ABSTRACT
Individuals with intellectual disabilities often fail to learn complex tasks. Modified Goal Management Training (mGMT) or Errorless Learning combined with assistive technology (App + EL) can help. The goal is to demonstrate the effectiveness of mGMT and/or App + EL in learning complex tasks. We employed a randomized controlled crossover design. One group started with mGMT (N = 16), and the other with App + EL (N = 15). We compared their performance with that of a passive control group (N = 15). The training consisted of six sessions of 30 minutes each. Success was analyzed using the Goal Attainment Scale (GAS). Three different tasks were assessed before and after each intervention period: “Practiced”, “Non-Practiced”, or “Previously Practiced”. Generalization was evaluated through neuropsychological tests. Results indicated that both interventions significantly improved “Practiced” tasks compared with “Non-Practiced” tasks and the control group. Crossing the intervention did not interfere with the stable performance on the “Previously Practiced” task. However, starting with mGMT reduced, but did not eliminate, the efficacy of App + EL after crossing, but this pattern was not observed for the reverse sequence. Only the Tower of London task documented improvements related to interventions. In conclusion, the mGMT and App + EL were effective in learning complex tasks and retaining performance after learning a second task.
Trial registration: German Clinical Trials Register identifier: DRKS00021674.
Introduction
Individuals with intellectual disabilities often encounter challenges when performing multistep actions and may experience significant limitations in their ability to perform daily tasks. These difficulties can be attributed, at least in part, to deficits in executive functions (EF), which play a pivotal role in the planning, organization, and execution of complex actions. EF refers to the cognitive abilities essential for controlling and regulating behaviour. They facilitate the flexible coordination of these processes and are involved in goal development, goal achievement, adaptation to unexpected events, navigation of novel situations, and planning across multiple steps (García-Pintor et al., Citation2023; Müller, Citation2013; Reischies, Citation2007).
Impairments in EF can arise from a variety of brain conditions and can result in difficulties such as goal neglect or losing track of the intended objective. Notably, individuals with Down syndrome (DS; Rowe et al., Citation2006), Prader-Willi syndrome (Jauregi et al., Citation2007), Fragile X syndrome (Huddleston et al., Citation2014), Turner syndrome (Hong et al., Citation2009; Lasker et al., Citation2007), Williams syndrome (Howlin & Udwin, Citation2006; Mervis & John, Citation2010; Rhodes et al., Citation2011), and autism spectrum disorders (Panerai et al., Citation2014) have been found to have lower EF test scores than their neurotypical peers. Given the essential role of the skills encompassed within the EF construct in various aspects of daily life management, it becomes evident that impairments in this domain can lead to reduced independence, a heightened need for supervision, and a diminished quality of life (Domire & Wolfe, Citation2014; Hendricks, Citation2010).
To date, various interventions have been developed to address EF impairment, and Goal Management Training (GMT) is one method that is frequently studied (Levine et al., Citation2000; Levine et al., Citation2011). GMT is a standardized metacognitive therapy that aims to enhance awareness and cognitive control in individuals with EF deficits, enabling them to perform essential daily life skills. Levine et al. (Citation2000) divided GMT into five stages, each addressing an integral part of effective goal management. By following these stages (stop-state-split-learn-check), participants were trained to interrupt their ongoing behaviour and consider task demands. They were then guided to define the main goal, break down complex goals into subgoals, establish goal hierarchies, learn the subgoals through encoding and retention, and monitor their performance to ensure that their actions lead to the desired goal. If discrepancies persisted after the final stage, participants were required to repeat all five stages starting from the beginning. Multiple studies have demonstrated the effectiveness of GMT in individuals with brain injuries (Stamenova & Levine, Citation2019). Post-training evaluations have shown improvements in self-report questionnaires, standardized cognitive executive function tests (Krasny-Pacini et al., Citation2014; Levine et al., Citation2011; Miotto et al., Citation2009; Müller et al., Citation2019a), and real-life domains, such as financial management (Grant et al., Citation2012) or meal preparation (Levine et al., Citation2000). However, despite its significant potential applicability to individuals with intellectual disabilities (Emerson et al., Citation2004), GMT has not yet been implemented and evaluated in this specific population. This may be partially attributed to the unproofed assumption that GMT, in its initial application, is cognitively demanding for individuals with intellectual disabilities.
Another pivotal approach that supports the execution of daily tasks is the use of assistive technology (AT). AT encompasses various items and devices designed to enhance, maintain, and improve functional capabilities. Reminders and prompt system-based AT can assist individuals with EF impairments in correctly executing sequential actions. The RehaGoal App, which provides step-by-step guidance through complex tasks (Müller et al., Citation2019b), is one example of such an assistive technology. This app has already been successfully employed in single case studies involving meal preparation tasks for individuals with intellectual disabilities and autism (Aust & Müller, Citation2022; Ertas et al., Citation2021). Inspired by the GMT approach (Levine et al., Citation2011), the RehaGoal App allows users to break down complex main goals into manageable sub-goals or steps, enabling them to practice these steps using predefined workflows (Gabel et al., Citation2020). It incorporates micro-prompting elements and reminder components, enabling therapists to integrate the task steps into those workflows, allowing patients to perform their tasks individually and in a goal-oriented manner, taking small steps as necessary, ultimately achieving greater independence in daily life. It offers an intuitive menu navigation system, an in-app workflow authoring system, image-based display options, and adjustable font size (Müller et al., Citation2019b). Each task can consist of a textual description accompanied by an image, and the task history feature enabled users to track their progress. The therapist interface was specifically designed to facilitate creating individual workflows with ease by utilizing a range of predefined function blocks that can be interconnected.
The RehaGoal App's structure allows the integration of task execution with Errorless Learning (EL) and the Method of Vanishing Cues (MVC). EL is an implicit learning process that focuses on eliminating errors. Within this framework, task sub-steps can be practiced one at a time with appropriate demonstrations and gradual fading of cues and prompts upon successful completion (Clare & Jones, Citation2008; Maxwell et al., Citation2001; Sohlberg et al., Citation2005). EL can be implemented using different chaining techniques, such as “forward chaining” (FC) and “backward chaining” (BC). FC entails a step-by-step approach to process consecutive sub-steps, whereas BC begins by practicing the final sub-step initially, and subsequently extending the process by incorporating the penultimate step upon successful independent completion. The MVC describes the progressive removal of cues and prompts during the learning process to minimize the occurrence of errors. Initially, task performance was supported with the highest level of assistance, with the aid gradually reducing until the user could execute the task independently. BC has been effective in teaching children with autism how to tie shoelaces (Rayner, Citation2011; Richard & Noell, Citation2019) and write their names (Moore et al., Citation2013). Moreover, it has been successful in instructing adults with autism and intellectual disabilities on how to access specific websites (Jerome et al., Citation2007). Combining BC and MVC has been shown to be particularly effective (Hunkin & Parkin, Citation1995).
To the best of our knowledge, no randomized controlled trials have compared the GMT and EL combined with AT as approaches for increasing performance in complex tasks and reducing EF impairment in individuals with intellectual disabilities. This study investigated whether using the RehaGoal App with EL (BC and MVC), a modified version of Goal Management Training (mGMT), or a combination of both enhanced task performance in adults with intellectual disabilities compared with a passive control group. Additionally, we evaluated the stability of retention performance, transfer effects on self-selected tasks, potential sequence effects, and neuropsychological test data.
Methods
Participants
The study sample consisted of individuals with intellectual disabilities undergoing occupational rehabilitation and/or employed in sheltered workshops operated by Mehrwerk gGmbH Braunschweig and DRK-inkluzivo gGmbH Wolfenbüttel from 1 March 2020 to 20 December 2021. Data collection was temporarily suspended due to the COVID-19 lockdown from March 23rd to the end of June 2020.
Participants were required to meet the following inclusion criteria:
Having diminished level of intelligence (IQ score below 69), assessed using the Culture Fair Intelligence Test (CFT 20-R). This instrument was selected because of its language-free nature, norms specifically applicable to the target population, and economic feasibility.
Identification by caregivers as individuals facing challenges in action planning. Caregivers were provided with a comprehensive list of symptoms associated with EF impairment and their manifestations in everyday life. Confirmation of at least three of these symptoms was used to indicate EF impairment.
Under the age of 45 (to exclude participants with dementia).
Sufficient receptive language abilities per evaluation and caregiver report to enable appropriate responses to simple instructions.
The exclusion criteria consisted of the following:
A history of diagnosed neurodegenerative disorders.
A history of diagnosed severe neuropsychiatric disorders in accordance with the ICD-10 guidelines.
Physical disabilities affecting hand and/or arm movements, hindering practical task performance.
We assumed an effect size of one SD for our intervention, resulting in a sample size of 16 patients per group (Kutschmann et al., Citation2006). Anticipating a similar number of dropouts, we initially included 62 participants. Sixteen patients dropped out of the study, resulting in 16 participants in the intervention group, 15 in the other intervention group, and 15 in the control group (). presents the demographic characteristics, IQ scores, and disease profiles of the three groups. No significant differences were identified between the participants in the three groups for any of these variables.
Figure 1. Flow chart of the recruitment and randomization procedure.
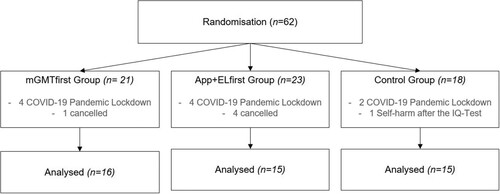
Table 1. Demographic and clinical characteristics of participants.
Study design
All participants and their caregivers were provided with an information sheet and consent form written in simple language. Informed consent was obtained from all the participants and their legal representatives. The study was approved by the Ethics Committee of the Medical Board and Ostfalia University of Applied Science and prospectively registered in the DRKS-German Clinical Trials Register (DRKS00021674) prior to data acquisition.
This study utilized a double-blind, randomized, controlled crossover design incorporating two intervention groups and a passive control group (). After the recruitment phase, a clinical psychologist who was uninvolved with recruitment and unaware of the participants’ backgrounds randomly allocated each participant to one of three study groups (mGMTfirst, App + ELfirst, or control). Randomization was performed using Microsoft Excel's Random Number Generator. Group assignment was performed without information about the participants’ diagnostic results based on the randomization sequence to ensure blind randomization.
Procedure
In Phase I, the mGMTfirst group received the mGMT intervention, while the App + ELfirst group utilized the RehaGoal App with EL to learn the correct execution of their self-selected task. Following a one-week break, in Phase II, each group received the respective, previously unapplied intervention to practice the second task that had not yet been addressed (). Both study phases consisted of six sessions, each lasting 30 minutes, with the specific content outlined in . Neuropsychological tests were administered only at the beginning and end of the study (T1 and T3, respectively).
Figure 2. Study design.
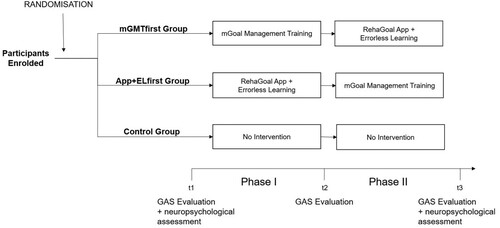
Figure 3. GAS measurements at T1, T2, and T3 for the mGMTfirst Group.
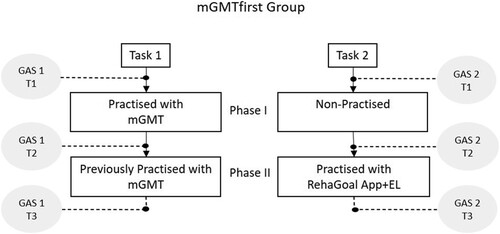
Figure 4. GAS measurements at T1, T2, and T3 for the App+ELfirst Group.
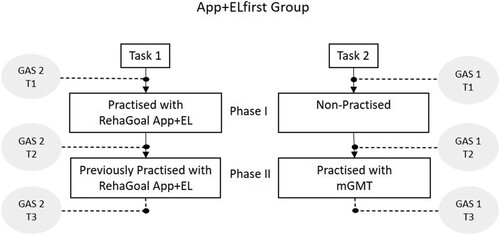
Table 2. Procedures for both intervention sessions.
The mGMTfirst intervention, which had previously demonstrated successful outcomes in a pilot study involving individuals with intellectual disabilities (Ertas et al., Citation2019), focused on training participants to periodically interrupt ongoing behaviours, bring their overarching task goal to mind, segment it into subtasks, and monitor their performance to optimize organization and goal attainment for their self-selected tasks. A therapist offered systematic guidance and instructed the participants to adhere to the provided instructions throughout the six sessions. In selecting which modules or content to modify and use for the GMT intervention, we were guided by the participants’ performance and language proficiency. We also needed to keep the intervention duration short to fit within the time constraints of the clinicians. A team of three psychologist made the decisions regarding content inclusion. Although homework is an essential part of the original GMT intervention, we chose to omit it due to the variable levels of homework support among participants. The unpredictability and potential inequity in access to support resources could compromise the consistency and fairness of the study results. Furthermore, homework completion could present additional challenges in terms of motivation and self-regulation, as participants might find it difficult to sustain their motivation and independently manage their learning activities.
During the RehaGoal App with EL intervention, the participants collaboratively established a workflow for their respective tasks with the therapist. The task steps were displayed on a smartphone, and the therapist assisted participants in learning these steps using the EL approach, focusing on preventing errors during task execution. Error reduction was achieved through (1) target sequencing, (2) prompting participants to perform the task as illustrated in the app, (3) immediate error correction, and (4) progressive removal of cues (according to the MVC) only after participants successfully performed the subtask in several attempts. Initially, participants were shown the final step of the task sequence. Once proficiency in that step was achieved, participants progressed to learning the preceding step in combination with the final step, continuing this incremental process throughout the remaining four therapy sessions. The participants had access to visual aids, instructions in a text box below the visual aids, and text-to-speech features for guidance.
The control group did not receive any treatment.
Assessment
Primary outcome measure
The participants were asked to identify two challenging tasks frequently leading to errors and interruptions during their working hours. In cases where participants encountered difficulty identifying appropriate tasks within their typical work routines, suitable tasks such as composing letters were identified through collaborative efforts between the study team and job supervisors.
Performance on the selected tasks was assessed using the Goal Attainment Scale (GAS), the primary outcome measure. Using the GAS, five outcome levels were specified individually for each goal, ranging from +2 to −2, reflecting outcomes that are “much better than expected” (+2), “better than expected” (+1), “expected” (0), “less than expected” (−1), and “much less than expected” (−2; Kiresuk & Sherman, Citation1968).
Evaluations of task performance were conducted by therapists blinded to the intervention conditions at the baseline assessment (T1), after Phase I (T2), and after Phase II (T3; and ). Three task states were distinguished for the evaluation: “Practiced” (the task is carried out with the support of either mGMT or the RehaGoal App with EL), “Non-Practiced” (performing the task without any intervention support) and “Previously Practiced” (the task has already been performed with one of the interventions in Phase I and were performed in Phase II without that specific intervention).
Secondary outcome measures
The secondary outcome measurements, including neuropsychological tests () that assessed the participants’ EF were administered at the beginning and end of the study to identify any generalization of the training to cognitive functions.
Table 3. Secondary outcome measures.
Statistical analysis
A mixed ANOVA with two within-subject factors and one between-subject factor was conducted. The two within-subject factors were Time (T1, T2, T3) and Task (Task 1, Task 2), while the between-subject factor was Group (mGMTfirst, App + ELfirst, control). Regression analysis was utilized to examine whether age, disease or IQ at T1 or T2 significantly predicted improvements in GAS scores for the “Practiced” task. Secondary outcome measures were determined using an analysis of variance (ANOVA) with repeated measures, treating Time (T1 vs. T3) as the within-subjects variable and Group (mGMTfirst, App + ELfirst, control) as the between-subjects variable.
Statistical significance was set at p < .05. All statistical analyses were performed using IBM SPSS software (Version 18).
Results
Effect of the intervention
The mixed ANOVA revealed several significant main effects and interaction effects. There was a significant main effect for Time (F(2.42) = 60.782; p < 0.001; η² = 743) and for Group (F(2.43) = 7.343; p < 0.002; η² = .255). However, the main effect for tasks was not significant. A significant three-way interaction effect was found among Time, Task, and Group (F(4.86) = 8.612; p < 0.001; η² = .286). Additionally, significant two-way interaction effects were identified between Time and Group (F(4.86) = 9.654; p < 0.001; η² = .310), Task and Group (F(2.43) = 6.305; p < 0.004; η² = .227), and Time and Task (F (2.42) = 5.646; p < 0.007; η² = .212).
Post hoc analysis
The statistical results for pairwise between-group comparisons are detailed in . The Bonferroni-adjusted post-hoc tests at T1 showed no significant differences between the two intervention groups and the control group in either task. However, at T2, both intervention groups exhibited an intervention-specific significant improvement compared to the control group in the “Practiced” task. The intervention effect was not transferred to the “Non-Practiced” task. At T3, both intervention groups significantly improved their GAS scores for the new task compared with the control group. Moreover, their performance on the “Previously Practiced” task was better than that of the control group. Performance on the “Previously Practiced” task and the intervention involving the second task did not differ significantly between the two intervention groups, indicating the retention of task performance even after learning the second task.
Table 4. Pairwise comparison of performance in GAS.
A second ANOVA for repeated measurement with the within-subject factor Phase (Phase1, Phase 2) and between-subject factor was Group (mGMTfirst, App + ELfirst) was performed to analyse the sequence effect. For Phase 1, the difference in the “Practiced” task between T1 and T2 was used, and for Phase 2, the difference between T2 and T3 was used. The ANOVA revealed a significant main effect for Phase (F(1. 29) = 4.276, p = 0.048, η² = .129). Although there was no significant main effect for Group, an interaction effect between Time and Group was significant (F(1.29) = 9.002, p = 0.019, η² = .174). While no significant differences were detected between groups during Phase 1, a significant difference emerged in Phase 2 (F(1, 29) = 5.418, p = 0.027, η² = 0.157).
The mean GAS scores for each group at the three assessment points (T1, T2, and T3) are presented in . Regarding the mGMT intervention, performance at T2 improved in the mGMTfirst Group (M = 1.44, SD = 0.89) and at T3 in the App + ELfirst Group (M = 0.40, SD = 0.80). Conversely, for the RehaGoal App with EL intervention, performance at T2 improved in the App + ELfirst Group (M = 1.40, SD = 1.21) but a smaller increase at T3 in the mGMTfirst Group (M = 0.40, SD = 1.35). These findings suggest that the mGMT intervention exhibited equivalent effectiveness in both phases, while the efficacy of the RehaGoal App with EL intervention was diminished when applied subsequently in Phase 2 (, italics scores).
Table 5. Mean GAS scores for each group at three measurement Ttme points (T1, T2, T3).
The GAS score at T3 for the “Previously Practiced” task reflected the performance retention and showed no statistically significant performance drop after introducing the second intervention.
Further specific GAS results
Regression analysis revealed that etiology, age, and IQ were not significant predictors of GAS improvement.
Comparison of neuropsychological variables between the groups
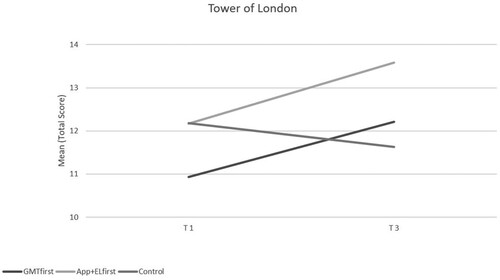
From the neuropsychological test data, a significant interaction was observed only for the ToL test. A repeated-measures ANOVA revealed a main effect of Time (F(1, 34) = 5.72, p = . 022, η² = .144), no main effect for Group, and a significant Time x Group interaction, (F(1, 34) = 5.72, p = . 022, η² = .144). Both intervention groups demonstrated improvements compared to the control group (). Despite the different baseline scores at T1, both intervention groups exhibited similar patterns of improvement; however, this intergroup effect was not statistically significant.
Figure 5. Comparison of Tower of London mean scores at T1 and T3 for the three groups.
The mean neuropsychological test scores, which were not significantly different before and after the intervention, are presented in .
Table 6. Mean neuropsychological test scores for the three groups.
Discussion
The present study aimed to examine the effectiveness of two interventions, the mGMT and the RehaGoal App with EL, in improving the performance of complex tasks among individuals with intellectual disabilities compared to a control group. Both interventions elicited significant improvements in goal attainment for “Practiced” tasks (at T2) compared to “Non-Practiced” tasks and the control group task. These findings suggest that individuals with intellectual disabilities can learn to execute complex tasks through repetitive practice within a two-week timeframe and is in line with previous case studies (Levine et al., Citation2000; Moore et al., Citation2013; Rayner, Citation2011; Richard & Noell, Citation2019; Smith et al., Citation2015).
The intervention effects on the “Practiced” tasks remained stable from T2 to T3. Delayed retention performance stability has been investigated in several previous studies. Notably, a case study conducted by Jerome et al. (Citation2007) demonstrated that adults with intellectual disabilities could learn computer-based leisure skills through EL with BC, which were also retrievable after some time. Another case study by Richard and Noell (Citation2019) revealed that most pediatric participants with autism could fully learn shoe-tying skills, which were learned through the utilization of Video Prompting and BC. The acquired skills were retained after a one-week interval. Regarding the utilization of GMT, the study by Grant et al. (Citation2012) showed that participants with traumatic brain injury could maintain or even surpass the acquired material after two months. Moreover, a meta-analysis conducted by Stamenova and Levine (Citation2019) that included individuals with diverse etiologies provided evidence of the significant impact of GMT implementation on instrumental activities of daily living, which remained observable during subsequent follow-up assessments. However, these studies did not examine the stability of task performance after learning a new task using a different intervention was investigated. In this regard, our study serves as an important addition, as it demonstrates the sustained stability of task performance in delayed retention, even after participants were engaged in practicing an additional task using a different intervention approach. Additionally, our study demonstrated that individuals with intellectual disabilities could learn at least two completely different tasks consecutively (both intervention groups differed significantly from the control group in their performance on the second “Practiced” task), which is an essential finding for the implementation of treatment in the real world resulting from various situations.
However, the sequence in which the interventions were applied was critical to the participant outcomes. The RehaGoal App + EL intervention exhibited a smaller improvement when implemented a second time (after the mGMT training). One possible explanation for this difference may be the perceived sense of autonomy, which is likely to be heightened as a result of the metacognitive therapeutic approach employed in GMT (Cuberos-Urbano et al., Citation2018). Prior familiarity with the mGMT intervention may have constrained the efficacy of the RehaGoal App. The utilization of the RehaGoal App after the introduction of the mGMT training might have prompted participants to systematically interact with the app by activating it upon the completion of each sub-step and proceeding with the subsequent tasks. This tightly integrated guidance could have engendered a sense of frustration, particularly after the participants experienced a higher degree of autonomy in task execution during the prior mGMT intervention. Another explanation might be that the use of EL during Phase I relied on implicit learning that did not interfere with mGMT training as a second intervention, which is more explicit. Therefore, no carry-over effect was present in this intervention sequence compared to the other sequences, where explicit learning to solve a complex task might interfere with the implicit learning of a chain of task steps.
We observed no transfer effect on the GAS for the “Non-Practiced” tasks. Previous research indicates that individuals with executive dysfunction encounter challenges in spontaneously generalizing acquired information to novel contexts (Cicerone & Wood, Citation1987; Von Cramon & Matthes-von Cramon, Citation1994). Although contrasting findings were reported in studies conducted by Richard and Noell (Citation2019) and Jerome et al. (Citation2007), demonstrating the ability of individuals with intellectual disabilities to transfer skills learned through EL to tasks within the same functional context, it is important to note that the tasks used in those studies exhibited a high degree of similarity (e.g., tying different shoes). However, the tasks used in the present study differed significantly.
Additionally, we found no significant impact of etiology, sex, or IQ on the enhancement of task performance. According to existing research, only the study by Bertens et al. (Citation2016) in individuals with brain injuries showed that older age is associated with better performance in everyday tasks following conventional GMT, while a higher IQ was associated with enhanced performance after errorless GMT. No relevant studies examining individuals with intellectual disabilities were identified. Consequently, future research should consider the notable diversity in cognitive abilities within the sample, as this variability may affect the generalizability and applicability of the findings.
For the secondary outcome measures, the neuropsychological tests, only the Tower of London Test documented a significant effect on the number of correct steps. Both intervention groups improved compared with the control group, which achieved slightly inferior results. This finding indicates that the combination of both interventions has a positive impact on problem-solving ability. However, given the numerous statistical comparisons of neuropsychological test results, any interpretation requires replication. The underlying reason for the significant interaction remains undetermined, as none of the groups exhibited a substantial enhancement, suggesting that the observed interaction may be incidental.
Regarding the study design, recruiting participants posed no difficulties as data collection occurred at their respective workplaces. Sixteen participants withdrew from this study. Ten of these withdrawals were attributed to COVID-19 pandemic-related lockdown. Before beginning any intervention, one participant withdrew from the diagnostic phase because of feeling overwhelmed. In the App + ELfirst group, three additional participants discontinued participation. Two participants expressed a preference for working together, whereas one cited the extensive number of sessions as the reason for discontinuation. In the control group, one participant withdrew after the diagnostic phase, citing self-harming behaviour as the cause.
Considering the influence of pandemic-related lockdown measures on the progression of the study, the overall retention rate remained satisfactory. Furthermore, those who continued to participate in the study demonstrated high compliance and successfully completed the study sessions.
This study had limitations that should be acknowledged when interpreting the findings. The assessment instruments used as secondary outcome parameters were not optimally tailored to the target population. The scarcity of neuropsychological tests suitable for individuals with intellectual disabilities necessitated using a conventional test, recognizing that it may not be fully suitable for this particular target group. However, these tests lack normative data specifically applicable to this population. Therefore, adjustments were made to the instructions to ensure the language simplicity.
Moreover, the study may not have been sufficiently powered for the ANOVA analysis in the neuropsychological tests. However, as previously mentioned, these outcomes were part of a secondary analysis, and therefore, all these measurements should be regarded as preliminary.
Additionally, the self-selection of tasks closely aligned with the participants’ job-related tasks represents both a strength and limitation. This approach fosters participants’ motivation as they engage in tasks that they perceive as individually meaningful and highly relevant. However, this introduces variability among participants, as they typically select tasks with varying levels of difficulty or specificity. This variability may manifest both at the intra-individual level, where participants encounter varying levels of difficulty across two different tasks and at the inter-individual level, where different participants face varying levels of task difficulty. Moreover, implementing an individual goal attainment scale designed to align with individually selected tasks adds complexity to comparing task improvements among participants, making it challenging to draw definitive conclusions. The inclusion criteria's reliance on carers also adds another layer of complexity. Carers were given a comprehensive list of symptoms associated with EF impairment and its impact on daily life. Given the difficulties carers may have in differentiating between EF deficits and low intellectual functioning in daily life, some participants included in the study might experience difficulties due to intellectual impairment rather than solely executive dysfunction.
The comprehensive nature of this study, which encompassed three measurement points, precluded the feasibility of conducting a long-term follow-up assessment, representing a study limitation given the absence of a comprehensive evaluation to examine the enduring impact of the intervention over an extended duration.
Conclusion
In conclusion, our research findings demonstrate the efficacy of both the RehaGoalApp with EL and mGMT interventions in improving task performance among adults with intellectual disabilities. Moreover, we found a stable retention effect, even after learning successfully a second task, as a possible source of interference. Therefore, both interventions therefore hold the potential for enhancing the independence and overall quality of life of individuals with intellectual disabilities. However, the effects of both interventions were restricted to the task, as we did not find convincing evidence regarding the transfer to solving other tasks.
Another important finding of our study is that the intervention order may matter. If different tasks are learned, training should start with RehaGoal App with EL using the mGMT method. Unfortunately, the study design did not allow us to conclude that repeating the same method twice led to similar results. Therefore, continued research and implementation of these interventions are warranted to further advance this field and improve the well-being of this population.
Acknowledgements
We thank Franziska Marwedel, Katharina Brunner, Alex Fräßdorf and Lena Kamann for their support in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aschenbrenner, S., Tucha, O., & Lange, K. (2000). Regensburger Wortflüssigkeits-test. Hogrefe.
- Aust, J., & Müller, S. V. (2022). Menschen mit intellektuellen Beeinträchtigungen. In E.-W. Luthe, S. V. Müller, & I. Schiering (Eds.), Gesundheit. Politik - Gesellschaft - Wirtschaft. Assistive Technologien im Sozial- und Gesundheitssektor (pp. 121–139). Springer Fachmedien Wiesbaden. https://doi.org/10.1007/978-3-658-34027-8_7
- Bertens, D., Fasotti, L., Boelen, D. H., & Kessels, R. P. (2016). Moderators, mediators, and nonspecific predictors of treatment outcome in an intervention for everyday task improvement in persons with executive deficits after brain injury. Archives of Physical Medicine and Rehabilitation, 97(1), 97–103. https://doi.org/10.1016/j.apmr.2015.07.021
- Cicerone, K. D., & Wood, J. C. (1987). Planning disorder after closed head injury: A case study. Archives of Physical Medicine and Rehabilitation, 68, 111–115.
- Clare, L., & Jones, R. S. P. (2008). Errorless learning in the rehabilitation of memory impairment: A critical review. Neuropsychology Review, 18(1), 1–23. https://doi.org/10.1007/s11065-008-9051-4
- Cuberos-Urbano, G., Caracuel, A., Valls-Serrano, C., García-Mochón, L., Gracey, F., & Verdejo-García, A. (2018). A pilot investigation of the potential for incorporating lifelog technology into executive function rehabilitation for enhanced transfer of self-regulation skills to everyday life. Neuropsychological Rehabilitation, 28(4), 589–601. https://doi.org/10.1080/09602011.2016.1187630
- Domire, S. C., & Wolfe, P. (2014). Effects of video prompting techniques on teaching daily living skills to children with autism spectrum disorders. Research and Practice for Persons with Severe Disabilities, 39(3), 211–226. https://doi.org/10.1177/1540796914555578
- Emerson, E., Hatton, C., Thompson, T., & Parmenter, T. R. (2004). The international handbook of applied research in intellectual disabilities. Wiley. https://doi.org/10.1002/9780470713198
- Ertas, F., Aust, J., Lorenz, T., Schiering, I., Brunner, K., & Müller, S. V. (2021). Der Einsatz der RehaGoal App durch Menschen mit einer intellektuellen Beeinträchtigung bei der Arbeit zu Hause während der Corona-Pandemie. Zeitschrift für Neuropsychologie, 32(1), 13–23. https://doi.org/10.1024/1016-264X/a000317
- Ertas, F., Gentz, M. L., Frässdorf, A., & Müller, S. V. (2019, August). Goal Management Training enhanced self-awareness in people with Down Syndrome – a pilot-study. Poster session presentation at the meeting of the world congress of the international association für the scientific study of intellectual and developmental disabilities, Glasgow.
- Gabel, A., Ertas, F., Pleger, M., Schiering, I., & Müller, S. V. (2020). Privacy-preserving metrics for an mHealth App in the context of neuropsychological studies. In P. Gómez Vilda, A. Fred, & H. Gamboa (Eds.), BIOSTEC 2020: Vol. 4, BIOSIGNALS (pp. 166–177). SCITEPRESS - Science and Technology Publications Lda. https://doi.org/10.5220/0008982801660177
- García-Pintor, B., Morales-Rodríguez, F. M., & Pérez-Mármol, J. M. (2023). The association between executive function and performing instrumental daily activities in people with intellectual disabilities. Healthcare, 11(17), 2374. https://doi.org/10.3390/healthcare11172374
- Grant, M., Ponsford, J., & Bennett, P. C. (2012). The application of goal management training to aspects of financial management in individuals with traumatic brain injury. Neuropsychological Rehabilitation, 22(6), 852–873. https://doi.org/10.1080/09602011.2012.693455
- Härting, C., Markowitsch, H. J., Neufeld, H., Calabrese, P., Deisinger, K., & Kessler, J. (2000). Wechsler Gedächtnistest - Revidierte Fassung: WMS-R; deutsche Adaptation der revidierten Fassung der Wechsler memory scale [German version of the Wechsler memory scale]. Hans Huber.
- Hendricks, D. (2010). Employment and adults with autism spectrum disorders: Challenges and strategies for success. Journal of Vocational Rehabilitation, 32(2), 125–134. https://doi.org/10.3233/JVR-2010-0502
- Hong, D., Scaletta Kent, J., & Kesler, S. (2009). Cognitive profile of Turner syndrome. Developmental Disabilities Research Reviews, 15(4), 270–278. https://doi.org/10.1002/ddrr.79
- Howlin, P., & Udwin, O. (2006). Outcome in adult life for people with Williams syndrome- results from a survey of 239 families. Journal of Intellectual Disability Research, 50(2), 151–160. https://doi.org/10.1111/j.1365-2788.2006.00775.x
- Huddleston, L. B., Visootsak, J., & Sherman, S. L. (2014). Cognitive aspects of Fragile X syndrome. Wiley Interdisciplinary Reviews: Cognitive Science, 5(4), 501–508. https://doi.org/10.1002/wcs.1296
- Hunkin, N. M., & Parkin, A. L. (1995). The method of vanishing cues: An evaluation of its effectiveness in teaching memory-impaired individuals. Neuropsychologia, 33(10), 1255–1279. https://doi.org/10.1016/0028-3932(95)00061-7
- Jauregi, J., Arias, C., Vegas, O., Alén, F., Martinez, S., Copet, P., & Thuilleaux, D. (2007). A neuropsychological assessment of frontal cognitive functions in Prader-Willi syndrome. Journal of Intellectual Disability Research, 51(Pt 5), 350–365. https://doi.org/10.1111/j.1365-2788.2006.00883.x
- Jerome, J., Frantino, E. P., & Sturmey, P. (2007). The effects of errorless learning and backward chaining on the acquisition of internet skills in adults with developmental disabilities. Journal of Applied Behavior Analysis, 40(1), 185–189. https://doi.org/10.1901/jaba.2007.41-06
- Kiresuk, T. J., & Sherman, R. E. (1968). Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Mental Health Journal, 4(6), 443–453. https://doi.org/10.1007/BF01530764
- Krasny-Pacini, A., Limond, J., Evans, J., Hiebel, J., Bendjelida, K., & Chevignard, M. (2014). Context-sensitive goal management training for everyday executive dysfunction in children after severe traumatic brain injury. The Journal of Head Trauma Rehabilitation, 29(5), E49–E64. https://doi.org/10.1097/HTR.0000000000000015
- Kutschmann, M., Bender, R., Grouven, U., & Berg, G. (2006). Aspekte der Fallzahlkalkulation und Powerberechnung anhand von Beispielen aus der rehabilitationswissenschaftlichen Forschung [Aspects of sample size determination and power calculation illustrated on examples from rehabilitation research]. Die Rehabilitation, 45(6), 377–384. https://doi.org/10.1055/s-2006-940113
- Lasker, A. G., Mazzocco, M. M. M., & Zee, D. S. (2007). Ocular motor indicators of executive dysfunction in fragile X and Turner syndromes. Brain and Cognition, 63(3), 203–220. https://doi.org/10.1016/j.bandc.2006.08.002
- Levine, B., Robertson, I. H., Clare, L., Carter, G., Hong, J., Wilson, B. A., Duncan, J., & Stuss, D. T. (2000). Rehabilitation of executive functioning: An experimental-clinical validation of goal management training. Journal of the International Neuropsychological Society: JINS, 6(3), 299–312. https://doi.org/10.1017/S1355617700633052
- Levine, B., Schweizer, T. A., O'Connor, C., Turner, G., Gillingham, S., Stuss, D. T., Manly, T., & Robertson, I. H. (2011). Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Frontiers in Human Neuroscience, 5, 9. https://doi.org/10.3389/fnhum.2011.00009
- Maxwell, J. P., Masters, R. S. W., Kerr, E., & Weedon, E. (2001). The implicit benefit of learning without errors. Quarterly Journal of Experimental Psychology, 54(4), 1049–1068. https://doi.org/10.1080/713756014
- Mervis, C. B., & John, A. E. (2010). Cognitive and behavioral characteristics of children with Williams syndrome: Implications for intervention approaches. American Journal of Medical Genetics. Part C, Seminars in Medical Genetics, 154C(2), 229–248. https://doi.org/10.1002/ajmg.c.30263
- Miotto, E. C., Evans, J. J., Lucia, M. C. S. d., & Scaff, M. (2009). Rehabilitation of executive dysfunction: A controlled trial of an attention and problem solving treatment group. Neuropsychological Rehabilitation, 19(4), 517–540. https://doi.org/10.1080/09602010802332108
- Moore, D. W., Anderson, A., Treccase, F., Deppeler, J., Furlonger, B., & Didden, R. (2013). A video-based package to teach a child with autism spectrum disorder to write her name. Journal of Developmental and Physical Disabilities, 25, 493–503. https://doi.org/10.1007/s10882-012-9325-x
- Müller, S. V. (2013). Störungen der Exekutivfunktionen (1. Aufl.). Hogrefe Verlag.
- Müller, S. V., Ertas, F., Aust, J., Gabel, A., & Schiering, I. (2019b). Kann eine mobile Anwendung helfen abzuwaschen? Zeitschrift für Neuropsychologie, 30(2), 123–131. https://doi.org/10.1024/1016-264X/a000256
- Müller, S. V., Klein, T., Benke, T., Bohlhalter, S., Hildebrandt, H., Meiling, C., Hucke, B., Münte, T. Penner, I.-K., Schwerdtfeger, K., Thöne-Otto, A. & Wallesch, C. (2019a). Diagnostik und Therapie von exekutiven Dysfunktionen bei neurologischen Erkrankungen, S2e-Leitlinie. In Deutsche Gesellschaft für Neurologie (Ed.), Leitlinien für Diagnostik und Therapie in der Neurologie (pp. 1–67). www.dgn.org/leitlinien.
- Panerai, S., Tasca, D., Ferri, R., Genitori D'Arrigo, V., & Elia, M. (2014). Executive functions and adaptive behaviour in aAutism spectrum disorders with and without intellectual disability. Psychiatry Journal, 941809. https://doi.org/10.1155/2014/941809
- Rayner, C. (2011). Teaching students with autism to tie a shoelace knot using video prompting and backward chaining. Developmental Neurorehabilitation, 14(6), 339–347. https://doi.org/10.3109/17518423.2011.606508
- Reischies, F. M. (2007). Exekutive Funktionen und Arbeitsgedächtnis. In F. M. Reischies (Ed.), Psychopathologie (pp. 101–107). Springer. https://doi.org/10.1007/978-3-540-37254-7_6
- Rhodes, S. M., Riby, D. M., Matthews, K., & Coghill, D. R. (2011). Attention-deficit/hyperactivity disorder and Williams syndrome: Shared behavioral and neuropsychological profiles. Journal of Clinical and Experimental Neuropsychology, 33(1), 147–156. https://doi.org/10.1080/13803395.2010.495057
- Richard, P. R., & Noell, G. H. (2019). Teaching children with autism to tie their shoes using video prompt-models and backward chaining. Developmental Neurorehabilitation, 22(8), 509–515. https://doi.org/10.1080/17518423.2018.1518349
- Rowe, J., Lavender, A., & Turk, V. (2006). Cognitive executive function in Down's syndrome. The British Journal of Clinical Psychology, 45(1), 5–17. https://doi.org/10.1348/014466505X29594
- Smith, K. A., Shepley, S. B., Alexander, J. L., & Ayres, K. M. (2015). The independent use of self-instructions for the acquisition of untrained multi-step tasks for individuals with an intellectual disability: A review of the literature. Research in Developmental Disabilities, 40, 19–30. https://doi.org/10.1016/j.ridd.2015.01.010
- Sohlberg, M. M., Ehlhardt, L., & Kennedy, M. (2005). Instructional techniques in cognitive rehabilitation: A preliminary report. Seminars in Speech and Language, 26(4), 268–279. https://doi.org/10.1055/s-2005-922105
- Stamenova, V., & Levine, B. (2019). Effectiveness of goal management training® in improving executive functions: A meta-analysis. Neuropsychological Rehabilitation, 29(10), 1569–1599. https://doi.org/10.1080/09602011.2018.1438294
- Tucha, O,LKW. (2004). Turm von London-Deutsche Version [Tower of London – German Version]. Hogrefe.
- Von Cramon, D. Y., & Matthes-von Cramon, G. (1994). Back to work with a chronic dysexecutive syndrome? (A case report). Neuropsychological Rehabilitation, 4, 399–417. https://doi.org/10.1080/09602019408401608
- Wilson, B. A., Alderman, N., Burgess, P. W., et al. (1997). Behavioural assessment of the dysexecutive syndrome. In P. Rabbitt (Ed.), Methodology of frontal and executive function (pp. 232–243). Routledge.
