ABSTRACT
Background
Some physiotherapists find assessing and managing clients experiencing psychological distress challenging and are uncertain regarding the boundaries of the profession’s scope.
Objective
To map the approaches recommended for physiotherapists in scholarly literature, with respect to the assessment and management of clients experiencing psychological distress.
Methods
A systematic mapping review was conducted. CINAHL, APA PsycINFO, Embase, and Medline ALL databases were systematically searched for secondary and tertiary literature relevant to the research objective. Recommended approaches were extracted from each article and analyzed descriptively and thematically.
Results
3884 records were identified with 40 articles meeting the inclusion/exclusion criteria. Most recommendations related to identifying, assessing, and managing pain-related distress, with depression screening and referral also receiving some attention. Three approaches to detecting and assessing psychological distress were identified: 1) brief depression screen; 2) integrated suicide/nonsuicidal self-harm and depression screen; and 3) multidimensional screen and health-related distress assessment. Regarding the management of psychological distress the main approaches identified were: 1) education and reassurance; 2) cognitive-behavioral approaches; 3) mindfulness; and 4) case management.
Conclusion
While assessment and management of health-related distress by physiotherapists is commonly recommended, further guidance is needed to differentiate various forms of distress.
Introduction
In 1975, Emeritus Professor and prominent psychiatrist Beverley Raphael published an article in the Australian Journal of Physiotherapy arguing that physiotherapists, due to the nature of the clients with whom they work and whether employed in public or private practice, need to be prepared to support clients who are experiencing overwhelming feelings of anxiety, anger, sadness, loss, resentment, fear, or disappointment (Raphael, Citation1975). Despite almost 50 years having passed since the publication of Raphael’s paper and the knowledge that physiotherapists frequently encounter people experiencing psychological distress, it appears that many physiotherapists lack confidence in the assessment and management of clients experiencing psychological distress (Driver, Kean, Oprescu, and Lovell, Citation2017; Henning and Smith, Citation2022; Lucas and Parker, Citation2022; McGrath, Verdon, Parnell, and Pope, Citation2023; Singla, Jones, Edwards, and Kumar, Citation2015).
While there is no universally accepted definition of psychological distress, it is often described in terms of symptoms of depression and anxiety (Drapeau, Marchand, and Beaulieu-Prévost, Citation2012; Mirowsky and Ross, Citation2003; Phillips, Citation2009). However, focusing only on these symptoms fails to capture the entire spectrum of psychological distress, which may also include grief, rumination, feelings of vulnerability, despair, sadness, anguish, helplessness, fear, hopelessness, loneliness, worthlessness, and irritability (Laporte and Aita, Citation2021; Mirowsky and Ross, Citation2003). Psychological distress may also emerge in the presence or absence of a stressor (Drapeau, Marchand, and Beaulieu-Prévost, Citation2012; Ridner, Citation2004). When referring to psychological distress that is, at least in part, associated with a specific stressor, some researchers use more specific terminology such as trauma-, poverty-, illness-, or pain-related distress (Cano and Goubert, Citation2017; DePrince, Chu, and Pineda, Citation2011; Lo et al., Citation2011; Sharkey et al., Citation2018; Thomas et al., Citation2018).
Given the variability in the forms of psychological distress that can be experienced, it is unsurprising that physiotherapists have reported frequently encountering clients experiencing psychological distress associated with a range of different stressors, with illness/injury-, financial-, and bereavement-related distress (McGrath, Parnell, Verdon, and Pope, Citation2022; McGrath, Verdon, Parnell, and Pope, Citation2023). In total, the physiotherapists participating in the study by McGrath, Verdon, Parnell, and Pope (Citation2023) perceived that approximately 36 out of every 100 clients they encountered experienced some degree of psychological distress, of which almost half were perceived to be experiencing severe psychological distress. The frequency and variety of the forms of client psychological distress encountered pose a significant clinical challenge to physiotherapists, and this challenge is likely worsened by a lack of clarity around the role of physiotherapists in working with clients experiencing psychological distress (Lord, Citation2018; McGrath, Parnell, Verdon, and Pope, Citation2022; McGrath, Verdon, Parnell, and Pope, Citation2023; Ribeiro et al., Citation2022; van Dijk et al., Citation2023).
While physiotherapists should not attempt to subvert the role of mental health professionals, their exposure to clients experiencing psychological distress necessitates recognition of, and at least some involvement in the management of the distress (Connaughton, Citation2018; Watson and Kendall, Citation2000). According to the International Organization of Physical Therapy in Mental Health (IOPTMH), all physiotherapists should be able to engage with and explore the perspectives of clients experiencing distress, and assist them to navigate the mental health care system (Probst et al., Citation2020). Furthermore, as primary contact health professionals, physiotherapists have a responsibility to respond appropriately to presenting problems identified during the consultation, which may involve screening for psychological distress and considering its management within care planning (American Physical Therapy Association, Citation2023; Physiotherapy Board of Australia, Physiotherapy Board of New Zealand, Citation2015). The purpose of screening is generally described as identifying important areas which may need further evaluation (American Psychological Association, American Psychological Association Practice Organization Work Group, Citation2014; Franzen, Citation2003). While sometimes considered interchangeably with screening, assessment aims to identify and comprehensively understand the construct at issue (e.g. anxiety), including its severity and the broader context in which it is occurring (American Psychological Association, American Psychological Association Practice Organization Work Group, Citation2014; Franzen, Citation2003).
When faced with uncertainty in clinical practice, physiotherapists may find it useful to draw on clinical guidelines, approaches, protocols, pathways, and instruments to guide their practice (Almond, Zou, and Forbes, Citation2021; Djulbegovic, Hozo, and Greenland, Citation2011; Scurlock-Evans, Upton, and Upton, Citation2014; Timmermans and Angell, Citation2001; Woolf et al., Citation1999). While physiotherapists generally acknowledge the importance of drawing on the literature to inform their practice, barriers such as limited time and skills in locating, appraising, and extracting relevant information from research articles have been found to impede this process (Scurlock-Evans, Upton, and Upton, Citation2014). Lennon et al. (Citation2020) and Keefe, Main, and George (Citation2018) argued that there is a paucity of clear guidance to assist physiotherapists in assessing and managing clients experiencing psychological distress or mental illness. Consequently, there is a lack of clarity around the role and scope of practice of physiotherapists in supporting clients experiencing psychological distress (Lennon et al., Citation2020; Lucas and Parker, Citation2022; McGrath, Verdon, Parnell, and Pope, Citation2023; Ribeiro et al., Citation2022).
Cupler et al. (Citation2020) posited that the development of an “evidence map” may help improve the translation of research to practice by providing practitioners with a concise, and comprehensive clinic-friendly tool that summarizes the evidence. Rather than mapping evidence, the aim of this review was to systematically map recommendations for physiotherapists published in the scholarly literature regarding approaches to the identification, assessment, and management of clients experiencing psychological distress.
Method
Research design
A systematic mapping review methodology was adopted. According to Hansen, Præstegaard, and Lehn-Christiansen (Citation2021) systematic mapping reviews analytically describe and interpret the research field, rather than identify scientific evidence. Systematic mapping reviews are particularly well suited to practice-relevant review questions (Grant and Booth, Citation2009). The protocol for this systematic mapping review was registered with Open Science Framework on July 13th 2022 (McGrath, Pope, Parnell, and Verdon, Citation2022). As there are no reporting guidelines for systematic mapping reviews, the Preferred Reporting Items for Systematic Reviews and Meta-analyses Extension for Scoping Reviews (PRISMA-ScR) was used (Tricco et al., Citation2018). While the initial aim was to map recommendations published in any type of scholarly literature such as research reports, journal articles, research theses and clinical guidance articles, after familiarity with the nature and breadth of the literature was gained during the initial title and abstract screening, the scope of our review was narrowed to only include secondary and tertiary literature that provided guidance on approaches to the identification, assessment, and management of psychological distress for physiotherapists based on pragmatic (i.e. resource and time limitations) and methodological considerations. While the definitions of secondary and tertiary literature vary, in the context of this review, secondary literature refers to literature that involves interpretation, synthesis or evaluation of primary sources, while tertiary literature refers to literature that includes distillation and collection of primary and secondary sources, and these sources are often composed of commentary and discussion of literature (Howlett and Rogo, Citation2021). The reviewers concluded that mixing primary research articles with secondary and tertiary literature would complicate analysis and mapping. The recommendations from primary research articles we screened tended to relate to future research rather than clinical practice, limiting their relevance to this review. Furthermore, when clinical recommendations were included in primary research articles, they tended to be highly tentative and specific to the results of the particular study being reported. In contrast, clinical recommendations from secondary and tertiary literature tended to be more general and aimed at translating a broader range of knowledge or evidence to practice. Articles published between January 1, 1990 and May 30, 2023 inclusive were eligible for inclusion. The year 1990 was chosen as the start date of the search as the “1990s saw evidence-based practice emerge as a new paradigm” (Turner, Citation2001). While systematic mapping reviews share similarities with both umbrella reviews and scoping reviews, umbrella reviews only include systematic reviews and meta-analyses and scoping reviews typically include primary research (Aromataris et al., Citation2015; Paolo and Joaquim, Citation2018; Pham et al., Citation2014).
Eligibility criteria
The inclusion and exclusion criteria for the systematic mapping review () were developed using the Population/Concept/Context Framework (Peters et al., Citation2020). For the purpose of this review, VandenBos’s (Citation2015) definition of “approach” as a particular method or strategy used to achieve a goal or purpose was used. Based on the existing work of key authors in the area (Drapeau, Marchand, and Beaulieu-Prévost, Citation2012; Laporte and Aita, Citation2021; Mirowsky and Ross, Citation2003; Payton, Citation2009), psychological distress was defined as follows. Psychological distress is a subjective, unpleasant emotional state that may be transitory, episodic, or permanent. Psychological distress is often characterized by depressive and anxiety symptoms but may also include a range of other negative emotions such as anger, frustration, grief, rumination, obsession, and feelings of being isolated or vulnerable. Psychological distress exists on a continuum, ranging from low to very high levels of psychological distress. Psychological distress may occur in response to a specific stressor or multiple stressors, or it may emerge in the absence of a stressor. The emotional symptoms of psychological distress may in some instances be the same as symptoms related with mental disorders such as major depressive disorder, generalized anxiety disorder, and post-traumatic stress disorder.
Table 1. Inclusion and exclusion criteria.
Given the ambiguity around the scope of practice of physiotherapists in the identification, assessment, and management of psychological distress, the eligibility criteria were designed to ensure included articles provided recommendations that have been made explicitly for physiotherapy practice, to enhance understanding current perceived role boundaries for physiotherapists ().
Search strategy
The literature search was completed on May 30th, 2023, using the search terms reported in . The search terms were informed by the literature on psychological distress and a review of the controlled vocabulary used in the selected databases. A preliminary search of CINAHL (EBSCO) was conducted in order to pilot the search strategy. No amendments to the search strategy were required. After piloting the search strategy, CINAHL (EBSCO) was searched again, along with the databases of APA PsycINFO (Ovid), Embase (Ovid), and Medline ALL (Ovid). The search strategy used to query the Medline ALL (Ovid) database is presented in as an example, with the search strategies for the APA PsycINFO (Ovid), Embase (Ovid), and CINAHL (EBSCO) databases reported in Supplemental Material 1. A citation search and reference list screening of potentially relevant and included articles was performed. Additionally, the reference lists of two recent reviews conducted in the general topic area were screened (Heywood et al., Citation2022; Ribeiro et al., Citation2022).
Table 2. Search terms.
Table 3. Search strategy for Medline ALL on the Ovid platform.
Screening and selection methods
The citation details for literature identified via the search strategy were imported into EndNote (Version 20) and Covidence (https://www.covidence.org/). Once imported, duplicates were removed and the titles and abstracts each screened by a single reviewer (RLM or SS) with only clearly irrelevant articles excluded at this stage. Each article identified as potentially relevant was assessed against the eligibility criteria by two reviewers (RLM or SS) independently. Any inconsistencies were handled by a discussion between the reviewers (RLM or SS) and if resolution could not be achieved, a third reviewer was consulted. Review by a third reviewer was not required as all inconsistencies were resolved through discussion between RLM or SS. The results of the search, screening and selection processes were documented in a PRISMA flow diagram (Haddaway, Page, Pritchard, and McGuinness, Citation2022).
Data extraction, analysis and presentation
Data from the included literature were extracted using a data chart form (Supplemental Material 2). RLM performed data extraction, with SS reviewing the extracted data to confirm accuracy. Data analysis involved descriptive analysis, interpretive thematic mapping, and summarizing of the data. Zotero (version 6.0.19), and Microsoft Excel (version 365) were used for the descriptive analysis. Thematic mapping was informed by Iterative Thematic Inquiry as described by Morgan and Nica (Citation2020). As per Iterative Thematic Inquiry, RLM drafted preliminary themes based on knowledge of the literature, which was continually updated as new data (i.e. the articles identified) reinforced, challenged, or expanded understanding. Once all data had been extracted, coding of the data was used to evaluate the identified themes and ensure they were grounded in the data. Microsoft Excel (version 365) and NVivo (version 10) were used to aid the reviewers in the thematic mapping process. As per the systematic mapping review convention, critical appraisals of the included literature were not performed (Grant and Booth, Citation2009; Hansen, Præstegaard, and Lehn-Christiansen, Citation2021)
Results
Overview
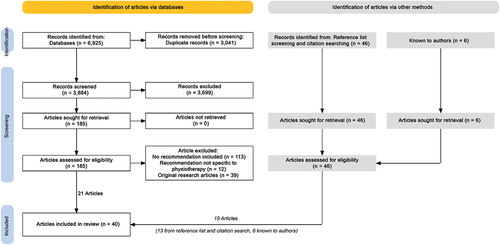
The search returned 6925 articles (). After the removal of duplicates (3041) the titles and abstracts of 3884 articles were screened for relevance. Of these, 185 articles were identified as potentially relevant. Subsequent full text review identified 21 articles as meeting the eligibility criteria of the systematic mapping review. Screening of the reference lists and a citation search using Scopus led to the identification of 13 further articles eligible for inclusion. Six other eligible articles known to the authors were also included in the review. In sum, 40 secondary or tertiary scholarly articles met the eligibility criteria and were included in the review.
Figure 1. Literature search, screening and selection flowchart (Haddaway, Page, Pritchard, and McGuinness, Citation2022).
summarizes the topics covered in the included articles and the contexts for which the recommendations they contained were intended. The majority of the articles (31/40) primarily offered guidance for physiotherapists on assessing and managing psychological distress in the context of people experiencing pain. Of these, eight articles focused on low back pain with other conditions of focus including: pelvic pain (3); pain associated with whiplash injuries (3); patellofemoral pain (1); cancer-related pain (1); and pain associated with temporomandibular disorders (1). The remaining articles provided guidance on the identification, assessment, and management of psychological distress in various other contexts including: acute care (1); post-intensive care (1); return to work rehabilitation (1); care of older adults (1); care of people with chronic physical illness (1); running activities postpartum (1); care of people with mild brain injuries (2); and care of people with depression (1).
Table 4. Recommended approaches identified in the review.
Types and distribution of included articles
The articles identified were published from 1999 to 2023, with a majority (22/40) having been published during or after 2018 (). The types of articles identified included thirteen perspectives, ten commentaries, nine reviews, four clinical practice guidelines, three masterclasses, and an editorial. One masterclass was published in two parts (Sterling, Citation2009; Sterling and Kenardy, Citation2008) and two perspectives were published as companion papers (Main et al., Citation2023, Citation2023). For the purpose of the current review, each article published in multiple parts or as companion papers was counted as a single article, given the close relationships between the components or companion parts. The articles were published across 13 journals, with over half published in either the Journal of Orthopaedic and Sports Physical Therapy (12) or the Physical Therapy and Rehabilitation Journal (11). The most common country listed as the address for the corresponding author was the United States (17). Of the authors whose clinical backgrounds could be ascertained (n = 122) there were 94 physiotherapists, 18 psychologists including one in training, one dual-qualified physiotherapist and psychologist, five physicians, two chiropractors including one in training, a counselor, and a nurse practitioner. With the exception of three articles (Cancelliere and Mohammed, Citation2019; Faulkner and Snell, Citation2023; Linton, Flink, and Vlaeyen, Citation2018) all were authored or coauthored by at least a physiotherapist. Fifteen articles were authored or coauthored by at least one psychologist.
Identification and assessment of psychological distress
All articles recommended the use of the clinical interview and/or a screening or assessment tool to identify and evaluate psychological distress. The screening and assessment tools identified in this review as recommended for use by physiotherapists are listed in . Screening for psychological distress was recommended and considered within the scope of physiotherapy practice in all included articles, for example:
Screening and addressing behavioral and mental health concerns is within the scope of the physiotherapy practice guidelines (Varela and Melvin, Citation2023).
Table 5. Screening and assessment instruments.
However, there was a consensus that the formal assessment of psychopathology is beyond the scope of physiotherapy.
It is rightly beyond the scope of physiotherapy practice formally to assess and treat specific psychological disorders (Watson, Citation1999).
It was suggested that physiotherapists have a responsibility to screen for depression and other mental disorders, such as generalized anxiety disorder and post-traumatic stress disorder (Donnelly, Brockwell, Rankin, and Moore, Citation2022; Smith et al., Citation2020; Varela and Melvin, Citation2023). Further limitations on the scope of physiotherapy in the assessment of mental health were highlighted by Harland and Lavallee (Citation2003). Harland and Lavallee (Citation2003) noted that without training, physiotherapists may not be able to use some questionnaires due to practical and legal issues:
Recognised training is necessary, both practically and legally, when dealing with questionnaires such as the Hospital Anxiety and Depression scale and Zung Depression Inventory (Harland and Lavallee, Citation2003).
In contrast, the assessment of psychosocial factors, including health-related psychological distress (i.e. mainly pain-related distress) was generally viewed to be within the scope of the physiotherapy profession. This assessment of health-related psychological distress allows physiotherapists to determine whether or not its management falls within their individual scope of practice.
The assessment of mental distress is another central aspect of pain research and treatment. When failing to measure these psychosocial factors, physical therapists lose the opportunity to address them in treatment when it is within their scope of practice (Vandyken and Hilton, Citation2017).
It was commonly acknowledged that there are differences between the scope of the physiotherapy profession in assessment of health-related distress, and the scope of an individual physiotherapist, for example:
It is acknowledged that each clinician has an individual scope of practice and may need to upskill or refer onwards for some components of multidimensional assessment/management (Rabey and Moloney, Citation2022).
Three general approaches to the identification and assessment of psychological distress were identified in this review and are now discussed in turn. Other approaches were also identified and are reported in .
Brief depression screen
An approach for physiotherapists recommended by several authors was to routinely screen for depression using a brief 2-item depression screen, followed by a longer screening tool when the 2-item screen is positive (Delitto et al., Citation2012; Spearing and Bailey, Citation2012; Vieira, Brown, and Raue, Citation2014; Wijma, van Wilgen CP, Meeus, and Nijs, Citation2016).
An efficient strategy is to complete the PHQ-2 and then complete the 7 remaining symptoms [in the PHQ-9] for those with a positive initial screen (Vieira, Brown, and Raue, Citation2014).
Due to its brevity, the brief 2-item depression screen could be verbal administered during the consultation or completed via self-report using the Patient Health Questionnaire-2 (PHQ-2).
Verbally Screening for Depression: 1. During the past month have you been feeling down, depressed, or hopeless? 2. During the past month have you been bothered by having little interest or pleasure in doing things? (Billek-Sawhney, Wagner, and Braun, Citation2014)
In addition to administering a longer depression screen, Delitto et al. (Citation2012) and Spearing and Bailey (Citation2012) suggested that physiotherapists should further explore the person’s depressive symptoms through the clinical interview, if competent.
A patient with a positive screening result for major or severe depressive symptoms should receive a focused clinical interview and should complete a full-length depressive symptom questionnaire (Delitto et al., Citation2012).
Billek-Sawhney, Wagner, and Braun (Citation2014) recommended a similar approach to screening for depression in the inpatient acute care setting. However, instead of completing the nine item Patient Health Questionnaire (PHQ-9) or a similar tool, Billek-Sawhney, Wagner, and Braun (Citation2014) recommended a third question, “is this something with which you would like help?” be added to the initial two screening questions, due to time constraints faced by physiotherapists in this context. Smith et al. (Citation2020) cautioned against the use of the 2-item depression screen with people experiencing post – intensive care syndrome, as the approach has not been validated with this population. While the above approach was described in reference to depression, Delitto et al. (Citation2012) suggested that a similar process could be used for clinicians who screen for other psychopathology (e.g. anxiety).
Integrated suicide/nonsuicidal self-harm and depression screen
As part of the depression screening, several authors also suggested that nonsuicidal self-harm and suicidal distress should be screened for (Delitto et al., Citation2012; Harrison, Thorp, and Ritzline, Citation2014; Simonds, Abraham, and Spitznagle, Citation2022; Stearns et al., Citation2021; Van Wyngaarden, Noehren, and Archer, Citation2019; Varela and Melvin, Citation2023; Vieira, Brown, and Raue, Citation2014). For example:
The screening for suicide occurs in part through assessment of depression (Varela and Melvin, Citation2023).
While not all authors who recommend the use of the PHQ-9, Patient Health Questionnaire Anxiety and Depression Scale (PHQ-ADS), Edinburgh Postnatal Depression Scale (EPDS), Beck Depression Inventory (BDI), or Zung Self-Rating Depression Scale (ZSDS) mentioned that these questionnaires ask about some aspect of suicidality, Varela and Melvin (Citation2023) and Simonds, Abraham, and Spitznagle (Citation2022) drew specific attention to this, within the PHQ-9 and EPDS, respectively:
The 9-item questionnaire … include[s] suicidal ideation … [Specifically] the sense of hopelessness is elaborated upon in the ninth question that screens for suicidal ideation … Higher scores on the ninth question prompts clinicians to discuss suicidal ideations with their patients, referring practitioners, and mental health providers (Varela and Melvin, Citation2023).
Any positive response to the suicidal ideation on item #10 [of the EPDS] (even with a score < 10) should be considered a red flag …. (Simonds, Abraham, and Spitznagle, Citation2022).
When suicidal ideation was identified, Billek-Sawhney, Wagner, and Braun (Citation2014) and Varela and Melvin (Citation2023) recommended that these thoughts be explored, such as if the person has a plan for suicide and means available to them:
Any messages expressed by the patient related to suicide must be followed up … Follow-up questions should explore whether the patient has a plan, has means/access, and has intent to harm. ‘Attempted suicide should be considered a cry for help’ (Billek-Sawhney, Wagner, and Braun, Citation2014).
Multidimensional screen and health-related distress assessment
An approach commonly recommended for physiotherapists practicing in pain, disability, and musculoskeletal settings involved conducting an initial screen of all patients attending with pain-related issues followed by further assessment of positive or concerning findings (Caneiro et al., Citation2022; Caneiro, Bunzli, and O’Sullivan, Citation2021; Hodges, Citation2019; Main et al., Citation2023, Citation2023; O’Sullivan et al., Citation2018; O’Sullivan, Smith, Beales, and Straker, Citation2017; Rabey and Moloney, Citation2022; Stearns et al., Citation2021). It was recommended that a multidimensional screening tool, such as the Örebro Musculoskeletal Pain Questionnaire (OMPQ), the Optimal Screening for Prediction of Referral and Outcome Yellow Flag (OSPRO-YF), the Keele STarT Back Screening Tool (SBST) or the Keele STarT Musculoskeletal Tool be employed as the use of multiple full-length unidimensional tools to assess several psychological constructs could result in an excessive administrative burden for the client and the physiotherapist during an initial consultation. To further reduce administrative burdens it was recommended by several authors that screening prior to the physiotherapy consultation be carried out using self-report questionnaires and multidimensional instruments, for example:
Multidimensional tools (eg, the OSPRO-YF and the Örebro Musculoskeletal Pain Questionnaire) are an attractive option for screening because they evaluate multiple dimensions of distress with low response burden (Stearns et al., Citation2021).
Relevant items from the multidimensional screening tools can subsequently be explored by the physiotherapist as part of the clinical interview and with unidimensional tools, exploring constructs relating to pain such as pain and/or movement-related fear and anxiety.
The use of a screening questionnaire prior to the interview provides the clinician with a perspective on the person’s pain and disability levels, cognitions, and emotions, providing opportunity for targeted exploration of their concerns within the interview (Caneiro et al., Citation2022).
Unidimensional tools, such as the Pain Catastrophizing Scale, the Tampa Scale of Kinesiophobia, and the Fear-Avoidance Beliefs Questionnaire were commonly recommended in the included articles (see ). The exploration of pain-related distress as part of a clinical interview was informed by several psychological theories and approaches, including the Fear Avoidance Model, the transdiagnostic approach, fear learning, and the Common-Sense Model (Bunzli et al., Citation2017; Caneiro et al., Citation2022; George and Zeppieri, Citation2009; Linton, Flink, and Vlaeyen, Citation2018). For example, Bunzli et al. (Citation2017) described how the Common-Sense Model can be used as a clinical framework to assess pain-related fear. While the Common-Sense Model primarily explores illness representations, the construct referred to as emotional response requires specific questioning to identify and characterize pain-related distress (Caneiro, Bunzli, and O’Sullivan, Citation2021):
How does the pain make you feel? How do you feel about losing the ability to do things you love? Does this pain get you down? Do you worry about your pain? Do you fear your pain or doing damage to yourself?
To understand the experience of a person’s pain-related distress, it was recommended that physiotherapists adopt a narrative style of assessment in which the lived experience and context of the person’s pain and movement-related fears are considered (Caneiro et al., Citation2022; Caneiro, Bunzli, and O’Sullivan, Citation2021; De Baets et al., Citation2023; O’Sullivan et al., Citation2018; O’Sullivan, Smith, Beales, and Straker, Citation2017). Similarly, Linton, Flink, and Vlaeyen (Citation2018) emphasized the importance of physiotherapists understanding the person’s broader context, as this might shed light on the mechanisms shared by co-occurring problems such as pain and generalized anxiety. Going further, Rabey and Moloney (Citation2022) recommended a thorough assessment of pain-related stressors, including concurrent generalized psychological distress, early-life stress and trauma including adverse childhood experiences and episodes of extreme stress.
The clinical interview allows in depth exploration regarding potential physical and psychological stressors, their relevance to the individual’s presentation, and any management of such stressors undertaken (eg, psychotherapy, sleep hygiene, alterations to training) (Rabey and Moloney, Citation2022).
In addition, several authors recommended guided behavioral assessments/experiments as part of a movement and activity-related fear assessment conducted by physiotherapists (Caneiro et al., Citation2022; De Baets et al., Citation2023; O’Sullivan et al., Citation2018).
Thorough behavioral assessment is imperative, even for patients who do not self-report high levels of fear of movement as it may highlight within-person discrepancies. An emotional response may only be triggered when one is confronted with the feared activity or when one believes the task needs to be performed (De Baets et al., Citation2023).
Van Wyngaarden, Noehren, and Archer (Citation2019) recommended an approach for physiotherapists which combined the brief depression screen, and the multidimensional screen and health related distress assessment approach. In this approach, during the first consultation with someone experiencing musculoskeletal pain, the PHQ-2 and OSPRO‐YF are administered, with the exception of people with low back pain. If the presentation involves low back pain, the PHQ-2 and SBST are administered, with the OSPRO‐YF administered at the second consultation to reduce client burden. If the PHQ-2 is positive, the PHQ‐9 is completed.
It is recommended that the PHQ‐2 be administered to all physical therapy patients upon initial intake. The PHQ‐9 only needs to be administered when a patient scores ≥ 3 on the PHQ‐2 (Van Wyngaarden, Noehren, and Archer, Citation2019).
If high scores are identified on specific subscales of the OSPRO‐YF, unidimensional tools which assess pain-related distress are used.
Management of psychological distress
The direct treatment of generalized psychological distress (e.g. depression, anxiety, and post-traumatic stress) and non-pain-related psychological distress (e.g. relationship issues and financial strain) was generally viewed in included articles as outside the scope of physiotherapy practice, for example:
Directly treating depression is not in the scope of practice for physiotherapists; however, a respectable knowledge of the condition contributes to the therapeutic plan of care within the interdisciplinary team (Varela and Melvin, Citation2023).
However, the management of health-related distress, particularly pain-related distress (e.g. pain-related fear and kinesiophobia) was generally described as within the scope of physiotherapy practice:
Managing the distress that is primarily related to a patient’s pain and physical incapacity has to be part of the physiotherapist’s responsibility to the patient. In contrast, it is not the physiotherapist’s obligation to directly manage distress that is primarily due to other factors (e.g. marriage breakdown and financial worries) (Watson, Citation1999).
The management of psychosocial factors, including health-related distress, as part of psychologically informed physiotherapy was the topic of most of the recently published literature included in this review. Psychologically informed physiotherapy has been described as follows:
[Psychologically informed physiotherapy] focuses on addressing psychological factors related with rehabilitative outcomes like pain and physical function, rather than on mental illness requiring specialist care (Main et al., Citation2023).
Several approaches for physiotherapists to managing psychological distress and health-related distress were described in the included articles, these being: 1) education and reassurance; 2) cognitive-behavioral approaches; 3) mindfulness; and 4) case-management including referral. In addition to these approaches, exercise, relaxation, sleep interventions, coping skills training, stress inoculation, problem solving, emotional ventilation, and resilience training were also briefly mentioned as interventions worthy of consideration by physiotherapists (Billek-Sawhney, Wagner, and Braun, Citation2014; Cancelliere and Mohammed, Citation2019; Daley et al., Citation2021; Donnelly, Brockwell, Rankin, and Moore, Citation2022; Faulkner and Snell, Citation2023; Harrison, Thorp, and Ritzline, Citation2014; Hodges, Citation2019; Rabey and Moloney, Citation2022), for example:
[In the management of] acute psychological distress … provide strategies to assist with the management of these emotional symptoms (ie, relaxation strategies such as diaphragmatic breathing) (Faulkner and Snell, Citation2023).
Education and reassurance
There was a general consensus across the included articles that physiotherapists should use education and reassurance to manage client psychological distress (Cancelliere and Mohammed, Citation2019; Chimenti, Frey-Law, and Sluka, Citation2018; Delitto et al., Citation2012; Faulkner and Snell, Citation2023; Main and Watson, Citation1999; Smith et al., Citation2020; Vieira, Brown, and Raue, Citation2014), for example:
In treating patients with heightened somatic awareness [e.g. concern or fear], it is important for manual therapists to offer repeated explanation and reassurance to the patients about the nature of their pain (Main and Watson, Citation1999).
The educational and reassurance-based approaches recommended for physiotherapists generally consisted of providing informative resources, de-threatening symptoms, normalizing emotional responses, establishing recovery expectations, and outlining management options. With regard to supporting people experiencing generalized psychological distress such as depression, Vieira, Brown, and Raue (Citation2014) recommended that physiotherapists provide appropriate education to older adults with depression or suspected depression in order to facilitate referral to a mental health professional:
It is critical to use appropriate patient educational materials about depression and the need for a referral for further evaluation (Vieira, Brown, and Raue, Citation2014).
In comparison to supporting someone with generalized psychological distress, the role of physiotherapists in supporting people experiencing health-related psychological distress was more involved. It was generally recommended that physiotherapists provide condition-specific education and reassurance regarding the client’s prognosis and normalize emotional responses to physical health issues (Cancelliere and Mohammed, Citation2019; Faulkner and Snell, Citation2023; Smith et al., Citation2020). For example, Smith et al. (Citation2020) recommended that physiotherapists provide education and reassurance to people with post–intensive care syndrome:
Unique learning needs among people with [post–intensive care syndrome] and their family members include … reassurance as they address the fears related with the episode of critical illness and the sequelae of problems; [and] confirmation about their recovery in response to interventions … (Smith et al., Citation2020).
While reassurance and education by physiotherapists was generally recommended, Main et al. (Citation2023) cautioned against providing overly optimistic reassurance and education, as it can create unrealistic client expectations that may lead to further distress (e.g. disappointment, anger, and frustration) which may impede recovery. However, some degree of optimism is needed as it appears to be associated with improved outcomes (Main et al., Citation2023). Consequently, Main et al. (Citation2023) and Main et al. (Citation2023) recommended physiotherapists offer education and reassurance that is guarded, yet cautiously optimistic, with a focus on intermediate client-centered goals as a path forward, rather than concentrating on the eventual outcome. Education and reassurance aimed at reducing health-related distress were not perceived as an isolated approach in physiotherapy care. Rather, education and reassurance were seen as fundamental components of management that complement or underpin other interventions aimed at reducing health-related distress. For example, Alappattu and Bishop (Citation2011) recommended that physiotherapists provide education regarding psychological factors such as pain-related fear and anxiety as part of the provision of cognitive coping strategies. Similarly, George and Zeppieri (Citation2009) described how education from physiotherapists can help decrease pain-related fear and support other interventions, such as graded exposure, which are also aimed at decreasing pain-related fear:
Patients receive education that decreases the fear and threat related with [low back pain]. Also, patients receive positive reinforcement for performing fearful activities and utilizing beneficial coping strategies. Therefore, it is impossible to separate the effects of the education and activity implementation components of the graded exposure treatment. In our opinion it is best to view graded exposure as a combined cognitive and behavioral treatment that encourages confrontation of fearful activities during rehabilitation of LBP (George and Zeppieri, Citation2009).
Cognitive-behavioral approaches
It was recommended in the included literature that cognitive-behavioral approaches aimed at reducing health-related fear, particularly pain-related fear and anxiety, be integrated into physiotherapy practice (Alappattu and Bishop, Citation2011; George and Zeppieri, Citation2009; Stearns et al., Citation2021; Varela and Melvin, Citation2023). Cognitive-behavioral approaches are characterized by an explicit focus on targeting maladaptive cognitions, emotions, and behaviors to improve clinical outcomes. Cognitive-behavioral approaches were generally described as a part of psychologically informed physiotherapy:
Cognitive-behavioral physical therapy is emerging in physical therapist practice and may be an effective intervention not only for psychological distress but for cognitive influences in older adults … Multiple interventions fall within the realm of cognitive-behavioral physical therapy, although a key component is that symptoms of a patient’s condition (e.g. pain) are a central tenet of treatment (Simon and Hicks, Citation2018).
The recommended cognitive-behavioral approaches for use by physiotherapists are aimed at addressing maladaptive thoughts and behaviors which perpetuate pain, pain-related disability, and pain-related distress:
Psychologically informed physical therapy [interventions may include] … behavioral therapies (to modify behaviors), cognitive behavioral therapies (to address cognitions about pain), or acceptance-based therapies that encourage return to function despite pain (Hodges, Citation2019).
The recommended cognitive-behavioral approaches incorporate a diverse range of interventions and techniques that may be used by physiotherapists, such as graded exposure, graded activity, and acceptance and commitment-based approaches.
Treatment considerations for those who screen positive in the fear avoidance domain include graded exposure and cognitive behavioral strategies (Stearns et al., Citation2021).
Varela and Melvin (Citation2023) suggested that physiotherapists consider functional behavioral interventions designed to facilitate problem solving skills, cognitive restructuring, and coping mechanisms reinforcing self-awareness, mastery and efficacy. The interdependent relationship between physical health issues such as pain and psychological distress means that while physiotherapists are not directly treating depression or other mental disorders (Varela and Melvin, Citation2023) these cognitive-behavioral interventions reduce health-related distress and allostatic load which are underlying transdiagnostic factors (Faulkner and Snell, Citation2023; Linton, Flink, and Vlaeyen, Citation2018; Rabey and Moloney, Citation2022).
Vandyken and Hilton (Citation2017) recommended physiotherapists consider implementing cognitive functional therapy, cognitive behavioral therapy, and graded exposure to address pain-related fear. Cognitive functional therapy draws on components of cognitive behavioral approaches such as cognitive restructuring and graded exposure in vivo to reduce pain and movement-related fear (O’Sullivan et al., Citation2018). Several authors of included articles described cognitive-behavioral approaches to the treatment by physiotherapists of pain-related fear, which have been informed by the Common-Sense model (Bunzli et al., Citation2017; Caneiro et al., Citation2022; Caneiro, Bunzli, and O’Sullivan, Citation2021). According to Bunzli et al. (Citation2017) a Common-Sense Model informed approach to treating pain-related fear involves motivational, reflective, and validating communication techniques. It also incorporates exposure control, which involves gradually exposing the person to the tasks they fear, as an approach to challenging unhelpful cognitions (Caneiro et al., Citation2022). This was further described as follows:
Identified processes should be targeted in treatment, ie, graduated exposure to address avoidance that is maintaining anxiety and low mood (Faulkner and Snell, Citation2023).
Behavioral exposure specifically targets pain-related fear and avoidance by gradually exposing the person to the tasks they fear or avoid while challenging unhelpful cognitions and disconfirming threat expectations (Caneiro et al., Citation2022).
However, as previously mentioned by Rabey and Moloney (Citation2022), while management of some psychological factors may be within the scope of the physiotherapy profession, a particular management approach may not be within the scope of an individual physiotherapist. In the context of cognitive-behavioral interventions, Alappattu and Bishop (Citation2011) recommended that physiotherapists consider using cognitive-behavioral interventions they are competent to use:
The presence of psychological variables may require cognitive behavioral interventions … Physical therapists trained in musculoskeletal dysfunction of the pelvic floor may include certain cognitive-behavioral interventions within their scope of practice (Alappattu and Bishop, Citation2011).
Mindfulness
Mindfulness was recommended by several authors as an approach to managing psychological distress that could be employed by physiotherapists (Billek-Sawhney, Wagner, and Braun, Citation2014; Donnelly, Brockwell, Rankin, and Moore, Citation2022; Simon and Hicks, Citation2018; Vandyken and Hilton, Citation2017). Rabey and Moloney (Citation2022) suggested that mindfulness was particularly useful as it influences a broad range of allostatic load biomarkers which underpin distress. Consistent with the broad effects of mindfulness, the approach was recommended for physiotherapists managing a variety of different forms of distress, including depression, anxiety, stress, pain catastrophizing, and pain-related fear (Simon and Hicks, Citation2018; Vandyken and Hilton, Citation2017; Varela and Melvin, Citation2023).
Researchers have also shown antidepressant benefits for individuals engaged in yoga and mindfulness practices (Billek-Sawhney, Wagner, and Braun, Citation2014).
While the management of depression and anxiety with mindfulness was mentioned, the form of psychological distress primarily discussed in this context was pain-related distress. Bunzli et al. (Citation2017) highlighted the potential benefits of mindfulness, stating that it can help regulate pain-related emotional responses. However, given the broad effects of mindfulness, Simon and Hicks (Citation2018) noted that the focus of mindfulness is largely global, rather than specific to pain:
However, mindfulness-based stress reduction is unique to cognitive-behavioral therapy in that the focus is more global (i.e. not specific to pain) (Simon and Hicks, Citation2018).
Several authors suggested that mindfulness can be incorporated with movement, such as Tai Chi and yoga, as part of “mindful movement” (Billek-Sawhney, Wagner, and Braun, Citation2014; Simon and Hicks, Citation2018; Vandyken and Hilton, Citation2017).
Case-management including referral
While the included literature suggested that physiotherapists have a role in the direct management of psychological distress, particularly health-related distress, there was a general consensus that a multidisciplinary approach to management of psychological distress was preferred when the distress is persistent, or preexisting (Alappattu and Bishop, Citation2011; Caneiro, Bunzli, and O’Sullivan, Citation2021; Daley et al., Citation2021; Faulkner and Snell, Citation2023; Linton and Shaw, Citation2011; Simonds, Abraham, and Spitznagle, Citation2022; Stearns et al., Citation2021; Sterling, Citation2009; Varela and Melvin, Citation2023; Vieira, Brown, and Raue, Citation2014; Watson, Citation1999):
Physiotherapists do not have the experience or training to manage [psychological distress] … not directly attributable to the pain condition … and need to refer on to specialist practitioners or develop a working relationship with mental health practitioners to facilitate joint management of these patients (Watson, Citation1999).
Physiotherapists must also collaborate and rely on specialists once a mental health concern is independently recognized (Varela and Melvin, Citation2023).
Consider referral/engagement in other services to address and manage preinjury mental health difficulties (Faulkner and Snell, Citation2023).
While persistent psychological distress, distress unrelated to the physical health issue, and preexisting psychological distress were suggested as indicators of a need for referral by physiotherapists, there was no consensus on the level of psychological distress necessitating referral. Delitto et al. (Citation2012) highlighted this issue in their low back pain clinical practice guideline for physiotherapists:
The authors of these clinical guidelines acknowledge that this is a general description for a rather important process. However, there are no absolute guidelines for the levels of psychological symptoms that indicate referral (Delitto et al., Citation2012).
Some authors of included articles provided recommendations for physiotherapists based on scores from psychological questionnaires, while others provided general guidance on the timing of referral. As health-related distress was considered a common and normal response to physical health conditions, Sterling and Kenardy (Citation2008) recommended referral to mental health care only if whiplash-related distress persisted beyond 3–4 weeks. Similarly, Daley et al. (Citation2021) recommended referral when the client’s complaint is not improving and there are psychological factors involved:
For patients with multiple psychosocial risk factors who are not progressing or participating in treatment, referral to a psychologist may be beneficial. Discussion with stakeholders regarding psychologist referral is encouraged (Daley et al., Citation2021).
Main and Watson (Citation1999) cautioned that the unnecessary referral of non-psychopathological distress could be harmful:
Patients presenting with painful conditions and related loss of function are very rarely psychiatrically ill, and inappropriate referral may simply magnify their distress (Main and Watson, Citation1999).
In determining the need for referral Wijma, van Wilgen CP, Meeus, and Nijs (Citation2016) recommended that physiotherapists consider their own skills alongside those of their clients by asking themselves: “is this patient in the right place here with me, or should he/she be treated in a multidisciplinary setting or referred to another provider?”
Referral options generally included the client’s primary medical practitioner and psychologist. However, other professionals such as social workers, counselors, and spiritual care practitioners were also mentioned. For example, Alappattu and Bishop (Citation2011) highlighted that pain-related distress among women with chronic pelvic pain can be associated with sexual dysfunction, and loss of partner intimacy. They proposed that a referral from the physiotherapist to a sex counselor or therapist should be considered for women who report sexual dysfunction or intimacy issues due to pelvic pain, indicating the necessity for an interdisciplinary approach to care:
The consequences of pain-related psychological variables in musculoskeletal pain include disuse and disability. In women with CPP, the sequelae likely include sexual dysfunction and loss of partner intimacy … [A] referral to a sex counselor or therapist is recommended [for these] women (Alappattu and Bishop, Citation2011).
Caneiro, Bunzli, and O’Sullivan (Citation2021) emphasized the need for a multidisciplinary approach involving physiotherapists should operate within a shared framework, providing consistent messages to the individual, and thereby reducing care fragmentation and client anxiety.
Clinicians should refer patients for co-care in the presence of comorbid mental (e.g. emotional distress, depression, eating disorders) and physical health conditions (e.g. type 2 diabetes, heart disease, morbid obesity). We contend that multi-disciplinary care including psychologist, pain physician, medical doctor and physiotherapist needs to be integrated, so the team shares a common framework and delivers consistent messages that prevents care fragmentation and patient distress (Caneiro, Bunzli, and O’Sullivan, Citation2021).
As part of this process, Vieira, Brown, and Raue (Citation2014) recommended that physiotherapists working with older adults approach the discussion of depression sensitively. Vieira, Brown, and Raue (Citation2014) made this recommendation as clients may have concerns related to the stigmatization of mental illness and barriers such as financial barriers to accessing mental health care:
Patients often need a great deal of encouragement and support to follow through with appointments for mental issues that they may not feel are essential … A good approach to increase the acceptability of further evaluation is to use the language of the patient (e.g. “feeling low or down” instead of “depressed”) and discuss mental health referral in the context of other medical conditions [such as] … poststroke depression.
Of the authors who discussed management of clients experiencing suicidal thoughts and behaviors (Harrison, Thorp, and Ritzline, Citation2014; Simonds, Abraham, and Spitznagle, Citation2022; Stearns et al., Citation2021; Varela and Melvin, Citation2023), the recommended approach was generally an immediate referral to emergency care or another appropriate mental health service. For example:
If a patient verbalizes suicidal ideation, then immediate referral to an appropriate health care practitioner is warranted (Harrison, Thorp, and Ritzline, Citation2014).
Delitto et al. (Citation2012) and Billek-Sawhney, Wagner, and Braun (Citation2014) recommended that physiotherapists refer any client with an intent and a plan for suicide for an immediate suicide risk assessment by mental health and medical professionals. Stearns et al. (Citation2021) recommended physiotherapists proactively establish a referral network, including crisis line services, to ensure they are well prepared to support a client experiencing suicidal thoughts.
Discussion
This systematic mapping review of recommended approaches for physiotherapists to the identification, assessment, and management of clients experiencing psychological distress mapped recommendations from 40 secondary or tertiary scholarly articles. Most of the included articles were published in the past decade and were written by physiotherapists and psychologists. The majority of included articles focused on the identification, assessment and management of health-related distress, with a particular emphasis on pain-related distress. There was attention given to depression screening and referral, while other forms of psychological distress, such as generalized anxiety and post-traumatic stress disorder, were not discussed as frequently. Three recommended approaches to detecting and assessing psychological distress were identified: 1) brief depression screen; 2) integrated suicide/non-suicidal self-harm and depression screen; and 3) multidimensional screen and health-related distress assessment approach. As for the management of psychological distress, the main recommended approaches identified were: 1) education and reassurance; 2) cognitive-behavioral; 3) mindfulness; and 4) case management (including referral).
Given physiotherapists across all clinical areas of practice encounter clients experiencing psychological distress (Lucas and Parker, Citation2022; McGrath, Verdon, Parnell, and Pope, Citation2023) the identification, assessment and management of psychological distress should be of clinical and research interest to all physiotherapy subdisciplines. According to the IOPTMH, mental health physiotherapists possess the “knowledge, skills and attitudes to assess [but not diagnose], support, treat and refer people with mental illnesses” (Probst et al., Citation2019, Citation2020). Although the subdiscipline of mental health physiotherapy is well positioned to provide leadership in this area, the subdiscipline is relatively new and small in comparison to other established physiotherapy research and practice areas such as musculoskeletal and pain physiotherapy (Heywood et al., Citation2022). The holistic approach commonly advocated by musculoskeletal and pain physiotherapy researchers incorporates mental health, although there tends to be a stronger emphasis on cognitive and behavioral factors, and when emotional factors are considered it is typically limited to pain-related distress (Daluiso-King and Hebron, Citation2020; Dillon et al., Citation2023). Consequently, the articles included in this systematic mapping review largely pertained to the assessment and management of pain-related distress and were typically authored by researchers with expertise in musculoskeletal pain assessment and management. Since the turn of the millennium, there has been considerable development in psychological screening, risk identification, pain-related distress assessment, and pain-related distress management relevant to musculoskeletal and pain physiotherapy settings (Alvarez et al., Citation2022; Lentz et al., Citation2016; Main et al., Citation2023; Stearns et al., Citation2021; Stewart, Kempenaar, and Lauchlan, Citation2011). There has also been considerable interest in the intersection of depression and chronic pain in the field of physiotherapy (Carballo-Costa, Quintela-Del-Río, Vivas-Costa, and Costas, Citation2023). These developments are evident in this review. In contrast, the few articles identified which provide recommendations for the identification, assessment, and management of generalized psychological distress, non-health-related distress, and psychopathology may be explained by the relative lack of development in mental health physiotherapy and psychologically informed physiotherapy in other research subdisciplines, such as neurological physiotherapy (Lucas and Parker, Citation2022).
The three recommended approaches to detecting and assessing psychological distress identified in this review suggest that screening for all forms of psychological distress is within the scope of physiotherapy practice. However, when all articles were considered together, only the assessment of health-related distress, particularly pain-related distress, was perceived to fall within the scope of the profession, with the formal assessment of non-health-related distress and psychopathology positioned outside of scope. This interpretation is consistent with the ‘Flags’ framework developed by the Decade of the Flags Working Group (Nicholas, Linton, Watson, and Main, Citation2011). According to the Decade of the Flags Working Group, ‘orange flags’ are psychiatric symptoms that meet criteria for psychopathology that requires referral to a specialist mental health professional for assessment and management. In comparison, ‘yellow flags’ are normal but unhelpful psychological reactions, such as distress not meeting criteria for diagnosis of a mental disorder that may be addressed by suitably trained health professionals such as physiotherapists (Nicholas, Linton, Watson, and Main, Citation2011). However, given that many physiotherapists report a lack of confidence in assessing psychological factors, such as pain-related distress (Henning and Smith, Citation2022; Synnott et al., Citation2015) and that few have received training in psychological assessment (Driver, Lovell, and Oprescu, Citation2021; Simpson et al., Citation2021) currently the assessment of pain-related distress is best described as an advanced area of physiotherapy practice that is beyond the individual scope of most physiotherapists.
The four primary management approaches for psychological distress identified in this review: 1) education and reassurance; 2) cognitive-behavioral approaches; 3) mindfulness; and 4) case management including referral span the continuum of traditional (standard) physiotherapy practice and merge into that of psychologically informed physiotherapy. Although physiotherapists’ provision of education and case management is likely to be improved with training (Edgar and Connaughton, Citation2021; Synnott et al., Citation2016) the activities are considered to be within the remit of all physiotherapists by the Physiotherapy Board of Australia, Physiotherapy Board of New Zealand (Citation2015). In contrast, management approaches such as cognitive-behavioral and mindfulness-based approaches are likely to require additional training beyond that provided in qualifying physiotherapy programs (Alvarez et al., Citation2022; Coronado et al., Citation2020; Tatta, Citation2022). The finding of the review that the direct treatment of psychopathology is generally viewed as beyond the scope of physiotherapy is incongruent with the position of the IOPTMH. According to the IOPTMH, interventions such as exercise, and cognitive and behavioral physiotherapy approaches, intended to directly reduce psychological symptoms, fall within the scope of specialist mental health physiotherapists working within a multidisciplinary team (Probst et al., Citation2020). Working within a multidisciplinary team allows physiotherapists to collaborate with other mental health professionals to ensure that their approach is safe and high-quality (Probst et al., Citation2020). In addition, the use of cognitive-behavioral approaches and mindfulness-based interventions in the management of pain-related distress lie within the scope of specialist pain physiotherapists (Alvarez et al., Citation2022; Coronado et al., Citation2020; Keefe, Main, and George, Citation2018; Tatta, Willgens, and Palombaro, Citation2022). Safe and effective delivery of cognitive-behavioral approaches and mindfulness-based interventions by physiotherapists requires training, which may include competency assessment, supervision and feedback (Alexanders and Douglas, Citation2016; Driver, Lovell, and Oprescu, Citation2021; Linton and Shaw, Citation2011; Simpson et al., Citation2021). Several studies of physiotherapist-delivered psychological interventions included supervision by psychologists as part of training (Alvarez et al., Citation2022). However, due to the emerging and evolving nature of this aspect of physiotherapy practice, there is no widely accepted standard for training, assessment and supervision (Coronado et al., Citation2020). Therefore, it is suggested that the management of pain-related distress is within the profession’s scope, but it is beyond the individual scope of many physiotherapists. This interpretation is consistent with the Low Back Pain Clinical Care Standard’s Quick Guide for Physiotherapists (Maher and O’Sullivan, Citation2023) which recommends nonspecialist physiotherapists refer to specialist physiotherapists where clients are experiencing high levels of pain-related fear and distress, and to psychologists where clients are exhibiting high levels of anxiety, distress, depression, social stress, and unresolved trauma.
While not every included study explicitly referred to the revised flags framework (Nicholas, Linton, Watson, and Main, Citation2011) recommended approaches reviewed generally assumed that psychological distress can be divided into: yellow (i.e. subclinical and health-related distress); orange (i.e. symptoms of psychopathology); and red flags (i.e. severe depression and/or suicidality). However, differentiating normal distress from symptoms of psychopathology, as well as pain-related distress from depression, anxiety, and post-traumatic stress, is both conceptually and clinically challenging (Kirsh, Citation2010; Rusu, Santos, and Pincus, Citation2016; Stein and Nesse, Citation2015; Young, Lareau, and Pierre, Citation2014). Although a full discussion of the psychiatric nosology is beyond the scope of this review, there is strong evidence that psychological distress and psychopathological depression and anxiety lie on a continuum, with the boundaries between normal and abnormal being an artificial dichotomization (Ruscio, Citation2019). Furthermore, there is some debate regarding whether pain-related distress and depression/anxiety in the context of chronic pain are distinct constructs or just strongly related ones (Beesdo et al., Citation2009; Rusu, Santos, and Pincus, Citation2016). Consequently, it might be more appropriate to conceptualize yellow flags, orange flags, and red flags on a continuum.
Similar criticisms have been made by Stewart, Kempenaar, and Lauchlan (Citation2011) who argued that the flags framework misses the complexity of the psychological and social world of the individual. Main and George (Citation2011) acknowledged the importance of this criticism of the flags framework, but questioned whether such debate would advance clinical practice in the “real” world. Although screening tools and awareness of common forms can assist with identification of psychopathology, Kirsh (Citation2010) posited that they are not necessarily sufficient in differentiating normal distress from psychopathology among people experiencing persistent pain. To understand a person’s experience of distress requires an understanding of their context and the meaning of their distress (Johnstone and Dallos, Citation2014). However, most physiotherapists are not currently trained to obtain this. Physiotherapists, particularly physiotherapists assessing and managing pain-related distress, may benefit from mental health training to assist them to discern whether the psychological distress is generalized or specific to pain. This training is particularly important for physiotherapists, such as those working in rural areas, who may not be able to engage in timely co-care with mental health professionals due to significant workforce shortages (Cleary, Thomas, and Boyle, Citation2020). There are also concerns that universal depression and anxiety screening in primary care settings may lead to overdiagnosis and overtreatment (Thombs et al., Citation2023). Thombs et al. (Citation2023) suggested that a more effective approach might be to provide people experiencing mental health concerns with timely access to caring health professionals with time to talk through their concerns, understand them as a person, and work with them to identify the best way forward. Mental health training may help physiotherapists discern when screening is warranted in their specific context. Beyond that, mental health training would equip them to support people experiencing psychological distress, making it possible to connect them with mental health services in a manner that is considerate, compassionate, and understanding.
Limitations
The reviewers’ clinical and research background may have influenced the articles included in the review. The two reviewers RLM and SS who screened, assessed, and extracted the papers practice clinically in the area of pain. Therefore, papers discussing the identification, assessment, and management of pain-related distress may have been more easily identifiable to the reviewers. Furthermore, although the approach to searching the literature was systematic, the heterogeneity of the article topics and article types may mean some eligible articles may not have been included. Additionally, while full-text review involved a double review approach, a single screen approach to screening the titles and abstracts of records was adopted due to the large number of records returned from the database search. Consequently, the risk of eligible articles being incorrectly excluded during title and abstract screening higher is than with a double screening approach (Waffenschmidt et al., Citation2019). Another limitation of this review was that it was not designed to evaluate the evidence which formed the basis of the identified recommended approaches. Therefore, physiotherapists should exercise caution when using the results of this review to inform their practice if they have not evaluated the individual included articles and the original research on which they are based. However, physiotherapists may find this review helpful as a directory of literature that describes approaches recommended for physiotherapy practice.
Recommendations for physiotherapy research
More research is needed to further inform the scope and role of physiotherapists in psychological assessment, including providing further clarity around the roles of physiotherapists in general, pain physiotherapists, mental health physiotherapists, and physiotherapists from other specialized areas in psychological assessment. Furthermore, given physiotherapists work in a range of clinical settings and with varying levels of isolation, ranging from sole primary contact physiotherapists working in remote areas to physiotherapists working in multidisciplinary teams alongside psychologists, further research is needed to understand the training required for physiotherapists in this area of practice to facilitate optimal client care. Future research should include evaluation of the evidence behind each of the approaches identified in the review, including investigations of client experiences of physiotherapist-initiated psychological assessment.
Conclusion
This systematic mapping review mapped approaches recommended for physiotherapists to identify, assess, and manage clients experiencing psychological distress and published in the scholarly literature. Current recommendations largely emphasize the role of physiotherapists in assessing and managing health-related distress, particularly pain-related distress. In regard to depression and suicide, physiotherapists were advised to screen for this using questionnaires such as the PHQ-9 and refer onwards to a mental health professional for further assessment. Management of psychological distress was largely focused on reducing health-related distress, with case management including co-care and referral recommended for generalized and non-health-related psychological distress. Given the inseparability of physical and mental health and the high frequency of encounters with psychological distress in physiotherapy practice, physiotherapists may benefit from specific mental health training to assist them to understand the nature of the distress being experienced by their clients and to enable effective person-centered care.
Supplemental Material
Download Zip (45.9 KB)Acknowledgments
The research team acknowledge Dr. Jasmine B. MacDonald’s contribution to developing the protocol of this review. RLM would also like to acknowledge the support provided by the Australian Government Department of Health’s Rural Health Multidisciplinary Training Program.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/09593985.2023.2284823.
Additional information
Funding
References
- Alappattu MJ, Bishop MD 2011 Psychological factors in chronic pelvic pain in women: Relevance and application of the fear-avoidance model of pain. Physical Therapy 91: 1542–1550. 10.2522/ptj.20100368
- Alexanders J, Douglas C 2016 The role of psychological skills within physiotherapy: A narrative review of the profession and training. Physical Therapy Reviews 21: 222–227. 10.1080/10833196.2016.1274352
- Almond A, Zou Y, Forbes R 2021 Navigating diagnostic uncertainty in musculoskeletal practice: The perspectives and experiences of new graduate physiotherapists. Musculoskeletal Science and Practice 52: 102354. 10.1016/j.msksp.2021.102354
- Alvarez E, Garvin A, Germaine N, Guidoni L, Schnurr M 2022 Use of mental health interventions by physiotherapists to treat individuals with chronic conditions: A systematic scoping review. Physiotherapy Canada 74: 35–43. 10.3138/ptc-2020-0066
- American Physical Therapy Association 2023 APTA practice advisory: Screening patients for anxiety. https://www.apta.org/patient-care/interventions/patient-screenings/practice-advisory-screening-for-anxiety.
- American Psychological Association, American Psychological Association Practice Organization Work Group 2014 Distinguishing between screening and assessment for mental and behavioral health problems. https://www.apaservices.org/practice/reimbursement/billing/assessment-screening.
- Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P 2015 Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. International Journal of Evidence-Based Healthcare 13: 132–140. 10.1097/XEB.0000000000000055
- Beck AT, Guth D, Steer RA, Ball R 1997 Beck depression Inventory for primary care (BDI-PC). APA PsycTests. 10.1037/t07153-000
- Beck AT, Steer RA, Brown G 1996 Beck depression Inventory-II (BDI-II). APA PsycTests. 10.1037/t00742-000
- Beck AT, Ward CH, Mendelson M, Mock J, Erbauch J 1961 Beck depression Inventory (BDI). APA PsycTests. 10.1037/t00742-000
- Beekman E, Verhagen A 2018 Clinimetrics: Hospital anxiety and depression scale. Journal of Physiotherapy 64: 198. 10.1016/j.jphys.2018.04.003
- Beesdo K, Hoyer J, Jacobi F, Low NC, Höfler M, Wittchen HU 2009 Association between generalized anxiety levels and pain in a community sample: Evidence for diagnostic specificity. Journal of Anxiety Disorders 23: 684–693. 10.1016/j.janxdis.2009.02.007
- Billek-Sawhney B, Wagner A, Braun J 2014 Depression: Implications for the acute care therapist. Journal of Acute Care Physical Therapy 5: 77–88. 10.1097/01.JAT.0000453142.16547.86
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL 2015 The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress 28: 489–498. 10.1002/jts.22059
- Bunzli S, Smith A, Schütze R, Lin I, O’Sullivan P 2017 Making sense of low back pain and pain-related fear. Journal of Orthopaedic and Sports Physical Therapy 47: 628–636. 10.2519/jospt.2017.7434
- Butera KA, George SZ, Lentz TA 2020 Psychometric evaluation of the optimal screening for prediction of referral and outcome yellow flag (OSPRO-YF) tool: Factor structure, reliability, and validity. The Journal of Pain 21: 557–569. 10.1016/j.jpain.2019.09.003
- Cancelliere C, Mohammed RJ 2019 Brain drain: Psychosocial factors influence recovery following mild traumatic brain injury - 3 recommendations for clinicians assessing psychosocial factors. Journal of Orthopaedic and Sports Physical Therapy 49: 842–844. 10.2519/jospt.2019.8849
- Caneiro JP, Bunzli S, O’Sullivan P 2021 Beliefs about the body and pain: The critical role in musculoskeletal pain management. Brazilian Journal of Physical Therapy 25: 17–29. 10.1016/j.bjpt.2020.06.003
- Caneiro JP, Smith A, Bunzli S, Linton S, Moseley GL, O’Sullivan P, O’Sullivan P 2022 From fear to safety: A roadmap to recovery from musculoskeletal pain. Physical Therapy 102: zab271. 10.1093/ptj/pzab271
- Cano A, Goubert L 2017 What’s in a name? The case of emotional disclosure of pain-related distress. The Journal of Pain 18: 881–888. 10.1016/j.jpain.2017.01.008
- Carballo-Costa L, Quintela-Del-Río A, Vivas-Costa J, Costas R 2023 Mapping the field of physical therapy and identification of the leading active producers. A bibliometric analysis of the period 2000- 2018. Physiotherapy Theory and Practice 39: 2407–2419. 10.1080/09593985.2022.2073927
- Chimenti RL, Frey-Law LA, Sluka KA 2018 A mechanism-based approach to physical therapist management of pain. Physical Therapy 98: 302–314. 10.1093/ptj/pzy030
- Cleary A, Thomas N, Boyle F 2020 National mental health workforce strategy. https://www.health.gov.au/sites/default/files/documents/2021/08/national-mental-health-workforce-strategy-a-literature-review_0.docx
- Connaughton J 2018 Working in general practice treating people with comorbid mental health problems. In: Probst M Skjaerven L (Eds) Physiotherapy in mental health and psychiatry: A scientific and clinical based approach, pp. 200–205. Edinburgh, United Kingdom: Elsevier.
- Coons MJ, Hadjistavropoulos HD, Asmundson GJ 2004 Factor structure and psychometric properties of the pain anxiety symptoms Scale-20 in a community physiotherapy clinic sample. European Journal of Pain 8: 511–516. 10.1016/j.ejpain.2003.11.018
- Coronado RA, Brintz CE, McKernan LC, Master H, Motzny N, Silva FM, Goyal PM, Wegener ST, Archer KR 2020 Psychologically informed physical therapy for musculoskeletal pain: Current approaches, implications, and future directions from recent randomized trials. Pain Reports 5: e847. 10.1097/PR9.0000000000000847
- Crombez G, De Paepe AL, Veirman E, Eccleston C, Verleysen G, Van Ryckeghem DML 2020 Let’s talk about pain catastrophizing measures: An item content analysis. PeerJ 8: e8643. 10.7717/peerj.8643
- Cupler ZA, Alrwaily M, Polakowski E, Mathers KS, Schneider MJ 2020 Taping for conditions of the musculoskeletal system: An evidence map review. Chiropractic and Manual Therapies 28: 52. 10.1186/s12998-020-00337-2
- Daley D, Payne LP, Galper J, Cheung A, Deal L, Despres M, Garcia JD, Kistner F, Mackenzie N, Perry T et al. 2021 Clinical guidance to optimize work participation after injury or illness: The role of physical therapists. Journal of Orthopaedic and Sports Physical Therapy 51: CPG1–CPG102. 10.2519/jospt.2021.0303
- Daluiso-King G, Hebron C 2020 Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiotherapy Theory and Practice 38: 373–389. 10.1080/09593985.2020.1765440
- De Baets L, Meulders A, Van Damme S, Caneiro JP, Matheve T 2023 Understanding discrepancies in a person’s fear of movement and avoidance behavior: A guide for musculoskeletal rehabilitation clinicians who support people with chronic musculoskeletal pain. Journal of Orthopaedic and Sports Physical Therapy 53: 307–316. 10.2519/jospt.2023.11420
- Delitto A, George SZ, Dillen LV, Whitman JM, Sowa G, Shekelle P, Denninger TR, Godges JJ 2012 Low back pain: Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. Journal of Orthopaedic and Sports Physical Therapy 42: A1–A57. 10.2519/jospt.2012.42.4.A1
- DePrince AP, Chu AT, Pineda AS 2011 Links between specific posttrauma appraisals and three forms of trauma-related distress. Psychological Trauma: Theory, Research, Practice, & Policy 3: 430–441. 10.1037/a0021576
- Dillon M, Olson R, Mescouto K, Costa N, Setchell J 2023 How physiotherapists attend to the human aspects of care when working with people with low back pain: A thematic analysis. Health Sociology Review 32: 277–293. 10.1080/14461242.2022.2161927
- Djulbegovic B, Hozo I, Greenland S 2011 Uncertainty in clinical medicine. In: Gifford F (Ed) Philosophy of medicine, pp. 299–356. Amsterdam, the Netherlands: North-Holland.
- Donnelly GM, Brockwell E, Rankin A, Moore IS 2022 Beyond the musculoskeletal system: Considering whole-systems readiness for running postpartum. Journal of Women’s Health Physical Therapy 46: 48–56. 10.1097/JWH.0000000000000218
- Drapeau A, Marchand A, Beaulieu-Prévost D 2012 Epidemiology of psychological distress. In: L’Abate L (Ed) Mental illnesses: Understanding, prediction and control, pp. 105–134. London, United Kingdom: IntechOpen.
- Driver C, Kean B, Oprescu F, Lovell GP 2017 Knowledge, behaviors, attitudes and beliefs of physiotherapists towards the use of psychological interventions in physiotherapy practice: A systematic review. Disability and Rehabilitation 39: 2237–2249. 10.1080/09638288.2016.1223176
- Driver C, Lovell GP, Oprescu F 2021 Psychosocial strategies for physiotherapy: A qualitative examination of physiotherapists’ reported training preferences. Nursing and Health Sciences 23: 136–147. 10.1111/nhs.12771
- Dunn KM, Campbell P, Lewis M, Hill JC, van der Windt DA, Afolabi E, Protheroe J, Wathall S, Jowett S, Oppong R, et al. 2021 Refinement and validation of a tool for stratifying patients with musculoskeletal pain. European Journal of Pain 25: 2081–2093. 10.1002/ejp.1821
- Edgar S, Connaughton J 2021 Using mental health first aid training to improve the mental health literacy of physiotherapy students. Physiotherapy Canada 73: 188–193. 10.3138/ptc-2019-0036
- Edgerton K, Hall J, Bland MK, Marshall B, Hulla R, Gatchel RJ 2019 A physical therapist’s role in pain management: A biopsychosocial perspective. Journal of Applied Biobehavioral Research 24: e12170. 10.1111/jabr.12170
- Faulkner JW, Snell DL 2023 A framework for understanding the contribution of psychosocial factors in biopsychosocial explanatory models of persistent postconcussion symptoms. Physical Therapy 103: zac156. 10.1093/ptj/pzac156
- Franzen MD 2003 Psychological assessment in medical settings. In: Cohen L, McChargue D Collins F (Eds) The health psychology handbook: Practical issues for the behavioral medicine specialist, pp. 17–27. Thousand Oaks, United States: SAGE Publications.
- George SZ, Valencia C, Zeppieri G, Robinson ME 2009 Development of a self-report measure of fearful activities for patients with low back pain: The fear of daily activities questionnaire. Physical Therapy 89: 969–979. 10.2522/ptj.20090032
- George SZ, Zeppieri G 2009 Physical therapy utilization of graded exposure for patients with low back pain. Journal of Orthopaedic and Sports Physical Therapy 39: 496–505. 10.2519/jospt.2009.2983
- Gioia GA, Collins M, Isquith PK 2008 Improving identification and diagnosis of mild traumatic brain injury with evidence: Psychometric support for the acute concussion evaluation. Journal of Head Trauma Rehabilitation 23: 230–242. 10.1097/01.HTR.0000327255.38881.ca
- Grant MJ, Booth A 2009 A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information and Libraries Journal 26: 91–108. 10.1111/j.1471-1842.2009.00848.x
- Haddaway NR, Page MJ, Pritchard CC, McGuinness LA 2022 Prisma2020: An R package and shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and open synthesis. Campbell Systematic Reviews 18: e1230. 10.1002/cl2.1230
- Haggman S, Maher C, Refshauge K 2004 Screening for symptoms of depression by physical therapists managing low back pain. Physical Therapy 84: 1157–1166. 10.1093/ptj/84.12.1157
- Hansen LS, Præstegaard J, Lehn-Christiansen S 2021 Patient-centeredness in physiotherapy - a literature mapping review. Physiotherapy Theory and Practice 38: 1843–1856. 10.1080/09593985.2021.1923095
- Harland N, Lavallee D 2003 Biopsychosocial management of chronic low back pain patients with psychological assessment and management tools: Overview. Physiotherapy 89: 305–312. 10.1016/S0031-9406(05)60043-0
- Harrison AL, Thorp JN, Ritzline PD 2014 A proposed diagnostic classification of patients with temporomandibular disorders: Implications for physical therapists. Journal of Orthopaedic and Sports Physical Therapy 44: 182–197. 10.2519/jospt.2014.4847
- Henning M, Smith M 2022 The ability of physiotherapists to identify psychosocial factors in patients with musculoskeletal pain: A scoping review. Musculoskeletal Care 21: 502–515. 10.1002/msc.1725
- Heywood SE, Connaughton J, Kinsella R, Black S, Bicchi N, Setchell J 2022 Physical Therapy and mental health: A scoping review. Physical Therapy 102: zac102. 10.1093/ptj/pzac102
- Hill S 2010 The illness perceptions questionnaire-revised (IPQ-R). Journal of Physiotherapy 56: 280. 10.1016/S1836-9553(10)70062-X
- Hodges PW 2019 Hybrid approach to treatment tailoring for low back pain: A proposed model of care. Journal of Orthopaedic and Sports Physical Therapy 49: 453–463. 10.2519/jospt.2019.8774
- Horowitz MJ, Wilner N, Alvarez W 1979 Impact of Event Scale (IES). APA PsycTests. 10.1037/t00303-000
- Howlett B, Rogo E 2021 What evidence-based practice is and why it matters. In: Howlett B, Shelton T Rogo E (Eds) Evidence based practice for health professionals, pp. 1–24. Burlington, United States: Jones and Bartlett Learning.
- Hunter EE, Murphy M 2011 Zung self-rating depression scale. In: Kreutzer J, DeLuca J Caplan B (Eds) Encyclopedia of clinical neuropsychology, pp. 2746–2747. New York, United States: Springer.
- Iles R, Sheehan L, Munk K, Gosling C 2020 Development and pilot assessment of the pace tool: Helping case managers identify and respond to risk factors in workers’ compensation case management. Journal of Occupational Rehabilitation 30: 167–182. 10.1007/s10926-019-09858-x
- Jamison JR 2006 Differential diagnosis for primary care, a handbook for health care practitioners. Philadelphia: Elsevier (Churchill Livingstone)
- Johnstone L, Dallos R 2014 Introduction to formulation. In: Johnstone L Dallos R (Eds) Formulation in psychology and psychotherapy: Making sense of people’s problems (2nd), pp. 1–17. United Kingdom: East SussexRoutledge.
- Julian LJ 2011 Measures of anxiety: State-Trait anxiety Inventory (STAI), Beck anxiety Inventory (BAI), and Hospital anxiety and depression Scale-anxiety (HADS-A). Arthritis Care and Research 63: S467–S472. 10.1002/acr.20561
- Keefe FJ, Main CJ, George SZ 2018 Advancing psychologically informed practice for patients with persistent musculoskeletal pain: Promise, pitfalls, and solutions. Physical Therapy 98: 398–407. 10.1093/ptj/pzy024
- Kirsh KL 2010 Differentiating and managing common psychiatric comorbidities seen in chronic pain patients. Journal of Pain and Palliative Care Pharmacotherapy 24: 39–47. 10.3109/15360280903583123
- Kroenke K, Spitzer RL, Williams JB 1999 Patient Health Questionnaire-9 (PHQ-9). APA PsycTests. 10.1037/t06165-000
- Kroenke K, Spitzer RL, Williams JB 2003 The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care 41: 1284–1292. 10.1097/01.MLR.0000093487.78664.3C
- Kroenke K, Wu J, Yu Z, Bair MJ, Kean J, Stump T, Monahan PO 2016 Patient health Questionnaire anxiety and depression Scale (PHQ-ADS). APA PsycTests. 10.1037/t55980-000
- Laporte G, Aita M 2021 Psychological distress as a unique concept: A response to Molgora et al. (2020). Journal of Affective Disorders 278: 13–14. 10.1016/j.jad.2020.09.050
- Lennon O, Ryan C, Helm M, Moore K, Sheridan A, Probst M, Cunningham C 2020 Psychological distress among patients attending physiotherapy: A survey-based investigation of Irish physiotherapists’ current practice and opinions. Physiotherapy Canada 72: 239–248. 10.3138/ptc-2019-0010
- Lentz TA, Beneciuk JM, Bialosky JE, Zeppieri G, Dai Y, Wu SS, George SZ, George SZ 2016 Development of a yellow flag assessment tool for orthopaedic physical therapists: Results from the optimal screening for prediction of referral and outcome (OSPRO) cohort. Journal of Orthopaedic and Sports Physical Therapy 46: 327–343. 10.2519/jospt.2016.6487
- Linton SJ, Boersma K 2003 Early identification of patients at risk of developing a persistent back problem: The predictive validity of the örebro musculoskeletal pain questionnaire. The Clinical Journal of Pain 19: 80–86. 10.1097/00002508-200303000-00002
- Linton SJ, Flink IK, Vlaeyen JW 2018 Understanding the etiology of chronic pain from a psychological perspective. Physical Therapy 98: 315–324. 10.1093/ptj/pzy027
- Linton SJ, Nicholas M, MacDonald S 2011 Development of a short form of the Örebro musculoskeletal pain screening questionnaire. Spine 36: 1891–1895. 10.1097/BRS.0b013e3181f8f775
- Linton SJ, Shaw WS 2011 Impact of psychological factors in the experience of pain. Physical Therapy 91: 700–711. 10.2522/ptj.20100330
- Lo C, Hales S, Zimmermann C, Gagliese L, Rydall A, Rodin G 2011 Measuring death-related anxiety in advanced cancer: Preliminary psychometrics of the death and dying distress scale. Journal of Pediatric Hematology/Oncology 33: S140–S145. 10.1097/MPH.0b013e318230e1fd
- Lord S 2018 Perceptions of Physiotherapists Regarding Their Role in the Management of Patients with Mental Health Disorders. Doctoral Dissertation, University of the Witwatersrand.
- Lucas L, Parker J 2022 Physiotherapists perceived role in managing anxiety in patients with relapsing-remitting multiple sclerosis: A mixed-methods study. Archives of Physiotherapy 12: 2. 10.1186/s40945-021-00124-z
- Maher C, O’Sullivan P 2023 Low back pain standard an opportunity for physios. In Motion May: 33-39. https://australian.physio/inmotion/low-back-pain-standard-opportunity-physios.
- Main CJ, Ballengee LA, George SZ, Beneciuk JM, Greco CM, Simon CB 2023 Psychologically informed practice (PIP): The importance of communication in clinical implementation. Physical Therapy 103: zad047. 10.1093/ptj/pzad047
- Main CJ, George SZ 2011 Psychologically informed practice for management of low back pain: Future directions in practice and research. Physical Therapy 91: 820–824. 10.2522/ptj.20110060
- Main CJ, Simon CB, Beneciuk JM, Greco CM, George SZ, Ballengee LA 2023 The psychologically informed practice (PIP) consultation roadmap: A clinical implementation strategy. Physical Therapy Physical Therapy 103: zad048. 10.1093/ptj/pzad048
- Main CJ, Watson PJ 1999 Psychological aspects of pain. Manual Therapy 4: 203–215. 10.1054/math.1999.0208
- Main CJ, Wood PL, Hollis S, Spanswick CC, Waddell G 1992 The distress and risk assessment method: A simple patient classification to identify distress and evaluate the risk of poor outcome. Spine 17: 42–52. 10.1097/00007632-199201000-00007
- McGrath RL, Parnell T, Verdon S, Pope R 2022 “People suffer and we see this”: A qualitative study of the forms of patient psychological distress encountered by physiotherapists. Physiotherapy Theory and Practice Online ahead of print. 10.1080/09593985.2022.2141085
- McGrath RL, Pope R, Parnell T, Verdon S 2022 Assessing and managing physiotherapy clients experiencing psychological distress: A scoping review protocol. Open Science Framework 10.17605/OSF.IO/MJB6N
- McGrath RL, Verdon S, Parnell T, Pope R 2023 Australian physiotherapists’ perceived frequency of contact with clients experiencing distress: A cross-sectional survey. Physiotherapy Theory and Practice 1–18 Online ahead of print. 10.1080/09593985.2023.2204962
- McNeil DW, Rainwater AJ 1998 Development of the fear of pain questionnaire-III. Journal of Behavioral Medicine 21: 389–410. 10.1023/A:1018782831217
- Mirowsky J, Ross CE 2003 Social causes of psychological distress. 2nd New York, United States: Transaction Publishers.
- Mitchell T, Beales D, Slater H, O'Sullivan PB 2018 Musculoskeletal clinical translation framework: From knowing to doing. Perth: Curtin University.
- Morgan DL, Nica A 2020 Iterative thematic inquiry: A new method for analyzing qualitative data. International Journal of Qualitative Methods 19: 1–11. 10.1177/1609406920955118
- Motlagh H 2010 Impact of event scale-revised. Journal of Physiotherapy 56: 203. 10.1016/S1836-9553(10)70029-1
- Ng TS 2012 Brief illness perception questionnaire (brief IPQ). Journal of Physiotherapy 58: 202. 10.1016/S1836-9553(12)70116-9
- Nicholas MK, Linton SJ, Watson PJ, Main CJ 2011 The “Decade of the flags” working group 2011 early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain: A reappraisal. Physical Therapy 91: 737–753 10.2522/ptj.20100224
- Nijs J, Wijma AJ, Leysen L, Pas R, Willaert W, Hoelen W, Ickmans K, van Wilgen CP 2019 Explaining pain following cancer: A practical guide for clinicians. Brazilian Journal of Physical Therapy 23: 367–377. 10.1016/j.bjpt.2018.12.003
- O’Sullivan PB, Caneiro JP, O’Keeffe M, Smith A, Dankaerts W, Fersum K, O’Sullivan K 2018 Cognitive functional therapy: An integrated behavioral approach for the targeted management of disabling low back pain. Physical Therapy 98: 408–423. 10.1093/ptj/pzy022
- O’Sullivan PB, Smith A, Beales D, Straker L 2017 Understanding adolescent low back pain from a multidimensional perspective: Implications for management. Journal of Orthopaedic and Sports Physical Therapy 47: 741–751. 10.2519/jospt.2017.7376
- Paolo FP, Joaquim R 2018 Ten simple rules for conducting umbrella reviews. Evidence-Based Mental Health 21: 95–100. 10.1136/ebmental-2018-300014
- Parkitny L, McAuley J 2010 The depression anxiety stress scale (DASS). Journal of Physiotherapy 56: 204. 10.1016/S1836-9553(10)70030-8
- Payton AR 2009 Mental health, mental illness, and psychological distress: Same continuum or distinct phenomena? Journal of Health and Social Behavior 50: 2 213–227. 10.1177/002214650905000207
- Peters MD, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H 2020 Scoping reviews (2020 version). In: Aromataris E Munn Z (Eds) JBI manual for evidence synthesis, Adelaide, Australia: Joanna Briggs Institute.
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA 2014 A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Research Synthesis Methods 5: 371–385. 10.1002/jrsm.1123
- Phillips MR 2009 Is distress a symptom of mental disorders, a marker of impairment, both or neither? World Psychiatry 8: 91–92.
- Physiotherapy Board of Australia, Physiotherapy Board of New Zealand 2015. Physiotherapy practice thresholds in Australia and Aotearoa New Zealand. https://physiocouncil.com.au/wp-content/uploads/2017/10/Physiotherapy-Board-Physiotherapy-practice-thresholds-in-Australia-and-Aotearoa-New-Zealand.pdf.
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D 2011 Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): Depression, anxiety, and anger. Assessment 18: 263–283. 10.1177/1073191111411667
- Probst M, Brunner E, Connaughton J, Sallinen M, Skjaerven L 2020 Educational standards: Describing Minimal Requirements of mental health Courses in physiotherapy education. https://www.ioptmh.org/_files/ugd/9f5f61_0c2220d67fbc47ecb3ed41567d262b03.pdf.
- Probst M, Skjaerven L, Connaughton J, Brunner E, Sallinen M, Slootweg L, Van Damme T, Stubbs B, Vancampfort D, Staub C, et al. 2019. Policy statement: The role of Physical therapists within mental health and psychiatry. https://www.ioptmh.org/_files/ugd/9f5f61_43fe2b1bad6a42939129e588e7aa30e1.pdf.
- Rabey M, Moloney N 2022 “I don’t know why I’ve got this pain!” Allostasis as a possible explanatory model. Physical Therapy 102: zac017. 10.1093/ptj/pzac017
- Radloff LS 1977 Center for Epidemiological studies depression Scale. APA PsycTests. 10.1037/t02942-000
- Raphael B 1975 Crisis and the physiotherapist. Australian Journal of Physiotherapy 21: 51–56. 10.1016/S0004-9514(14)61207-1
- Rebbeck T 2017 The role of exercise and patient education in the noninvasive management of whiplash. Journal of Orthopaedic and Sports Physical Therapy 47: 481–491. 10.2519/jospt.2017.7138
- Ribeiro C, Tsang L, Lin B, Kemp-Smith K, Phillips J, Furness J 2022 Physiotherapists’ perceptions of their role in treating and managing people with depression and anxiety disorders: A systematic review. Online ahead of print. 10.1080/09593985.2022.2122915
- Ridner SH 2004 Psychological distress: Concept analysis. Journal of Advanced Nursing 45: 536–545. 10.1046/j.1365-2648.2003.02938.x
- Ruscio AM 2019 Normal versus pathological mood: Implications for diagnosis. Annual Review of Clinical Psychology 15: 179–205. 10.1146/annurev-clinpsy-050718-095644
- Rusu AC, Santos R, Pincus T 2016 Pain-related distress and clinical depression in chronic pain: A comparison between two measures. Scandinavian Journal of Pain 12: 62–67. 10.1016/j.sjpain.2016.04.001
- Schultz IZ, Crook J, Berkowitz J, Milner R, Meloche GR 2005 Predicting return to work after low back injury using the psychosocial risk for occupational disability instrument: A validation study. Journal of Occupational Rehabilitation 15: 365–376. 10.1007/s10926-005-5943-9
- Scurlock-Evans L, Upton P, Upton D 2014 Evidence-based practice in physiotherapy: A systematic review of barriers, enablers and interventions. Physiotherapy 100: 208–219. 10.1016/j.physio.2014.03.001
- Seng EK, Klepper JE 2017 Cogniphobia Scale for headache disorders (CS-HD). APA PsycTests. 10.1037/t64748-000
- Sharkey CM, Bakula DM, Baraldi AN, Perez MN, Suorsa KI, Chaney JM, Mullins LL 2018 Grit, illness-related distress, and psychosocial outcomes in college students with a chronic medical condition: A path analysis. Journal of Pediatric Psychology 43: 552–560. 10.1093/jpepsy/jsx145
- Shaw WS, Pransky G, Patterson W, Winters T 2005 Early disability risk factors for low back pain assessed at outpatient occupational health clinics. Spine 30: 572–580. 10.1097/01.brs.0000154628.37515.ef
- Shrestha SD, Pradhan R, Tran TD, Gualano RC, Fisher JR 2016 Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting Perinatal Common Mental Disorders (PCMDS) among women in low-and lower-middle-income countries: A systematic review. BMC Pregnancy and Childbirth 16: 72. 10.1186/s12884-016-0859-2
- Simonds AH, Abraham K, Spitznagle T 2022 Clinical practice guidelines for pelvic girdle pain in the postpartum population. Journal of Women’s and Pelvic Health Physical Therapy 46: E1–E38. 10.1097/JWH.0000000000000236
- Simon CB, Hicks GE 2018 Paradigm shift in geriatric low back pain management: Integrating influences, experiences, and consequences. Physical Therapy 98: 434–446. 10.1093/ptj/pzy028
- Simpson P, Holopainen R, Schütze R, O’Sullivan P, Smith A, Linton SJ, Nicholas M, Kent P 2021 Training of physical therapists to deliver individualized biopsychosocial interventions to treat musculoskeletal pain conditions: A scoping review. Physical Therapy 101: zab188. 10.1093/ptj/pzab188
- Singla M, Jones M, Edwards I, Kumar S 2015 Physiotherapists’ assessment of patients’ psychosocial status: Are we standing on thin ice? A qualitative descriptive study. Manual Therapy 20: 328–334. 10.1016/j.math.2014.10.004
- Smith JM, Lee AC, Zeleznik H, Coffey Scott JP, Fatima A, Needham DM, Ohtake PJ 2020 Home and community-based physical therapist management of adults with post–intensive care syndrome. Physical Therapy 100: 1062–1073. 10.1093/ptj/pzaa059
- Snell DL, Siegert RJ, Debert C, Cairncross M, Silverberg ND 2020 Fear avoidance behavior after traumatic brain injury Questionnaire (FAB-TBI). APA PsycTests. 10.1037/t82263-000
- Spearing R, Bailey J 2012 Depression and chronic physical illness: Its prevalence and diagnosis, and implications for therapeutic practice. International Journal of Therapy and Rehabilitation 19: 394–403. 10.12968/ijtr.2012.19.7.394
- Spitzer RL, Kroenke K, Williams JBW, Löwe B 2006 A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine 166: 1092–1097. 10.1001/archinte.166.10.1092
- Stearns ZR, Carvalho ML, Beneciuk JM, Lentz TA, Lentz TA 2021 Screening for yellow flags in orthopaedic physical therapy: A clinical framework. Journal of Orthopaedic and Sports Physical Therapy 51: 459–469. 10.2519/jospt.2021.10570
- Stein DJ, Nesse RM 2015 Normal and abnormal anxiety in the age of DSM-5 and ICD-11. Emotion Review 7: 223–229. 10.1177/1754073915575407
- Sterling M 2009 Physical and psychological aspects of whiplash: Important considerations for primary care assessment, part 2 - case studies. Manual Therapy 14: e8–e12. 10.1016/j.math.2008.03.004
- Sterling M 2011 General health Questionnaire-28 (GHQ-28). Journal of Physiotherapy 57: 259. 10.1016/S1836-9553(11)70060-1
- Sterling M 2014 Physiotherapy management of whiplash-associated disorders (WAD). Journal of Physiotherapy 60: 5–12. 10.1016/j.jphys.2013.12.004
- Sterling M, Kenardy J 2008 Physical and psychological aspects of whiplash: Important considerations for primary care assessment. Manual Therapy 13: 93–102. 10.1016/j.math.2007.11.003
- Stewart J, Kempenaar L, Lauchlan D 2011 Rethinking yellow flags. Manual Therapy 16: 196–198. 10.1016/j.math.2010.11.005
- Sullivan MJ, Adams H, Horan S, Maher D, Boland D, Gross R 2008 The role of perceived injustice in the experience of chronic pain and disability: Scale development and validation. Journal of Occupational Rehabilitation 18: 249–261. 10.1007/s10926-008-9140-5
- Sullivan MJ, Bishop SR, Pivik J 1995 Pain catastrophizing Scale (PCS). APA PsycTests. 10.1037/t01304-000
- Synnott A, O’Keeffe M, Bunzli S, Dankaerts W, O’Sullivan P, O’Sullivan K 2015 Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: A systematic review. Journal of Physiotherapy 61: 68–76. 10.1016/j.jphys.2015.02.016
- Synnott A, O’Keeffe M, Bunzli S, Dankaerts W, O’Sullivan P, Robinson K, O’Sullivan K 2016 Physiotherapists report improved understanding of and attitude toward the cognitive, psychological and social dimensions of chronic low back pain after cognitive functional therapy training: A qualitative study. Journal of Physiotherapy 62: 215–221. 10.1016/j.jphys.2016.08.002
- Tatta J 2022 Introducing a physical therapist-led acceptance and commitment therapy training for pain: A clinical perspective. Internet Journal of Allied Health Sciences & Practice 20: 16. 10.46743/1540-580X/2022.2061
- Tatta J, Willgens AM, Palombaro KM 2022 Mindfulness and acceptance–based interventions in physical therapist practice: The time is now. Physical Therapy 102: zab293. 10.1093/ptj/pzab293
- Thomas F, Hansford L, Ford J, Wyatt K, McCabe R, Byng R 2018 Moral narratives and mental health: Rethinking understandings of distress and healthcare support in contexts of austerity and welfare reform. Palgrave Communications 4: 39. 10.1057/s41599-018-0091-y
- Thombs BD, Markham S, Rice DB, Ziegelstein RC, Ziegelstein RC 2023 Screening for depression and anxiety in general practice. BMJ 382: 1615. 10.1136/bmj.p1615
- Timmermans S, Angell A 2001 Evidence-based medicine, clinical uncertainty, and learning to doctor. Journal of Health and Social Behavior 42: 342–359. 10.2307/3090183
- Traeger A, McAuley JH 2013 STarT back screening tool. Journal of Physiotherapy 59: 131. 10.1016/S1836-9553(13)70170-X
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L et al. 2018 Prisma extension for scoping reviews (PRISMA-SCR): Checklist and explanation. Annals of Internal Medicine 169: 467–473. 10.7326/M18-0850
- Turner P 2001 Evidence-based practice and physiotherapy in the 1990s. Physiotherapy Theory and Practice 17: 107–121. 10.1080/095939801750334185
- VandenBos GR 2015 APA dictionary of Psychology. 2nd p. 70. Washington DC, United States: American Psychological Association.
- van Dijk H, Köke AJ, Elbers S, Mollema J, Smeets R, Wittink H 2023 Physiotherapists using the biopsychosocial model for chronic pain: Barriers and facilitators - a scoping review. International Journal of Environmental Research and Public Health 20: 1634. 10.3390/ijerph20021634
- Vandyken C, Hilton S 2017 Physical therapy in the treatment of central pain mechanisms for female sexual pain. Sexual Medicine Reviews 5: 20–30. 10.1016/j.sxmr.2016.06.004
- Van Wyngaarden JJ, Noehren B, Archer KR 2019 Assessing psychosocial profile in the physical therapy setting. Journal of Applied Biobehavioral Research 24: e12165. 10.1111/jabr.12165
- Varela AJ, Melvin A 2023 The theatre of depression: A role for physical therapy. Physiotherapy Theory and Practice 39: 1325–1341. 10.1080/09593985.2022.2041136
- Vieira ER, Brown E, Raue P 2014 Depression in older adults: Screening and referral. Journal of Geriatric Physical Therapy 37: 24–30. 10.1519/JPT.0b013e31828df26f
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ 1993 Fear-avoidance beliefs Questionnaire (FABQ). APA PsycTests. 10.1037/t11850-000
- Waffenschmidt S, Knelangen M, Sieben W, Bühn S, Pieper D 2019 Single screening versus conventional double screening for study selection in systematic reviews: A methodological systematic review. BMC Medical Research Methodology 19: 132. 10.1186/s12874-019-0782-0
- Ware JE 2000 SF-36 health survey update. Spine 25: 3130–3139. 10.1097/00007632-200012150-00008
- Ware JE, Snow KK, Kosinski M, Gandek B 1993 SF-36 health survey: Manual and interpretation guide. Boston, United States: The Health Institute, New England Medical Center Hospitals. https://search.worldcat.org/title/sf-36-health-survey-manual-and-interpretation-guide/oclc/28895942
- Watson PJ 1999 Psychosocial assessment: The emergence of a new fashion, or a new tool in physiotherapy for musculoskeletal pain? Physiotherapy 85: 530–535. 10.1016/S0031-9406(05)61246-1
- Watson PJ, Kendall N 2000 The assessment of psychosocial yellow flags in physiotherapy practice. In: Gifford L (Ed) Topical issues in pain 2. Biopsychosocial assessment. Relationships and pain, pp. 85–110. Falmouth, United Kingdom: CNS Press.
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, Marx BP 2017 Clinician-administered PTSD Scale for DSM-5. pp. CAPS–5. APA PsycTests. 10.1037/t71324-000
- Weermeijer JD, Meulders A, Meulders, A 2018 Clinimetrics: Tampa scale for kinesiophobia. Journal of Physiotherapy 64: 126. 10.1016/j.jphys.2018.01.001
- Wicksell RK, Renöfält J, Olsson GL, Bond FW, Melin L 2008 Psychological Inflexibility in pain Scale (PIPS). APA PsycTests. 10.1037/t23288-000
- Wideman TH, Sullivan MJL 2012 Development of a cumulative psychosocial factor index for problematic recovery following work-related musculoskeletal injuries. Physical Therapy 92: 58–68. 10.2522/ptj.20110071
- Wijma AJ, van Wilgen CP, Meeus M, Nijs J 2016 Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiotherapy Theory and Practice 32: 368–384. 10.1080/09593985.2016.1194651
- Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, Lynch AD, Snyder-Mackler L, McDonough CM 2019 Patellofemoral pain: Clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American Physical Therapy Association. Journal of Orthopaedic and Sports Physical Therapy 49: CPG1–CPG95. 10.2519/jospt.2019.0302
- Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J 1999 Clinical guidelines: Potential benefits, limitations, and harms of clinical guidelines. BMJ 318: 527–530. 10.1136/bmj.318.7182.527
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer O 1983 Geriatric depression Scale (GDS). APA PsycTests. 10.1037/t00930-000
- Young G, Lareau C, Pierre B 2014 One quintillion ways to have PTSD comorbidity: Recommendations for the disordered DSM-5. Psychological Injury and Law 7: 61–74. 10.1007/s12207-014-9186-y