Abstract
Purpose: To examine the impact of neonatal brachial plexus palsy (NBPP) on societal participation of adolescents and adults.
Methods: This cross-sectional study was conducted among patients with NBPP, aged ≥16 years, who had visited our NBPP clinic. Patients completed questions on the influence of NBPP on their choices regarding education/work and their work-performance, the Impact on Participation/Autonomy questionnaire and the Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-P). In addition, health-related quality of life (HRQoL) was assessed.
Results: Seventy-five patients participated (median age 20, inter quartile range 17–27). Twenty were full-time students, 28 students with a job, 21 employed, two unemployed, and four work-disabled. Sixty-six patients had had a job at some stage. Patients’ overall HRQoL was comparable to the general population. 27/75 patients reported that NBPP had affected their choices regarding education and 26/75 those regarding work. 33/66 reported impact on their work performance. On the Impact on Participation/Autonomy questionnaire, 80% (49/61) reported restrictions in the work-and-education domain, 74% in social-relations and 67% in autonomy-outdoors. 37/61 reported participation restrictions on the USER-P.
Conclusions: Although their overall HRQoL was not impaired, a substantial proportion of adolescent/adult patients reported that NBPP had an impact on choices regarding education and profession, as well as on work-performance. Restrictions in participation, especially in work and education were also reported. Guiding patients in making choices on education and work at an early stage and providing tailored physical as well as psychosocial care may prevent or address restrictions, which may improve participation.
Adolescent and adult patients with neonatal brachial plexus palsy perceive restrictions in societal participation, especially regarding the work-and-education domain.
All patients with neonatal brachial plexus palsy may perceive restrictions in societal participation regardless of lesion severity, treatment history and side of the lesion.
Adolescents and adults with neonatal brachial plexus palsy report that their choices regarding education and work, as well as their work-performance are influenced by their neonatal brachial plexus palsy.
Patients with neonatal brachial plexus palsy should be followed throughout their life in order to provide them with appropriate information and treatment when health- or participation-related issues arise.
Rehabilitation treatment is the best option to address all of the aforementioned issues, as surgical options in adolescents and adults are limited.
Implications for Rehabilitation
Introduction
Neonatal brachial plexus palsy (NBPP) is caused by traction to the brachial plexus during delivery and can result in severe disabilities of the arm. The incidence varies between 1.6 and 4.6/1000 live births [Citation1,Citation2]. Severity of the injury ranges from mild (neurapraxia/axonotmesis) to severe (neurotmesis/avulsion), but the majority of NBPP is mild and complete, or almost complete, functional recovery will occur in about 70–80% [Citation1,Citation3]. The remaining patients are left with a functional deficit that probably results in problems in one or more domains of the International Classification of Functioning, Disability and Health (ICF) [Citation4]. Mild injuries can be treated conservatively, while children with more severe injuries often require primary surgery (nerve reconstruction) at a young age (3–9 months) [Citation5,Citation6]. Depending on recovery after conservative treatment or primary surgery, secondary surgery (muscle-tendon transfers/osseous surgery) may be indicated at a later age [Citation7–11]. Despite these interventions, patients with NBPP may still have residual functional limitations that may lead to restrictions or limitations in one or more domains of the ICF.
The above-mentioned surgical and non-surgical interventions are performed in infants and children to improve arm function, activity levels and future societal participation, including education, employment, leisure activities, and community living. However, outcome regarding participation among patients with NBBP in later life has rarely been examined [Citation12], and long-term follow-up studies including adults are limited or outdated [Citation13]. The few available studies among adolescents (≥16 years) and adult patients with NBPP mainly evaluated daily functioning (e.g., dressing, washing) and found that patients experienced limitations, mostly due to pain [Citation14,Citation15]. Although daily activities, such as cycling and swimming, were limited, patients could still participate in them [Citation16]. A qualitative study using focus groups included adolescents aged 16 and 17 years and reported perceived problems with activities (e.g., self-care, eating) and sports participation (e.g., swimming, gymnastics, football, dancing). This study, however, also reported that the older participants had adapted to their disabilities over time and therefore perceived less problems [Citation17]. Another study found that participation among patients with NBPP (aged 15-17 years) did not differ from that of age-matched healthy peers [Citation18]. Another study reported that few adult patients experienced limitations of work-performance [Citation14]. The main drawback of these studies is that adult patients were either not included, or included in limited numbers only. Furthermore, no validated instruments specifically designed to measure participation were used.
Currently, no study is available in the literature that reports on the possible influence of NBPP on choices regarding education and work. Studies in other medical conditions that cause limitations to upper extremity function (e.g., cerebral palsy, spinal cord injury [SCI] or hereditary motor and sensory neuropathy [HMSN]) reported restrictions in participation in later life (e.g., education, employment, leisure activities, and community living) [Citation19–23]. For patients with these conditions, factors influencing restrictions in participation included condition severity, upper extremity functioning, dexterity and level of education [Citation19–23].
It is unknown to what extent participation by patients with NBPP is influenced by lesion-extent, the affected side, health-related quality of life (HRQoL), upper extremity functioning and pain.
The aim of this study was to investigate if, and to what extent, adolescents (≥16 years) and adults with NBPP face participation restrictions, and if NBPP has any influence on choices regarding education and work as well as on work-performance. A secondary aim was to determine which factors were associated with restrictions in participation in this patient group. We hypothesized that more restrictions in participation among patients with NBPP would be associated with right-sided lesions, greater lesion extent, having had primary and/or secondary surgery, poorer upper extremity function, poorer HRQoL and having bodily pain.
Methods
Study design and patients
A cross-sectional study on the functioning and quality of life of patients with NBPP of all ages (n = 1142) was conducted between October 2014 and March 2015 [Citation24]. The study was conducted at the Leiden Nerve Center (a specialized multidisciplinary NBPP clinic located at the Leiden University Medical Center). It was approved by the local medical ethics committee (P14.071).
For the larger study, all patients with a diagnosis of NBPP who had visited the Leiden Nerve Center at least once were eligible. Patients were excluded if their medical record was not available or if concurrent or other medical diagnoses that might affect arm function were mentioned in their medical record (e.g., traumatic brachial plexus lesions, cerebral palsy, birth reduction defects: anatomical upper arm anomalies).
Eligible patients and/or their parents were sent an invitation (including information) to participate. The invitation included a statement that all data would be treated confidentially and analyzed anonymously. On a pre-stamped return card, they could indicate whether they were willing to participate, and if so, whether they wanted to participate using paper or electronic questionnaires. Parents of patients under 18 years of age and all patients aged 12 years and older provided written informed consent. After informed consent, patients were sent the set of questionnaires or received an e-mail with a link giving access to the electronic questionnaires. Patients not responding to the invitation received a reminder by mail, phone or e-mail at their last known contact details within 2–4 weeks. Participants who had not completed the questionnaires within 2–4 weeks were reminded by email or phone.
The aims of this cross-sectional study were set in advance and, as the cohort included patients with a large variety of ages, it used age-appropriate questionnaires. The full set of questionnaires used in the study (including those used for the present study) were tested prior to the start. The present study only used data from patients aged ≥16 years. The study was conducted and reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies [Citation25].
NBPP and patient characteristics
Age, gender, lesion-extent (i.e., upper plexus lesions: C5–C6 or C5–C7, and 2: total plexus lesions: C5–C8 or C5–T1), affected side (right/left/both), treatment history (i.e., conservative, primary [nerve] surgery secondary [orthopedic] surgery, both primary and secondary surgery) were extracted from the medical record and current status regarding discharge from follow-up (yes/no) was recorded. All this information was recorded by the two first authors and entered into an existing database, in part comprising the same data, thereby creating a quality check on the data.
Participation
Study and work
To analyze work and education status and the possible influence of NBPP on these aspects, we used a questionnaire constructed for the occasion. Eight questions were formulated, based on the expert opinions of all authors, addressing important issues of education and work for adolescents and adults with NBPP (see ).
Impact on Participation and Autonomy (IPA)
The IPA, Dutch Language Version (IPA-DLV) instrument was developed using the ICF components and has proven to be a valid and reliable tool to use in chronic disease populations [Citation26–28]. This tool was, however, not specifically designed for NBPP. IPA measures patient-perceived participation in five domains: autonomy indoors (self-care and mobility indoors, seven items), family role (housekeeping and spending income, seven items), autonomy outdoors (leisure activities and mobility outdoors, five items), social relations (equal communication and intimate relations, seven items) and work and education (paid work, volunteer work and education, six items). Each item in the domains is scored on a five-point rating scale (0: very good to 4: very poor). Domain scores range from 0 to 4, with higher scores indicating lower participation. A score of 0 means no restrictions are reported. IPA also includes nine items to determine the extent to which patients perceive their restrictions in participation as problematic, on a three-point rating scale (0 = no problem to 2 = severe problem).
Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-P)
The USER-P questionnaire is a generic 31-item, self-reported outcome instrument for adults, suitable and reliable for evaluating physical disabilities, including musculoskeletal and neurological conditions [Citation29].
This tool was designed to rate objective and subjective participation in rehabilitation in three domains: frequencies, restrictions, and satisfaction. The frequency scale quantifies how much time is spent per week on several participation activities (e.g., work, education, housekeeping, leisure activities, sports, visiting family and friends). The USER-P assesses perceived restrictions and patient satisfaction with regard to performing these activities. Scores range from 0 to 100, with higher scores indicating better functioning (higher frequency, less restrictions, and greater satisfaction).
Measures of current HRQoL and functioning (including pain)
Short Form-36 (SF-36)
The current perceived HRQoL and its association with participation were determined using the SF-36, Dutch Language Version (SF-36-DLV) [Citation30]. This generic HRQoL instrument has been used before in other NBPP studies [Citation14]. In the SF-36, eight domain scores can be calculated, including the bodily pain score. Scores range from 0 to 100, with higher scores indicating better functioning/HRQoL. In addition, two summary scores can be calculated: a physical and a mental component score (PCS and MCS, respectively). These scores are based on normative sample data for Dutch adults (n = 1062), with mean summary scores (PCS/MCS) of 50 (SD 10) [Citation31–33]. This enabled comparison with the outcomes of the present study.
Disabilities of the Arm, Shoulder and Hand (DASH)
The current perceived upper extremity functioning and its association with participation were determined using the DASH, Dutch Language Version (DASH-DLV) [Citation34]. This questionnaire has also previously been used in other NBPP studies, allowing comparison of outcomes [Citation14]. The general part (DASH-mean) consists of 30 questions and there is an additional specific module for work (DASH-work, four questions) and a module for sports (DASH-sport, four questions). Scores range from 0 to 100, with lower scores indicating better functioning. US reference scores are available to compare DASH outcomes [Citation35].
Statistical analysis
Descriptive statistics (medians with interquartile ranges [IQR] or means with standard deviations [SD] based on the distribution of the data [Kolmogorov–Smirnov’s test]) were used for patient and lesion characteristics, and for measures of participation and quality of life.
In order to investigate response-bias, the characteristics of the study participants in terms of age, gender, affected side, treatment history and current state of follow-up were compared with eligible patients who did not participate, using Mann–Whitney’s U and Chi Square tests.
To determine which factors were associated with participation, separate linear regression analyses (with categorical or continuous predictors) were performed for all IPA and USER-P subscales, adjusted for age and gender (significance level p < 0.05). For each factor, a new analysis was performed. In essence a “univariate” linear regression analysis, adjusted for age and gender was performed for each independent factor.
Factors entered independently were: lesion extent (upper plexus lesions/total plexus lesions), treatment history (conservative, primary [nerve] surgery, secondary [orthopedic] surgery, primary and secondary surgery) affected side (right/left/both) SF-36 PCS, SF-36 MCS, SF-36 bodily pain score and DASH-mean. β-Estimates were reported to describe the association between the independent factor and the outcome variable. Due to the explorative nature of this study, we did not correct for multiple testing [Citation36].
Results
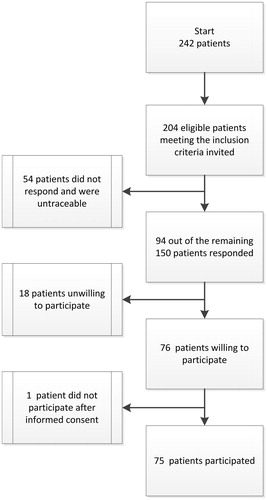
Recruitment and inclusion: There were 242 patients aged ≥16 years of whom 38 were excluded based on the exclusion criteria (medical record not available: n = 16, concurrent or other medical diagnoses: n = 22). For 54 patients, the last known phone number proved incorrect and these patients did not respond to our invitation by mail either. Eventually, 94 of the remaining 150 patients responded, yielding a response rate of 63%. Of the 94 responding patients, 76 patients were willing to participate. One did not return any of the questionnaires and was therefore additionally excluded. shows the flow of these patients.
Patient characteristics: shows the patient characteristics and the HRQoL, pain and upper extremity functioning scores. The median age of the patients was 20 years (IQR 17–27). Ninety-two percent had upper plexus lesions (C5–C6/C5–C7). Characteristics of participants (n = 75) and non-participants (n = 129) were comparable, except for gender (more females in the participants group: 65% versus 47%, p = 0.03) and lesion extent (more C5–C7 lesions in the participants group: 40% versus 12% p < 0.001). The participants reported good overall HRQoL on the SF-36: the component scale scores (MCS/PCS) were comparable to those of the Dutch general population. Upper extremity functioning as reported on the DASH also appeared to be good and was comparable to that of the US general population.
Table 1. Patient characteristics, and DASH and SF-36 scores of 75 adolescents and adult patients with NBPP.
Education and work status were as follows: 20 participants (27%) were full-time students, 28 (37%) students who also had a job on the side, 21 (28%) had paid employment, two (3%) were unemployed and four (5%) were work-disabled due to their NBPP. Educational levels were comparable to those in the general Dutch population [Citation37]. The impact of NBPP on choice of education and profession and its impact on performance during these activities are shown in .
Table 2. Education status, work status and the influence of NBPP on education and work among 75 adolescent and adult patients with NBPP.
shows the participation outcomes (IPA/USER-P). Due to missing values, scores of only 61 participants could be calculated. Overall the IPA median standardized domain sum scores were rather low, indicating that the participants perceived few participation restrictions. This is also reflected in the number of participants who perceived their participation as good or very good. Median scores ranged from 0.14 to 1.00, with the lowest score for autonomy indoors (self-care and mobility indoors) and the highest for work and education. Eighty percent of the participants reported at least one restriction in the work and education domain. At least one restriction in the domains of autonomy outdoors (leisure activities and mobility outdoors) and social relations (equal communication and intimate relations) was reported by 74% and 67% of participants, respectively. The highest percentage of participants rating their restrictions in participation as problematic (minor or severe) was in the work (occupation) and education domain.
Table 3. Participation scores (IPA and USER-P) of 61 adolescent and adult patients with NBPP.
According to the USER-P outcomes, 61% of the participants reported perceiving restrictions in participation. Although the number of perceived restrictions was low, the participants did feel dissatisfied with them. In contrast, 82% of the participants reported on the USER-P that they were satisfied with their paid or unpaid work and/or education.
shows the factors influencing participation. Higher DASH-mean scores and lower SF-36 bodily pain, PCS and MCS scores, were independently associated with higher scores on almost all IPA domains (all p < 0.05 to p < 0.001), indicating poorer participation and less autonomy. As regards the scores on the USER-P domains of restriction and satisfaction, the same factors negatively influenced participation (all p < 0.05 to p < 0.001), which means that these factors led to more restrictions and less satisfaction. No evidence was found for lesion extent, treatment history or affected side influencing participation outcomes.
Table 4. Factors influencing participation in 61 adolescent and adult patients with NBPP (linear regression analyses adjusted for age and gender).
Discussion
Participants of this cross-sectional study among adolescents (≥16 years) and adults with NBPP reported good quality of life and upper extremity functioning overall. Although participation was generally also reported to be good, participants did report restrictions in societal participation, mainly related to work (work performance), and influence of NBPP on choice of education and profession. Half of the participants who had had a job at some point, felt professionally hampered by their NBPP. Of the 61 participants who completed the IPA, 49 (80%) reported limitations in the work and education domain. Scores on the USER-P indicated restrictions in participation, and satisfaction with participation possibilities in our participants was somewhat diminished. Restrictions in participation were associated with poorer upper extremity functioning, poorer HRQoL and more pain (DASH/SF-36). No evidence was found for an association with lesion extent, treatment history or affected side. This may indicate that all patients with NBPP, regardless of the initial severity of their lesion may perceive restrictions in participation in later life.
No study previously assessed the impact of NBPP on choice of education and work, and to our knowledge, this is the first study to report on restrictions in participation among adolescents and adults with NBPP, based on validated participation outcome instruments.
Many of our participants reported that NBPP influenced their choice of education and profession. The actual percentages might even be higher, as a large part of our study population was under 20 years of age (n = 36) and might not yet have decided on further education and/or profession. A follow-up study among the same population in a few years could reveal whether the younger participants who currently reported no influence, perceive impact on future choices.
In the current study, we only provided outcomes for the total group and did not differentiate the analyses or results according to lesion-extent or bilateral involvement. Although these patients may perceive more restrictions in participation, the regression analysis provided no evidence for an influence of lesion-extent or bilateral involvement on participation outcomes. Future studies on participation issues should include more patients with total plexus lesions and/or bilateral involvement, to investigate whether lesion-extent or bilateral involvement does indeed not affect participation outcomes.
Participation levels of adolescents (aged 15–17 years) have been investigated previously by Strombeck and Fernell [Citation18], who reported no differences with age-matched controls. The NBPP group in their study had the same interests, activities and social life as the control group, but had lower self-esteem regarding sports and motor activities and worried more about social life and school factors. We feel that these findings actually support our conclusion that participation is influenced by NBPP. Activities and sports are usually chosen within the patients’ capabilities, probably excluding several sports/activity options, which influences participation.
There have been few studies among adolescents (≥16 years) and adult patients with NBPP, that focused on the presence of pain and limitations in activities of daily living [Citation14–16]. In line with their findings, our study participants also reported pain and limitations in activities. Partridge and Edwards [Citation15] reported that adult patients with NBPP experience increasing pain over time and this pain was the most impairing factor in their daily life. de Heer et al. [Citation14] recently confirmed this finding in a small group of adult patients with NBPP (n = 27), for whom pain, rather than arm-hand function, explained difficulties in performing activities of daily living. We found that both pain and arm-hand functioning (DASH-mean) restricted societal participation. Furthermore, in contrast to the study by de Heer et al., we found substantial restrictions in work-performance. Thirty-three of our participants (33/66 [50%] of the participants who have, or had, work) reported feeling hampered by their NBPP in performing their jobs. The reasons for this difference might be that our population was bigger and more of our patients had a job. Furthermore, our population was more severely affected, as 34/75 (45%) of our participants had undergone primary (nerve) surgery compared to 6/27 (22%) in de Heer’s study. However, in our population we found no association between lesion severity and treatment history on the one hand and participation outcomes (IPA and USER-P) on the other. We also found that reported restrictions in participation, including those in the work and education domain, were not influenced by the side of the lesion. Yang et al. reported that only 17% of children with a right-sided lesion were right-handed, compared to 90% in the healthy population [Citation38]. This indicates that these children have developed left-hand preference due to their right-sided lesion in order to have one good arm/hand. The fact that the side of the lesion did not correlate with “work and education participation” in our study may indicate that bimanual functioning may be more important than handedness.
The aforementioned studies regarding problems of daily living may have had biases that influenced the outcome. Kirjavainen et al. [Citation16] included only surgically treated patients, leading to a bias towards more severe lesions, and did not specify the number of participating adolescents and adults [Citation16]. All patients in the study by Partridge and Edwards [Citation15] were members of the Erb’s Palsy Group in the United Kingdom, which could possibly have led to confounding by indication (i.e., patients who are members of patient groups and respond to surveys sent out by these groups, are usually the more affected patients). The present study included patients with lesions ranging from relatively mild, treated conservatively, to severe lesions that warranted nerve reconstruction. We hope to have provided a better representation of the NBPP population, although we acknowledge that including patients from a tertiary referral clinic has probably led to inclusion bias as well.
Our main outcome measures for societal participation, the IPA and USER-P questionnaires, have not been used previously in NBPP studies, nor have they been validated for this patient group. However, they have been used and validated in several other chronic conditions affecting upper limb function, such as stroke, SCI, and HMSN [Citation26,Citation29].
On the IPA, our NBPP patients reported better societal participation than patients after SCI, with 55% of these SCI patients reporting poor social participation and autonomy on several IPA-domains [Citation20]. In our NBPP study we found 3–36% (depending on the IPA domain) of participants reporting fair to poor societal participation. Most restrictions in participation were reported in the work and education domain. Compared to IPA scores of patients with HMSN type 1A [Citation23], our patients reported similar restrictions in autonomy outdoors and work and education.
On the USER-P, patients with SCI had a perceived restrictions score of 72.7 points (IQR 54.5–87.9) and a satisfaction score of 72.5 (IQR 58.3–80.6) [Citation19]. Our participants had a higher perceived restrictions score (median 96.9/IQR 90–100), but had comparable satisfaction scores (median 77.8/IQR 69.6–91.7) [Citation19].
Contrary to the conditions in the above studies, our participants had had their deficit(s) since birth. Thus, we had expected that our patients with NBPP would adapt more automatically regarding their participation level, and feel satisfied with choices made within their possibilities. Such adaptation was suggested by the results of the focus group study that was conducted earlier at our center by Sarac et al. [Citation17]. In this study, children seemed to adapt more fully to their disability with age, and personal and environmental factors played an important role in this [Citation17]. In comparison, the same restricted societal participation, as found in the current study, was found in young adults with cerebral palsy, who also have their deficits from birth: about 20–30% of young adults with cerebral palsy report restrictions in societal participation [Citation21]. Future participation studies should also address the influence of psychosocial adjustment and family dynamics in adult patients with NBPP.
We used the SF-36 and DASH questionnaires to determine current HRQoL and upper extremity functioning because reference values for the general population were available and because they have previously been used in other NBPP studies on participation [Citation14,Citation33,Citation35]. SF-36 and DASH scores in our population are comparable to those reported by de Heer et al., but DASH-work scores in our population were somewhat higher than reported in that study [Citation14]. As outcomes on the SF-36 and DASH were also comparable to the general population [Citation30,Citation33,Citation35], the question remains whether these instruments are sensitive and specific enough to detect the specific limitations in the NBPP population (e.g., insufficient bimanual activities in the DASH to measure problems in unilateral impairments).
Half of the study population were no longer in clinical follow-up at the Leiden Nerve Center at the time of this study. We discharge patients from follow-up when good neurological recovery has taken place or if residual deficits have reached a plateau. We provide them with information for the future and advise them to make a new appointment for renewed evaluation or treatment if necessary. However, it turns out that many of them reported restrictions in participation, pain and functional limitations, but did not seek to contact us. We do not know who is the primary medical caregiver for these patients and with whom they discuss their participation limitations. These issues should be addressed in future studies to further optimize care and clinical follow-up for adolescents and adults with NBPP.
Possible interventions in adult patients with NBPP are limited and have not been well described. The findings in this study indicate that there is a need for interventions in adulthood. Rehabilitation programs or information provision programs are needed for adolescent and adult patients to enable them to cope better with their disability. These programs could, for example, focus on patient education (especially in the work and education domain), vocational rehabilitation, psychosocial wellbeing, improving ergonomics and pain reduction.
The present study had a number of limitations. It had a cross-sectional design with no follow-up, using only self-reported questionnaires. This might lead to overestimation or underestimation of results, as participants might be influenced by unknown factors at the time of completing the questionnaires (e.g., bad mood, stress, etc.). Only 75 of the 204 eligible patients participated in the present study. This number was limited because not all eligible patients could be traced and reached. The number of participants may also have been influenced by the fact that over half of the eligible patients were no longer in follow-up and their last visit could be years ago. The response rate was further reduced as some of the 75 participating patients did not complete all questionnaires (n = 9 for DASH and SF-36, n = 14 for IPA and USER-P), even after several reminders, possibly due to questionnaire burnout. The participating group (n = 75) did not differ significantly from the non-responding group (n = 129) in terms of patient and disease characteristics. Patients seen at our NBPP clinic were referred to us because of a severe lesion, which might lead to confounding by indication. However, we believe the responders, including conservatively treated patients, are sufficiently representative of adolescents and adults seen at NBPP clinics in an academic setting.
As discussed above, the generic participation outcome measures used in the present study were not validated for use in patients with NBPP. However, as shown in a recent review regarding outcome measures in NBPP, no appropriate NBPP-specific participation outcome measures are available [Citation12]. The outcome measures used in our study seem to provide valuable information, and further studies into the validity and reliability of their use in the NBPP population should be undertaken to fill the gap in available outcome measures in this important ICF domain. In addition, future long-term NBPP studies among children and adults should at least include participation outcome measures.
In conclusion, adolescents and adults with NBPP participating in the current study reported restrictions in societal participation, particularly in terms of work and education, and they perceived NBPP as an influence on their choice of education and profession, and on their work performance. These findings are relatively new and reveal a need for optimization of care, follow-up and information, focusing on the participation components of the ICF for adolescents and adult patients with NBPP.
Disclosure statement
The authors report no conflict of interest.
References
- Pondaag W, Malessy MJ, van Dijk JG, et al. Natural history of obstetric brachial plexus palsy: a systematic review. Dev Med Child Neurol. 2004;46:138–144.
- Hoeksma AF, Wolf H, Oei SL. Obstetrical brachial plexus injuries: incidence, natural course and shoulder contracture. Clin Rehabil. 2000;14:523–526.
- Chauhan SP, Blackwell SB, Ananth CV. Neonatal brachial plexus palsy: incidence, prevalence, and temporal trends. Semin Perinatol. 2014;38:210–218.
- WHO. ICF 2016; [cited 2016 Jul 01]. Available from: http://www.who.int/classifications/icf/en/
- Gilbert A, Pivato G, Kheiralla T. Long-term results of primary repair of brachial plexus lesions in children. Microsurgery. 2006;26:334–342.
- Pondaag W, Malessy MJ. The evidence for nerve repair in obstetric brachial plexus palsy revisited. Biomed Res Int. 2014;2014:434619.
- Hale HB, Bae DS, Waters PM. Current concepts in the management of brachial plexus birth palsy. J Hand Surg Am. 2010;35:322–331.
- Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005;14:233–244.
- Lagerkvist AL, Johansson U, Johansson A, et al. Obstetric brachial plexus palsy: a prospective, population-based study of incidence, recovery, and residual impairment at 18 months of age. Dev Med Child Neurol. 2010;52:529–534.
- Arzillo S, Gishen K, Askari M. Brachial plexus injury: treatment options and outcomes. J Craniofac Surg. 2014;25:1200–1206.
- Thatte MR, Mehta R. Obstetric brachial plexus injury. Indian J Plast Surg. 2011;44:380–389.
- Sarac C, Duijnisveld BJ, van der Weide A, et al. Outcome measures used in clinical studies on neonatal brachial plexus palsy: a systematic literature review using the International Classification of Functioning, Disability and Health. PRM. 2015;8:167–185. quiz 85–86.
- Gjorup L. Obstetrical lesion of the brachial plexus. Acta Neurol Scand. 1966;42:Suppl. 18:1–80.
- de Heer C, Beckerman H, Groot V. Explaining daily functioning in young adults with obstetric brachial plexus lesion. Disabil Rehabil. 2015;37:1455–1461.
- Partridge C, Edwards S. Obstetric brachial plexus palsy: increasing disability and exacerbation of symptoms with age. Physiother Res Int. 2004;9:157–163.
- Kirjavainen MO, Remes VM, Peltonen J, et al. Permanent brachial plexus birth palsy does not impair the development and function of the spine and lower limbs. J Pediatr Orthop B. 2009;18:283–288.
- Sarac C, Bastiaansen E, Van der Holst M, et al. Concepts of functioning and health important to children with an obstetric brachial plexus injury: a qualitative study using focus groups. Dev Med Child Neurol. 2013;55:1136–1142.
- Strombeck C, Fernell E. Aspects of activities and participation in daily life related to body structure and function in adolescents with obstetrical brachial plexus palsy: a descriptive follow-up study. Acta Paediatr. 2003;92:740–746.
- Mader L, Post MW, Ballert CS, et al. Metric properties of the Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-Participation) in persons with spinal cord injury living in Switzerland. J Rehabil Med. 2016;48:165–174.
- Craig A, Nicholson Perry K, Guest R, et al. Adjustment following chronic spinal cord injury: determining factors that contribute to social participation. Br J Health Psychol. 2015;20:807–823.
- Donkervoort M, Roebroeck M, Wiegerink D, et al. Determinants of functioning of adolescents and young adults with cerebral palsy. Disabil Rehabil. 2007;29:453–463.
- van Meeteren J, Roebroeck ME, Celen E, et al. Functional activities of the upper extremity of young adults with cerebral palsy: a limiting factor for participation? Disabil Rehabil. 2008;30:387–395.
- Videler AJ, Beelen A, van Schaik IN, et al. Limited upper limb functioning has impact on restrictions in participation and autonomy of patients with hereditary motor and sensory neuropathy 1a. J Rehabil Med. 2009;41:746–750.
- van der Holst M, van der Wal CW, Wolterbeek R, et al. Outcome of secondary shoulder surgery in children with neonatal brachial plexus palsy with and without nerve surgery treatment history: a long-term follow-up study. J Rehabil Med. 2016;48:609–617.
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18:800–804.
- Cardol M, de Haan RJ, van den Bos GA, et al. The development of a handicap assessment questionnaire: the Impact on Participation and Autonomy (IPA). Clin Rehabil. 1999;13:411–419.
- Cardol M, de Haan RJ, de Jong BA, et al. Psychometric properties of the Impact on Participation and Autonomy Questionnaire. Arch Phys Med Rehabil. 2001;82:210–216.
- Cardol M, Beelen A, van den Bos GA, et al. Responsiveness of the Impact on Participation and Autonomy questionnaire. Arch Phys Med Rehabil. 2002;83:1524–1529.
- Post MW, van der Zee CH, Hennink J, et al. Validity of the Utrecht scale for evaluation of rehabilitation-participation. Disabil Rehabil. 2012;34:478–485.
- Aaronson NK, Muller M, Cohen PD, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51:1055–1068.
- Ware J. SF-36 health survey manual and interpretation guide. Boston (MA): The Health Institute, New England Medical Center; 1994.
- VanderZee KI, Sanderman R, Heyink JW, et al. Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med. 1996;3:104–122.
- Ware JEKM, Keller SD. SF-36 physical and mental summary scales: a user’s manual. 2nd ed. Boston (MA): The Health Institute; 1994.
- Veehof MM, Sleegers EJ, van Veldhoven NH, et al. Psychometric qualities of the Dutch language version of the Disabilities of the Arm, Shoulder, and Hand questionnaire (DASH-DLV). J Hand Ther. 2002;15:347–354.
- Hunsaker FG, Cioffi DA, Amadio PC, et al. The American academy of orthopaedic surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84-A:208–215.
- Wason JM, Stecher L, Mander AP. Correcting for multiple-testing in multi-arm trials: is it necessary and is it done? Trials. 2014;15:364.
- Centraal Bureau voor Statistiek (Netherlands Statistics C. Bevolking; hoogst behaald onderwijsniveau; geslacht, leeftijd en herkomst [Internet]. Centraal Bureau voor Statistiek (Netherlands Statistics, CBS); 2016; [cited 2016 Nov 29]. Available from: http://statline.cbs.nl/Statweb/publication/?DM=SLNL&PA=82275NED&D1=0&D2=0&D3=0&D4=0-1,4-5&D5=0-1,7,11&D6=60-63,65-67&VW=T
- Yang LJ, Anand P, Birch R. Limb preference in children with obstetric brachial plexus palsy. Pediatr Neurol. 2005;33:46–49.