002/pon.5443
- Yang, C., Sriranjan, V., Abou-Setta, A. M., Poluha, W., Walker, J. R., & Singh, H. (2018). Anxiety Associated with Colonoscopy and Flexible Sigmoidoscopy: A Systematic Review. The American Journal of Gastroenterology, 113(12), 1810–1818. https://doi.org/10.1038/s41395-018-0398-8